Abstract
The purpose of our study was to assess prospectively the value of MRI in characterization of soft tissue tumors (STT) and soft tissue tumor-like lesions in a multi-institutional setting by a group of experts. The material consisted of 548 untreated and proven STT or tumor-like lesions originating from a multi-institutional database of STT in which 930 consecutive patients with STT examined by MRI were registered between 1 January 2001 and 28 April 2003. Based on MRI findings, a suitably ordered differential diagnosis was made in consensus by two radiologists (J.L.M.A.G and A.M.D.S). MRI diagnoses were compared with histology results (455 cases, 83%) and/or 6-month follow-up (93 cases, 17%) as reference standards. The correlation between the MRI and histological diagnosis and between the radiological and histological phenotype were statistically determined. One hundred twenty-three patients presented with a malignant STT; 425 patients presented with a benign one. Concerning differentiation between malignant and benign lesions (dignity), a sensitivity of 93%, specificity of 82%, negative predictive value (NPV) of 98% and positive predictive value (PPV) of 60% with accuracy of 85% were obtained. Concerning phenotype characterization, if only the first MRI diagnosis was taken into account, a sensitivity of 67%, specificity of 98%, NPV of 98%, PPV of 70% and accuracy of 96% were obtained. For benign lesions, sensitivity of 75%, specificity of 98%, NPV of 98%, PPV of 76% and accuracy of 97% were obtained. The phenotype’s definition of malignant STT had a sensitivity of 37%, a specificity of 96%, NPV of 96%, PPV of 40% and an accuracy of 92%. A correct diagnosis compared with histological assessment was proposed in 227(50%) of the 455 histologically confirmed cases. Despite non-quantified MR parameter evaluation, the results of our prospective study were better than those reported in previous studies and demonstrated the need for a centralized approach to such rare pathology.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Magnetic resonance imaging (MRI) is generally considered to be the most accurate imaging technique for local staging of musculoskeletal tumors [18, 28, 36, 40, 46, 48, 59, 64]. Characterization is defined as the differentiation between benign and malignant lesions, definition of phenotype and histology of soft tissue tumors (STT), while grading means definition of the malignancy grade of soft tissue sarcomas (STS). Individual parameters such as morphology (shape, volume, and margins), homogeneity, signal intensity (SI) and changing SI on different pulse sequences are used for differentiation of malignant from benign lesions and characterization of STT [23, 61]. Unfortunately, because of low specificity and sensitivity, no single MRI feature can be used to differentiate accurately malignant from benign STT. Static, dynamic and first-pass MRI using gadolinium-chelate injection with definition of enhancement rate improve differentiation of necrotic from viable tissue, but because benign lesions may be highly vascular and malignant ones poorly vascularized, there still is controversy about the specificity of these parameters in differentiating malignant from benign lesions [20, 57, 58, 60]. Diagnosis of STT can be achieved by using a number of individual parameters or a combination of them, which can be quantified and incorporated into a mathematical diagnostic formula or by using a more subjective approach to the same parameters based on the skill of an expert group [17, 52]. The best differentiation of malignant from benign lesions and characterization figures are reached by a combination of a series of individual parameters. Authors of previous prospective studies [8, 37, 43] in which the accuracy of MRI in the differentiation of malignant from benign lesions and characterization of STT were studied have reported sensitivities between 94 and 100% and specificities between 17 and 90%. The exact histology of the lesions was predicted in 22–44% and in 58% of the benign group; predicting the histology of malignant lesions was not successful at all. However, because of methodological differences such as study samples that were not appropriate for lesion prevalence and differences in characterization and differentiation of malignant from benign lesion classification, these studies are difficult to compare [19]. Compared to previous studies, our patient selection has the best accordance with the known prevalence figures of benign and malignant STT.
The purpose of our study was to evaluate prospectively the accuracy (sensitivity, specificity, negative predictive value and positive predictive value) of MRI in differentiating benign from malignant lesions and in the determination of phenotype and histology of STT and soft tissue tumor-like lesions in a study population reflecting an appropriate sample according to lesion prevalence.
