Abstract
Objective
Umbilical venous catheter (UVC) insertion is frequently performed in critically ill neonates, with catheter position evaluated by an abdominal radiograph. The position of the catheter can be difficult to assess based on supine film alone. We aimed to determine whether ultrasound enables precise evaluation of the catheter tip position.
Methods
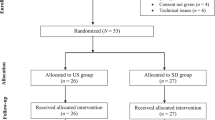
We prospectively evaluated UVC position in 75 neonates by ultrasound and supine abdominal radiograph. Distance from the catheter tip to the diaphragm was measured for both modalities. Anatomical location of the catheter was recorded for both studies. The Student’s t-test was used to compare the means of the differences in catheter position on radiograph and ultrasound.
Results
In 46 patients there was no difference in the distance between the catheter tip and the diaphragm on ultrasound and radiograph. In 29 babies there was a difference of 1-to-7 mm. Ultrasound identified malposition of the catheter in three cases in which the position of the catheter on the plain film was deemed acceptable.
Conclusions
Our study suggests that ultrasound is reliable and may replace plain radiograph for the identification of the UVC position, preventing complications from malposition, and reducing exposure to ionizing radiation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Venous umbilical catheters are widely used in neonatal care, especially in premature or critically ill neonates. In our neonatal intensive care unit, up to 80% of premature babies with birth weight less than 1,500 g receive medicines, fluids, and often parenteral nutrition through such catheters [1]. Double-lumen UV catheters are used, to allow simultaneous administration of the fluids and drugs.
The umbilical vein enters the abdomen and joins the inferior vena cava just below the diaphragm. The optimal position of the catheter tip is at the level of ductus venosus, or in the inferior vena cava distal to the right atrium (RA) [1]. Any more proximal position of the catheter can lead to partial administration of fluids and drugs into the portal venous system [2]. Only an AP view of the abdomen is routinely performed to check the catheter position after insertion. However the last portion of the ductus venosus runs in the sagittal plain, and therefore it is not visualized properly on this view. As a result, catheter malposition can be easily missed [2, 3].
In 1995 Greenberg et al. checked the catheter position with color Doppler echocardiography at the time of insertion, with excellent results [4]. Nevertheless, this technique is not implemented routinely [4], possibly because it needs additional training and requires dedicated pediatric radiologist time.
Catheter malposition can lead to serious complications [2, 5–8]. In recent years, we have had several cases of liver fluid collections secondary to umbilical catheter malposition discovered by ultrasound in babies with altered hepatic functions. Several of these collections required percutaneous drainage due to clinical signs of infection. We therefore decided to evaluate catheter placement on ultrasound, with the goal of avoiding complications due to catheter malposition. In this study we aimed to determine the accuracy of ultrasound in comparison with routinely performed AP radiograph for the assessment of umbilical venous catheter tip position.
Materials and methods
This prospective clinical study was approved by our institutional review board. Parents signed informed consent. Catheter insertion was clinically indicated for fluid and drug administration in these premature or critically ill neonates.
The study began with a form of training. We placed a 300 g piece of bovine liver in water, and inserted the catheter repeatedly through various venous openings. Both radiologists participating in this study evaluated the catheter and tip location using several transducers, with no particular difficulty. As can be seen on Fig. 1, the catheter is clearly visualized and the tip is easily identifiable. Based on this experience, we were prepared to begin ultrasound evaluation of catheter tip position in neonates.
During a one-year period beginning January 1, 2009, we performed 75 ultrasounds in 75 consecutive patients. All patients in whom an umbilical venous catheter was inserted were included in the study. There were 49 boys and 26 girls. Patient age varied from several hours to 3 days, mean 2.5 days; gestational age at birth was 24 to 40 weeks, mean 30 weeks 6 days ±4 weeks 3 days; and patient weight ranged from 450 to 3,600 g, mean 1,580 g. The same double-lumen venous catheter was used in all patients (4Fr-L20cm-1.4 mm, Vycon, France).
Plain films of the abdomen were obtained immediately after catheter insertion, as a part of our routine protocol using AMX 4(+) GE, Milwaukee, WI, USA mobile X-Ray machine. The effective radiation dose for every exposure was 0.005 mSv. Ultrasound studies were performed at a mean interval of 5 h after radiograph (range 15 min to 38 h) by one of two pediatric radiologists (N.S., K.R.) using convex 5–7 MHz and linear 7–12 MHz transducers and an HD11 system (Phillips Medical Systems, Andover, MA). The radiologist performing ultrasound assessment was blinded to radiography findings until the ultrasound examination was completed and findings were recorded.
