Abstract
Objective
To investigate whether ultrasound-guided umbilical venous catheter (UVC) insertion (US group) reduced the rate of malpositioning of the catheter tip compared to the standard method of insertion (SD group).
Methods
In this open-label, randomized, controlled trial, neonates admitted to NICU within the first week of life were randomly assigned to the US group (n = 26) or SD group (n = 27). Neonates with major congenital anomalies of the thorax and abdomen were excluded. The primary outcome was the rate of malpositioning of the catheter tip.
Results
The rate of malpositioning of the catheter tip was observed in a significantly lower number of neonates in the US group as compared to the SD group (11/26, 42.3% vs. 20/27, 74%; RR = 0.57, 95% CI: 0.34 to 0.94, p = 0.019). As more of the UVCs were positioned optimally in the first attempt in the US group than SD group, the need for repeated attempts at catheter repositioning was reduced, resulting in reduced procedure time (minutes) [mean (SD), 23.96 (6.42) vs. 30 (1.83); mean difference 6.04 (95% CI: 3.46 to 8.62), p = 0.005]. This also led to a reduction in the additional X-ray exposure in the US group (n = 11) compared to the SD group (n = 20) [95% CI: 3.12 to 44.26; p = 0.020].
Conclusion
Ultrasound-guided UVC insertion significantly reduced the rate of catheter tip malposition. It also reduced the number of attempts at catheter manipulation, procedure time, and X-ray exposures. With adequate training, it could be incorporated into routine bedside practice during UVC insertion for optimum placement.
Trial Registration
Clinical Trial Registry of India (www.ctri.nic.in) CTRI/2021/03/031894.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The insertion of central umbilical venous catheters (UVCs) for intravenous therapy in the care of premature and critical infants is the standard of care in the neonatal intensive care unit (NICU). The catheter tip position is routinely assessed by anteroposterior (AP) thoracoabdominal radiography, although views like cross-table lateral abdominal X-ray can also be used. Obtaining two X-ray views can be reserved for situations where a decision regarding catheter position cannot be made with a single view [1]. In recent years, ultrasonography is being increasingly used for the determination of catheter tip position, especially in the developed countries as this provides real-time assessment of the tip position and has several advantages over radiography [2, 3].
Many studies have evaluated the role of ultrasonography in the localization of the tip of the central catheter (UAC/UVC and PICC) in neonates [2,3,4]. Ultrasonography was shown to have better sensitivity and specificity, greater positive predictive value as well as negative predictive value in identifying the tip of central catheters when compared with radiography. Ultrasonography allows healthcare personnel to immediately manipulate the line at the time of insertion to an appropriate tip position if it is found to be misplaced. The ability for instant assessment of tip position of central lines minimizes the chances of catheter malposition, which can lead to complications like pericardial effusion, cardiac tamponade, thrombosis, cardiac arrhythmias, pleural effusion, endocarditis, liver hematoma, liver injury, and portal hypertension [4,5,6,7].
Given the advantage of ultrasonography in UVC tip localization, this study was conducted to evaluate whether UVC insertion under ultrasound guidance reduces the rate of catheter tip malposition in comparison to standard insertion in neonates admitted to NICU.
Materials and Methods
This open-labelled, randomized, controlled trial was carried out in a level-3 neonatal unit in a teaching hospital in Western India from March to August 2021.
All neonates admitted to NICU requiring umbilical venous catheter insertion within the first week of life were eligible for participation in the study. Infants with major congenital anomalies of the thorax and abdomen were excluded.
The study commenced after approval of Institutional Ethics Committee (IEC/104/20) and CTRI registration. Informed written consent was obtained from one of the parents before enrollment of neonates .
Eligible neonates were randomized to an ultrasound-guided UVC placement group or a standard UVC placement group. Block randomization was used, with a variable block size of 2 to 8 using computer-generated random numbers for random sequence generation. Allocation concealment was done using serially numbered, opaque, and sealed envelopes. The envelope was opened by the neonatal fellow on duty after obtaining informed consent. Blinding of the clinicians was not possible due to the nature of the intervention. However, the consultant interpreting the radiographs was blinded to group allocation.
UVC, when indicated, was inserted with aseptic precautions using a PVC umbilical catheter (Vygon™) of size 5 Fr in neonates weighing ≥ 1500 g and 3.5 Fr in neonates weighing < 1500 g. After the procedure, radiography was done with a portable in-house digital X-ray machine and was digitally transferred to the consultant who was unaware of the group allocation, for interpretation of the catheter tip position.
