Abstract
The purpose is to evaluate the accuracy of integrated FDG-PET/CT, compared with PET alone, for diagnosis of suspected recurrence of uterine cervical cancer. Fifty-two women who had undergone treatment for histopathologically proven cervical cancer received PET/CT with suspected recurrence. PET-alone and integrated PET/CT images were evaluated by two different experienced radiologists by consensus for each investigation. A final diagnosis was confirmed by histopathology, radiological imaging, and clinical follow-up for over 1 year. Patient-based analysis showed that the sensitivity, specificity, and accuracy of PET/CT were 92.0% (23/25), 92.6% (25/27), and 92.3% (48/52), respectively, while for PET, the corresponding figures were 80.0% (20/25), 77.8% (21/27), and 78.8% (41/52), respectively. PET/CT resolved the false-positive PET results due to hypermetabolic activity of benign/inflammatory lesions and physiological variants, and was able to detect lung metastasis, local recurrence, peritoneal dissemination, para-aortic lymph node metastasis, and pelvic lymph node metastasis missed by PET alone. However, tiny local recurrence and lymph node metastasis could not be detected even by PET/CT. FDG-PET/CT is a useful complementary modality for providing good anatomic and functional localization of sites of recurrence during follow-up of patients with cervical cancer.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
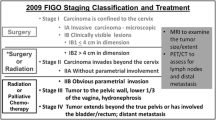
Despite continuing advances in surgical and non-surgical therapeutic strategies, cancer recurrence and distant metastasis after initial treatment are often a major problem for women with gynecologic cancers. Early and accurate detection of recurrence in patients with cervical cancer has an important influence on therapy, and selection of appropriate treatment strategies can be expected to have a significant impact on overall survival [1, 2]. Physical examination at control visits and measurement of tumor markers have often been used for follow-up. However, benign gynecologic as well as benign and malignant nongynecologic conditions are known to be associated with elevated levels of tumor markers, and such markers do not provide any information about the location of recurrence [3].
In gynecological malignancies, conventional morphological imaging modalities, including radiography, computed tomography (CT), and magnetic resonance (MR) imaging, are widely used to diagnose recurrent lesions. However, when used alone, these conventional imaging modalities are poor at visualizing small disseminated lesions and small lymph node metastases, and for differentiating recurrence from postoperative or post-radiation changes [4–8].
In the late 1990s, positron emission tomography (PET) with 2-[18F]fluoro-2-deoxy-D-glucose (18F-FDG), which exploits the increased utilization of glucose by malignant cells and thereby high uptake of glucose, has opened a new field in clinical imaging. It is possible to diagnose cancer recurrence and distant metastasis by PET in the preclinical stage before it becomes evident on conventional diagnostic imaging modalities. However, PET lacks anatomic information, and precise localization of any suspicious lesions may be difficult. Early diagnosis of cancer recurrence by PET is also impaired by the presence of increased uptake in physiologic, nonpathologic, or inflammatory states [9, 10].
Integrated PET/CT, in which a full-ring-detector clinical PET scanner and multidetector row helical CT scanner are combined, makes it possible to acquire both metabolic and anatomic imaging data using a single device in a single diagnostic session and provides precise anatomic localization of suspicious areas of increased FDG uptake and rules out false-positive PET findings [11].
There have been several studies of FDG-PET [12–19] and only two reports of integrated FDG-PET/CT [20, 21] describing their usefulness for the diagnosis of recurrent uterine cervical cancers. Chung et al. [20] and Sironi et al. [21] discussed the diagnostic accuracy of PET/CT, but did not compare PET/CT interpretation with PET-alone interpretation. Therefore, the true potential and the degree of superiority of an inline PET/CT system compared with PET examination for diagnosis remain unknown. The purpose of the present study was to assess the patient- and lesion-based diagnostic accuracy of PET/CT, as compared with PET alone, for the follow-up of patients previously treated for cervical cancer.
