Abstract
Aim of this study was to develop a time-efficient sequence protocol for a 1.0 T dedicated MR system to be used for whole-organ scoring of osteoarthritis (OA). Thirty-four knees were examined using a protocol that included fat suppressed fast spin echo proton density weighted sequences (PDFS) in three planes plus a coronal STIR sequence. Two radiologists scored each knee by consensus for five OA features. In separate sessions, all knees were scored using three different combinations of sequences: (1) all four sequences (reference protocol, 16 min 31 s scanning time), (2) three PDFS sequences without STIR (“No STIR”, 12 min 25 s scanning time) and (3) sagittal and axial PDFS sequences plus a coronal STIR sequence (“No PDFS”, 11 min 49 s scanning time). Agreement of the readings using both subsets of sequences compared to the reference protocol was evaluated using weighted kappa statistics. κ-coefficients showed good or excellent agreement for both sequence subsets in comparison to the reference protocol for all assessed features. κ-coefficients for No PDFS/No STIR: bone marrow abnormalities (0.74/0.67), subarticular cysts (0.84/0.63), marginal osteophytes (0.77/0.71), menisci (0.75/0.79), tibial cartilage (0.71/0.78). Optimization of sequence protocols consisting of three sequences results in time savings and cost efficiency in imaging of knee OA without loss of information over a more time consuming protocol.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Magnetic resonance imaging (MRI) has emerged as the method of choice for the assessment of many musculoskeletal disorders, including osteoarthritis (OA) of the knee joint. The technique allows an evaluation of the joint as a whole organ, and provides a much more detailed picture of the changes associated with OA than other techniques [1–4].
Dedicated low-field and recently intermediate-field MRI-systems have been developed as an alternative to high-field systems for cost-saving reasons as well as higher patient comfort and have been applied especially for the evaluation of musculoskeletal disorders including OA of the knee [5–8].
Recently developed standardized scoring methods for the assessment of knee OA allow the application of MRI to large-scale epidemiological studies [4]. To date studies evaluating OA on a dedicated intermediate-field MR system have not been performed.
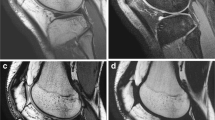
Different fast spin echo (FSE) sequences using frequency selective fat suppression techniques have proven to be a valid tool in MR imaging of cartilage as well as subchondral bone and other intrinsic soft tissue structures of the knee joint [9–11]. Due to superior contrast between cartilage and surrounding structures as well as excellent depiction of bone marrow edema-like lesions, fat suppressed sequences are also commonly employed for the assessment of knee OA [3]. In this study frequency selective fat suppression could be applied for proton density-weighted (PDw) sequences on an intermediate-field 1.0 T system. A shortcoming of dedicated low- and intermediate-field MR systems is the compromised peripheral field homogeneity. For this reason other fat suppression techniques such as the more robust STIR sequence may be added to achieve homogeneous fat suppression (Figs. 1 and 2). This leads to an increase in imaging time.
Bone marrow edema-like lesion in the medial tibial plateau. A Coronal PDFS image. High-intensity bone marrow abnormality (arrow) extends into an area of partial fat sat failure (arrowheads). Exact scoring concerning the size of the lesion is not possible. B Sagittal PDFS image shows the same impaired delineation of marrow abnormality and fat sat failure. C Coronal STIR image. True extent of lesion is shown (arrows)
Bone marrow abnormalities. A Coronal STIR sequence. Hyperintense marrow abnormalities are seen in the subspinous region, the medial tibial plateau, the medial femoral condyle and the medial aspect of the lateral femoral condyle adjacent to the trochlear groove (arrows). B Coronal PDFS sequence. An additional area of hyperintensity mimicking an edema-like lesion is shown in the region of the lateral tibial plateau (white arrow). Cause of this signal abnormality is an ill-defined area of peripheral fat suppression failure (black arrows). Note cartilage loss (grade-5 lesions) medial tibia and femur (arrowheads)
As imaging time is crucial in a routine clinical setting as well as in large epidemiological and clinical trials for reasons of cost efficiency and patient comfort, the development and application of the shortest possible sequence protocol is of paramount importance.
