Abstract
The purpose was to describe the MRI morphological features and signal intensity (SI) characteristics of 24 histologically proven cases of musculoskeletal soft tissue lymphoma presenting clinically as a suspected primary soft tissue sarcoma. This was a retrospective review of clinical notes and MRI studies of 24 patients with a histologically confirmed diagnosis of lymphoma. All patients presented to a specialist orthopaedic oncology unit with a suspected primary soft tissue sarcoma. Features assessed included lesion size and morphology, location, extension across anatomical compartments and signal intensity characteristics. The lesions were predominantly poorly defined with peritumoral oedema in ten cases. All tumours were of intermediate T1W SI, while 85% of lesions also showed intermediate T2W SI. Almost all cases that were located just deep to the fascia showed subcutaneous extension, while 50% had involvement of more than one muscle compartment. In 29% of cases, there was extension of tumour along the neurovascular bundle. Histo-pathologically, 23 lesions were non-Hodgkin’s B-cell lymphoma. The MRI features of primary musculoskeletal soft tissue lymphoma include a mass with intermediate SI on T1W and T2W images, involvement of more than one anatomical compartment, subcutaneous extension and extension along the neurovascular bundle.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Lymphoma can arise in lympho-reticular tissue anywhere in the body, and haematogenous spread from nodal disease leads to extra-nodal involvement and disseminated disease. Extra-nodal involvement of lymphoma in the lung, gastrointestinal tract, central nervous system, salivary glands, gonads and thyroid is well recognised and occurs in approximately 20% of cases [1], but clinically detectable involvement of skeletal muscle is distinctly uncommon. One study found only 8 patients with soft tissue lymphoma in 7,000 cases of lymphoma [2], and another indicated that primary lymphomatous involvement of skeletal muscle is seen in only 0.3% of Hodgkin’s lymphoma and 1.5% of non-Hodgkin’s lymphoma [3]. Sarcoma is the most commonly suspected diagnosis in patients presenting with non-fatty intramuscular masses. However, it is important to make the correct diagnosis, as isolated intramuscular lymphoma has the same favourable prognosis as other stage I non–Hodgkin’s lymphomas [4].
This study reviews the magnetic resonance imaging (MRI) features of 24 cases of pathologically proven musculoskeletal soft tissue lymphoma presenting to an orthopaedic oncology unit as a suspected primary soft tissue sarcoma.
Materials and methods
The case records and MRI features of 24 patients with pathologically proven lymphoma presenting as a suspected primary soft tissue sarcoma between June 2000-June 2006 were retrospectively reviewed. Due to the tertiary referral status of the unit, patients usually presented following MRI at the referring hospital, resulting in a wide variety of imaging protocols. However, all studies were performed on high field magnets. MRI sequences included T1-weighted spin echo (W SE) images (n=23), T2-weighted fast spin echo (W FSE) images (n=14), fat-suppressed T2W FSE images (n=8) and short tau inversion recovery (STIR) sequences (n=16) in a variety of planes. Thirteen patients had T1W SE images repeated following administration of intravenous contrast medium.
All the images were reviewed by the senior authors, who are the lead radiologists at the tertiary referral unit for soft tissue and bone tumours. Information obtained included the site of lesion, lesion morphology and size, patterns of local extension, surrounding reactive soft tissue oedema and lesion signal intensity (SI) characteristics. Regarding the latter, the predominant SI of the lesion was compared to skeletal muscle for T1W SE images and to skeletal muscle and subcutaneous fat for T2W FSE, FS T2W FSE and STIR images.
All patients underwent image-guided percutaneous needle biopsy. The histology was reviewed in all patients, and the diagnosis and sub-type of the lymphoma were confirmed.
Results
Clinical findings
The study group consisted of 24 patients (14 male and 10 female), with a mean age of 39.6 years (range 35–91 years). In two cases, there was a history of previous non-Hodgkin’s lymphoma, which was in remission. In the remaining patients, there was no significant previous medical history. The most common sites of involvement were the calf, thigh and arm (Table 1).