Ultrasound-guided UVC placement (US group):
Ultrasonography (USG) was done with a portable ultrasound machine (Sonosite Edge™) with a sector probe (4–8 Hz) simultaneously with umbilical venous catheter insertion. Ultrasound examination of all neonates was done by a single investigator trained in point-of-care ultrasonography for neonates and the insertion of the catheter was done by a trained neonatal fellow. Sterility of the probe was maintained by cleaning with a 70% isopropyl alcohol swab and covering the probe with a sterile finger glove. While the catheter was being inserted, the ultrasound probe was placed longitudinally in the subcostal area and the catheter tip was inserted till it was visualized at the IVC-RA junction by ultrasound. Tip position was further confirmed in short axis parasternal and apical views and checked for optimal insertion.
During insertion, if the catheter aberrantly coursed towards the portal vein, it was pulled back a few centimeters and reinserted. During reinsertion, gentle pressure was applied with the ultrasound probe in the epigastrium over the liver area as described by Kishigami et al. to compress the hepatic portal venous sinuses, till the catheter tip reached the right position [8]. After catheter insertion, radiography was ordered to confirm the tip location. The radiograph also helped to identify those situations where the UVC continued to be visualized in the portal vein or other aberrant location or was not visualized at all on ultrasonography.
Standard UVC placement (SD group):
In this group, the catheter insertion length (in cm) was calculated according to the formula by Shukla and Ferrara [(3 × Birth weight + 9) / 2] + 1 [9]. The catheter insertion was done by a trained neonatal fellow and the tip position was checked immediately on the X-ray film.
A catheter tip position on AP view X-ray between the T8 and T10 vertebra was defined as optimal [7, 10,11,12]. Catheters were considered malpositioned if the tip was coiled or curved (within the portal vein, splenic vein, or elsewhere), too high (above T8), or too low (below T10). In both groups, on the radiograph, if the catheter tip was visualized to be placed in the liver or splenic vein, it was removed and a PICC was inserted. If the catheter tip was found to be high or low, necessary repositioning was done and confirmed with repeat radiography. If the position was still lower than optimal, then the catheter was used for administering intravenous fluids only and removed within 1 wk. Fixation of the UVC was done only after final confirmation of the line position on radiography in both groups. As a part of the study, the maximum number of radiographs per neonate was restricted to two.
The primary outcome was the rate of catheter tip malposition in the two groups which was based on the first radiograph after UVC insertion.
The secondary outcomes included the following:
-
1.
The number of neonates requiring an additional radiograph for position confirmation.
-
2.
Time taken for catheter insertion: The time from actual catheter placement till the catheter fixation. UVC was fixed in both groups after necessary repositioning, and the catheter tip confirmed to be in optimal position with a repeat radiography.
-
3.
The proportion of neonates with the successful placement of UVC using the technique described by Kishigami et al. in the ultrasound-guided placement group [8].
Depending on a survey done in the authors’ unit in the 3 mo preceding the study, the rate of UVC malposition was found to be 75%. With an assumption to achieve a relative reduction of 50% (an absolute reduction of approximately 40%) in catheter malposition rate when put under ultrasound guidance, a two-sided alpha error of 0.05 and power of 80%, the sample size was estimated as 26 infants in each group.
The statistical analysis was performed using Stata 12.0 (Stata Corp, College Station, Texas, US). Analysis was performed with the intention to treat. The continuous data were represented as mean (SD) for normally distributed data and median (IQR) if data was skewed. Continuous data were analyzed by Student t-test/ Wilcoxon rank-sum test as applicable. Categorical data were represented as percentages and were analyzed using the Chi-square test or Fisher exact test. A p value of < 0.05 was taken as significant.
Results
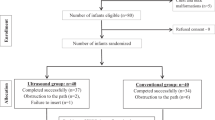
Sixty-eight neonates were assessed for eligibility during the study period from March 2021 to August 2021 (Fig. 1). Of these, 5 were excluded as they had major congenital anomalies. The parents of 4 neonates refused consent. Other reasons for the exclusion of 6 neonates were technical problems like the X-ray machine not working or the ultrasound machine not being available. A total of 53 neonates were enrolled in the study with 26 neonates allocated to the US group and 27 in the SD group. There were no protocol deviations. Baseline demographic variables and postnatal morbidities were comparable between the two groups (Table 1). All 53 neonates were analyzed for the primary outcome.
Ultrasound-guided UVC placement reduced the rate of malpositioning of the catheter tip by 43% (RR: 0.57, 95% CI: 0.34–0.94; p = 0.019) (Table 2), as compared to standard UVC insertion. Catheter tip was high in 2 (8%) in the US group vs. 5 (18.5%) in the SD group (RR: 0.41, 95% CI: 0.09–1.95: p = 0.244). Catheter tip was low in 5 infants in each group (RR: 1.03, 95% CI: 0.34–3.17; p = 0.947). Only 4 (15%) babies in the US group required removal of the catheter due to impaction in the liver as against 10 (37%) in SD group (RR: 0.41, 95% CI: 0.15–1.16, p = 0.074).