This study compared two different time-saving sequence protocols with a prior defined reference sequence set with the aim of developing a time-saving sequence protocol for the semiquantitative evaluation of knee OA on a dedicated intermediate-field MR system.
Materials and methods
Subjects
Thirty-four knees of 23 subjects with suspected or proven OA of the knee joint underwent MR imaging. The subjects were participants of the large epidemiological Multicenter Osteoarthritis Study—MOST. To be eligible for MOST, a subject must have either frequent knee symptoms (defined as pain, aching or stiffness in or around the knee on most days of the last 30 days reported at a telephone screening interview as well as at a clinic eligibility screen) or the subject must belong to a high risk group for the development of knee OA (obesity, prior knee injury or surgery). The MR exams of 34 knees selected for this study were randomly drawn from a larger database of 203 examinations (113 subjects).
Informed consent was obtained in all participants and the MOST protocol was approved by the institutional review boards at the two MOST clinical centers, the Universities of Iowa and Alabama, Birmingham. None of the participants had contraindications for MRI.
MR imaging
All MR examinations were performed on a dedicated extremity MRI system (OrthOne™, ONI, Wilmington, MA) working at 1.0 T using a superconductive magnet. Patients were imaged with a 180 mm inner diameter circumferential send–receive extremity coil. The protocol consisted of an axial proton-density weighted fat suppressed sequence [=PDFS] (TR 4,680 ms, TE 13 ms, 3-mm slice thickness, 0-mm interslice gap, 20 slices, 288×192 matrix, two NEX, 140 mm2 FOV, echo train length 8, 2 min 59 s scanning time), a sagittal PDFS sequence (TR 6,300 ms, TE 35 ms, 3-mm slice thickness, 0-mm interslice gap, 32 slices, 288×192 matrix, two NEX, 140 mm2 FOV, echo train length 8, 4 min 44 s scanning time), a coronal PDFS sequence (TR 5,050 ms, TE 35 ms, 3-mm slice thickness, 0-mm interslice gap, 28 slices, 288×192 matrix, two NEX, 140 mm2 FOV, echo train length 8, 4 min 42 s scanning time) and a corresponding coronal STIR sequence (TR 6,650 ms, TE 15 ms, TI 100 ms, 3-mm slice thickness, 0-mm interslice gap, 28 slices, 256×192 matrix, two NEX, 140 mm2 FOV, echo train length 8, 4 min 6 s scanning time).
The resulting images were downloaded onto a SUN workstation (Sun Microsystems, Inc., Santa Clara, CA) where they were presented with optimized window width/window level settings. The exams were read from screen without hardcopies.
Imaging evaluation
Readings
All of the MRI exams were read by two experienced musculoskeletal radiologists (F.R., A.G.) in consensus using three different protocols. One protocol included the axial PDFS, sagittal PDFS and coronal STIR sequence (=“No PDFS” sequence protocol with a total imaging time of 11 min 49 s). The second set included an axial PDFS, sagittal PDFS and a coronal PDFS sequence (=“No STIR” sequence set with a total of 12 min 25 s imaging time) and the last set included all four sequences (“Reference” or “All”-sequence protocol with 16 min 31 s total imaging time). The last set was defined as the standard of reference. As the readers were reading the same exams three times, for each reading the order of MR exams was randomly mixed. The readers were blinded to participant data such as name or date of exam. A time interval of 1 week between each reading increased the likelihood that readers would not remember specific MRI scoring.
OA features
Reading included semiquantitative analysis of several OA features that may be evaluated on coronal images: (1) bone marrow edema, (2) subarticular cysts, (3) marginal osteophytosis, (4) menisci, and (5) tibial cartilage morphology. A semiquantitative grading score for each individual feature was introduced.
Evaluated locations
Bone marrow edema-like lesions as well subarticular cysts were scored at 15 different locations (medial and lateral femur anterior, central and posterior, respectively, medial and lateral tibia anterior, central and posterior, respectively, plus the subspinous area as well as the medial and lateral patella) (Fig. 3). Marginal osteophytes were scored at four sites (medial and lateral femur, medial and lateral tibia). Meniscal lesions were scored at six different locations (medial and lateral meniscus, anterior central and posterior, respectively). Tibial cartilage morphology was scored at six different locations (medial and lateral tibia anterior, central and posterior, respectively).
