Abstract
Objective
To evaluate the diagnostic accuracy of water-excitation (WE) 3D FLASH and fat-saturated (FS) proton density-weighted (PDw) TSE MR imaging for detecting, grading, and sizing articular cartilage lesions of the knee.
Design and patients
A total of 26 patients underwent MR imaging prior to arthroscopy with the following sequences: (1) WE 3D FLASH: 28/11 ms, scan time: 4 min 58 s, flip angle: 40°; (2) FS PDw TSE: 3433/15 ms, scan time: 6 min 15 s, flip angle: 180°. Grade and size of the detected lesions were quantified and compared with the results of arthroscopy for each compartment.
Results
The sensitivity, specificity, positive and negative predictive values, and accuracy for detecting cartilage lesions were 46%, 92%, 81%, 71% and 74% for WE 3D FLASH and 91%, 98%, 96%, 94% and 95% for FS PDw TSE MR imaging. WE 3D FLASH correlated significantly with arthroscopy for grading on the patella (P<0.0001) and the femoral trochlea (P=0.02) and for sizing on the femoral trochlea (P=0.03). FS PDw correlated significantly (P<0.0001) with arthroscopy for grading and sizing on all compartments.
Conclusion
FS PDw TSE is an accurate method for detecting, grading and sizing articular cartilage lesions of the knee and yielded superior results relative to WE 3D FLASH MR imaging.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
With the development of new options for the treatment of hyaline cartilage lesions, it has become increasingly important to make the diagnosis early, accurately, and non-invasively [1, 2, 3]. MR imaging has been accepted as the best non-invasive modality for the analysis of articular cartilage and has become an essential tool for pre- and postoperative evaluation [2, 3, 4, 5, 6, 7, 8, 9]. However, the sequence that is best suited for the detection of chondral abnormalities is still under debate.
Recently, rapid water-excitation (WE) three-dimensional (3D) fast low angle shot (FLASH) sequences have been successfully used to quantify cartilage thickness and volume [10, 11, 12, 13]. To our knowledge, the ability of a WE 3D FLASH sequence to image, grade, and size cartilage lesions has not been evaluated in a systematic study.
Proton density-weighted (PDw) sequences have been successfully used for the detection of cartilage lesions of the knee [4, 6, 14], but only limited information about the combination with fat saturation (FS), which might further improve the detection rate, is available.
The purpose of this retrospective study was to compare the value of WE 3D FLASH and FS PDw TSE MR imaging to detect, grade, and size cartilage lesions of the knee with arthroscopy as the standard of reference.
Materials and methods
A total of 26 knees from 26 patients (mean age 37±14 years, range 21–56 years; 14 men, 12 women) with suspected internal derangements but without a history of acute trauma were included in this retrospective study. The patients were included when no contraindication for MR imaging was present, after informed consent was obtained and the local ethics committee approved the study. MR imaging of the knee was performed within the 2 months prior to arthroscopy (mean 23 days, median 20 days).
MR imaging was done on a 1.5 T MR scanner (Magnetom Vision, Siemens Medical Systems, Erlangen, Germany; gradient strength 25mT/m) using a dedicated knee coil. The protocol included, in the transverse and sagittal planes: (1) WE 3D FLASH: 28/11 ms, flip angle 40°, number of excitations 1, scan time 4 min 58 s; (2) FS PDw TSE: 3433/15 ms, flip angle 180°, number of excitations 3, scan time 6 min 15 s. The echo train length was 7, echo spacing was 15 ms. The following parameters were the same for both sequences: slice thickness 2 mm, no interslice gap, slab thickness 92 mm, FOV 145×145 mm, and matrix 256×256. The MR images were transferred to a workstation for cartilage lesion sizing and grading, and analyzed by consensus by two experienced musculoskeletal radiologists. In a random order the images were evaluated in a session for each sequence starting with WE 3D FLASH followed by FS PDw TSE 20 days later. The readers were masked to the results of arthroscopy, all clinical data, the other sequence session and the other sequences of the knee MR imaging protocol. Optimization of windowing and leveling were done individually and depending on the case for optimal image display, as is done in clinical routine. The contrast-to-noise ratios (CNRs) of cartilage versus fluid and cartilage versus subchondral bone were calculated according to the formula: CNR=(Scartilage−Sother)/SDair. Therefore the signal intensities (S) and standard deviations (SD) of cartilage, air, fluid, and bone were determined retrospectively in 10 randomly chosen patients by averaging regions of interest (ROIs) over areas that were arthroscopically proven normal. The readers defined the location and size of three ROIs, which were placed within the cartilage and the adjacent subchondral bone on each lateral patellar facet, lateral femoral condyle and lateral tibial plateau. Background measurements were obtained from one "air" ROI. Fluid signal was obtained from one area that demonstrated joint fluid. The diameter of the round ROIs was slightly smaller than the cartilage thickness, 19.6 mm2 for subchondral bone, and as large as possible for joint fluid and background [4].