Materials and methods
To optimize the methodology and to cope with population biases in radiological studies, our prospective study had to meet a high score on the scale of methodological quality (SMQ) for clinical studies of radiological examinations proposed by Arrivé et al. [4]. We applied the 15 SMQ standards (SMQS) they defined to our study. All SMQS standards except three (11, 13 and 14) were met. The SMQS concerning the avoidance of diagnostic review bias (the referring radiologist and pathologist are informed about the MRI differential diagnosis), concerning the intra-observer variability that was not tested in our study and concerning the inter-observer variability that was not tested in a consensus report were not met.
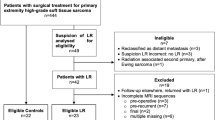
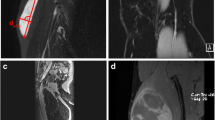
The material consisted of 548 untreated and proven STT or tumor-like lesions originating from a multi-institutional national database of STT in which 930 consecutive patients with STT examined by MRI for clinically obvious or incidentally detected mass lesions by MRI, histology or follow-up were registered between 1 January 2001 and 28 April 2003. The cooperating MR centers (n=58) were asked to present every soft tissue tumor or tumor-like lesion without selection to the principal investigator (database manager) prospectively (before biopsy or therapy). Retroperitoneal lesions, recurrences and not confirmed cases were excluded. Thirty-seven patients were examined at 1-T field strength and 411 on 1.5-T field strength. The study protocol included SE T1-WI and TSE T2-WI with and without FS or STIR in minimally two orthogonal planes (SE T1-WI n=545, TSE T2-WI n=291, SE T1-WI FS n=196, STIR n=185, TSE T2-WI FS n=311). TSE T2-WI or STIR sequences were available for 496 patients; TSE T2-WI FS and STIR sequences were available in 45 cases. In 52 cases, neither STIR nor TSE T2-WI FS were available; these were all cases without high SI in the lesion on T1-WI. Partial flip angle imaging was performed in a minority of cases and was excluded in the diagnostic process. In 503 cases, intravenous low molecular gadolinium chelate was administered (SE T1-WI n=304, SE T1-WI FS n=331, SE T1-WI, and SE T1-WI FS n=132). T1-WI was performed with fat-suppressed sequences before and after gadolinium chelate administration in 175 cases. SE T1-WI FS images before gadolinium administration were obtained to objectify the enhancement in cases with high SI of the lesion before gadolinium administration and because of its additional value in characterization of STT [24]. Dynamic gadolinium-enhanced GE T1-WI imaging with time intensity curves were available only in a minority of cases (n=5) and excluded in the diagnostic process.
After registration, a consensus second opinion report was made by two experienced radiologists (J.L.M.A.G with 12 years of experience and A.M.D.S with 15 years of experience); it was stored and sent to the referring co-investigator within 24 h. Age and gender of the patient as well as clinical information were available for the radiologist. Differentiating malignant from benign lesions and characterization were defined using parameters described in the literature [16]. In a consensus report, the intra- and inter-observer variability was not tested (SMQS standard 13 and 14 are not met).
The thresholds to differentiate between malignant and benign STT were interpreted in a non-quantified way. They were based on parameters such as origin, size, shape, margins, SI on different pulse sequences, signal homogeneity, changing pattern of homogeneity (T1–T2), grade and pattern of contrast enhancement, low SI septations, hemorrhage, peri-tumoral edema, distribution (intra-compartimental or extra-compartimental, neurovascular bundle displacement or encasement and bone involvement), fluid-fluid levels, signal voids, fat induction and intra-tumoral necrosis [9, 11, 17, 22].
Characterization (definition of phenotype and specific diagnosis) of the lesion was performed using the same parameters as for differentiation between malignant and benign lesions together with age and location, multiplicity and presence of concomitant diseases.