Regional subdivision of the articular surfaces (adapted from [4]). Bone marrow edema-like lesions and subarticular cysts are scored at 15 different locations. The patella (left image) is divided into a medial (M) and lateral (L) compartment. The femur and tibia are also divided into a medial and lateral region (M and L on the right image). The letter S represents the tibial area beneath the tibial spines. A further subdivision was applied to the femoral and tibial surfaces into anterior (A), central (C) and posterior (P) regions (center image)
Grading system
For the evaluation of the different OA features, a modified whole organ-scoring system was applied [4]. A four-point grading score was used to describe the extent of bone marrow edema-like lesions and subarticular cysts (0=no lesion, 1=<25% of region, 2=25–50% of region, 3=>50% of region) (Fig. 4). Marginal osteophytes were evaluated with a seven-point grading scale (0=none, 1=equivocal finding, 2=small horizontal spur, 3=moderate horizontal or small curved spur, 4=large horizontal or moderate curved spur, 5=moderate-large curved spur, 6=large, exuberant spur). The menisci were graded on a five-point scale (0=intact, 1=minor radial or parrot-beak tear, 2=non-displaced tear or prior surgical repair, 3=displaced tear, partial maceration or partial resection, 4=complete maceration and destruction or complete resection). Tibial cartilage scoring consisted of six grades [0=normal thickness and signal, 1=solitary focal defect, 2=areas of partial-thickness loss with areas of preserved thickness, 3=diffuse (<75%) partial-thickness loss, 4=areas of full-thickness loss with areas of partial-thickness loss, 5=diffuse (>75%) full-thickness loss] (Fig. 5).
Scoring of subarticular marrow lesions (adapted from [4]). This score is based on the extent of regional marrow involvement by areas of free water signal with ill-defined (bone marrow edema) or well-defined (cysts) margins. (0=no marrow lesion, 1=<25% of region, 2=25–50% of region, 3=>50% of region)
Cartilage scoring (adapted from [4]). A six-point grading scheme was applied. Grade 0 represents the normal articular surface. Grade 1 describes a focal defect. Grades 2 to 5 describe diffuse partial or full-thickness cartilage loss
To determine the degree of agreement between the two sequence sets with only three sequences (No STIR and No PDFS) and the sequence set including all sequences (reference set), weighted kappa coefficients were calculated (using linear weights). A kappa value greater than zero was considered to indicate a positive correlation: 0.01–0.20 poor agreement, 0.21–0.40 fair agreement, 0.41–0.60 moderate agreement, 0.61–0.80 good or substantial agreement and 0.81–1.00 excellent or almost perfect agreement [12]. For each weighted kappa coefficient, 95% confidence intervals were calculated. Any kappa values for which the 95% confidence intervals did not overlap would therefore be statistically different at p<0.05.
Results
Bone marrow abnormalities (edema-like lesions)
Concerning bone marrow edema-like lesions, the weighted kappa coefficients for agreement between the No PDFS and the All-sequence set were 0.74 and 0.67 for the No STIR vs. the All-sequence set indicating good or substantial agreement for both sequence protocols in comparison to the reference standard (Fig. 6). Disagreement within one grade was found for 507 of 510 regions (=99.4%) for the No PDFS set and for 505 of 510 regions (=99.0%) for the No STIR protocol. In only three cases was there disagreement of two grades for the No PDFS protocol (=0.6%) and in five cases for the No STIR protocol (=1.0%) (Tables 1 and 2). Disagreement of three grades was not found in any case for both sequence protocols.
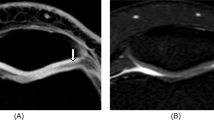
Osteophytosis, bone marrow abnormalities and cartilage loss. Changes are depicted with similar quality in the coronal images for A the PDFS sequence and B the STIR sequence. The sagittal PDFS sequence shows the anterior–posterior extent of the lesions (C). Note cartilage loss (=grade-5 lesion) of the medial femoral condyle as well as of the tibia (arrows). Osteophytes are seen on the sagittal image anteriorly and posteriorly as well as in the coronal images marginally (arrowheads)
Subarticular cysts
There were 19 cystic lesions detected with the reference protocol. Eighteen lesions were described using the No STIR-protocol, 19 lesions were found when the No PDFS sequence set was applied.
