Abstract
Basilar expansion of the sphenoidal sinus (BESS) was studied in order to demonstrate its critical relevance in endoscopic or microscopic endonasal surgical interventions, including access to the sphenoidal sinus itself or in transsphenoidal pituitary approaches. Direct evaluation of anatomical specimens (25 dry skulls and 25 formalin-fixed hemi heads) and the use of computerized tomography (CT) (50 dry skulls and 750 patients) showed a high BESS frequency (69%). The authors considered BESS to be critical when the posterior wall of the clivus was 2-mm thick and found a high incidence of this important anatomical variation (44%). This study also evaluated the relationship between the sinonasal septa, the clivus, and the internal carotid arteries, and a considerable regularity in the location of these structures was seen. The septa were anatomically related to the internal carotid arteries in 55% and to the clivus in 33% of the cases. In conclusion, the high frequency of critical BESS here described is relevant to endoscopic or microscopic endonasal surgical interventions, including access to the sphenoidal sinus itself or in transsphenoidal pituitary approaches.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There is significant variation in the structure of the sphenoidal sinus among different human skulls, even when both sides of the same skull are analyzed, as previously described by Zuckerlandl [1] in 1892. This variability appears to contribute to the few papers published in the literature defining standard sinonasal configuration and the significance of its internal septa and limits.
Sphenoid bone growth occurs in processes, each with its own ossification center [1–4]. These centers are arranged along an anterior-posterior plane on both sides of the sphenoid bone allowing the sinuses to be divided into three types: anterior to the fusion plane of the pre- and basisphenoid, slightly anterior to the clivus, or in an intermediate position [3]. A four-group division was previously proposed [4]. The first group, or conchal sinuses, includes the anterior expansion of the sinuses to the conchal presphenoid. The second group, or presphenoidal sinuses,” includes those expanding to the presphenoid (but not to the basisphenoid). The third group, or basisphenoidal sinuses,, is formed by sinuses that reach but do not exceed the limit of the basisphenoid. The fourth group includes sinuses extending to the basilar portion of the occipital bone, characterizing the sphenoid-occipital sinuses. This latter group corresponds to the basilar prolongation previously described by Sieur and Jacob in 1901 [2] and Testut and Jacob in 1909 [5]. An alternative classification based on a surgical approach has only the pre- and postsellar types [6].
Development of the human sphenoidal sinus in different stages of life is slow and continuous [7]. The process of aeration in the sphenoidal sinus is not seen before 6 months of age but is present in about 50% of 2-year-old children. This frequency increases to 90% at 4 years of age and reaches 100% by 10 years of age [8]. Imaging studies using computerized tomography (CT) of patients with ages from 1 to 80 years demonstrated that the expansion of the sphenoidal sinus starts at 5 years of age, shows different degrees of aeration after 6 years of age, and becomes slower with aging (Yonetsu et al. 1999) [9].
Despite the wide variation seen in the conformation of the sphenoidal sinus, its anatomy resembles a cubical structure, limited by anterior (nasoethmoidal), internal–lateral (septal), external–lateral (cavernous), superior (pituitary), and inferior (choanal) walls [10–13]. The different forms of aeration allowed various authors to designate sinonasal expansions according to the sphenoidal processes. Expansion of the anterior clinoid process, or anterior expansion, is one of the most important anatomical variations, defining a strict relationship with the optic canal [14]. Palatine expansion occurs along the anterior–posterior plane contiguous to the maxillary sinus. Located inferior and laterally, the presence of the pterygoid expansion exposes the foramen rotundum and pterygoid canal. A more developed expansion, spreading over the great wing of the sphenoidal bone, is known as the alar expansion.
The basilar expansion of the sphenoidal sinus (BESS) is a posterior expansion anterior and inferior to the clivus. When it reaches the basilar portion of the occipital bone, direct contact with the meningeal planes, basilar plexus, basilar artery, and pons may be established. A review of published literature regarding BESS frequency and its surgical importance showed various descriptions, mainly based on its presence and/or form. Thus, BESS is also known as the postsellar expansion, basilar extension, basilar prolongation [2, 5], posterior prolongation [3, 13], basilar recess [1], sinonasal recess, occipital recess, occipital-sphenoidal sinus [4], and expansion to the body of the occipital bone [15].
