Abstract
Objectives
To evaluate the diagnostic accuracy and variability of 3 semi-quantitative (SQt) methods for assessing right ventricular (RV) systolic function from cardiac MRI in patients with acquired heart disease: tricuspid annular plane systolic excursion (TAPSE), RV fractional-shortening (RVFS) and RV fractional area change (RVFAC).
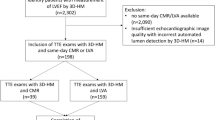
Methods
Sixty consecutive patients were enrolled. Reference RV ejection fraction (RVEF) was determined from short axis cine sequences. TAPSE, RVFS and RVFAC were measured on a 4-chamber cine sequence. All SQt analyses were performed twice by 3 observers with various degrees of training in cardiac MRI. Correlation with RVEF, intra- and inter-observer variability, and receiver operating characteristic (ROC) curve analysis were performed for each SQt method.
Results
Correlation between RVFAC and RVEF was good for all observers and did not depend on previous cardiac MRI experience (R range = 0.716–0.741). Conversely, RVFS (R range = 0.534–0.720) and TAPSE (R range = 0.482–0.646) correlated less with RVEF and depended on previous experience. Intra- and inter-observer variability was much lower for RVFAC than for RVFS and TAPSE. ROC analysis demonstrated that RVFAC <41% could predict a RVEF <45% with 90% sensitivity and 94% specificity.
Conclusions
RVFAC appears to be more accurate and reproducible than RVFS and TAPSE for SQt assessment of RV function by cardiac MRI.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Evaluation of right ventricular (RV) structure and function is of importance in the management of most cardiac disorders. Indeed, previous studies have demonstrated the key role of RV function in predicting outcome in both congenital (CHD) [1] and acquired heart disease (AHD), including heart failure [2, 3], ischaemic cardiopathies [4], pulmonary hypertension [5], arrhythmogenic right ventricular dysplasia (ARVD) [6], valvular heart disease [7], myocarditis [8] and dilated cardiomyopathies [9]. Yet, evaluation of RV function is often neglected in patients with AHD compared with CHD patients, in whom RV function and volumes are extensively evaluated. Non-invasive cardiac imaging plays a leading role in RV function assessment. However, RV imaging has always been considered challenging, mainly because of the complex motion and anatomy of the RV. Various imaging techniques can be used to evaluate RV function: transthoracic echocardiography (TTE) [10], cardiac MRI, radionuclide-based techniques [11] or multislice computed tomography [12]. Cardiac MRI, with the quantitative (Qt) 3D volumetric method, is considered the most reliable method for assessing RV volumes and ejection fraction (EF) and is routinely performed in a large spectrum of diseases [13]. However, cardiac MRI remains time consuming for RV function assessment, as reported in previously published studies [14–16]. Indeed, post-processing software solutions are less efficient for RV automatic segmentation than for LV, and RV segmentation remains mostly manual, even though improvement in post-processing has recently been reported [17]. Therefore, the Qt method is rarely performed in daily practice, and RV functional assessment is mostly visually performed except in cases of specific indication, such as in patients with CHD, or in the context of research studies. Thus, for daily evaluation of patients with AHD, a quick and accurate method applicable as a first-line screening test would be useful, in order to determine those patients who would deserve exhaustive Qt evaluation. For that purpose, various semi-quantitative (SQt) methods have been described: tricuspid annular plane systolic excursion (TAPSE), RV fractional shortening (RVFS) and RV fractional area change (RVFAC). TAPSE and RVFAC were initially described in echocardiography with conflicting results according to various studies [18–22]. More recently, TAPSE and RVFS were also evaluated with cardiac MRI in a few studies [23, 24] but to date, no cardiac MRI study has evaluated the interest of RVFAC compared with TAPSE and RVFS. Moreover, the reproducibility of these SQt methods and particularly the effect of observers’ experience were not clearly reported.
The aim of this study was to evaluate the diagnostic accuracy and variability of TAPSE, RVFS and RVFAC to assess RV systolic function from cardiac MRI in patients with acquired heart disease.
Materials and methods
This study was performed in accordance with the Standards for the Reporting of Diagnosis accuracy studies (STARD) statement recommendations [25].