MRI findings
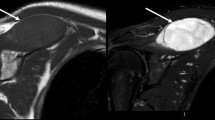
Regarding lesion morphology, 8 masses were lobular and well-defined, while 16 cases showed poorly defined margins (Fig. 1a–c). The mean cranio-caudal lesion length was 12.7 cm; the mean antero-posterior and transverse diameters were 6 cm and 5.95 cm, respectively. The largest lesion measured 40×7×8 cm. There was peritumoral oedema in 11 cases (Fig. 1a,b).
Lesion morphology. A 54-year-old female with calf lymphoma. Axial T2W FSE image (a) of the calf showing a well-defined, lobular intermediate SI mass (arrows) located deep to the fascia within both the anterior and lateral compartments. A 73-year-old female with calf lymphoma. Coronal fat-suppressed T2W FSE (b) and axial T2W FSE (c) images showing a poorly defined intermediate SI mass (arrows) located within the anterior, lateral and deep and intermediate posterior compartments of the calf with extension through the fascia (arrowheads). Note also extensive perifascial oedema
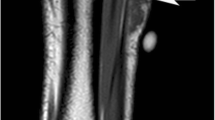
The T1W SE SI was iso-(n=8) (Fig. 2a) or hyperintense (n=15) (Fig. 2b) to skeletal muscle (T1W SE images were not available for review in one case). The SI on T2W FSE images was intermediate between fat and skeletal muscle in 14 cases (Fig. 1a,c), being homogenous in 10 of these (Fig. 2c). On fat-suppressed T2W FSE images, one lesion was isointense to fat, one lesion was isointense to muscle, three lesions had intermediate SI between fat and muscle, and three lesions were hyperintense to fat. In all available cases, STIR images showed hyperintense SI (n=16) (Fig. 2d), while available post-contrast T1W SE images showed heterogeneous enhancement in nine cases (Fig. 2e,f).
Lesion SI characteristics. A 73-year-old female with calf lymphoma. Axial T1W SE image (a) showing a poorly defined mass (arrows) that is isointense to skeletal muscle. A 37-year-old male with arm lymphoma. Coronal T1W SE image (b) showing a superficial mass in the posterolateral aspect of the mid-arm (arrows) that is mildly hyperintense compared to skeletal muscle. A 66-year-old male with distal thigh lymphoma. Axial T2W FSE image (c) showing a homogeneously intermediate SI mass (arrows) in the popliteal fossa. Same case as (b). Coronal STIR image (d) through the arm showing a heterogeneous hyperintense mass (arrows). Axial post-contrast T1W SE image (e) through the arm showing a lesion with mainly uniform enhancement (arrows) and a small area of necrosis (arrowhead). A 36-year-old male with calf lymphoma. Axial post-contrast T1W SE image (f) showing a lesion with predominant necrosis and peripheral enhancement (arrows)
Involvement of more than one muscle compartment was present in 12 cases (50%). All five calf lesions involved more than one compartment (Figs. 1, 2a,f), and there was extension of contiguous tumour to four compartments in two cases. Multi-compartment involvement by tumour was seen in one case in the thigh, one case in the para-scapular region and three cases in the arm; the anatomical distribution of disease is shown in Table 2.
Thickening of the skin and subcutaneous fat was seen in 11 cases (Figs. 1b,c and 3) and was presumed to represent lymphomatous infiltration, since no histological proof from biopsy was available to confirm this. Tumors located superficially within the muscle showed direct extension through deep fascia into the subcutaneous fat (n=9), and there was infiltration of the adjacent skin in two cases. In three other cases, subcutaneous oedema only was seen. T2W FSE images were the most useful in distinguishing infiltration from oedema, as the intermediate SI mass is clearly identified breaching the fascia and infiltrating the high SI subcutaneous fat (Fig. 1c). Infiltrated skin showed marked thickening and distortion (Fig. 3).