As a result of development of novel endonasal surgical techniques, such as image-guided surgery associated with endoscopic and/or microscopic approaches, BESS is now being considered an important sinonasal type [16–22]. These new methodologies allow careful study of BESS in cases of drainage of intrasinus inflammatory processes (e.g., mucocele, mucopyocele, fungal sinusitis) as well as access to the pituitary gland and apex petrosus [22, 23], preventing complications resulting from clival perforation. It should be noted, however, that when BESS is present, the bony protection of the internal carotid artery is absent, exposing this vessel to significant risk of damage. Pertinent literature mentions considerable variation in the sinonasal septa associated with BESS [24, 25]. These are frequently related to the internal carotid arteries and may hinder transsphenoidal access to the pituitary gland.
The sphenoidal sinus is a region that poses high surgical risk, and the use of skull base surgical techniques using transsphenoidal approach is increasing. Thus, the objective of this study was to assess the frequency and types of sphenoidal sinus posterior expansion as well as its septation and resulting relationship with the internal carotid artery.
Materials and methods
This study was conducted by the Institute of Biomedical Sciences of the University of São Paulo and the Hospital Beneficência Portuguesa of São Paulo in accordance with current regulations regarding trials in humans. Digitalized photographic documentation of the anatomical research was obtained from adult males and females, 25 being formalin-fixed (10%) hemi heads and 25 dried hemi skulls.
The radiological study was performed using the helical CT technique (Hispeed CT/i, GE Medical Systems, Milwaukee, WI, USA) employing axial and reformatted sagittal images. The first group included 750 CT exams from patients aged 18 years or older belonging to the files of the Med Imagem radiological department from the Hospital Beneficência Portuguesa in São Paulo analyzed within a 6-month period. Images obtained from 50 dried skull bases formed the second experimental group. Specimens were preselected by transillumination, and those in which BESS was likely to be present were evaluated to establish reliable parameters to estimate minimum thickness of the clivus.
Both in anatomical and radiological specimens, two types of BESS were considered: those extending to the posterior wall of the sella turcica along a line perpendicular to the planum sphenoidale, and clivus thickness equal to or greater than 2 mm were considered to be noncritical BESS. More relevant than the degree of posterior extension, the main criterion for establishing critical BESS was a clivus thickness of less than 2 mm (Fig. 1).
Based on the posterior insertion of the intersinus septum, the following six groups of sphenoidal sinus were determined: critical dominant, unilateral, bilateral, noncritical dominant, unilateral, and bilateral. When the septum was not directly inserted into the clivus allowing the relationship between the expanded sphenoidal sinus with both right and left internal carotid arteries, it was considered as dominant (Fig. 2a). The unilateral expanded sphenoidal sinus exhibited the septum inserted into the clivus and consequently was related only to one internal carotid artery (Fig. 2b). The bilateral type always showed the septum inserted into the clivus, and each expanded sinus related to its ipsilateral internal carotid artery (Fig. 2c).
Drawings and schematic representations in the axial plane illustrating the main septa of the sphenoidal sinus. Yellow triangles and red circles represent fusion points of the posterior part of the sphenoidal bone and internal carotid arteries, respectively. a Dominant critical basilar expansion of the sphenoidal sinus (BESS); b dominant unilateral critical BESS; c bilateral critical BESS
The relationship of the intersinus and accessory septa with the carotic sulci was also evaluated in all six groups.
Results
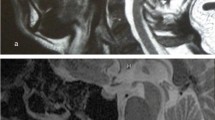
Thickness of the posterior wall of the sphenoidal sinus in the dried hemi skulls was variable, occasionally very thin, or even dehiscent. This feature was used to distinguish between critical and noncritical BESS types. Presence of a thin mucous membrane and the typical consistency of the dura mater in the hemi heads did not affect discrimination of these two BESS types (Fig. 3).
a Hemi head showing critical basilar expansion of the sphenoidal sinus (BESS) where the thin posterior wall of the sphenoidal sinus (arrow), the venous basilar plexus attached to the clivus (arrowheads), and the dura mater (double arrows) are clearly shown. b Hemi skulls showing critical BESS type. The upper portion of the square is tangential to the planum sphenoidale in both figure (scale in millimeters)
CT images reliably reproduced bony tissue of the posterior wall of the sphenoidal sinus. Thus, from a total of 750 CT exams, BESS was seen in 518 cases (69%) where 334 (44%) exhibited critical BESS and 184 (25 %) had noncritical BESS. The number and percentages of the six groups of BESS are expressed in Table 1.
Two patients with dominant and critical BESS exhibited a cerebral spinal fluid (CSF) fistula, one spontaneous and the other of traumatic origin (Fig. 4).