Patients
The institutional review board approved the study and all patients gave written informed consent. From June 2008 to August 2008, all patients referred to our centre with a clinical indication of cardiac MRI were invited to participate in the study. Exclusion criteria were as follows: age <18 years; contraindication for MRI; arrhythmias during cardiac MRI examination; CHD; and patients referred for an examination that did not include ventricular function analysis (i.e. MR angiography of pulmonary veins or thoracic aorta). The target sample size (60 patients) was defined from the results of a literature study. Baseline population characteristics are summarised in Table 1. Sixty consecutive patients were included. Mean patients’ age was 53.5 ± 17.5 years and 42 (70%) were male. Clinical indications were represented by a panel of the currently most frequent cardiac MRI indications in patients with AHD.
Cardiac MR protocol
Cardiac MRI examinations were performed at 1.5 T (Symphony Tim®, Siemens Medical Systems, Erlangen, Germany). A dedicated eight-element phased-array cardiac coil was used. A retrospective synchronisation with a balanced steady-state free precession (bSSFP) sequence was performed for cine analysis, with repeated breath-holds of 10–15 s. All conventional planes (2-, 3- and 4-chambers views) were acquired and a total of 8–12 contiguous cine short axis (SA) slices were performed from the base to the apex of the ventricles. Sequence parameters were as follows: TR = 50 ms; TE = 1.7 ms; flip angle = 55°; slice thickness = 7 mm; matrix size = 256 × 216; Field of view = 360–420 mm; 20 images per cardiac cycle. Other sequences (i.e. T2-weighted sequences, first-pass perfusion, phase contrast or late gadolinium enhancement) were performed according to clinical indication, but not considered in the present study.
Cardiac MR analysis
Observers
Three observers with various training-degree in cardiac MRI participated in the image analysis: observer 1 (Obs1) with 3 years’ training, observer 2 (Obs2) with 1 year’s training and observer 3 (Obs3) who had no cardiac MRI experience. Before the study, Obs3 received a 3-h basic cardiac MRI course including anatomy and the principles of cardiac segmentation with 5 examinations selected in our database. Analyses were randomly performed and each measurement was performed blinded to the medical history. All analyses were retrospectively performed after completing inclusion of the 60 patients.
Quantitative analysis
All measurements were performed using commercially available software (Argus, Siemens Medical Solutions). In order to determine the RVEF (standard of reference of the study), the 2 most experienced observers (Obs1 and Obs2) independently assessed the Qt RV parameters (RVEF, end-diastolic and end-systolic RV volumes) from cine SA slices. Both observers manually delineated endocardial and epicardial borders on all SA slices, at end-diastole (ED) and end-systole (ES). Trabeculae and papillary muscles were included in the RV cavity. ED and ES were located on a mid-ventricular SA slice, and visually defined as the image with the largest and the smallest cavity respectively. The reference RVEF was then considered to be the mean value of Obs1 and Obs2 measurements.
Semi-quantitative analysis
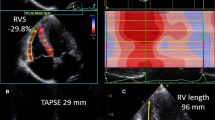
Semi-quantitative RV parameters (TAPSE, RVFS and RVFAC) were determined using a 4-chamber view cine sequence (Fig. 1). TAPSE is the difference between ED and ES RV length. These lengths are measured from the lateral part of the tricuspid annulus to the RV apex. RVFS is the TAPSE indexed to the ED RV length. To determine RVFAC, ED and ES RV areas were measured on a 4-chamber view; RVFAC was obtained by dividing the difference between the ED and ES areas by the ED area. As for Qt measurements, trabeculae and papillary muscles were included in the RV cavity for RVFAC measurement. For all SQt measurements, RV ED and ES were defined respectively as images with the largest and the smallest RV cavity area. To evaluate intra- and inter-observer variability and the effect of previous experience, each SQt analysis was performed twice at least 1 month apart.
Obs1 and Obs2 performed Qt and SQt analyses blinded from each other with at least a 2-week interval.