Materials and methods
Patients
Fifty-two consecutive patients (age range 37—78 years; mean 58 years) who had undergone treatment for histopathologically proven uterine cervical cancer underwent PET/CT examinations with suspected recurrence at our institution between April 2005 and June 2006, with the approval of the institutional review board. Informed consent was obtained from each patient after the nature of the procedures had been fully explained. Further details of these patients and their demographic data are listed in Table 1. Recurrence was suspected on the basis of physical examination (n = 21 patients), elevated levels of tumor markers (SCC, CEA, CA125, or CA 19–9) (n = 17), abnormal findings of conventional morphological imaging modalities, including CT and/or MR imaging (n = 6), both elevation of tumor marker levels and conventional imaging findings (n = 4), or an abnormal Papanicolau (Pap) smear (n = 4).
FDG-PET/CT study
Whole-body imaging was performed using a combined PET/CT scanner (Biograph Sensation 16, Siemens Systems, Erlangen, Germany). Whole-body CT covered a region ranging from the meatus of the ear to the mid thigh. The technical parameters of the 16-detector-row helical CT scanner were a gantry rotation speed of 0.5 s, a table speed of 24 mm per gantry rotation, 120 kVp, 40 mA, 2.5-mm slice thickness, and no specific breath-holding instructions. No oral or intravenous contrast materials were administered for the CT scan. The PET component of the combined imaging system had an axial view of 16.2 cm (per bed position) with an interslice spacing of 3.75 mm in one bed position and provided an image from the meatus of the ear to the mid thigh with six to seven bed positions. The transaxial field of view and pixel size of the PET images reconstructed for fusion were 58.5 cm and 4.57 mm, respectively, with a matrix size of 128 × 128. To avoid artifacts caused by the urinary tract, patients were asked to drink 1,000 ml of water orally 1–2 h prior to image acquisition and to void just before the start of acquisition. Urinary bladder catheterization was not used. After at least 4 h of fasting, patients received an intravenous injection of 4.0 MBq/kg body weight of FDG. The blood glucose levels were checked in all patients before FDG injection, and no patients showed a blood glucose level of more than 160 mg/dl. About 50 min later, CT images were acquired for 30 s. A whole-body emission PET scan for the same axial coverage was performed with 3 min of acquisition per bed position using a three-dimensional acquisition mode. Attenuation-corrected PET images were reconstructed with an ordered-subset expectation maximization iterative reconstruction algorithm (eight subsets, three iterations). PET, CT, and fused PET/CT images were generated for review on a computer workstation (AZE Virtual Place Version 3.0035).
Data interpretation and image analysis
PET images were retrospectively assessed in consensus by two experienced radiologists (reader A and reader B with 2 and 8 years of experience in PET, respectively) who had no knowledge of the other imaging results or the clinical data. PET images were viewed in coronal, axial, and sagittal sections, as is typically performed during clinical interpretation of these images. When focal 18F-FDG uptake, with an intensity higher than that of surrounding tissues, was seen in areas unrelated to physiologic or benign processes, it was defined as recurrence and/or distant metastasis by PET interpretation.
PET/CT images were retrospectively interpreted by the consensus of two experienced radiologists (reader C and reader D with 3 and 5 years of experience in PET/CT, respectively) who had no knowledge of the other imaging results or the clinical data. Attenuation-corrected PET images, CT images, and co-registered PET/CT images were displayed together on the monitor. Lymph nodes (LNs) with increased FDG uptake on PET scan, even if they were smaller than 1 cm in short-axis diameter on CT images, were defined as LN metastasis. Semiquantitative analysis was not done in this study.
Diagnostic ability was determined on a patient-basis and also on a ten-lesion location basis (retrovesical region, lung, liver, bone, peritoneum, supraclavicular LN, mediastinal and hilar LN, para-aortic LN, pelvic LN, and inguinal LN).
The final diagnosis was obtained from the results of histopathological examination (n = 21) or clinical follow-up for periods longer than 1 year (range 12–25 months; mean 17 months) on the basis of tumor marker levels and contrast-enhanced CT findings (n = 14), tumor marker levels and PET/CT findings (n = 12), and tumor marker levels (n = 5).