The observers were requested to give a tissue-specific (differential) diagnosis with a maximum of three possibilities in order of decreasing probability. Lesions were characterized as malignant if the differential diagnosis contained at least one malignant diagnosis. Lesions were characterized as benign if all diagnoses were benign. Non-specificity of a benign-looking lesion was reflected in the proposition of a biopsy. Non-specificity of a malignant-looking lesion was categorized as sarcoma not otherwise specified (NOS).
The reference standard was histology by biopsy and/or resection of the lesion. In selected cases, another reference standard was used, i.e., follow-up of at least 6 months without clinical or MRI evolution of benign tumors or tumor-like lesions. These selected cases were benign lesions with typical MRI presentation like cavernous hemangioma (n=14), lymphangioma (n=3), lipoma (n=14), pigmented villonodular synovitis (n=2), giant cell tumor of tendon sheath (n=1), neurinoma (n=5), elastofibroma dorsi (n=2) and plantar fibromatosis (n=2), concomitant diseases, i.e., hemangioma with typical MRI presentation in known Maffucci’s syndrome (n=1) and Klippel Trenaunay (n=1) and neurofibroma with typical MRI presentation in neurofibromatosis (n=2). Tumor-like lesions with typical MRI presentation were meningocoele (n=1), varicose vein (n=1), ganglion cyst (n=4), synovial (n=1) or tendon sheath effusion (n=1) and myositis (n=5). Tumor-like lesions with typical MRI presentation and spontaneous resolution were muscle strain (n=3), posttraumatic contusional tumor-like lesion (n=7) and hematoma (n=8). Infectious tumor-like lesions included a case with recent Bartonella henselae serology and typical history of cat scratch disease with lymphadenopathy (n=1), and (culture and) resolution under antibiotics of soft tissue abscess (n=2), diffuse soft tissue infection (n=1) or infectious lymphadenopathy (n=4) or lymphangitis (n=1). A tumor-like lesion with typical MRI presentation (aneurysmatically widened and partially thrombosed ulnar artery at Guyon’s canal), location and clinical history of repetitive trauma is hypothenar hammer syndrome (n=2); there was typical location, hyperuricemia and regression under uricosuria therapy in gouthy tophus (n=1), history of injection in injection granuloma (n=2) and typical dermal presentation of granuloma annulare (n=1). Histologically proven cases were anonymously stored in the database and identified by a storage number.
Final diagnosis was proven by histologic examination (n=455) or follow-up (n=93) in 548 cases. The tumor was removed in 278 patients; 148 patients had only a biopsy, and in 29 both biopsy and removal were performed.
Histology result of biopsies and/or removed specimens were compared in a prospective way with the MR reports. In the characterization results, only lesions with proven histology by biopsy and/or removed specimens were included. The referring radiologist and pathologist were informed about the MRI differential diagnosis; SMQS 11 (avoidance of diagnostic review bias) was not met. Sarcomas, metastases and cases with discordance between histological and MR findings were reviewed by a “Peer Review Committee” of six pathologists, experts in histology of STS. Up to now, this committee already has reviewed 125 cases. In case of non-conformity between the experts, additional histochemical examination was performed (n=16). Finally, a consensus histology report was made. If, despite histochemical examination, tumors could not be further differentiated, they were classified as NOS. Six cases were stored as high grade sarcoma NOS. Cases without proven diagnosis [not operated and/or insufficient follow-up (n=378)] with doubtful histology because of insufficient or not representative biopsy material (n=4) were excluded (n=382).
Concerning differentiation between benign and malignant tumors, all lesions, including the lesions confirmed by follow-up, were used. True negatives were defined as lesions with benign histology and benign MRI diagnosis (all diagnoses given in the differential diagnosis); true positives were defined as lesions with malignant histology and at least one malignant MRI diagnosis given.
Tumors were classified along with their histological phenotype (type of tissue from which the tumor arises) according to the histological classification of the World Health Organization (WHO) [21] adapted by Weiss and Goldblum [62]. Each histological category is divided into a benign and a malignant group.