Statistical analysis
Continuous variables are expressed as mean ± SD and qualitative variables as number and percentage. Considering that the second measurement of SQt parameter was performed to evaluate intra-observer variability, only the first measurement of each observer was taken into account to evaluate inter-observer variability, correlation between SQt and Qt methods, and ROC analyses. Pearson’s correlation coefficient was used to evaluate the relation between the Qt and SQt methods. The Bland-Altman method [26], the coefficient of variation (CV) and the intra-class correlation coefficient (ICC) were used to evaluate the intra- and inter-observer variability. In order to evaluate the diagnostic performance of each SQt method in predicting an RVEF <45%, we performed receiver operating characteristic (ROC) curve analysis and we calculated areas under the curve (AUC) for each observer’s measurements. The statistical significance of the difference between AUC was evaluated using the method of DeLong et al. [27]. p < 0.05 was considered significant. All statistical analyses were performed using MedCalc for Windows, version 11.3.2.0 (MedCalc Software, Mariakerke, Belgium).
Results
Correlation between semi-quantitative and quantitative methods
All SQt measurements correlated significantly with RVEF. RVFAC correlated better with RVEF for all observers and this was not related to cardiac MRI experience (R = 0.741 for Obs1 and Obs2, = 0.716 for Obs3) (Table 2). In comparison, RVFS and TAPSE correlated less well with RVEF and differed among Obs1 (R = 0.720 for RVFS, = 0.646 for TAPSE), Obs2 (R = 0.583 for RVFS, = 0.499 for TAPSE) and Obs3 (R = 0.534 for RVFS, = 0.482 for TAPSE). For the most experienced observer (Obs1) the correlation coefficient of TAPSE (R = 0.646), RVFS (R = 0.720) and RVFAC (R = 0.741) were comparable. On the contrary, a marked difference between the correlation coefficient of TAPSE (R = 0.482), RVFS (R = 0.534) and RVFAC (R = 0.716) was observed for the less experienced Obs3. Quantitative RV function assessment revealed that 10/60 (17%) patients had an RVEF <45%. In this patients’ subgroup, correlation between RVFAC and RVEF was slightly decreased but remained comparable between observers (R = 0.607 for Obs1, = 0.638 for Obs2, = 0.572 for Obs3). On the contrary, an effect of cardiac MRI experience was observed for TAPSE (R = 0.691 for Obs1, = 0.341 for Obs2 and = 0.451 for Obs3) and for RVFS (R = 0.762 for Obs1, = 0.453 for Obs2, = 0.616 for Obs3).
Reproducibility of semi-quantitative parameters
All observers had lower intra-observer variability for RVFAC compared with RVFS and TAPSE (Fig. 2, Table 3). Intra-observer variability of RVFAC was less subject to initial observer experience (CV and ICC ranging respectively from 6.7% and 0.955 for Obs1 to 13.8% and 0.825 for Obs3). Intra-observer variability was more experience-dependent for both RVFS (CV and ICC ranging respectively from 11.3% and 0.906 for Obs1 to 23.8% and 0.760 for Obs3) and TAPSE (CV and ICC ranging respectively from 11.6% and 0.912 for Obs1 to 26.0% and 0.756 for Obs3).
Inter-observer reproducibility (Fig. 3, Table 4) was good for RVFAC (CV and ICC ranging respectively from 7.7 to 10.5% and 0.825 to 0.937) and better than for RVFS (CV and ICC ranging respectively from 19.3 to 25.2% and 0.675 to 0.774) and TAPSE (CV and ICC ranging respectively from 21.0 to 25.3% and 0.709 to 0.784).
ROC analysis
Accuracy related to observer experience
All SQt parameters had a significant diagnostic value in predicting an RVEF <45% (p < 0.0001 in all cases) (Fig. 4, Table 5). However, RVFAC was the most accurate parameter for all observers, without any effect of observer’s experience on accuracy (AUC = 0.956 for Obs1, = 0.930 for Obs2, = 0.944 for Obs3, p = NS). On the contrary, TAPSE and RVFS were experience-dependent and their accuracy was significantly lower for Obs3 (AUC = 0.835 for TAPSE and 0.870 for RVFS) in comparison to Obs 1 (AUC = 0.929 for TAPSE and 0.944 for RVFS) (p < 0.05 in both cases). Also, Obs3 had significantly lower AUC for TAPSE than for RVFAC (p = 0.02), contrary to Obs1 and Obs2. No significant inter-observer difference was found among AUC of TAPSE, RVFS and RVFAC for the 2 most experienced observers, although a systematic trend for best accuracy was found for Obs1.
