Abstract
We compared the cost effectiveness of recent approaches [coronary angiography and calcium scoring using computed tomography (CT) and stress magnetic resonance imaging (MRI)] to the diagnosis of coronary artery disease (CAD) with those of the traditional diagnostic modalities [conventional angiography (CATH), exercise ECG, and stress echocardiography] using a decision tree model. For patients with a 10% to 50% pretest likelihood of coronary artery disease, non-invasive coronary angiography using CT was the most cost effective approach, with costs per correctly identified CAD patient of €4,435 (10% likelihood) to €1,469 (50% likelihood). Only for a pretest likelihood of 30% to 40% was calcium scoring using CT more cost effective than any of the traditional diagnostic modalities, while MRI was not cost effective for any pretest likelihood. At a pretest likelihood of 60%, CT coronary angiography and CATH were equally effective, while CATH was most cost effective for a pretest likelihood of at least 70%. In conclusion, up to a pretest likelihood for coronary artery disease of 50%, CT coronary angiography is the most cost-effective procedure, being superior to the other new modalities and the most commonly used traditional diagnostic modalities. With a very high likelihood for disease (above 60%), CATH is the most effective procedure from the perspective of society.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cost-effectiveness analyses for new imaging modalities have become increasingly important worldwide [1–12]. Especially, non-invasive cardiac imaging using multislice computed tomography (MSCT) and magnetic resonance imaging (MRI) is evolving rapidly [13–17] and is also gaining acceptance among referring physicians and patients. However, it is not known how these new modalities compare economically with conventional coronary angiography and other traditional non-invasive diagnostic modalities. Treatment of coronary artery disease (CAD) accounts for costs of €6.1 billion annually in Germany and the overall cost for one CAD patient during his or her entire life is €64,000 [18]. We used a decision tree model to assess the cost effectiveness of new modalities for diagnosis of CAD in relation to pretest likelihood of disease and to compare them with traditional approaches.
Materials and methods
Based on the decision tree developed by Patterson et al. [6, 7], which allows one to assess cost effectiveness according to the pretest likelihood of disease, Dewey and Hamm recently suggested a cost-effectiveness analysis model for diagnosis of CAD in the German situation [19]. This method was adopted for the present study to compare (1) coronary angiography using multislice computed tomography (MSCT), (2) calcium scoring using electron-beam computed tomography (EBT), and (3) dobutamine stress magnetic resonance imaging (MRI) with traditional approaches to diagnosis of CAD (Fig. 1). The traditional modalities investigated for comparison were: conventional coronary angiography (CATH), exercise ECG (Ex-ECG), and dobutamine stress echocardiography (ECHO). In the mathematical model applied, hypothetical patient cohorts with different pretest likelihoods were submitted to the six different diagnostic strategies shown in Fig. 1. This approach of submitting hypothetical cohorts of patients with different pretest likelihoods for CAD to the different diagnostic strategies separately was initially suggested by Patterson et al. [6, 7] and has the advantage of evaluating diagnostic tests regardless of currently accepted therapeutic approaches. Pretest likelihoods for patients with suspected CAD are defined by different cardiovascular risk factors (such as gender and age) and anginal symptoms and can be calculated easily using tables or regression models [20, 21] (see Table 1). CATH was used for confirmation of the diagnosis in strategies 1 to 5 in patients whose non-invasive test results were positive or non-diagnostic (Fig. 1). The sixth strategy investigated was immediate CATH. Modality-specific parameters used for analysis were derived from the literature and are listed in Table 2. For the purpose of identifying diagnostic test accuracies we chose well-known meta-analyses of diagnostic performance, which are already available on the per-patient level for all tests but CT coronary angiography. For CT coronary angiography we used the results of an interim analysis of a meta-analysis (including studies with at least 12-slice CT) that is currently being conducted at our institution and which identified 12 studies (see Table 2). For all tests, significant CAD for calculation of per-patient sensitivities and specificities was defined as at least one coronary vessel with at least one stenosis with ≥50% diameter reduction on conventional coronary angiography. The cost for performing calcium scoring using EBT was based on the cost for MSCT coronary calcium scoring, since there is no cost difference between those two methods in the reimbursement system. This also has the advantage of reflecting the clinical ability to perform calcium scoring using MSCT [22–24]. Diagnostic accuracy of calcium scoring, however, was based on the results obtained with EBT, since far fewer data are available for MSCT in this regard.