Arthroscopy was performed by one experienced orthopedic surgeon who was informed only of the location, but not the size or grade, of the cartilage lesions as detected by the conventional clinical MR imaging protocol. Each knee compartment was inspected thoroughly and the detected cartilage lesions were sized and graded using the hook length of the probe as the reference.
In all patients, the following cartilage surfaces of the knee were evaluated with both MR imaging and arthroscopy: (1) patellar facets, (2) femoral trochlea, (3) medial femoral condyle, (4) lateral femoral condyle, (5) medial tibial plateau, and (6) lateral tibial plateau.
The cartilage lesions, as detected by MR imaging and arthroscopy, were graded according to the modified classification of Noyes and Stabler [15]: grade 0, arthroscopy and MR imaging: cartilage intact; grade 1, arthroscopy: cartilage softened but intact cartilage surface; MR imaging: abnormal internal signal intensity (1a, mild; 1b, severe); grade 2, arthroscopy and MR imaging: partial-thickness cartilage lesion (2a<50%, 2b>50%); grade 3, arthroscopy and MR imaging: cartilage completely denuded with exposure of bone (3a, without bone erosion; 3b, with bone erosion). The most advanced stage of each cartilage lesion defined the grade of the entire lesion. The size of the lesions was quantified for both MR imaging and arthroscopy as the product of the maximum diameter of the lesions and a second measurement perpendicular to the maximum diameter.
The statistical analysis was performed with JMP 4.0 software (SAS Institute, Cary, NC, USA) and included calculation of the sensitivities, specificities, positive predictive values, negative predictive values, and accuracies. Additionally the correlation of lesion grading (nonparametric Kendall-Tau-b test) and sizing (nonparametric Spearman rank test) between arthroscopy as the standard of reference and the MR imaging sequences was performed for each compartment. A P value of less than 0.05 indicated significance.
Results
All 156 articular surfaces of 26 knees were assessed with both arthroscopy and MR imaging. The results of lesion grading and the correlations of lesion grading and sizing between arthroscopy and the two MR sequences are given in Tables 1, 2, 3.
On arthroscopy 92 articular surfaces were intact; of the 64 lesions six were graded as stage 1a, four as 1b, eight as 2a, 33 as 2b, 12 as 3a, and one as 3b. The mean lesion size was 172±112 mm2 (range 50–600 mm2).
The mean CNRs and SDs for WE 3D FLASH and FS PDw TSE MR imaging for cartilage versus bone were 29.1±8.8 and 21.7±4.0 respectively, and 21.9±12.1 and 26.1±4.5 respectively for cartilage versus fluid.
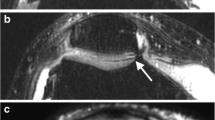
On WE 3D FLASH MR imaging normal cartilage appeared with high signal and good contrast to synovial fluid and other surrounding structures, especially subchondral bone (Fig. 1). Thirty true-positive, 34 false-negative (6 grade 1a, 4 grade 1b, 4 grade 2a, 13 grade 2b, 6 grade 3a, 1 grade 3b), 85 true-negative, and seven false-positive findings resulted in a sensitivity, specificity, positive and negative predictive value, and accuracy of 46%, 92%, 81%, 71%, and 74%, respectively. Significant correlations between WE 3D FLASH and arthroscopy for lesion grading were found on the patella and femoral trochlea and for lesion sizing on the femoral trochlea (Tables 2, 3).
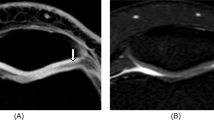
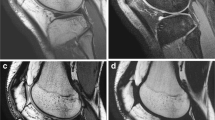
On FS PDw TSE MR imaging, intact cartilage appeared with low to intermediate signal (Fig. 1). High signal intensity of joint fluid and cartilage edema assisted in the visualization of cartilage contour irregularities and internal derangement (Fig. 2, 3, 4). Fifty-eight findings were true-positive, six false-negative (3 grade 1a, 1 grade 1b, 1 grade 2a, 1 grade 2b), two false-positive, and 90 true-negative (Table 1). Sensitivity, specificity, positive predictive value, negative predictive value, and accuracy were 91%, 98%, 96%, 94%, and 95%, respectively. The correlation between arthroscopy and FS PDw TSE for grading and sizing cartilage lesions was significant in all compartments (Tables 2, 3).