Optimal thresholds for detecting a RV dysfunction
Optimal thresholds of SQt parameter to predict RVEF <45% for each observer are listed in Table 5. For Obs1, who was both the most reproducible and best correlated with RVEF, an RVFAC <41% was able to predict an RVEF <45% with 90% sensitivity and 94% specificity. Similarly, an RVFS <20% and a TAPSE <16 mm predicted an RVEF <45% with respectively 90%/80% sensitivity and 88%/90% specificity.
Segmentation times
Mean time to completion of the Qt method was 13.4 ± 3.9 min for Obs1 and 18.9 ± 4 min for Obs2, i.e. the mean time of analysis was 16.2 ± 4.8 min. On the contrary, post-processing of SQt parameters took less than 2 min for all observers, with mean time of analysis at 1.3 ± 0.2 min for RVFAC, 0.5 ± 0.2 min for RVFS and 0.4 ± 0.1 min for TAPSE.
Discussion
Correlation of RVFAC, TAPSE and RVFS with RVEF
All SQt parameters correlated significantly with RVEF but we demonstrated that RVFAC performed better than TAPSE and RVFS. Contrary to TTE [18–22], few studies have investigated the accuracy of SQt methods in assessing RV function from cardiac MRI.
Two previous cardiac MRI studies have evaluated the TAPSE: Morcos et al. [24] demonstrated that TAPSE correlated poorly with RVEF (R = 0.50, p < 0.05) in patients with tetralogy of Fallot, whereas Nijveldt et al. [23] found a better correlation (R = 0.62, p < 0.01) in 60 subjects including controls and patients with pulmonary hypertension, acute myocardial infarction and Brugada syndrome. Our results are in line with those published by Nijvedlt et al., probably because we had no patients with CHD in our cohort. Also, we demonstrated that the relation between TAPSE and RVEF depended on the experience of the observer.
We found that RVFS correlated better with RVEF than did the TAPSE. This is in agreement with a previous study [23] and can be explained by the indexation of the RVFS to the RV length. Indeed, TAPSE values are strongly influenced by the length of the RV, itself depending on the subject’s constitutional cardiac anatomy.
To our knowledge, this is the first cardiac MRI study describing the usefulness of RVFAC for RV function assessment in clinical practice. Indeed, Kind et al. [28] recently reported a correlation coefficient of 0.76 between RVFAC and RVEF, but they did not compare this result with other longitudinal and transverse parameters evaluated in their study. Our results confirm previous reports based on TTE [19–22], which demonstrated that RVFAC was more accurate than TAPSE. This better correlation is certainly due to the fact that RVFAC is varying accordingly with both the longitudinal and transverse motion of the RV. On the contrary, TAPSE and RVFS only depend on the longitudinal shortening. In the subgroup of patients with RVEF <45% the correlation between RVFAC and RVEF was slightly decreased. This could be related to the small proportion of patients with a decreased RVEF (n = 10/60, 17%). However, the correlation between RVFAC and RVEF remained comparable between observers, contrary to RVFS and TAPSE, for which correlation was clearly lower in less experienced observers.
Reproducibility of RVFAC, TAPSE and RVFS measurements
Contrary to echocardiographic studies [22], RVFAC was the most reproducible semi-quantitative parameter in this study. This is probably due to the high-quality imaging provided by bSSFP sequences, facilitating the delineation of endocardial borders.
On the other hand, tricuspid annulus and RV apex are not always easy to define on cardiac MRI and subject to a wide range of variability. Importantly, RVFAC was less dependent on the observer’s experience than TAPSE or RVFS, resulting in a significant reduction of variability. These findings could make RVFAC applicable in centres with limited experience in cardiac MRI.
Diagnostic accuracy of RVFAC, TAPSE and RVFS
Our report indicates that, regardless of the experience of the observer, all SQt parameters had diagnostic value regarding RV function. However, RVFAC was both the most accurate and the least experience-dependent method. We demonstrated that a TAPSE <16 mm and an RVFS <20% predicted an RVEF <45% with 80/90% and 90/88% sensitivity/specificity respectively. These cut-off values are in agreement with a previously published study [23]. We also demonstrated that an RVFAC <41% predicted RV dysfunction with 90% sensitivity and 94% specificity. As far as we know there have been no previous cardiac MRI studies that have evaluated the diagnostic accuracy of RVFAC for assessing RV systolic function. Our results are in accordance with previous TTE studies that demonstrated an excellent correlation between TTE measurements of RVFAC and MRI-derived RVEF [19–22].