Statistical analysis
We performed a patient-based and lesion-based analysis of the fused PET/CT and PET-alone interpretations on the consensus verdict in general. Sensitivity, specificity, and accuracy were calculated using standard statistical formulas, and 95% confidence interval (95% CI) was determined for each parameter. McNemar test was used to determine statistical significance of differences among PET/CT and PET-alone interpretations. Differences at p value less than 0.05 were regarded as statistically significant.
Results
In 25 (48%) of the 52 patients, recurrence and distant metastasis were confirmed by pathologic examinations (n = 21) and clinical follow-up study (n = 4). On patient-based analysis, PET/CT interpretation was true-positive in 23 of the 25 patients with recurrence and true-negative in 25 of the 27 patients without recurrence; PET-alone interpretation was true-positive in 20 of the 25 patients with recurrence and true-negative in 21 of the 27 patients without recurrence (Table 2). PET/CT interpretation yielded a higher diagnostic result than PET-alone interpretation, and the difference in accuracy was statistically significant (p = 0.023, McNemar test). The differences in sensitivity and specificity were not statistically significant (p = 0.248 and 0.134, respectively, McNemar test).
Because inguinal LN metastasis was not observed, nine lesion sites including the retrovesical region, lung, liver, bone, peritoneum, supraclavicular LN, mediastinal and hilar LN, para-aortic LN, and pelvic LN were evaluated for each patient (Table 3). Therefore, a total of 468 regions of interest (ROIs) from PET/CT were studied in the 52 patients. PET/CT revealed four false-negative lesions and two false-positive lesions, whereas PET alone revealed nine false-negative lesions and 11 false-positive lesions. The sensitivity, specificity, and accuracy of PET/CT in terms of overall lesion sites were 89.5% (95% CI, 79.7% to 99.2%) (34/38), 99.5% (95% CI, 98.9% to 100%) (428/430), and 98.7% (95% CI, 97.7% to 99.7%) (462/468), respectively, whereas those of PET were 76.3% (95% CI, 62.8% to 89.8%) (29/38), 97.4% (95% CI, 96.0% to 98.9%) (419/430), and 95.7% (95% CI, 93.9% to 97.6%) (448/468), respectively. Although the difference in sensitivity was not statistically significant (p = 0.074, McNemar test), the differences in specificity and accuracy reached the statistical significance (p = 0.0077 and p = 0.00051, respectively, McNemar test).
The four false-negative lesions revealed by PET/CT comprised two lesions of local recurrence, which was confirmed by PAP smear and surgery, and two lesions of para-aortic LN metastases measuring 4 mm and 7 mm, which were confirmed by surgery. The two false-positive lesions revealed by PET/CT comprised one that was over-diagnosed as mediastinal and hilar LN metastasis, which was proved to be sarcoidosis by biopsy, and one that was over-diagnosed as bone metastasis due to osteolytic change of the L3 vertebra by CT and moderate focal FDG accumulation by PET, which was confirmed not to be malignant by bone biopsy and follow-up MR imaging. The nine false-negative lesions revealed by PET comprised three lesions of local recurrence, three lesions of para-aortic LN metastases measuring 4 mm, 7 mm, and 10 mm, one tiny peritoneal dissemination (Fig. 1), one small lung metastasis (Fig. 2), and one pelvic LN metastasis measuring 8 mm. The 11 false-positive lesions revealed by PET comprised two foci of physiological FDG uptake in the intestine that were misinterpreted as peritoneal dissemination, two foci of physiological FDG uptake in the intrapelvic vessel (Fig. 3) and bowel that were misinterpreted as pelvic LN metastases, one focus of physiological FDG uptake in the ureter that was misinterpreted as para-aortic LN metastasis, one focus of reactive and physiological FDG uptake in the mediastinal and hilar LN that was misinterpreted as LN metastasis, one sarcoidosis that was misinterpreted as mediastinal and hilar LN metastasis, one pulmonary tuberculosis that was misinterpreted as lung metastasis, one acute cholangitis that was misinterpreted as liver metastasis, one thyroid benign tumor that was misinterpreted as supraclavicular LN metastasis, and one lesion of vertebra degenerative change that was misinterpreted as bone metastasis. There were no cases of false negativity revealed by PET/CT and true positivity revealed by PET alone. There were also no cases of false positivity revealed by PET/CT and true negativity revealed by PET alone.