A 54-year-old woman with an arthroscopically proven grade 1b lesion of the lateral patellar facet in the transverse plane. No distinct signal alterations or surface irregularities are visible with WE 3D FLASH (A) MR imaging. Note the area of increased internal cartilage signal (arrow) on FS PDw TSE (B). A WE 3D FLASH: 28/11 ms, flip angle 40°. B FS PDw TSE: 3433/15 ms, flip angle 180°
A 32-year-old woman with an arthroscopically proven grade 2b lesion on the medial patellar facet (arrows) in the transverse plane. On WE 3D FLASH (A) the lesion was graded as 2a. The lesion is correctly graded on FS PDw TSE (B) MR imaging. Note that on FS PDw TSE MR imaging the surface irregularities can be visualized better due to the arthrographic effect of the bright joint fluid. A WE 3D FLASH: 28/11 ms, flip angle 40°. B FS PDw TSE: 3433/15 ms, flip angle 180°
A 44-year-old woman with an arthroscopically proven grade 3a lesion on the patella and a grade 3b lesion on the trochlear groove in the sagittal plane (arrows). With WE 3D FLASH (A) the patellar lesion was underestimated as grade 2b. Correct grading was performed on FS PDw TSE (B) MR imaging. Note that both lesions are better depicted on FS PDw TSE MR imaging due to the arthrographic effect and the signal changes due to cartilage and bone edema. A WE 3D FLASH: 28/11 ms, flip angle 40°. B FS PDw TSE: 3433/15 ms, flip angle 180°
Discussion
Water-excitation 3D FLASH MR imaging is a relatively new means of analyzing articular cartilage. The majority of reports refer to the analysis of cartilage volume, thickness, and 3D analysis [10, 11, 12, 13]. The sequence has been recommended as an alternative time-saving method for detecting cartilage lesions [1] but to our knowledge quantitative data about grading and sizing based on a systematic study are not available. The principle is the selective excitation of non-fat-bound protons, which obviates the time-consuming spectral fat saturation pre-pulse. The major advantages of the sequence are: relatively short acquisition time, high-resolution images, prevention of chemical shift artifacts, possibility of contrast enhancement, and acquisition of a volumetric data set for reliable 2D and 3D quantitative analysis of cartilage, e.g., volume and thickness measurements [1, 12, 13]. Despite these advantages the performance of water-excitation MR imaging was disappointing for detecting, grading, and sizing of articular cartilage lesions in the present study. Although highly specific, only a weak sensitivity for the detection of cartilage lesions was found. Correlations with arthroscopy were significant only for lesion grading on the patella (P<0.0001) and the femoral trochlea (P=0.02) and for sizing on the femoral trochlea (P=0.03). CNRs for cartilage versus bone and fluid were high, which explains the suitability of this sequence for 3D volumetric evaluations of cartilage. Although cartilage is displayed with high signal intensity, signal changes due to cartilage derangement are not as clearly visible as on FS PDw TSE. Therefore, low-grade lesions without surface fibrillation especially may not be detected. Other disadvantages are sensitivity to susceptibility artifacts and truncation artifacts [1, 6, 16, 17, 18]. These factors can explain why lesions were missed or misinterpreted.