Segmentation time
Despite automatic post-processing improvements [17], it remains difficult to assess RV function with a Qt 3D volumetric approach in a reasonable amount of time. Indeed, we found that even for an observer with 3 years’ experience RV post-processing took about 13.4 ± 3.9 min. On the contrary, all SQt methods are quick and can be routinely applied. Evaluation of RV function was demonstrated to be a prognostic factor in most ischaemic and non-ischaemic cardiomyopathies [1–9]. Thus, cardiac MRI reports should contain RV function estimation. In our study we demonstrated that RVFAC could be used as a quick screening test to evaluate RV function using a bSSFP four-chamber view.
Limitations
First, this study was monocentric and enrolled a limited number of patients. However, patients included in the study are representative of current routine cardiac MRI indications, with a panel of ischaemic and non-ischaemic AHD. Second, we did not investigate patients with CHD in this study. However, in cases of CHD, the Qt approach remains the standard and should be systematically performed because of the complex RV geometry and function. Third, we used in our study a threshold of 45% to define an abnormal RVEF. Another study has considered a threshold as low as 35% [23]. However, a threshold of 45% is in accordance with the lower range of normal RVEF used in clinical practice [29]. Moreover, in a setting of screening RV dysfunction, a threshold as low as 35% or 40% could depress the test sensitivity and therefore decrease its accuracy. Fourth, MR examinations were performed with our routine protocols and therefore, due to variable field of view and fixed number of images per RR interval, neither the spatial nor temporal resolution were constant. This could have slightly influenced the results of quantitative measurements. Finally, a comprehensive evaluation of the RV function cannot be obtained from a simple RVEF estimate. In many clinical situations such as CHD or suspected ARVD [30], RV volumes have to be precisely determined. MRI is the unquestionable reference examination for RV volume assessment, which cannot be inferred from SQt methods.
Conclusion
Despite its important prognostic value, RV function often remains disregarded in patients referred for cardiac MRI examination. We demonstrated that right ventricular fractional area change was a feasible, fast, accurate and reproducible semi-quantitative method for evaluating RVEF in daily practice, even in non-experienced observers. Thus, the time-consuming quantitative method could be reserved for patients with abnormal right ventricular fractional area change.
References
Davlouros PA, Niwa K, Webb G, Gatzoulis MA (2006) The right ventricle in congenital heart disease. Heart 92(Suppl 1):i27–i38
Gavazzi A, Berzuini C, Campana C et al (1997) Value of right ventricular ejection fraction in predicting short-term prognosis of patients with severe chronic heart failure. J Heart Lung Transplant 16:774–785
Ghio S, Gavazzi A, Campana C et al (2001) Independent and additive prognostic value of right ventricular systolic function and pulmonary artery pressure in patients with chronic heart failure. J Am Coll Cardiol 37:183–188
Mehta SR, Eikelboom JW, Natarajan MK et al (2001) Impact of right ventricular involvement on mortality and morbidity in patients with inferior myocardial infarction. J Am Coll Cardiol 37:37–43
Chin KM, Kim NH, Rubin LJ (2005) The right ventricle in pulmonary hypertension. Coron Artery Dis 16:13–18
Hulot JS, Jouven X, Empana JP, Frank R, Fontaine G (2004) Natural history and risk stratification of arrhythmogenic right ventricular dysplasia/cardiomyopathy. Circulation 110:1879–1884
Haddad F, Denault AY, Couture P et al (2007) Right ventricular myocardial performance index predicts perioperative mortality or circulatory failure in high-risk valvular surgery. J Am Soc Echocardiogr 20:1065–1072
Mendes LA, Dec GW, Picard MH, Palacios IF, Newell J, Davidoff R (1994) Right ventricular dysfunction: an independent predictor of adverse outcome in patients with myocarditis. Am Heart J 128:301–307
Juillière Y, Barbier G, Feldmann L, Grentzinger A, Danchin N, Cherrier F (1997) Additional predictive value of both left and right ventricular ejection fractions on long-term survival in idiopathic dilated cardiomyopathy. Eur Heart J 18:276–280