Among the secondary outcomes, 11 neonates in the US group and 20 neonates in the SD group needed additional radiographs (95% CI: 3.12–44.26; p = 0.020]. The malposition rate was significantly lesser in the US group in the subgroup of very-low-birth-weight neonates [6 (50%) vs. 11 (91%); p = 0.033]. The mean time (SD) required for UVC insertion was 23.96 ± 6.42 min in the US group vs. 30 ± 1.83 min in the SD group [mean difference 6.04 (95% CI: 3.46–8.62), p = 0.005].
In the US group, the technique of aligning the umbilical vein and ductus venosus as described by Kishigami et al. [8] was done in 15 neonates, and it was found to be successful in 8 neonates (53.3%).
Discussion
There have been multiple studies comparing formulae for calculating the umbilical catheter insertion length using birth weight and/or shoulder–umbilicus length, but none of the formulae or methods have proved to be accurate in estimating the length of umbilical catheter insertion [13,14,15]. Even when the best formula is used, almost half of the UVCs inserted may be malpositioned and need manipulation [13]. Ultrasound-guided insertion has the benefit of achieving optimum catheter tip position and allowing correction of malpositioned catheter tips in real-time in the same session.
In this open-labelled, randomized, controlled trial, there was a significant reduction in the rate of malpositioning of the catheter tip when UVC was inserted under ultrasound guidance compared to the standard method of insertion. The malposition rate in the present study was 42.3% in the US group and 74% in the SD group. Amongst the very-low-birth-weight neonates, where 3.5 Fr catheters were inserted, similar results were seen with a 45% reduction in malpositioning of the catheter tip in the US group. Gohil et al. found the overall malposition rate of UVCs to be over 60% with standard insertion practices [12] whereas Mutlu et al. reported it to be 19% in a study cohort of 974 neonates [7].
Fleming and Kim [16], in their study on ultrasound-guided umbilical catheter insertion, decreased the time of line placement by 46% (p < 0.001), while in the present study, it was reduced by 20% (p = 0.005). The number of radiographs taken was reduced by half in the US group which was statistically significant (p = 0.020). Fewer catheter tip malpositions also resulted in reduced manipulation-related risks and, radiation exposure. Safe tip placement of UVC is critical in minimizing catheter-related complications. No immediate catheter-related complications were noted in the present study.
One important reason behind the high rates of UVC malposition is the inherent nature of the ductus venosus (DV) path, its narrow origin, and the lack of linear alignment of the umbilical vein (UV) with the DV [1]. Despite being able to visualize the catheter in real-time on ultrasonography, all attempts to cross DV and reach the IVC-RA junction failed in 36% of cases (4 out of 11), as the catheter would either enter into the portal vein or coil inside the liver. Kishigami et al. described a technique of aligning the UV and DV by compressing the upper abdomen near the portal sinus of the liver. It decreased the rate of portal placement of the UVC from 43% to 7% [8]. In the present study, the added use of the Kishigami technique resulted in the successful repositioning of the catheter tip in 53% of babies in the US group. The real-time utilization of the Kishigami technique for preventing malpositioning of the catheter tip is an additional benefit of the ultrasound-guided UVC placement.
Similar to the present study, Barone et al. [17] have advocated a structured protocol for ultrasound-based tip navigation and tip location during placement of central venous access devices (including UVC) in neonates called Neo-ECHOTIP. However formal training, which is simple and feasible is required for placing the ultrasound-guided UVCs.
Rubortone et al. [5] in their study concluded that training of medical staff for real-time ultrasonography is feasible, which led to increase in implementation of ultrasound. Thus more number of UVCs were placed in correct position and it ultimately reduced the need of repeat X-rays. In the present study, there was 45% reduction in additional X-ray exposures in the US group.
For determining the position of the catheter tip, ultrasonography has greater sensitivity (93.3%) and specificity (95.6%) compared to radiography (66.7% and 63.0%, respectively, p < 0.001) [18]. However, there can be a situation when the catheter is not visualized at all on ultrasonography. In such situations, the role of the radiography in confirming catheter tip position remains important.
The strength of the present study is its applicability in a busy NICU. Once adequately trained in point-of-care ultrasound, the Neonatology team can place the line, and confirm the position real-time while insertion. The authors had the advantage of availability of a portable in-house digital X-ray machine and console, thereby reducing the total time for the procedure. Use of the Kishigami technique reduced rates of malpositioning of the catheter tip.
However, there were a few limitations. The role of other variables like the size of the umbilical catheter and the day of insertion of the catheter affecting the primary outcome were not evaluated. Also, long-term catheter-related complications during the hospital stay were not evaluated.
Conclusion
The use of ultrasonography in guiding UVC placement reduces rates of malpositioning of the catheter tip compared to standard insertion. It also reduces the time taken for insertion, number of manipulations, and radiation exposure. With adequate training, it could be incorporated into routine bedside practice during UVC insertion for optimum placement.