Definition of cost effectiveness
Cost effectiveness [2] was defined as the ratio of the direct and indirect costs for a test and the number of patients correctly diagnosed as having CAD [7]. A decrease in the cost per correct diagnosis thus indicates improved cost effectiveness. Correct diagnosis of absence of disease was not considered a direct criterion of effectiveness, whereas complications in patients with a false-negative diagnosis were included as indirect cost.
Definition of cost
The cost of a diagnostic test strategy comprised the following components: direct cost (reimbursement rates for the modalities) multiplied by the number of patients and indirect cost (cost of subsequent tests, cost of complications associated with the diagnostic modality, cost of additional tests, and cost resulting from diagnosis of a patient as false negative, multiplied by the respective number of patients). The overall cost of a diagnostic strategy (see Fig. 1) was calculated for each patient cohort with a defined pretest likelihood varying from 10% to 100% as the sum of all direct and indirect cost items multiplied by the respective number of patients. No attempt was made to take into consideration the actual cost from the perspective of healthcare providers, as those amounts are subject to wide regional variation. Instead, we used the established reimbursement rates for the six tests, as these most truly reflect the perspective of society. Since diagnostic tests for CAD are mainly performed on an outpatient basis, reimbursement rates for the tests were taken from the current German outpatient reimbursement system (“Einheitlichen Bewertungsmaßstab EBM 2000plus” [51]). The underlying reimbursement point value (“Punktwert”) used for calculation purposes was 5.11¢. The total cost for each test was calculated by adding the cost of drugs administered (Table 2). The cost for complications (including mortality) was calculated by assuming acute myocardial infarction as a typical example of a serious complication and thus calculating the cost of a typical complication on the basis of the study by Patterson and co-workers [7]. The costs of myocardial infarction comprise (1) hospitalisation, (2) rehabilitation and (3) non-productive time. Based on the current German reimbursement system for inpatients (“Diagnosis-related groups”, DRGs), the basic reimbursement for a myocardial infarction is €2,999.81, with relative weightings of 1.776 and 1.237, resulting in a total reimbursement of €6,210.48 and €4,325.65 (mean €5,268.07) for F41Z and F42Z (“Invasive cardiac diagnostic evaluation in acute myocardial infarction with very severe and without complications or co-morbidities, respectively”). The cost of rehabilitation is €3,000 [52]. With an assumed absence of the patient from work for 2 months, the cost of non-productive time is €3,474, based on the gross domestic product per inhabitant [53]. The average overall cost of a myocardial infarction thus amounts to €11,742.07. In addition, the analysis included complication-related costs resulting from CAD’s being missed by the tests used (false negative). This cost was also calculated on the assumption that myocardial infarction is a typical complication and that there is a likelihood of 25% of myocardial infarction over a follow-up period of 10 years [7]. An annual discounting of 5% was assumed for complication-related costs.
Sensitivity and break-even analysis
A sensitivity analysis was performed to test the robustness of the model with the following variations of the standard parameters (Table 2): (1) increasing or decreasing the accuracies of all non-invasive tests in the 95% confidence intervals, (2) increasing and decreasing the complication rates of CATH (2.0% and 0.5%), (3) assuming higher and lower complication-related costs (€15,000 and €5,000, respectively) and (4) taking into account expensive and less expensive CATH (€750 and €500). It is useful to consider cost and value from a different perspective [2]. Thus, in addition, a break-even analysis based on our own experience from the perspective of healthcare providers was performed for MSCT coronary angiography (Table 3).
Results
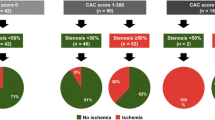
The proportion of patients with coronary artery disease that were correctly identified by MSCT, EBT, and MRI depended on sensitivity, specificity, and the rate of non-diagnostic examinations and differed relevantly for the new modalities (Fig. 2). CATH, as the gold standard in the present cost effectiveness analysis, was 100% accurate, while its advantage over the other modalities increased with the pretest likelihood for CAD. MSCT was the second best method with regard to accuracy, followed by EBT, MRI, and ECHO (Fig. 2).