In seven cases, there was extension of the tumour along the neurovascular bundle with complete encasement of the vessels in six cases and partial encasement in one (Fig. 4a,b). The lesion extended proximally in five of the cases and distally in two. In two cases, tumours presented as discontinuous masses that were widely separated (Fig. 5). There was extension into the adjacent bone in four cases in the form of contiguous marrow SI abnormality (Fig. 6)
Vascular involvement. A 73-year-old female with calf lymphoma and extension into the popliteal fossa. Axial T2W FSE image (a) showing an intermediate SI mass (arrows) partially encasing the popliteal vessels. A 58-year-old male with lymphoma of the axilla. Sagittal post-contrast T1W SE image (b) showing a mass (arrows) completely encasing the axillary artery and vein (arrowheads)
Non-contiguous disease. Same case as Fig. 1b,c. Coronal STIR image showing a lobular hyper-intense mass in the popliteal fossa (arrows) with proximal spread along the neurovascular bundle (arrowhead)
Pathology
Needle biopsy showed 91.6% (n=22) of the cases to be B-cell lymphoma; one was mixed B/T-cell lymphoma, and one was a T-cell lymphoma. Further analysis of the B-cell lymphomas revealed 12 large cell diffuse, 4 follicular and 1 lymphocytic lymphoma. Five of the cases were not further characterised.
Discussion
Various studies in the literature have shown that muscle lymphoma is very rare. Only 472 extremity soft tissue lymphomas (0.01%) were documented in a review of 39,179 soft tissue tumours over a 10-year period [5]. Involvement of muscle by lymphoma can occur in one of the three ways: as part of disseminated disease, as extension from adjacent bone or lymph nodes or very rarely as primary extra-nodal disease. It has been suggested that primary lymphoma of muscle may arise within aberrant lymph nodes, although these lymph nodes are not histologically recognizable at the time of diagnosis [2]. In a large retrospective study from the Mayo Clinic, Travis et al. [2] reported primary muscle lymphoma in only 8 of 7,000 cases of malignant lymphoma. Many studies have found that the thigh and upper arm are the commonest sites affected by soft tissue lymphoma [2, 6–9]. The present study was consistent with this, but also found an equal number of cases occurring in the calf (Table 1).
The role of imaging in muscle lymphoma has been discussed in various reports. The CT features are often non-specific, as the mass may be homogenous and of low attenuation [10] or of similar attenuation to muscle [11]. Following intravenous contrast medium, the masses may have similar attenuation to the adjacent skeletal muscle [11] or show avid homogenous contrast enhancement [8]. Hence, CT is not considered very useful for evaluating soft tissue lymphoma.
There are various small series and case reports describing the MRI findings in muscle lymphoma. Eustace et al. [12] reported three cases of biopsy-proven muscle lymphoma. All the cases showed muscle enlargement, isointensity on T1W and hyperintensity on T2W with homogenous enhancement. Hosono et al. [13] described the MRI and CT features in four pathologically proven cases of muscle lymphoma. The MRI findings consisted of enlargement of muscle with preservation of fat planes, extension along the muscle fascicles, hyper- or isointensity on T1W and increased SI on T2W with homogenous enhancement. Beggs (n=5) [14] and Lee (n=5) [15] described similar MRI signal characteristics to the above studies, but also infiltration of the adjacent subcutaneous fat and involvement of multiple muscle compartments.
On T2W FSE images, soft tissue lymphoma masses showed predominantly intermediate SI between that of fat and muscle. A homogeneous, intermediate SI soft tissue mass on T2W FSE images was the commonest pattern. T2W FSE images are now routinely used in musculoskeletal imaging, and these result in higher SI from fat than conventional T2W SE images, which may explain some of the apparent differences in SI characteristics between the present and previous studies [13–15]. On T1W SE images, all masses were homogeneously iso- or hyperintense to muscle, with the majority being mildly hyperintense (15/23), even in the absence of haemorrhage. These findings show some correlation with previous studies: Beggs [14] and Hosono [13] noted T1 hyperintensity in three of five and two of four cases, respectively, but isointensity was the norm in cases reported by Lee [15] and Eustace [12] (five of seven and three of three cases, respectively). In the cases that received intravenous contrast medium, there was usually heterogeneous enhancement. Both diffuse homogeneous [13–15] and heterogeneous [14] enhancements have previously been reported, and we conclude that post-contrast studies are not specific in characterising a lymphomatous mass.