MR imaging with FS PDw TSE was highly specific and sensitive for the detection of cartilage lesions and correlated significantly with arthroscopy for grading and sizing in each compartment. Intact cartilage appeared with a low to intermediate signal. FS PDw TSE MR imaging has several advantages. It provides information on cartilage water content and therefore edema assists in the visualization of cartilage subsurface derangement [19]. The arthrographic effect of the joint fluid assists in the visualization of cartilage surface irregularities, which may obviate the need for MR arthrography. Furthermore, static field inhomogeneity is compensated by the refocusing effect of the 180º flip angle [1, 20, 21]. These factors can explain why cartilage derangement is better visible on FS PDw TSE MR imaging. Additionally the technique is well suited for imaging of other joint structures, which allows a sufficient evaluation of the entire joint in one step [6, 18, 22, 23, 24]. Our results compare well with those of Potter et al. [6] who showed, in 88 patients, a sensitivity, specificity, and accuracy of 87%, 94%, and 92%, respectively, for a fat-saturated PDw spin echo sequence . In 27 patients Gagliardi et al. [21] found a sensitivity, specificity, and accuracy of up to 75%, 100%, and 98% respectively, for the detection of patellar cartilage lesions. The lower sensitivity in this study may be explained by the fact that no fat saturation was used. The latter, however, is often included in clinical imaging protocols to expand the dynamic range of MR imaging for subtle cartilage variations, to intensify cartilage signal, and to reduce chemical shift artifacts [1, 14, 16]. Bachmann et al. [4] used a PDw sequence and reported in 50 knees a remarkably lower sensitivity and accuracy of 45% and 64%, respectively, but a comparable specificity of 98%. Recht et al. [14] reported worse results with a sensitivity, specificity, and accuracy of 25%, 95%, and 70%, respectively. The discrepancy between these two studies and those of Potter et al. [6], Gagliardi et al. [21] and the present study may be explained by the use of cadaver knees with MR imaging after freezing, storing, and thawing, which may affect signal intensities [25]. These procedures may cause diffusion effects of articular fluid or intra-cartilaginous edema in addition to post mortem changes. Additionally neither study included fat saturation, which could improve the detectability of cartilage lesions. Furthermore, Gagliardi et al. [21], Bachmann et al. [4], and Recht et al. [14] used either a smaller matrix, resulting in lower spatial resolution, only the transverse imaging plane, or a higher slice thickness in their imaging protocol, which may lower the detection rate of cartilage defects. Disadvantages of the technique can be magic angle artifact, the 2D acquisition principle and a lower contrast between cartilage and subchondral bone, which make it less suitable for cartilage thickness and volume measurements [8, 9, 10].
There are several limitations to this study. First, and most important, is the relatively small number of patients, which is, if six different cartilage compartments and six-fold graduation are used, quite low. Therefore reasonable tests for significant differences between the sequences, or the analysis of interobserver differences with independent readers, were not possible. The value of statistical analysis is limited in compartments with a small number of lesions such as the lateral femoral condyle (with only five lesions) or the small number of grade 1a and 1b lesions. Additionally the medial and lateral patellar surfaces were graded as a single compartment although they interact with different compartments and therefore different mechanical stresses. A separation into a medial and lateral patellar compartment may therefore yield, to some extent, different results. Secondly, arthroscopy is not a perfect gold standard and its potential accuracy in the evaluation of cartilaginous disorders has been questioned several times by other authors [2, 4, 17, 22]. In particular, lesions demonstrating cartilage derangement without surface irritation have a strong risk of being graded as false-negative on arthroscopy causing a false-positive finding on MR imaging when compared with arthroscopy. Furthermore, with arthroscopy there are blind spots in the joint that may be difficult to assess. In this context, it must be considered that there was a certain degree of bias in the study as information on the location of cartilage lesions was available to the surgeon at the time of arthroscopy.
We conclude that FS PDw TSE is well suited for revealing, grading, and sizing articular cartilage lesions of the knee and yielded superior results in comparison with WE 3D FLASH MR imaging.
References
Disler DG, Recht MP, McCauley TR. MR imaging of articular cartilage. Skeletal Radiol 2000; 29:367–377.
Bredella MA, Tirman PF, Peterfy CG, et al. Accuracy of T2-weighted fast spin-echo MR imaging with fat saturation in detecting cartilage defects in the knee: comparison with arthroscopy in 130 patients. AJR Am J Roentgenol 1999; 172:1073–1080.
McCauley TR, Disler DG. Magnetic resonance imaging of articular cartilage of the knee. J Am Acad Orthop Surg 2001; 9:2-8.
Bachmann G, Heinrichs C, Jurgensen I, Rominger M, Scheiter A, Rau WS. Comparison of different MRT techniques in the diagnosis of degenerative cartilage diseases. In vitro study of 50 joint specimens of the knee at T1.5. Rofo 1997; 166:429–436.
Brossmann J, Frank LR, Pauly JM, et al. Short echo time projection reconstruction MR imaging of cartilage: comparison with fat-suppressed spoiled GRASS and magnetization transfer contrast MR imaging. Radiology 1997; 203:501–507.
Potter HG, Linklater JM, Allen AA, Hannafin JA, Haas SB. Magnetic resonance imaging of articular cartilage in the knee. An evaluation with use of fast-spin-echo imaging [see comments]. J Bone Joint Surg Am 1998; 80:1276–1284.