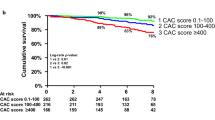
The costs per correctly identified CAD patient decreased hyperbolically with increasing pretest likelihood for all modalities (Fig. 3). Nevertheless, the total costs per patient increased with the pretest likelihood (data not shown). For patients with a pretest likelihood of CAD in the range of 10% to 50%, MSCT was the most cost-effective approach, with costs per correctly identified CAD patient of €4,435 (10% likelihood) to €1,469 (50% likelihood, Fig. 3a). Ex-ECG was more cost effective than ECHO, at a likelihood of 10% (€5,313 vs €5,583), while ECHO was the most cost-effective traditional approach for patients, with a likelihood of 20% (€3,207) to 30% (€2,416, Fig. 3a). At a pretest likelihood of 60%, MSCT and CATH were equally effective, with costs of €1,345, while CATH was most cost effective for a pretest likelihood of at least 70%, with costs of €1,153 (70% likelihood) to €807 (100% likelihood, Fig. 3a). For a pretest likelihood of 30% to 40%, EBT was more cost effective than any of the traditional diagnostic modalities, but not MSCT, with costs of €2,345 (30% likelihood) to €1,897 (40% likelihood, Fig. 3b). However, for likelihoods of 50% or greater, CATH was more cost effective than EBT (Fig. 3b). MRI was not cost effective for any pretest likelihood (Fig. 3c).
The dependency of cost effectiveness on pretest likelihood is illustrated by examples of three patient types (Fig. 4). In patients with a low-to-intermediate (13% and 30%) pretest likelihood for CAD, MSCT was most cost effective (Fig. 4a,b). When pretest likelihood was higher (63%), CATH was the most cost-effective procedure from the perspective of society (Fig. 4c).
Cost effectiveness (cost per correctly identified CAD patient) of MSCT in comparison with the traditional diagnostic modalities for examples of three different patient types: 1a 40-year-old female smoker with atypical angina pectoris (13% pretest likelihood); 2 a 35-year-old male patient with typical angina pectoris but without risk factors (30% pretest likelihood); 3 a 60-year-old female diabetic patient with typical angina pectoris (63% pretest likelihood). Pretest likelihoods were estimated with the logistic regression model of Pryor et al. [21]
Sensitivity analysis
At a maximally increased and decreased accuracy within the 95% confidence interval, MSCT was the most cost-effective modality up to a pretest likelihood of 60% and 50%, respectively. The order of the non-invasive modalities remained unchanged by this simulation. At a sole reduction of the accuracy within the 95% confidence interval, EBT was more cost effective than the traditional approaches only for a pretest likelihood of 40%.
When the accuracy of EBT was maximally increased within the 95% confidence interval, EBT was more cost effective than the traditional approaches for pretest likelihoods of 20% to 50%. If the diagnostic accuracy of MSCT was simultaneously reduced at a maximally increased accuracy of EBT (“worst-case scenario”), MSCT remained more effective than EBT from an economic perspective, indicating robustness of the model. Since no 95% confidence intervals were available for dobutamine stress MRI, no simulations could be obtained for this modality. Neither increasing (2.0%) nor decreasing (0.5%) the complication rates of CATH changed the order of the modalities, and CATH was most effective for pretest likelihoods of 50% or greater. At higher and lower complication-related costs (€15,000 and €5,000), MSCT remained most cost effective up to pretest likelihoods of 60% and 70%, respectively. On condition of an increase (€750) and decrease (€500) of the reimbursement for CATH, this invasive modality was more cost effective than MSCT from 80% and 50% on, respectively. The cost-effectiveness order of the modalities was not changed by these sensitivity modulations. Up to reimbursement rates of €260, MSCT was still the most cost-effective non-invasive modality at all pretest likelihoods. At higher reimbursement rates other non-invasive modalities overtook MSCT from an economic perspective.