The weighted kappa coefficients for subarticular cysts were 0.84 and 0.63 for the No PDFS protocol and the No STIR protocol, respectively, indicating almost perfect and good agreement. Perfect agreement was shown for 503 (=98.6% for No PDFS) and 498 (=97.6% for No STIR) out of 510 evaluated regions. Disagreement within one grade was observed in seven of 510 regions (=1.4% for No PDFS) and in eight of 510 regions (=1.6% for No STIR), respectively. Disagreement of two grades was found in no case for the No PDFS protocol and in four cases for the No STIR protocol. In these four cases two subarticular cysts were scored as bone marrow edema-like lesions and two regions of edema-like changes were scored as cysts. In none of the cases was there disagreement of three grades.
Marginal osteophytes
Concerning marginal osteophytes the weighted kappa coefficients were 0.77 (No PDFS) and 0.71 (No STIR) indicating good agreement for both sequence protocols in comparison to the reference protocol (Fig. 6). Perfect agreement was observed in 118 of 136 locations (=86.8% for No PDFS) and 108 of 136, respectively (=79.4% for No STIR). Deviation of one or two grades was seen in 18 (No PDFS) and 25 cases (No STIR). Disagreement of more than two grades was found in three cases for the No PDFS protocol and in three cases for the No STIR protocol. In one case a grade-6 osteophyte was observed in the No PDFS protocol reading while the gold standard reading did not show an osteophyte at all. The explanation for this discrepant finding was that the observed structure was seen but graded as a large loose body with the All-sequence set (Tables 3 and 4).
Menisci
The weighted kappa coefficients for meniscal scoring were 0.75 (No PDFS) and 0.79 (No STIR) indicating good agreement for both sequence sets in comparison to the All-sequence protocol (Fig. 7). In 183 of 204 possible locations perfect agreement was observed for the No PDFS sequence protocol (=89.7%) and in 188 of 204 for the No STIR protocol (=92.2%). Deviation of one grade was seen in 13/204 (=6.4% for NO PDFS) and in nine of 204 locations for the No STIR protocol (=4.4%). Disagreement of two grades or more was observed for 8/204 (=3.9% for No PDFS) and 7/204 (=3.4% for No STIR), respectively (Tables 5 and 6).
Tibial cartilage
The weighted kappa coefficients for tibial cartilage morphology indicated good agreement with the reference sequence set for both protocols (0.71 for the No PDFS protocol and 0.78 for the No STIR protocol). Of 204 possible locations, 156 were scored in perfect agreement for the No PDFS protocol (=76.5%) and 170 of 204 for the No STIR protocol (=83.3%). Of 204 locations, 11 (=5.4% for No PDFS) and ten (=4.9% for No STIR) were scored within one grade deviation. Thirty-seven locations showed disagreement of two or more grades for the No PDFS protocol (=18.1%) and 24 locations for the No STIR protocol (=11.8%) (Tables 7 and 8). Most cases of disagreement were found for grade-2 lesions. However, no particular direction of disagreement was observed. Cases of normal cartilage were scored as grade-2 lesions and vice versa. Examples of severe cartilage loss (grade-5 lesions) are shown in Figs. 2 and 6.
Overall agreement in all features
Weighted kappa coefficients and 95% confidence intervals for the agreement of both sequence protocols with the reference sequence set are presented in Table 9. Since the 95% confidence intervals of the two kappas of each analyzed OA feature overlap, there is no significant difference between the kappas of each analyzed OA feature.
Discussion
We performed this study to develop an optimized sequence protocol and reduce scanning time without losing relevant information about the different features of OA. In evaluating two abbreviated protocols, we found that with both sets of abbreviated sequences, compared to the prior defined reference sequence set, knee findings were, in general, visible without loss of information.
A newly introduced intermediate-field dedicated MR system was used in this study to evaluate OA of the knee. As frequency selective fat suppression is not possible on low-field dedicated MR systems, other techniques such as the STIR sequence or three-point Dixon water-fat separation have to be employed for fat suppression [13, 14]. For 1.0 T extremity MRI systems, frequency selective fat suppression is feasible and may be applied for superior image contrast of most features evaluated in OA of the knee joint including the articular cartilage [3, 10, 15].