Spontaneous (a, b) and traumatic (c, d) cerebral spinal fluid (CSF) fistulae in right-dominant, critical basilar expansion of the sphenoid sinus (BESS). Arrows indicate bony dehiscence at the clivus (a) and at surgery, an endoscopic view based on image-guided surgery (b). Fractured clivus (single arrows) and pneumoencephalos (double arrows) demonstrated by axial (c) and sagittal (d) computed tomography scans. (Figure 4b - courtesy of Dr. Aldo Stamm, Hospital Prof. Edmundo Vasconcelos, São Paulo, SP, Brazil)
The typical and rare posterior recess [6, 18] was present in one hemi-head only and in one of CT scan (Fig. 5).
When the presence of septa was analyzed only within the 334 cases of critical BESS, which effectively have clinical and surgical importance, the intersinus and accessory septa had the distribution shown in Table 2.
According to the subgroups described in this paper and their frequency, a pattern of BESS may be established, as shown in Fig. 2, in which the most common types, together with the intersinus septa and the fusion points in the posterior part of the sphenoidal bone, are illustrated.
Discussion
Apparently, the first report on the posterior expansion of the sphenoidal sinus was published by Zuckerkandl [1] in 1892, and this condition was later described by the classic authors as an anatomical variation [2, 5]. However, just five decades later, with the development of endoscopic techniques associated with endonasal surgery [18, 19], BESS is becoming an anatomical aspect of relevance in otolaryngology. The apparent lack of applicability led many authors to adopt different names for the same kind of expansion. Thus, the terms basilar or posterior prolongation [2, 3, 5, 13], occipital-sphenoidal sinus [4], posterior extension to the basilar portion [26, 27] and occipital recess [28] were widely employed in the specialized literature. However, in reports concerning lateral and anterior expansions of the sphenoidal sinus [6], BESS is only mentioned as a postsellar expansion, basilar extension, or basilar expansion.
In the present work, the term basilar expansion was adopted based on the developmental aspects of the paranasal sinuses originating from ostia that allow for aerial expansion through trabecular bone resorption. Furthermore, the following characteristics reinforce the present criteria: association with a thin clivus; proximity to the basilar region (also used to name the basilar region of the pons, the venous basilar plexus, and the basilar artery), and an expansion of the sphenoidal sinus posterior to the dorsum sellae based on a 90° angle with the planum sphenoidale. Although establishment of this angle was relevant in two of the present cases, the posterior wall of the sphenoidal sinus did not exceed this angle due to a vertical clivus. In these examples, the criterion of clivus thickness specifically prevailed. It must be emphasized that the angle with the planum sphenoidale is a criterion used in the present study in which the planum sphenoidale was considered to be a very reliable reference observed in the medial plane. Thus, the methodology used in this study may have led to the conclusion that BESS has a relatively high incidence, as it also includes the postsellar and posterior recesses [6].
Considering the different types of expansion of the sphenoidal sinus, even today, Cope’s classification [3] published in 1917 dividing this sinus into presphenoid, basisphenoid, and intermediate groups, is still relevant. This main criterion, based on ossification centers, was corroborated by Hammer and Rådberg in 1961 [14] and by Rhoton et al. in 1979 [29]. However, if the term occipitosphenoidal [4] previously used to refer to cases of posterior expansion of the sinus is accepted, data here presented may consider BESS as a normal anatomical feature. This is justified by the frequency and specific characteristics that exclude BESS as a simple sellar expansion [14].
BESS represents a feature of great surgical importance. Many complications may occur during the endoscopic approach via endonasal surgery, in which the form of BESS is critical. In fact, a previous paper reports fracture, vertigo, posterior headache, vomiting, and empyema in patients with sphenoidal sinus prolongations [2]. Recent reports of vasculitis of the basilar artery with ischemic infarction of the pons secondary to sphenoidal sinusitis [30], cases of spontaneous CSF fistula [31–33], and frequent exposure of the internal carotid arteries support this theory [34]. In addition, a thin clivus is a potentially weak region in cases of a skull-base fracture, a point susceptible indeed to traumatic CSF fistula, as seen in two cases in the present study.
Correlation between radiological images and anatomical specimens to study sphenoidal aeration was first performed in 1925 by Canuyt and Terracol [12]. Later, reports using planigraphy [14, 24, 35], a technique that avoids overlapping of surrounding structures out of the focal plane, improved the ability to evaluate the different types of sinus expansion. Although studies of this sphenoidal region using CT scans were performed (e.g., Mutlu [36]), the main interest was to detect the presence of and variations in septa or crests within the sinus.