Break-even analysis
For the current reimbursement rate of MSCT and at ten coronary examinations per day the expenses were always higher than the takings (Fig. 5a). At a reimbursement rate of MSCT that still allowed this test to be most cost effective from societal perspective (€260), the break-even point would come only after the rather long period of 64 months (Fig. 5b). In a high-referral centre (30 coronary MSCT examinations per day), already with the present reimbursement rate the break-even point could be reached after a short period of 23 months (Fig. 5c). However, since such high referral rates are rather unlikely, MSCT coronary angiography would only be profitable in a reasonable time frame after investment if reimbursement were three-times higher than with the present outpatient reimbursement system in Germany (Fig. 5d).
a–d Break-even analysis for MSCT coronary angiography with four simulations. For the calculated current reimbursement rate (€124.43) and at ten coronary examinations per day (2,200 examinations per year) the expenses are always higher than the takings (a). If the reimbursement rate of MSCT including contrast agent costs were increased to €260 (net reimbursement for radiologist: €208.74)—still allowing MSCT to remain the most cost-effective modality from the perspective of society—the break-even point would come only after 64 months (b). If 30 examinations were to be performed per day (6,600 examinations per year) at the current reimbursement rate the break-even point could be reached after 23 months (c). Since such a high referral rate would be unlikely as of yet, and the plausibility inspection of a radiologist’s maximum working time allows only 12 hours daily, we also simulated a similar favourable outcome with a break-even point after 23 months in d. In this case ten examinations would be performed per day at a reimbursement rate increased by a factor of 3 (including contrast agent cost 424.55; net reimbursement for radiologist €373.29)
Discussion
The economic efficiency of medical strategies from the perspective of society has become increasingly important worldwide [1–12]. In the cost-effectiveness analysis presented here we examined new non-invasive modalities and the most common traditional approaches to the diagnosis of CAD. Myocardial stress scintigraphy [single-photon emission computed tomography (SPECT)] was not included as one of the traditional approaches in the present study because it has already recently been shown not to be cost effective for diagnosis of CAD, based on the current German reimbursement system [19]. Our results show that, at pretest likelihoods of up to 50%, MSCT is the most cost-effective test to diagnose CAD, while, at higher likelihoods of disease (above 60%), CATH is the most recommendable approach.
There was a hyperbolic decrease in costs for each patient correctly diagnosed with CAD as the pretest likelihood increased. This observation is attributable to the fact that a correct diagnosis was classified as a positive effect in the cost-effectiveness analysis model and that this positive effect becomes more frequent as the pretest likelihood increases. The pretest likelihood of CAD is a major determinant of the ranking of the investigated diagnostic tests in terms of cost effectiveness. For instance, MSCT is most cost effective for a low-to-intermediate pretest likelihood of CAD (up to 50%), whereas CATH without prior invasive tests is most cost effective for a likelihood of 60% or greater. These observations clearly indicate that estimation of pretest likelihood of disease is an important criterion in selecting the most appropriate diagnostic strategy. Simple tools are available for determining pretest likelihood in the routine clinical setting [20, 21] (Table 1). Dewey and Hamm have recently applied the model developed by Patterson et al. [6, 7] to analyse the cost effectiveness of the traditional diagnostic modalities for CAD in Germany [19]. In this study it was concluded that CATH is the most-cost effective procedure for a pretest likelihood of 50% or greater, while Ex-ECG and ECHO are the preferred modalities for diagnosis of CAD at lower pretest likelihoods, from an economic perspective. Our study adds knowledge with regard to the up-and-coming non-invasive cardiac imaging modalities MSCT, EBT, and MRI. The results of the present study suggest that EBT (or MSCT) for calcium scoring and stress MRI cannot be recommended from an economic perspective, while MSCT coronary angiography has the potential to reduce cost in patients with a pretest likelihood of up to 50%.
The analysis of cost effectiveness using the mathematical models presented here has a number of limitations: (1) The relevance of the results for clinical practice is much lower than that of findings obtained in clinical studies that investigate cost effectiveness in addition to the efficiency of a diagnostic test [8]. (2) In general, cost-benefit calculations might provide more information than an analysis of cost effectiveness [54]. However, cost per quality-adjusted life years saved is not the best outcome measure for evaluating the cost effectiveness of imaging examinations [11], and it appears more suitable to apply variables that represent the influence of imaging on subsequent management (e.g. correctly identified patients) [11]. (3) Correct exclusion of disease was not a direct criterion of effectiveness in the model used here but has an indirect effect in terms of lower costs in patients without complications. (4) Variations in the overall predictive accuracy as they are identified in different meta-analyses have a fairly large effect on the result. We tried to minimise these effects by carefully selecting data on sensitivity and specificity published in the most recent meta-analyses. Moreover, we performed a sensitivity analysis with variation of parameters within the 95% confidence intervals to test the robustness of the results. Another possible disadvantage is that we did not consider the cost of treating CAD. However, the advantage of the present cost-effectiveness model lies exactly in the fact that it evaluates diagnostic tests regardless of currently accepted therapeutic approaches [55]. Another advantage over previous cost-effectiveness studies [4] is that the pretest likelihood, as one of the main variables [11], was taken into account in the current analysis using variations from 10% to 100%. Also interpretability, as another main variable [11], was considered by including rates of non-diagnostic examinations. The calculated outpatient reimbursement rates from 2006 were the basis for the present study, since the diagnostic modalities analysed are most commonly applied in an outpatient setting.