A 57-year-old woman of initial FIGO stage-IIIc with peritoneal dissemination. a PET showed several physiological FDG uptakes in the bowels, and peritoneal dissemination was not suspected. b CT showed a soft tissue mass outside the bowel wall in the right middle abdomen (arrow). c PET/CT showed that intense FDG uptake corresponded to a peritoneal mass seen in (b) (arrow), suggesting the presence of peritoneal dissemination. Histopathological examination of the surgical specimen revealed peritoneal dissemination in the right middle abdomen
A 67-year-old woman of initial FIGO stage-IIIc with multiple tiny lung metastases. (a). PET showed no abnormal FDG uptake in the lung and lung metastasis was not suspected. b CT showed four tiny nodules in the lung (arrows), suggesting the presence of multiple lung metastases. c PET/CT did not show abnormal FDG uptake corresponding to three pulmonary nodules seen in (b) (arrows), probably due to small size of nodule. Follow-up chest CT revealed the growth of these lung nodules, and biopsy revealed these lung nodules were lung metastases
A 61-year-old woman of initial FIGO stage-IIIc without recurrence. a PET showed area of intense FDG uptake in left pelvic region (arrow), and lymph node metastasis was suspected. b CT showed no abnormal findings. c PET/CT showed abnormal FDG uptake seen in (a) corresponded to the left iliac artery (arrow), suggesting the physiological tracer uptake in the vessel. Follow-up enhanced CT revealed no apparent evidence of pelvic lymph node metastasis
Discussion
To our knowledge, this is the first study to investigate the additional diagnostic value of integrated PET/CT over PET alone and to evaluate PET/CT accuracy in the point of not only patient-specific analysis, but also lesion-specific analysis for diagnosing recurrence of uterine cervical cancer. On patient- and lesion-based analyses, PET/CT tended to improve the restaging performance when compared to PET alone by slightly increasing the sensitivity, specificity, and accuracy. Moreover, the differences in patient-based accuracy and in lesion-based specificity and accuracy reached statistical significance. Although the differences in patient-based sensitivity and specificity and in lesion-based sensitivity did not reach statistical significance, this might have been attributable to the relatively small number of patients examined.
Several authors have investigated the usefulness of PET for postoperative or post-therapy surveillance of patients with cervical cancer and found that the sensitivity, specificity, and accuracy were 86–100%, 60–94%, and 70–97%, respectively (Table 4) [12–19]. These studies revealed that false-negative cases included local recurrence in the retrovesical region, pelvic recurrence, lung metastasis, peritoneal dissemination, pelvic LN metastasis, and para-aortic LN metastasis, whereas false-positive cases were due to inflammatory lesions, physiological uptake, and postoperative change. Chung et al. [20] and Sironi et al. [21] demonstrated the patient-based diagnostic accuracy of integrated PET/CT for post-therapy surveillance of patients with cervical cancer with 90–93% sensitivity, 81–100% specificity, and 87–96% accuracy, and found that false-negative cases included local recurrence, whereas the false-positive cases included local recurrence, lung metastasis, peritoneal dissemination, pelvic LN metastasis, and para-aortic LN metastasis. Sironi et al. [21] discussed both patients of cervical cancer and endometrial cancer, and the analysis of only patients with cervical cancer was not performed.
The false-negative and false-positive cases in our series were similar to those of previous PET and PET/CT studies, and the limited sensitivity and specificity of PET alone were partially resolved by the ability of PET/CT to acquire both metabolic and anatomic imaging information. In our series, PET/CT correctly identified five lesions that had been missed by PET alone (local recurrence, para-aortic LN metastasis, pelvic LN metastasis, peritoneal dissemination as shown in Fig. 1, and lung metastasis as shown in Fig. 2), and nine lesions that had been overdiagnosed by PET alone (inflammatory/benign lesions such as pulmonary tuberculosis, acute cholangitis, thyroid benign tumor, and physiological uptake in the bowel, the vessel as shown in Fig. 3, and the ureter). However, even PET/CT was unable to detect tiny local recurrence and tiny para-aortic LN metastases. PET and PET/CT can only detect LNs that have a certain volume of malignant cells sufficient to change the observed glucose metabolism, and neither of these modalities can detect micrometastasis. The spatial resolution of PET scans is insufficient for detection of microscopic metastases to LNs [22]. With a given spatial resolution of 4–6 mm with currently available PET and PET/CT systems, the detection of microscopic lesions remains challenging. Improving the spatial resolution and sensitivity of PET and PET/CT scanners and developing new, more specific radioactive tracers may help to overcome this limitation in the future.