In what is regarded as sinonasal septation, even Zuckerkandl (1892) [1] described a high frequency of these structures within the sphenoidal sinus. The present analysis allowed identification of three basic types [3, 35] that reveal the correlation between accessory septa and synchondrosis of the ossification centers, i.e., sites of high bone density, and consequent resistance at their junctions. Thus, the assumption raised by Peele in 1957 [37] describing the presence of accessory septa cannot be fully corroborated. Peele, besides describing the relationship of the septa with synchondrosis, considered these structures to be present in any sinonasal wall. In fact, the current specimens did exhibit a regular pattern regarding location of the septa in the posterior sinonasal wall. Further, this is true for the left and right carotic sulci, where accessory septa were observed in 59% of cases.
Our data are conflicting when the frequency of septa (43% in the current study) is compared with reports describing intersinus septa in up to 68% of cases [29] and those referring to attachment of septa to the clivus in 63.8% of specimens studied [36]. This is even more pronounced when compared with lower frequencies (27%) reported elsewhere [6].
On the other hand, there are reports of the incidence of accessory septa of 76% [6] and 69% [36]. These figures are quite different from those identified in the present study where only 27% of cases exhibited accessory septa. However, the specimens evaluated here concern only a single condition of the sphenoidal sinus, i.e., when BESS was present. However, we consider these findings accurate, as the great variability in septa may hinder the transsphenoidal approach to the pituitary gland [24], and this variability may currently be considered an important intraoperative parameter.
The importance of classifying BESS as bilateral, unilateral, or dominant lies in the fact that transsphenoidal surgical access becomes more difficult when the sphenoidal sinus is less developed. Critical BESS facilitates the approach to lesions located at the clivus or petrous apex. Thus, a panoramic endoscopic vision is directly related to the size of the sinus, and the subgroups classified as dominant, unilateral, and bilateral described in this study make the approach to the different parasphenoidal diseases easier.
In conclusion, results of the present study suggest that CT scans can be a very important virtual and anatomical methodology. As a specific example, pituitary adenomas investigated mainly by magnetic resonance imaging (MRI) [38] also need to be evaluated by CT scan for proper planning of transsphenoidal access. The high incidence of critical BESS described in this study supports this assumption.
References
Zuckerkandl E (1892) Normale und pathologische Anatomie der Nasenhöhle und ihrer pneumatischen Anhänge, 2nd ed. Wien-Leipzig, W. Braumueller
Sieur J, Jacob O (1901) Recherches anatomiques, cliniques et opératoires sur les fosses nasales et lueurs sinus, 1st ed. J. Rueff, Éditeur, Paris
Cope VZ (1917) The internal structure of the sphenoidal sinus. Jour Anat 51:127–136
Congdon ED (1920) The distribution and mode of origin of septa and walls of the sphenoidal sinus. The Anatomical Record 18(2):97–123
Testut L, Jacob O (1909) Traité d’anatomie topographique, 2nd ed. Octave Doin et Fils, Éditeurs, Paris
Elwany S, Yacout YM, Talaat M et al (1983) Surgical anatomy of the sphenoidal sinus. J Laryngol Otol 97:227–241
Catala M (2003) Développement embryonnaire du sphénoïde. J Neuroradiol 30:193–200
Fujioka M, Young LW (1978) The sphenoidal sinuses: radiographic patterns of normal development and abnormal findings in infants and children. Radiology 129:133–136
Yonetsu K, Watanabe M, Nakamura T (2000) Age related expansion and reduction in aeration of the sphenoidal sinus: volume assessment by helical CT scanning. Am J Neuroradiol 21:179–182
Testut L (1911) Traité d’anatomie humaine, 6th edn. Octave Doin et Fils, Éditeurs, Paris
Skillern RH (1920) The accessory sinuses of the nose, 2nd edn. J.B. Lippincott Company, Philadelphia
Canuyt G, Terracol J (1925) Le sinus sphénoïdal, 1st edn. Masson et Cie, Editeurs, Paris