The break-even analysis shows that MSCT coronary angiography would only be profitable if reimbursement were three-times higher than with the present outpatient reimbursement system. From the perspective of society, however, MSCT would only be more cost effective than any other non-invasive modality if the overall cost were below €260. But, at the resulting net reimbursement rate for radiologists of €208.74, the break-even point would come only after the rather long period of 64 months (Fig. 5b), clearly illustrating the complexity of integrating the needs of healthcare providers and society into one strategy for the diagnosis of CAD.
Finally, we conclude that MSCT coronary angiography is the most cost-effective new modality for diagnosis of CAD which is also more effective than the traditional approaches up to a pretest likelihood of disease of 50%, from the perspective of society. However, from the perspective of the healthcare providers, MSCT coronary angiography would be profitable in a reasonably short course after investment only if the reimbursement rate were increased by a factor of 3. CATH remains the most cost-effective modality in patients with a rather high likelihood of CAD (above 60%).
References
Drummond MF, Jefferson TO (1996) Guidelines for authors and peer reviewers of economic submissions to the BMJ. The BMJ economic evaluation working party. BMJ 313:275–283
Lipton MJ, Metz CE (2000) Cost effectiveness in radiology. Eur Radiol 10 [Suppl 3]:S390–S392
McNeil BJ (2000) Changing roles of decision analysis and cost effectiveness analyses in medicine and radiology. Eur Radiol 10 [Suppl 3]:S340–S343
Garber AM, Solomon NA (1999) Cost effectiveness of alternative test strategies for the diagnosis of coronary artery disease. Ann Intern Med 130:719–728
Kuntz KM, Fleischmann KE, Hunink MG, Douglas PS (1999) Cost effectiveness of diagnostic strategies for patients with chest pain. Ann Intern Med 130:709–718
Patterson RE, Eng C, Horowitz SF, Gorlin R, Goldstein SR (1984) Bayesian comparison of cost effectiveness of different clinical approaches to diagnose coronary artery disease. J Am Coll Cardiol 4:278–289
Patterson RE, Eisner RL, Horowitz SF (1995) Comparison of cost effectiveness and utility of exercise ECG, single photon emission computed tomography, positron emission tomography, and coronary angiography for diagnosis of coronary artery disease. Circulation 91:54–65
Dewey M, Hamm B (2003) Cost effectiveness in diagnosis of coronary artery disease. Fortschr Rontgenstr 175:749–751
Rumberger JA, Behrenbeck T, Breen JF, Sheedy PF 2nd (1999) Coronary calcification by electron beam computed tomography and obstructive coronary artery disease: a model for costs and effectiveness of diagnosis as compared with conventional cardiac testing methods. J Am Coll Cardiol 33:453–462
Alanen J, Keski-Nisula L, Blanco-Sequeiros R, Tervonen O (2004) Cost comparison analysis of low-field (0.23 T) MRI- and CT-guided bone biopsies. Eur Radiol 14:123–128
Heller D, Hricak H (2000) Cost effectiveness of new technologies for staging endometrial cancer. Eur Radiol 10 [Suppl 3]:S381–S385
Hövels AM, Heesakkers RA, Adang EM, Jager GJ, Barentsz JO (2004) Cost-analysis of staging methods for lymph nodes in patients with prostate cancer: MRI with a lymph node-specific contrast agent compared to pelvic lymph node dissection or CT. Eur Radiol 14:1707–1712
Becker CR (2005) Coronary CT angiography in symptomatic patients. Eur Radiol 15 [Suppl 2]:B33–B41
Bogaert J, Dymarkowski S (2005) Delayed contrast-enhanced MRI: use in myocardial viability assessment and other cardiac pathology. Eur Radiol 15 [Suppl 2]:B52–B58
Dewey M, Borges AC, Kivelitz D et al (2004) Coronary artery disease: new insights and their implications for radiology. Eur Radiol 14:1048–1054