A striking feature in our study was extension of tumour into the subcutaneous tissues overlying the involved muscle, with occasional skin thickening. No biopsies of these superficial tissues were performed as muscle was targeted in each case, but MRI suggested lobular tumour extending to subcutaneous fat in continuity with a superficial muscle lesion (n=11) and extending to the overlying skin, which showed thickening (n=2). Isolated oedema in subcutaneous fat was seen in a further three cases. This can occur adjacent to other non-neoplastic muscle pathologies, for example, pyomyositis (pyogenic and tuberculous) and inflammatory myopathies [16–18] and was reported in myositis as early as 1991 by Fleckenstein et al. [19], but in our experience it is uncommon in sarcoma. Involvement of subcutaneous tissues by muscle lymphoma has previously been noted by Beggs (five of five) [14] and Lee (four of seven) [15].
Another important feature that may suggest lymphoma is involvement of more than one muscle compartment. In our study this was identified in 50 percent of cases, and MRI in these patients clearly showed the extent and groups of muscles involved. Eustace [12] and Hosono [13] also reported involvement of more than two muscle groups, but these studies did not emphasise multi-compartment involvement. Lee [15] and Beggs [14] have described this feature, and we agree that it may indicate lymphoma as the most likely diagnosis, as it would be a highly unusual pattern of disease extension with soft tissue sarcoma.
The present study has also noted extension of the tumour along the neurovascular bundle, which was seen in 7/24 cases and may represent infiltration along the lymphatics. However, this finding has not been discussed in any of the previous studies. This pattern of spread is highly unusual in sarcoma, with the exception of the rare epithelioid sarcoma in which extension along the neurovascular bundle is an uncommon but recognised occurrence, especially in tumours that have an infiltrative growth pattern [20]. Muscle lymphoma, therefore, behaves as an infiltrative lesion rather than a compartmental condition such as sarcoma.
There are a number of reasons why it is important to consider the possibility of lymphoma as the cause of a soft tissue mass arising in muscle. Histopathological analysis of the biopsy specimen may be influenced by the imaging diagnosis. If lymphoma is suspected, appropriate immunohistochemical characterization of tumours will drastically reduce the incidence of “undifferentiated” diagnoses and will optimise patient management [21]. Further, staging of lymphoma would probably include CT of the neck/chest/abdomen/pelvis, whereas staging of soft tissue sarcoma requires chest CT alone. Correct diagnosis is essential to guide appropriate management with chemotherapy and avoid unnecessary surgery. In our institution, percutaneous image-guided biopsy was performed in all these patients, which yielded adequate tissue for diagnosis, with no failed biopsy. All of the patients in this series were referred back to local haematology services for further staging and treatment.
Limitations of the study
This was a retrospective case series of patients with a proven diagnosis of muscle lymphoma. No control group was included to try to determine the sensitivity and specificity of the described signs, and therefore, no comments can be made regarding the diagnostic accuracy of MRI in cases of suspected soft tissue lymphoma. This would be a valuable study for further research.
Conclusion
The MRI findings in 24 patients with pathologically proven soft tissue lymphoma have been described in the largest imaging series to date. MRI features include a soft tissue mass with intermediate T2W FSE SI, often mildly hyperintense to muscle on T1W, involving more than one muscle compartment, with extension into the subcutaneous tissues and along the neurovascular bundle.