Rand T, Brossmann J, Pedowitz R, Ahn JM, Haghigi P, Resnick D. Analysis of patellar cartilage. Comparison of conventional MR imaging and MR and CT arthrography in cadavers. Acta Radiol 2000; 41:492–497.
Murphy BJ. Evaluation of grades 3 and 4 chondromalacia of the knee using T2*-weighted 3D gradient-echo articular cartilage imaging. Skeletal Radiol 2001; 30:305–311.
Ahn JM, Kwak SM, Kang HS, et al. Evaluation of patellar cartilage in cadavers with a low-field-strength extremity-only magnet: comparison of MR imaging sequences, with macroscopic findings as the standard. Radiology 1998; 208:57–62.
Graichen H, Springer V, Flaman T, et al. Validation of high-resolution water-excitation magnetic resonance imaging for quantitative assessment of thin cartilage layers. Osteoarthritis Cartilage 2000; 8:106–114.
Hyhlik-Durr A, Faber S, Burgkart R, et al. Precision of tibial cartilage morphometry with a coronal water-excitation MR sequence. Eur Radiol 2000; 10:297–303.
Springer V, Graichen H, Stammberger T, Englmeier KH, Reiser M, Eckstein F. Noninvasive analysis of cartilage volume and cartilage thickness in the human elbow joint using MRI. Anat Anz 1998; 180:331–338.
Heudorfer L, Hohe J, Faber S, Englmeier KH, Reiser M, Eckstein F. [Precision MRI-based joint surface and cartilage density analysis of the knee joint using rapid water-excitation sequence and semi-automatic segmentation algorithm]. Biomed Tech 2000; 45:304-310.
Recht MP, Kramer J, Marcelis S, et al. Abnormalities of articular cartilage in the knee: analysis of available MR techniques. Radiology 1993; 187:473–478.
Noyes FR, Stabler CL. A system for grading articular cartilage lesions at arthroscopy. Am J Sports Med 1989; 17:505–513.
Peh WC, Chan JH. Artifacts in musculoskeletal magnetic resonance imaging: identification and correction. Skeletal Radiol 2001; 30:179–191.
Disler DG, McCauley TR, Kelman CG, et al. Fat-suppressed three-dimensional spoiled gradient-echo MR imaging of hyaline cartilage defects in the knee: comparison with standard MR imaging and arthroscopy. AJR Am J Roentgenol 1996; 167:127–132.
Potter HG, Rodeo SA, Wickiewicz TL, Warren RF. MR imaging of meniscal allografts: correlation with clinical and arthroscopic outcomes. Radiology 1996; 198:509–514.
Gray ML, Burstein D, Xia Y. Biochemical (and functional) imaging of articular cartilage. Semin Musculoskelet Radiol 2001; 5:329–343.
Hohe J, Faber S, Stammberger T, Reiser M, Englmeier KH, Eckstein F. A technique for 3D in vivo quantification of proton density and magnetization transfer coefficients of knee joint cartilage. Osteoarthritis Cartilage 2000; 8:426–433.
Gagliardi JA, Chung EM, Chandnani VP, et al. Detection and staging of chondromalacia patellae: relative efficacies of conventional MR imaging, MR arthrography, and CT arthrography. AJR Am J Roentgenol 1994; 163:629–636.
Bredella MA, Tirman PF, Wischer TK, Belzer J, Taylor A, Genant HK. Reactive synovitis of the knee joint: MR imaging appearance with arthroscopic correlation. Skeletal Radiol 2000; 29:577–582.
Lee JH, Singh TT, Bolton G. Axial fat-saturated FSE imaging of knee: appearance of meniscal tears. Skeletal Radiol 2002; 31:384–395.
Jansson KA, Karjalainen PT, Harilainen A, et al. MRI of anterior cruciate ligament repair with patellar and hamstring tendon autografts. Skeletal Radiol 2001; 30:8-14.
Recht M, Bobic V, Burstein D, et al. Magnetic resonance imaging of articular cartilage. Clin Orthop 2001: Suppl 391:379–396.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mohr, A. The value of water-excitation 3D FLASH and fat-saturated PDw TSE MR imaging for detecting and grading articular cartilage lesions of the knee. Skeletal Radiol 32, 396–402 (2003). https://doi.org/10.1007/s00256-003-0635-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-003-0635-z