Guidelines for optimal post-therapy surveilliance in patients treated for cervical cancer still remain to be defined, and the conventional follow-up program consists of physical examination, tumor marker evaluation, conventional imaging procedures, and a pap smear. Our data suggest that, as observed previously in patients with suspected recurrence of gynecological malignancy [21, 23], a combination of tumor markers and PET/CT may be highly efficient for detecting recurrence in patients with cervical cancer.
We believe that the added value of PET/CT in terms of patient clinical management and selection of appropriate treatment strategies relies mainly on its accurate ability to localize sites of recurrent disease anywhere in the body by means of a single non-invasive procedure. This allows distinction between a local and a disseminated recurrence pattern, thus assisting in selection of the optimal therapy: surgical resection ± radiation versus systemic chemotherapy ± radiation [24]. Moreover, PET/CT makes it possible to avoid unnecessary therapy.
In this study, the CT component of PET/CT was low-dose, and no oral or intravenous contrast materials were used. Adding an oral contrast agent will likely help to better delineate normal bowel activity and pathologic intraabdominal activity (peritoneal implants). Use of an intravenous contrast agent will likely help to detect small LN, tiny liver metastases, small foci of peritoneal dissemination, and local recurrence. A further PET/CT study with oral and intravenous contrast material is warranted in order to define more precisely its clinical role and accuracy for detection of recurrent lesions.
This study had certain limitations. First, the number of patients with suspected cervical cancer recurrence in our series was relatively small. More studies are needed with a larger sample size to help verify the diagnostic accuracy of PET/CT. Secondly, the ideal gold standard for any analysis is histological confirmation of the findings. However clinical follow-up is a valid way to evaluate diagnostic accuracy and response to therapy, and it would have been unethical to investigate all PET/CT-detected lesions using invasive procedures. Positive findings are easy to confirm, but negative findings only mean that we it is not possible to acquire positive findings during the follow-up period, making it uncertain whether the findings are truly negative.
In conclusion, integrated FDG-PET/CT is a useful complementary modality for providing good anatomic and functional localization of sites of recurrence during follow-up of patients with cervical cancer.
References
Larson DM, Copeland LJ, Stringer CA, Gershenson DM, Malone JM Jr, Edwards CL (1988) Recurrent cervical carcinoma after radical hysterectomy. Gynecol Oncol 30:381–387
Chou HH, Wang CC, Lai CH (2001) Isolated paraaortic lymph node recurrence after definitive irradiation for cervical carcinoma. Int J Radiat Oncol Biol Phys 51:442–448
Niloff JM, Bast RC Jr, Schaetzl EM, Knapp RC (1985) Predictive value of CA 125 antigen levels in second-look procedures for ovarian cancer. Am J Obstet Gynecol 44:207–212
Low RN, Sigeti JS (1994) MR imaging of peritoneal disease: comparison of contrast-enhanced fast multiplanar spoiled gradient-recalled and spin-echo imaging. Am J Roentgenol 163:1131–1140
Sugiyama T, Nishida T, Ushijima K et al (1995) Detection of lymph node metastasis in ovarian carcinoma and uterine corpus carcinoma by preoperative computerized tomography or magnetic resonance imaging. J Obstet Gynecol 21:551–556
Forstner R, Hricak H, Powell CB, Azizi L, Frankel SB, Stern JL (1995) Ovarian cancer recurrence: value of MR imaging. Radiology 196:1131–1140