To our knowledge there is no literature available on frequency selective fat suppression for the evaluation of OA on dedicated MR systems. We found that due to peripheral partial fat saturation failure and field inhomogeneities, delineation of bone marrow edema-like changes is often compromised in a sequence protocol including frequency selective fat suppressed fast spine echo sequences in three planes (Figs. 1 and 2). An additional STIR sequence shows bone marrow edema-like changes without compromise but leads to an increase in imaging time.
Both evaluated protocols differed by a coronal sequence. The coronal plane is commonly used in OA scoring for the assessment of collateral ligaments and marginal osteophytes as well as an additional evaluation tool for meniscal scoring [4]. Bone marrow abnormalities and subarticular cysts especially on the lateral and medial aspects of the knee are also evaluated on the coronal plane. Semiquantitative tibial cartilage assessment as well as volumetric quantification have also been performed from coronal images [4, 16].
For assessment of the different OA features at different locations, the readers instead of comparing the two different sequences directly to each other employed all available sequences, as is the case in a routine clinical setting.
Bone marrow abnormalities are a common feature of OA of the knee. Agreement for both optimized sequence protocols was good when compared to the reference protocol. A discrete superiority in the agreement level could be shown for the No PDFS sequence protocol when compared to the No STIR protocol. An explanation for this is the possibly impaired differentiation of areas of bone marrow abnormalities and local fat suppression failure with the PDFS pulse sequences. This might also be the case for the evaluation of subarticular cysts as these hyperintense abnormalities on fat suppressed images are degraded in a similar fashion as bone marrow lesions by fat saturation failure.
Marginal osteophytes, which are evaluated on coronal sequences, are well delineated by MRI. Concerning marginal osteophytosis, our results showed good agreement for both sequence protocols with kappa coefficients of 0.77 (No PDFS) and 0.71 (No STIR) suggesting a slight superiority of the No PDFS set for osteophyte scoring.
Most meniscal tears are assessed on sagittal images but a small percentage may only be seen on coronal images [4] (Fig. 7). For meniscal evaluation both planes were used in our study. The kappa coefficients for both protocols showed good agreement to the All-sequence protocol (0.75 for No PDFS and 0.79 for No STIR). There were a relatively high number of disagreements of two or more grades for both sequences in comparison to the gold standard for both optimized sequence protocols. Meniscal subluxations and the expanded five-point grading scale we used may have contributed to these disagreements.
For tibial cartilage scoring good agreement was shown for both sequence protocols. The kappa coefficient for the No STIR protocol was somewhat higher (0.78) than for the No PDFS protocol (0.71) indicating slight superiority of the former. Most cases of disagreement were found for grade-2 lesions. Normal cartilage and areas of partial cartilage thickness loss could not always be differentiated. This may be explained by the variability of normal cartilage thickness and is a reflection of the difficulty to diagnose partial thickness loss by MRI. In our study design that employed all available sequences for tibial cartilage scoring, no advantage of the No STIR protocol over the No PDFS protocol could be shown.
It is possible that researchers and clinicians may be willing to obtain all four pulse sequences in the evaluation of the knee. However, total scanning time using these four sequences was 16 min 31 s in comparison to 11 min 49 s (No PDFS) or 12 min 25 s (No STIR), which will be of relevance in a large epidemiological trial of several thousand participants. This does not include planning of the sequence, which has to be added to the total time the patient will be occupying the scanning system.
In summary, the results of this study suggest that both evaluated sequence protocols show good agreement with the more time-consuming reference protocol, which resulted in time savings of 4 min 42 s (No STIR) or 4 min 6 s (No PDFS). Increasing experience with this intermediate-field extremity MR system and future development of additional pulse sequences will show if other sequence combinations may be more suitable for semiquantitative assessment of OA. In comparison to fat suppressed FSE sequences, the STIR sequence is known for its robustness concerning field homogeneity as well as fat suppression. Superiority was shown for the No PDFS protocol in the evaluation of marrow abnormalities, cysts and osteophytes as well as being the faster sequence set, while the No STIR protocol showed superior results for the evaluation of the menisci and tibial cartilage.