Lipton MJ, Bogaert J, Boxt LM, Reba RC (2002) Imaging of ischemic heart disease. Eur Radiol 12:1061–1080
Pugliese F, Mollet NR, Runza G et al (2005) Diagnostic accuracy of non-invasive 64-slice CT coronary angiography in patients with stable angina pectoris. Eur Radiol:1–8
Klever-Deichert G, Hinzpeter B, Hunsche E, Lauterbach KW (1999) Costs of coronary heart diseases over the remaining life time in coronary heart disease cases—an analysis of the current status of coronary heart disease cases in Germany from the social perspective. Z Kardiol 88:991–1000
Dewey M, Hamm B (2004) Comparison of the cost effectiveness of the most common diagnostic methods for coronary artery disease. Dtsch Med Wochenschr 129:1415–1419
Diamond GA, Forrester JS (1979) Analysis of probability as an aid in the clinical diagnosis of coronary-artery disease. N Engl J Med 300:1350–1358
Pryor DB, Shaw L, McCants CB et al (1993) Value of the history and physical in identifying patients at increased risk for coronary artery disease. Ann Intern Med 118:81–90
Horiguchi J, Fukuda H, Yamamoto H et al (2006) The impact of motion artifacts on the reproducibility of repeated coronary artery calcium measurements. Eur Radiol. DOI 10.1007/s00330-006-0278-2
Mahnken AH, Muhlenbruch G, Koos R et al (2006) Influence of a small field-of-view size on the detection of coronary artery calcifications with MSCT: in vitro and in vivo study. Eur Radiol 16:358–364
Wintersperger BJ, Nikolaou K (2005) Basics of cardiac MDCT: techniques and contrast application. Eur Radiol 15 [Suppl 2]:B2–B9
Nallamothu BK, Saint S, Bielak LF et al (2001) Electron-beam computed tomography in the diagnosis of coronary artery disease: a meta-analysis. Arch Intern Med 161:833–838
Nagel E, Lehmkuhl HB, Bocksch W et al (1999) Noninvasive diagnosis of ischemia-induced wall motion abnormalities with the use of high-dose dobutamine stress MRI: comparison with dobutamine stress echocardiography. Circulation 99:763–770
Sommer T, Hofer U, Omran H, Schild H (2002) Stress cine MRI for detection of coronary artery disease. Fortschr Roentgenstr 174:605–613
Kwok Y, Kim C, Grady D, Segal M, Redberg R (1999) Meta-analysis of exercise testing to detect coronary artery disease in women. Am J Cardiol 83:660–666
Gibbons RJ, Balady GJ, Beasley JW et al (1997) ACC/AHA Guidelines for exercise testing. A report of the American college of cardiology/American heart association task force on practice guidelines (Committee on Exercise Testing). J Am Coll Cardiol 30:260–311
Fleischmann KE, Hunink MG, Kuntz KM, Douglas PS (1998) Exercise echocardiography or exercise SPECT imaging? A meta-analysis of diagnostic test performance. JAMA 280:913–920
Geleijnse ML, Fioretti PM, Roelandt JR (1997) Methodology, feasibility, safety and diagnostic accuracy of dobutamine stress echocardiography. J Am Coll Cardiol 30:595–606
Katayama H, Yamaguchi K, Kozuka T, Takashima T, Seez P, Matsuura K (1990) Adverse reactions to ionic and nonionic contrast media. A report from the Japanese committee on the safety of contrast media. Radiology 175:621–628
Hiro J, Hiro T, Reid CL, Ebrahimi R, Matsuzaki M, Gardin JM (1997) Safety and results of dobutamine stress echocardiography in women versus men and in patients older and younger than 75 years of age. Am J Cardiol 80:1014–1020
Mertes H, Sawada SG, Ryan T et al (1993) Symptoms, adverse effects, and complications associated with dobutamine stress echocardiography. Experience in 1118 patients. Circulation 88:15–19
Picano E, Mathias W Jr, Pingitore A, Bigi R, Previtali M (1994) Safety and tolerability of dobutamine–atropine stress echocardiography: a prospective, multicentre study. Echo Dobutamine International Cooperative Study Group. Lancet 344:1190–1192