When the catheter tip was seen on radiograph, its anatomic location and distance from the tip to the diaphragm at the inferior vena cava crossing was measured in mm on the PACS system. The same information was recorded on ultrasound images during the exam (Fig. 2). The exact anatomical position of the catheter tip relative to the inferior vena cava and right atrium was recorded for ultrasonography. Time required for the visualization of the catheter tip on ultrasound was recorded.
a Abdominal radiograph demonstrating the umbilical venous catheter tip (arrow) below the diaphragm in a 1-day-old 1,250 g boy. b Ultrasound image obtained with convex 8–5 MHz transducer in the same patient shows the catheter well, with the tip (arrow) in the hepatic vein. Distance measurements between the catheter tip to the diaphragm are shown in dotted line on both modalities
The Student’s t-test was used to compare the means of the differences in catheter position on radiograph and ultrasound.
Results
The catheter tip was clearly visualized on ultrasound examination in 73 patients (97.3%) and on radiograph in all 75 (100%). The tip was positioned below the diaphragm in 63 patients (84.0%) and above it in 12 (16.0%) (Figs. 2 and 3).
In two patients (2.7%), the catheter tip was not seen on ultrasound. This finding was well-correlated with findings on abdominal radiograph, which demonstrated the tip of the catheter below the level of the liver in these patients.
In 73 babies (97.3%) the catheter tip was at the level of the liver or RA, enabling ultrasound visualization. In two infants (2.7%), the catheter was malpositioned with the tip entering in the liver parenchyma outside the vessels (Fig. 4). One of these neonates, in whom the ultrasound examination was performed with significant delay, 36 h after catheter placement, already had a fluid collection adjacent to the catheter tip (Fig. 5).
a Abdominal radiograph in a 2-day-old, 1,300 g baby boy. The catheter was judged to be satisfactorily positioned. b Ultrasound obtained with a 5–8 MHz transducer reveals the extraluminal position of the catheter (arrow) and hyperechoic collection of total parenteral nutrition fluid (arrowheads) in the liver parenchyma
Among 73 infants in whom the catheter was at the level of the liver or above, the distance from the catheter tip to the diaphragm was the same on both imaging modalities in 46 babies (63.0%). In these patients tip location varied from 30 mm below the diaphragm to 2 mm above. In 27 patients (37.0%) there was minor discrepancy, with radiograph tending to show the catheter tip slightly higher than ultrasound. The difference between the modalities ranged from 1-to-7 mm, with a mean difference for the whole study population of 0.3 ± 2.6 mm (median = 1 mm), however the difference did not reach statistical significance (p = 0.33).
The catheter was visualized on ultrasound within an average of 3 min, and never required more than 5 min of the radiologist’s time.
Discussion
Umbilical venous catheters are used in the neonatal intensive care unit for emergency vascular access and exchange transfusions. Double- and triple-lumen catheters enable simultaneous administration of incompatible solutions such as vasopressor agents, sodium bicarbonate, or calcium. The use of multi-lumen catheters reduces the need for multiple peripheral venous catheters and skin punctures, and is preferred in low-weight infants. If the catheter is used for exchange transfusion only, it could be advanced only as far as is necessary to establish good blood flow (2–5 cm). If the catheter is needed to monitor central venous pressure, it should be advanced through the ductus venosus into the inferior vena cava [1–3]. According to Oestreich, satisfactory position of the catheter is achieved on the first attempt in less than half of placements [2].
Catheter malposition may lead to severe complications, such as bleeding, perforation into the peritoneal cavity or urachus, arrhythmia, cardiac tamponade, thrombosis, pulmonary infarction or abscess, and liver damage, with fluid collections in the liver parenchyma [2, 5, 8]. Paraplegia and even death could be result of placement of the catheter into the left ascending lumbar vein [6, 7].
Umbilical vein catheters should enter the abdomen through umbilical vein, to the left portal vein and ductus venosus, continuing into the right or middle hepatic vein near the entry into the inferior vena cava, just below the diaphragm. The last portion of this complex course runs in the sagittal plane, therefore is not visualized properly on the AP view on standard radiograph; thus several studies have questioned the usefulness of radiograph to evaluate catheter position. Ultrasonography has been suggested as an aid to evaluation catheter placement [4–10].
Several papers describe attempts to evaluation catheter placement with sonography. In 1982, Oppenheimer et al. evaluated fifteen UVC placements by ultrasound, but had problems with visualization of the intrahepatic portion of the catheter [11]. With the high resolution transducers that we use today this segment is seen well.
Other attempts at ultrasound visualization used standard echocardiography views, with catheter position on the echocardiography correlated to vertebral bodies on plain film. Greenberg et al. in 1995 used echocardiography guidance to aid in positioning the catheter tip at the level of the inferior vena cava to the right atrium, with excellent results, demonstrating good correlation between catheter position in relation to the cardiac chambers on echocardiography and the vertebral bodies on the plain film [4]. The authors concluded that 82% of catheters positioned at the level of T7 were in the right atrium, 90% of those positioned at T8-T9 were at the level of the inferior vena cava to the right atrium, and all catheters at T11 and below were in the liver proximal to the ductus venosus. However, Ades et al. in 2003 found poor correlation between catheter position at the level of the inferior vena cava-right atrium on echocardiography with thoracic vertebral bodies on plain films [9].