Castro Lima O (1944) Seios paranasais e nervo óptico: contribuição ao estudo da neurite óptica retrobulbar rinogênica, 1st edn. Faculty of Medicine of Bahia, Salvador, BA
Hammer G, Rådberg C (1961) The sphenoidal sinus - an anatomical and roentgenologic study with reference to transsphenoid hypophysectomy. Acta Radiologica 56(6):401–422
Chiarugi G (1936) Instituzioni di anatomia dell’uomo, 4th ed. Società Editrice Libraria, Milano
Navarro JAC (2000) Surgical Anatomy of the Nose, Paranasal Sinuses, and Pterygopalatine Fossa. In: Stamm AC, Draf W (eds) Micro-endoscopic Surgery of the Paranasal Sinuses and the Skull Base. Springer, Berlin Heidelberg New York
Haetinger RG (2000) Imaging of the Nose and Paranasal Sinuses. In: Stamm AC, Draf W (eds) Micro-endoscopic Surgery of the Paranasal Sinuses and the Skull Base. Springer, Berlin Heidelberg New York
Heermann H (1958) Endonasal surgery with the use of the binocular Zeiss operating microscope. Arch Klin Exp Ohren Nasen Kehlkopfheilk 171:295–297
Messerklinger W (1978) Endoscopy of the Nose. Urban & Schwarzenberg, Baltimore-Munich
Navarro JAC (2001) The Nasal Cavity and Paranasal Sinuses - Surgical Anatomy, 1st edn. Springer, Verlag Berlin Heidelberg New York
Stamm AC, Pignatari S, Sebusiani BB, Galati MC, Mitsuda S, Haetinger RG (2002) Image-Guided Endoscopic Sinus and Skull Base Surgery. (Cirurgia Endoscópica Nasossinusal e da Base do Crânio Guiada por Computador) Revista Brasileira de Otorrinolaringologia 68:502–509
Stamm AC, Pignatari SSN (2005) Transnasal Endoscopic-Assisted Surgery of the Skull Base. In: Cummings C, Flint PN, Harker LA (eds) Otolaryngology and Head and Neck Surgery, Vol. IV, Elsevier/Mosby
Ferrier J-C, Klossek J-M (2003) Les mucocèles sphénoïdales. J Neuroradiol 30:219–223
Rothman SLG, Kier EL, Allen WE III (1976) The radiology of transsphenoidal hypophysectomy: a review of 100 cases. Am J Roentengenol 127(4):601–606
Katzenmeyer K, Bailey BJ (2000) Approaches to the Sphenoid. Ear Nose Throat J 70(7):438–440
Lang J (1989) Clinical anatomy of the nose, nasal cavity and paranasal sinuses. 1st edn. Thieme Medical Publishers, New York
Van Alyéa OE (1941) Sphenoidal sinus: anatomic study, with consideration of the clinical significance of the structural characteristics if the sphenoidal sinus. Arch Otolaryngology 2(8):225–253
Novosellac M, Pecina M, Nemanic D (1966) Recesus occipitalis sinus sphenoidalis. Rad Med Fak Zagreb 14:211–218
Rhoton AL, Hardy DG, Chambers SM (1979) Microsurgical anatomy and dissection of the sphenoid bone, cavernous sinus and sellar region. Surg Neurol 12:63–104
Sorimashi T, Kamada K, Ozawa T et al (2001) Basilar artery vasculitis secondary to sphenoidal sinusitis - case report. Neurol Med Chir (Tokyo) 41:454–457
Jenkins HA, Calcaterra TC (1977) Spontaneous cerebrospinal rhinorrhea from the sphenoidal sinus. Trans Am Acad Ophtalmol Otolaryngol 84(5):916–918
Coiteiro D, Távora L, Antunes JL (1995) Spontaneous cerebrospinal fluid fistula through the clivus: report of two cases. Neurosurgery 37(4):826–828
Stamm AC, Draf W (2000) Micro-endoscopic surgery of the paranasal sinuses and the skull base, 1st edn. Springer, Berlin Heidelberg New York
Jho HD, Carrau RL, McLaughlin ML, Somaza SC (1997) Endoscopic transsphenoidal ressection of a large chordoma in the posterior fossa. Acta Neurochir 139:343–348
Rothman SLG, Kier EL, Kirchner JE et al (1975) Preoperative laminographic evaluation of the sphenoidal sinus for transsphenoidal surgery. Laryngoscope 85:1986–1988
Mutlu C, Unlu HH, Goktan C et al (2001) Radiologic anatomy of the sphenoidal sinus for intranasal surgery. Rhinology 39(3):128–132
Peele JC (1957) Unusual anatomical variations of the sphenoidal sinuses. Laryngoscope 67:208–237
Bonneville JF, Bonneville F, Cattin F (2005) Magnetic resonance imaging of pituitary adenomas. Eur Radiol 15:543–548
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Haetinger, R.G., Navarro, J.A.C. & Liberti, E.A. Basilar expansion of the human sphenoidal sinus: an integrated anatomical and computerized tomography study. Eur Radiol 16, 2092–2099 (2006). https://doi.org/10.1007/s00330-006-0208-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-006-0208-3