Secknus MA, Marwick TH (1997) Evolution of dobutamine echocardiography protocols and indications: safety and side effects in 3011 studies over 5 years. J Am Coll Cardiol 29:1234–1240
Bundesgeschäftsstelle, Qualitätssicherung. BQS Qualitätsreport 2001. http://www.bqs-online.de, pp 88–95
Noto TJ Jr, Johnson LW, Krone R et al (1991) Cardiac catheterization 1990: a report of the Registry of the Society for Cardiac Angiography and Interventions (SCA&I). Catheter Cardiovasc Diagn 24:75–83
Nieman K, Cademartiri F, Lemos PA, Raaijmakers R, Pattynama PM, de Feyter PJ (2002) Reliable noninvasive coronary angiography with fast submillimeter multislice spiral computed tomography. Circulation 106:2051–2054
Ropers D, Baum U, Pohle K et al (2003) Detection of coronary artery stenoses with thin-slice multi-detector row spiral computed tomography and multiplanar reconstruction. Circulation 107:664–666
Mollet NR, Cademartiri F, Nieman K et al (2004) Multislice spiral computed tomography coronary angiography in patients with stable angina pectoris. J Am Coll Cardiol 43:2265–2270
Hoffmann U, Moselewski F, Cury RC et al (2004) Predictive value of 16-slice multidetector spiral computed tomography to detect significant obstructive coronary artery disease in patients at high risk for coronary artery disease: patient-versus segment-based analysis. Circulation 110:2638–2643
Mollet NR, Cademartiri F, Krestin GP et al (2005) Improved diagnostic accuracy with 16-row multi-slice computed tomography coronary angiography. J Am Coll Cardiol 45:128–132
Hoffmann MH, Shi H, Schmitz BL et al (2005) Noninvasive coronary angiography with multislice computed tomography. JAMA 293:2471–2478
Dewey M, Teige F, Schnapauff D et al (2006) Noninvasive detection of coronary artery stenoses with multislice computed tomography or magnetic resonance imaging. Ann Intern Med (in press)
Achenbach S, Ropers D, Pohle FK et al (2005) Detection of coronary artery stenoses using multi-detector CT with 16×0.75 collimation and 375 ms rotation. Eur Heart J (Epub)
Kefer J, Coche E, Legros G et al (2005) Head-to-head comparison of three-dimensional navigator-gated magnetic resonance imaging and 16-slice computed tomography to detect coronary artery stenosis in patients. J Am Coll Cardiol 46:92–100
Leber AW, Knez A, von Ziegler F et al (2005) Quantification of obstructive and nonobstructive coronary lesions by 64-slice computed tomography: a comparative study with quantitative coronary angiography and intravascular ultrasound. J Am Coll Cardiol 46:147–154
Martuscelli E, Romagnoli A, D’Eliseo A et al (2004) Accuracy of thin-slice computed tomography in the detection of coronary stenoses. Eur Heart J 25:1043–1048
Raff GL, Gallagher MJ, O’Neill WW, Goldstein JA (2005) Diagnostic accuracy of noninvasive coronary angiography using 64-slice spiral computed tomography. J Am Coll Cardiol 46:552–557
Kassenärztliche, Bundesvereinigung. Einheitlicher Bewertungsmaßstab (EBM 2000plus) 2005. http://www.ebm2000plus.de/
Tegtbur U, Machold H, Brinkmeier U, Busse M (2001) Ambulante kardiale Langzeitrehabilitation: 1-Jahres-Ergebnisse. Gesundheitswesen 63 [Suppl 1]:S39–S42
OECD. GDP per capita, 2001. In: OECD, 2003
Gandjour A, Lauterbach KW (2002) Cost effectiveness of quality improvement measures in health care. Med Klin 97:499–502
Elkin M (1982) President’s address. Issues in radiology related to the new technologies. Radiology 143:1–6
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dewey, M., Hamm, B. Cost effectiveness of coronary angiography and calcium scoring using CT and stress MRI for diagnosis of coronary artery disease. Eur Radiol 17, 1301–1309 (2007). https://doi.org/10.1007/s00330-006-0439-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-006-0439-3