References
Freeman C, Berg JW, Cutler SJ (1972) Occurrence and prognosis of extranodal lymphomas. Cancer 29:252–260
Travis WD, Banks PM, Reiman HM (1987) Primary extranodal soft tissue lymphoma of the extremities. Am J Surg Pathol 11:359–366
Komatsuda M, Nagao T, Arimori S (1981) An autopsy case of malignant lymphoma associated with remarkable infiltration in skeletal muscle. Rinsho Ketsueki 22:891–895
Reddy S, Saxena VS, Pellettiere EV, Hendrickson FR (1977) Early nodal and extra-nodal non-Hodgkin’s lymphomas. Cancer 40:98–104
Kransdorf MJ (1995) Malignant soft-tissue tumors in a large referral population: distribution of diagnoses by age, sex, and location. AJR Am J Roentgenol 164:129–134
Scally J, Garrett A (1989) Primary extranodal lymphoma in muscle. Br J Radiol 62:81
Nelson MC, Petrik JH, Lack EE, Glass-Royal M, Bogumill GP, Stull MA (1990) Lymphocyte-predominant Hodgkin disease manifested as a subcutaneous arm mass. AJR Am J Roentgenol 155:658–659
Grunshaw ND, Chalmers AG (1992) Skeletal muscle lymphoma. Clin Radiol 45:399–400
Metzler JP, Fleckenstein JL, Vuitch F, Frenkel EP (1992) Skeletal muscle lymphoma: MRI evaluation. Magn Reson Imaging 10:491–494
Malloy PC, Fishman EK, Magid D (1992) Lymphoma of bone, muscle, and skin: CT findings. AJR Am J Roentgenol 159:805–809
Panicek DM, Lautin JL, Schwartz LH, Castellino RA (1997) Non-Hodgkin lymphoma in skeletal muscle manifesting as homogeneous masses with CT attenuation similar to muscle. Skeletal Radiol 26:633–635
Eustace S, Winalski CS, McGowen A, Lan H, Dorfman D (1996) Skeletal muscle lymphoma: observations at MR imaging. Skeletal Radiol 25:425–430
Hosono M, Kobayashi H, Kotoura Y, Tsuboyama T, Tsutsui K, Konishi J (1995) Involvement of muscle by malignant lymphoma: MR and CT appearances. J Comput Assist Tomogr 19:455–459
Beggs I (1997) Primary muscle lymphoma. Clin Radiol 52:203–212
Lee VS, Martinez S, Coleman RE (1997) Primary muscle lymphoma: clinical and imaging findings. Radiology 203:237–244
Stiglbauer R, Graninger W, Prayer L, Kramer J, Schurawitzki H, Machold K, Imhof H (1993) Polymyositis: MRI-appearance at 1.5 T and correlation to clinical findings. Clin Radiol 48:244–248
Gordon BA, Martinez S, Collins AJ (1995) Pyomyositis: characteristics at CT and MR imaging. Radiology 197:279–286
Adams EM, Chow CK, Premkumar A, Plotz PH (1995) The idiopathic inflammatory myopathies: spectrum of MR imaging findings. Radiographics 15:563–574
Fleckenstein JL, Burns DK, Murphy FK, Jayson HT, Bonte FJ (1991) Differential diagnosis of bacterial myositis in AIDS: evaluation with MR imaging. Radiology 179:653–658
Hanna SL, Kaste S, Jenkins JJ, Hewan-Lowe K, Spence JV, Gupta M, Monson D, Fletcher BD (2002) Epithelioid sarcoma: clinical, MR imaging and pathologic findings. Skeletal Radiol 31:400–412
Berg AR, Linder J, Anderson RW, Tempero MA, Edney JA, Armitage JO (1985) The undifferentiated malignant neoplasm. Identification of lymphoma arising in skeletal muscle by immunohistochemical analysis. JAMA 254:2625–2626
Agur AMR (1991) Grant’s Atlas of Anatomy. 9th edn. Williams & Wilkins, Baltimore, Philadelphia, Hongkong
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Suresh, S., Saifuddin, A. & O’Donnell, P. Lymphoma presenting as a musculoskeletal soft tissue mass: MRI findings in 24 cases. Eur Radiol 18, 2628–2634 (2008). https://doi.org/10.1007/s00330-008-1014-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-008-1014-x