Lindqvist P, Calcutteea A, Henein M (2008) Echocardiography in the assessment of right heart function. Eur J Echocardiogr 9:225–234
Jain D, Zaret BL (1992) Assessment of right ventricular function. Role of nuclear imaging techniques. Cardiol Clin 10:23–39
Müller M, Teige F, Schnapauff HB, Dewey M (2009) Evaluation of right ventricular function with multidetector computed tomography: comparison with magnetic resonance imaging and analysis of inter- and intraobserver variability. Eur Radiol 19:278–289
Goetschalckx K, Rademakers F, Bogaert J (2010) Right ventricular function by MRI. Curr Opin Cardiol 22:451–455
Grothues F, Moon JC, Bellenger NG, Smith GS, Klein HU, Pennell DJ (2004) Interstudy reproducibility of right ventricular volumes, function, and mass with cardiovascular magnetic resonance. Am Heart J 147:218–223
Beygui F, Furber A, Delépine S et al (2004) Routine breath-hold gradient echo MRI-derived right ventricular mass, volumes and function: accuracy, reproducibility and coherence study. Int J Cardiovasc Imaging 20:509–516
Mooij CF, de Wit CJ, Graham DA, Powell AJ, Geva T (2008) Reproducibility of MRI measurements of right ventricular size and function in patients with normal and dilated ventricles. J Magn Reson Imaging 28:67–73
Grosgeorge D, Petitjean C, Caudron J, Fares J, Dacher JN (2010) Automatic cardiac ventricle segmentation in MR images: a validation study. Int J Comput Assist Radiol Surg. doi:10.1007/s11548-010-0532-6
Kaul S, Tei C, Hopkins JM, Shah PM (1984) Assessment of right ventricular function using two-dimensional echocardiography. Am Heart J 107:526–531
Anavekar NS, Gerson D, Skali H, Kwong RY, Yucel EK, Solomon SD (2007) Two-dimensional assessment of right ventricular function: an echocardiographic-MRI correlative study. Echocardiography 24:452–456
Kjaergaard J, Petersen CL, Kjaer A, Schaadt BK, Oh JK, Hassager C (2006) Evaluation of right ventricular volume and function by 2D and 3D echocardiography compared to MRI. Eur J Echocardiogr 7:430–438
Schenk P, Globits S, Koller J et al (2000) Accuracy of echocardiographic right ventricular parameters in patients with different end-stage lung diseases prior to lung transplantation. J Heart Lung Transplant 19:145–154
Wang J, Prakasa K, Bomma C et al (2007) Comparison of novel echocardiographic parameters of right ventricular function with ejection fraction by cardiac magnetic resonance. J Am Soc Echocardiogr 20:1058–1064
Nijveldt R, Germans T, McCann GP, Beek AM, van Rossum AC (2008) Semi-quantitative assessment of right ventricular function in comparison to a 3D volumetric approach: a cardiovascular magnetic resonance study. Eur Radiol 18:2399–2405
Morcos P, Vick GW 3rd, Sahn DJ, Jerosch-Herold M, Shurman A, Sheehan FH (2009) Correlation of right ventricular ejection fraction and tricuspid annular plane systolic excursion in tetralogy of Fallot by magnetic resonance imaging. Int J Cardiovasc Imaging 25:263–270
Bossuyt PM, Reitsma JB, Bruns DE et al (2003) Towards complete and accurate reporting of studies of diagnosis accuracy: the STARD initiative. Radiology 226:24–28
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44:837–845
Kind T, Mauritz GJ, Marcus JT et al (2010) Right ventricular ejection fraction is better reflected by transverse rather than longitudinal wall motion in pulmonary hypertension. J Cardiovasc Magn Reson 12:35
Haddad F, Hunt SA, Rosenthal DN, Murphy DJ (2008) Right ventricular function in cardiovascular disease, part I: anatomy, physiology, aging, and functional assessment of the right ventricle. Circulation 117:1436–1448
Marcus FI, McKenna WJ, Sherrill D et al (2010) Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: proposed modification of the task force criteria. Eur Heart J 31:806–814
Acknowledgment
The authors are grateful to Alexandre Klimoff and Agnes Malgouyres (Siemens France) who provided us with the Argus segmentation software used in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Caudron, J., Fares, J., Vivier, PH. et al. Diagnostic accuracy and variability of three semi-quantitative methods for assessing right ventricular systolic function from cardiac MRI in patients with acquired heart disease. Eur Radiol 21, 2111–2120 (2011). https://doi.org/10.1007/s00330-011-2152-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-011-2152-0