References
Doreswamy SM, Thomas S, Dutta S. Intra-and inter-rater agreement between x-ray views for umbilical catheter position. Am J Perinatol. 2021;38:609–13.
Zaghloul N, Watkins L, Choi-Rosen J, Perveen S, Kurepa D. The superiority of point of care ultrasound in localizing central venous line tip position over time. Eur J Pediatr. 2019;178:173–9.
Seigel A, Evans N, Lutz T. Use of clinician-performed ultrasound in the assessment of safe umbilical venous catheter tip placement. J Paediatr Child Health. 2020;56:439–43.
Sharma D, Farahbakhsh N, Tabatabaii SA. Role of ultrasound for central catheter tip localization in neonates: a review of the current evidence. J Matern Fetal Neonatal Med. 2019;32:2429–37.
Rubortone SA, Costa S, Perri A, D' Andrea V, Vento G, Barone G. Real-time ultrasound for tip location of umbilical venous catheter in neonates: a pre/post intervention study. Ital J Pediatr. 2021;47:68.
Hermansen MC, Hermansen MG. Intravascular catheter complications in the neonatal intensive care unit. Clin Perinatol. 2005;32:141–56.
Mutlu M, Aslan Y, Kul S, Yılmaz G. Umbilical venous catheter complications in newborns: a 6-year single-center experience. J Matern Fetal Neonatal Med. 2016;29:2817–22.
Kishigami M, Shimokaze T, Enomoto M, Shibasaki J, Toyoshima K. Ultrasound-guided umbilical venous catheter insertion with alignment of the umbilical vein and ductus venosus. J Ultrasound Med. 2020;39:379–83.
Shukla H, Ferrara A. Rapid estimation of insertional length of umbilical catheters in newborns. Am J Dis Child. 1986;140:786–8.
Verheij GH, Te Pas AB, Witlox RS, Smits-Wintjens VE, Walther FJ, Lopriore E. Poor Accuracy of methods currently used to determine umbilical catheter insertion length. Int J Pediatr. 2010;2010:873167.
Greenberg M, Movahed H, Peterson B, Bejar R. Placement of umbilical venous catheters with use of bedside real-time ultrasonography. J Pediatr. 1995;126:633–5.
Gohil B, Balasubramanian H, Kabra NS, Ahmed J, Dash S, Raval G. Malposition rate with varying umbilical vein catheter sizes in vlbw neonates: a randomized controlled trial. Perinatology. 2020;21:7–14.
Lean WL, Dawson JA, Davis PG, Theda C, Thio M. Accuracy of five formulae to determine the insertion length of umbilical venous catheters. Arch Dis Child Fetal Neonatal Ed. 2019;104:F165–9.
Goodarzi R, Tariverdi M, Khamesan B, Barchinejad M, Zare SH, Houshmandi MM. Dunn and Shukla Methods for Predicting Length of Umbilical Catheter in Newborns. Asian J Med Pharm Res. 2014;4:85–133.
Kieran EA, Laffan EE, O’Donnell CP. Estimating umbilical catheter insertion depth in 18 newborns using weight or body measurement: a randomised trial. Arch Dis Child Fetal 19 Neonatal Ed. 2016;101:F10–5.
Fleming SE, Kim JH. Ultrasound-guided umbilical catheter insertion in neonates. J Perinatol. 2011;31:344–9.
Barone G, Pittiruti M, Biasucci DG, et al. Neo-ECHOTIP: a structured protocol for ultrasound-based tip navigation and tip location during placement of central venous access devices in neonates. J Vasc Access. 2021. https://doi.org/10.1177/11297298211007703.
Michel F, Brevaut-Malaty V, Pasquali R, et al. Comparison of ultrasound and x-ray in determining the position of umbilical venous catheters. Resuscitation. 2012;83:705–9.
Acknowledgements
The authors are grateful to the Dean, LTMMC & GH for allowing them to conduct the study. They also thank the staff for their cooperation.
Funding
None.
Author information
Authors and Affiliations
Contributions
AK and SM developed the study protocol, implemented the study and collected data; SP helped in interpretation of outcome measurement; PK and TK helped in protocol development, supervised implementation, and contributed to writing the manuscript; JM supervised implementation and critical review of the manuscript. All authors have reviewed the manuscript and approved the submitted version. SM will act as the guarantor for this paper.
Corresponding author
Ethics declarations
Conflict of Interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kaur, A., Manerkar, S., Patra, S. et al. Ultrasound-Guided Umbilical Venous Catheter Insertion to Reduce Rate of Catheter Tip Malposition in Neonates: A Randomized, Controlled Trial. Indian J Pediatr 89, 1093–1098 (2022). https://doi.org/10.1007/s12098-022-04295-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-022-04295-w