References
Peterfy CG (1998) Magnetic resonance imaging. In: Brandt KD, Doherty M, Lohmander S (eds) Osteoarthritis. Oxford University Press, New York, pp 473–494
Peterfy CG (2002) Imaging of the disease process. Curr Opin Rheumatol 14:590–596
Guermazi A, Zaim S, Taouli B, Miaux Y, Peterfy CG, Genant HK (2003) MR findings in knee osteoarthritis. Eur Radiol 13:1370–1386
Peterfy CG, Guermazi A, Zaim S, Tirman PFJ, Miaux Y, White D, Kothari M, Lu Y, Fye K, Zhao S, Genant HK (2004) Whole-Organ Magnetic Resonance Imaging Score (WORMS) of the knee in osteoarthritis. Osteoarthr Cartil 12:177–190
Masciocchi C, Barile A, Satragno L (2000) Musculoskeletal MRI: dedicated systems. Eur Radiol 10:250–255
Peterfy CG, Roberts T, Genant HK (1998) Dedicated extremity MR imaging: an emerging technology. Magn Reson Imaging Clin N Am 6:849–870
Pessis E, Drape JL, Ravaud P, Chevrot A, Dougados M, Ayral X (2003) Assessment of progression in knee osteoarthritis: results of a 1 year study comparing arthroscopy and MRI. Osteoarthr Cartil 11:361–369
Drape JL, Pessis E, Auleley GR, Chevrot A, Dougados M, Ayral X (1998) Quantitative MR imaging evaluation of chondropathy in osteoarthritic knees. Radiology 208:49–55
Bredella MA, Tirman PF, Peterfy CG, Zarlingo M, Feller JF, Bost FW, Belzer JP, Wischer TK, Genant HK (1999) Accuracy of T2-weighted fast spin-echo MR imaging with fat saturation in detecting cartilage defects in the knee: comparison with arthroscopy in 130 patients. Am J Roentgenol 172:1073–1080
Mohr A (2003) The value of water-excitation 3D FLASH and fat-saturated PDw TSE MR imaging for detecting and grading articular cartilage lesions of the knee. Skelet Radiol 32:396–402
Recht MP, Kramer J, Marcelis S, Pathria MN, Trudell D, Haghighi P, Sartoris DJ, Resnick D (1993) Abnormalities of articular cartilage in the knee: analysis of available MR techniques. Radiology 187:473–478
Brennan P, Silman A (1992) Statistical methods for assessing observer variability in clinical measures. BMJ 304:1491–1494
Wohlgemuth WA, Roemer FW, Bohndorf K (2002) Short tau inversion recovery and three-point Dixon water-fat separation sequences in acute traumatic bone fractures at open 0.35 Tesla MRI. Skelet Radiol 31:343–348
Delfaut EM, Beltran J, Johnson G, Rousseau J, Marchandise X, Cotten A (1999) Fat suppression in MR imaging: techniques and pitfalls. Radiographics 19:373–382
Mohr A, Roemer FW, Genant HK, Liess C (2003) Using fat-saturated proton density-weighted MR imaging to evaluate articular cartilage. Am J Roentgenol 181:280–281
Burgkart R, Glaser C, Hyhlik-Durr A, Englmeier KH, Reiser M, Eckstein F (2001) Magnetic resonance imaging-based assessment of cartilage loss in severe osteoarthritis: accuracy, precision, and diagnostic value. Arthritis Rheum 44:2072–2077
Acknowledgements
The Multicenter Osteoarthritis Study (MOST) is a 7-year cooperative epidemiological study of knee osteoarthritis funded by the National Institute on Aging (NIA) within the National Institutes of Health (NIH).
NIA grant numbers: U01 AG18820, U01 AG19069, U01 AG18832, U01 AG18947.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Roemer, F.W., Guermazi, A., Lynch, J.A. et al. Short tau inversion recovery and proton density-weighted fat suppressed sequences for the evaluation of osteoarthritis of the knee with a 1.0 T dedicated extremity MRI: development of a time-efficient sequence protocol. Eur Radiol 15, 978–987 (2005). https://doi.org/10.1007/s00330-004-2608-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-004-2608-6