Connor JP, Andrews JI, Anderson B, Buller RE (2000) Computed tomography in endometrial carcinoma. Obstet Gynecol 95:692–696
Topuz E, Aydiner A, Saip P et al (2000) Correlation of serum CA125 level and computerized tomography (CT) imaging with laparotomic findings following intraperitoneal chemotherapy in patients with ovarian cancer. Eur J Gynecol Oncol 21:599–602
Cook GJ, Maisey MN, Fogelman I (1999) Normal variants, artifacts and interpretative pitfalls in PET imaging with 18-fluoro-2-deoxyglucose and carbon-11 methionine. Eur J Nucl Med 26:1363–1379
Kostakoglu L, Agress H Jr, Goldsmith SJ (2003) Clinical role of FDG PET in evaluation of cancer patients. Radiographics 23:315–340
Beyer T, Townsend DW, Brun T et al (2000) A combined PET/CT scanner for clinical oncology. J Nucl Med 41:1369–1379
Park DH, Kim KH, Park SY, Lee BH, Choi CW, Chin SY (2000) Diagnosis of recurrent uterine cervical cancer: computed tomography versus positron emission tomography. Korean J Radiol 1:51–55
Sun SS, Chen TC, Yen RF, Shen YY, Changlai SP, Kao A (2001) Value of whole body 18F-fluoro-2-deoxyglucose positron emission tomography in the evaluation of recurrent cervical cancer. Anticancer Res 21:2957–2961
Ryu SY, Kim MH, Choi SC, Choi CW, Lee KH (2003) Detection of early recurrence with 18F-FDG PET in patients with cervical cancer. J Nucl Med 44:347–352
Nakamoto Y, Eisbruch A, Achtyes ED et al (2002) Prognostic value of positron emission tomography using F-18-fluorodeoxyglucose in patients with cervical cancer undergoing radiotherapy. Gynecol Oncol 84:289–295
Havrilesky LJ, Wong TZ, Secord AA, Berchuck A, Clarke-Pearson DL, Jones EL (2003) The role of PET scanning in the detection of recurrent cervical cancer. Gynecol Oncol 90:186–190
Lai CH, Huang KG, See LC et al (2004) Restaging of recurrent cervical carcinoma with dual-phase [18F]fluoro-2-deoxy-D-glucose positron emission tomography. Cancer 100:544–552
Chang TC, Law KS, Hong JH et al (2004) Positron emission tomography for unexplained elevation of serum squamous cell carcinoma antigen levels during follow-up for patients with cervical malignancies.-a phase II study. Cancer 101:164–171
Yen TC, See LC, Chang TC et al (2004) Defining the priority of using 18F-FDG PET for recurrent cervical cancer. J Nucl Med 45:1632–1639
Chung HH, Jo H, Kang WJ et al (2007) Clinical impact of integrated PET/CT on the management of suspected cervical cancer recurrence. Gynecol Oncol 104:529–534
Sironi S, Picchio M, Landoni C et al (2007) Post-therapy surveillance of patients with uterine cancers: value of integrated FDG PET/CT in the detection of recurrence. Eur J Nucl Med Mol Imaging 34:472–479
Shim SS, Lee KS, Kim BT et al (2005) Non-small cell lung cancer: prospective comparison of integrated FDG PET/CT and CT alone for preoperative staging. Radiology 236:1011–1019
Bristow RE, Del Carmen MG, Pannu HK et al (2003) Clinically occult recurrent ovarian cancer: patient selection for secondary cytoreductive surgery using combined PET/CT. Gynecol Oncol 90:519–528
Belhocine T (2004) 18F-FDG PET imaging in post-therapy monitoring of cervical cancers: from diagnosis to prognosis. J Nucl Med 45:1602–1604
Acknowledgments
We thank the staff of the department of obstetrics and gynecology, especially Ichio Fukasawa and Noriyuki Inaba, for recruiting patients. We also thank Kennichi Kobayashi, Kazufumi Suzuki, Kaoru Ishida, and Tomoyuki Sakamoto for their excellent technical assistance and generous support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kitajima, K., Murakami, K., Yamasaki, E. et al. Performance of FDG-PET/CT for diagnosis of recurrent uterine cervical cancer. Eur Radiol 18, 2040–2047 (2008). https://doi.org/10.1007/s00330-008-0979-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-008-0979-9