In the majority of cases today, the catheter tip may be positioned at the level of inferior vena cava or even the ductus arteriosus, and not in right atrium [1], therefore echocardiography is not the ideal tool for evaluation of its position. To the best of our knowledge, no previous study has compared radiographic position of the catheter with position on ultrasound imaging using the diaphragm as a landmark, even though it is clearly identifiable with both modalities. We were able to demonstrate excellent visualization of the catheter on ultrasound at the level of the ductus venosus, at the inferior vena cava distal to the right atrium, in the right atrium, and in the liver parenchyma. There was good correlation between the findings at ultrasound and radiograph, using the diaphragm as a landmark. Insignificant differences that were observed can be explained by angulation of the X-Ray beam, oblique projection of the abdomen, or displacement of the catheter in the time interval between radiograph and US, which was 5 h on average.
The main advantage of ultrasonographic evaluation over the radiograph was early detection of catheter malposition, thus serious complications were avoided.
We have found this protocol to be reliable. Ultrasound assessment of catheter position is now mandatory in our center when a trained radiologist is available. When placement is clearly visualized at ultrasound, the need for radiograph, with the associated exposure to ionizing radiation, is avoided.
One can argue that ultrasound evaluation of catheter placement requires highly qualified personnel and is time consuming. It is true, that pediatric radiologist is not available around the clock in most institutions to help to insert the catheter, but even delayed evaluation of the catheter position can prevent severe complications. In our experience, after a brief training process, the procedure becomes less time-consuming and should not require more than 5 min of a radiologist’s time. Ultrasound thus has the potential to avoid routine use of radiograph for detection of umbilical arterial catheter location in neonate when an appropriately trained personal is available at the end of the catheter insertion procedure. Ultrasound is helpful in all cases when use of the catheter is technically difficult, and when the catheter’s position is questionable on plain film.
A relative limitation of the study was the delay of a few hours between radiograph and ultrasonography in some patients.
Conclusions
In our patients, ultrasonography provided precise detection of umbilical catheter tip positioning in most of the cases, enabling early detection of malposition and associated complications. A larger trial is needed to review the possibility of replacing radiographic evaluation of the UVC placement with ultrasound assessment.
References
Ringer SA, Gray JE (2008) Common neonatal procedures. In: Cloherty JP, Eichenwald EC, Stark AR (eds) Manual of neonatal care. Lippincott Williams & Wilkins-Wolters Kluwer, Philadelphia, pp 649–665
Oestreich AE (2010) Umbilical vein catheterization—appropriate and inappropriate placement. Pediatr Radiol 40:1941–1949
Narla LD, Hom M, Lofland GK, Moskowitz WB (1991) Evaluation of umbilical catheter and tube placement in premature infants. Radiographics 11:849–863
Greenberg M, Movahed H, Peterson B, Bejar R (1995) Placement of umbilical venous catheters with use of bedside real-time ultrasonography. J Pediatr 126:633–635
Berger TM, Stocker M, Caduff J (2006) Neonatal long lines: localisation with conventional radiography using a horizontal beam technique. Arch Dis Child Fetal Neonatal Ed 91:F311
Chen CC, Tsao PN, Yau KI (2001) Paraplegia: complication of percutaneous central venous line malposition. Pediatr Neurol 24:65–68
Groves AM, Kuschel CA, Battin MR (2005) Neonatal long lines: localisation with colour Doppler ultrasonography. Arch Dis Child Fetal Neonatal Ed 90:F5
Madar RJ, Deshpande SA (1996) Reappraisal of ultrasound imaging of neonatal intravascular catheters. Arch Dis Child Fetal Neonatal Ed 75:F62–64
Ades A, Sable C, Cummings S, Cross R, Markle B, Martin G (2003) Echocardiographic evaluation of umbilical venous catheter placement. J Perinatol 23:24–28
George L, Waldman JD, Cohen ML, Segall ML, Kirkpatrick SE, Turner SW, Pappelbaum SJ (1982) Umbilical vascular catheters: localization by two-dimensional echocardio/aortography. Pediatr Cardiol 2:237–243
Oppenheimer DA, Carroll BA, Garth KE, Parker BR (1982) Sonographic localization of neonatal umbilical catheters. AJR Am J Roentgenol 138:1025–1032
Author information
Authors and Affiliations
Corresponding author
Additional information
N. Simanovsky and N. Ofek-Shlomai contributed equally to this paper.
Rights and permissions
About this article
Cite this article
Simanovsky, N., Ofek-Shlomai, N., Rozovsky, K. et al. Umbilical venous catheter position: evaluation by ultrasound. Eur Radiol 21, 1882–1886 (2011). https://doi.org/10.1007/s00330-011-2129-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-011-2129-z