To include tumor-like lesions and tumors located in the soft tissues but not covered by the before-mentioned phenotypes, this classification was extended for tumor-like lesions, hamartomas, soft tissue lymphomas, epidermal tumors, metastases and lesions without phenotype differentiation (NOS) as well as to meet the need of MRI to discriminate osseous and cartilaginous lesions. Tumor-like lesions included synovial or tendon sheath cysts or ganglia, tenovaginitis, thrombosed vessels, varicose veins, hematoma, scar tissue, abscess, soft tissue infection or inflammation, tuberculosis, gouty tophus, lymphangitis, rheumatic node, endometrioma, bursal effusion or hemorrhage, granuloma annulare, periostitis, botryomycoma, trichilemmal, sebaceous, epidermal inclusion or pilonidal cyst, muscle strain and myositis, foreign body reaction and tumoral calcinosis. Mesothelial tumors were excluded. This gives an overview of the modified phenotypic classification. MRI diagnoses were also classified according to these 21 modified Weiss and Goldblum groups.
The MRI diagnosis and histological diagnosis, differentiation between benign and malignant lesions and phenotype conformity were statistically determined with the calculation of predictive value (positive and negative), sensitivity, specificity and accuracy with P-values using Fisher’s exact test and 95% confidence interval using the Walds method.
Results
The patients with proven diagnosis included 268 females and 280 males with ages between 3 days and 93 years, all with the clinical suspicion of a soft tissue mass. One hundred twenty-three patients presented with a malignant STT; 425 patients presented with a benign one. Concerning differentiation between malignancy and benignity, if only the first diagnosis given was taken into account, a TN diagnosis was made in 399 instances, a FN diagnosis was made in 24 instances, a FP diagnosis in 26 cases and a TP diagnosis in 99 cases. A sensitivity of 80%, specificity of 94%, NPV of 94% and PPV 79% with an accuracy (91%) was obtained (P<0.0001) and presented in USA 1.
Concerning differentiation between malignancy and benignity, taking into account all three MRI diagnoses, a true negative (TN) diagnosis was made in 349 instances; a false negative (FN) diagnosis was made in 8 cases. In four of them, a biopsy was proposed because of the non-specific presentation of the lesion on MRI. A false positive (FP) diagnosis was made in 76 and a true positive (TP) diagnosis in 115 patients. Sensitivity of 93%, specificity of 82%, negative predictive value (NPV) of 98% and positive predictive value (PPV) of 60% with accuracy of 85% was obtained (P<0.001) (Table 2). FN results are listed in Table 3.
Concerning phenotype characterization (histological tissue type characterization), on the first MRI diagnosis an overall sensitivity of 67%, specificity of 98%, accuracy of 96%, PPV of 70% and NPV of 98% was obtained. Overview of phenotype classification and statistical workup are given in Table 4.
Table 5 gives an overview of the statistical workup of the phenotype classification of benign lesions. For benign lesions a sensitivity of 75%, specificity of 98%, NPV of 98%, PPV of 76% and accuracy of 97% was obtained. Benign lesions of fatty origin presented with the best sensitivity of 84% and PPV of 97%, while the lowest sensitivity of 75% and PPV of 58% was noted for fibrous tumors. Table 6 gives a statistical work up of the phenotype classification of malignant lesions. The phenotype definition of malignant STT had a sensitivity of 37%, a specificity of 96%, a PPV of 40%, an NPV of 96% and an accuracy of 92%. Neural tumors presented with the best sensitivity (71%), but a low PPV of 33%. To obtain statistically relevant figures for sensitivity and specificity, individual phenotypes with too small numbers were deleted from Tables 4, 5, 6.
A match between the first proposed MRI diagnosis and histological result was found in 227 (50%) out of 455 histologically confirmed cases. The correct histological diagnosis was included in the (on MR) proposed diagnostic possibilities (maximum three) in 257 (56%) cases. A list of the 181 (54%) benign SST with a correct first diagnosis is given in Table 7.
A specific diagnosis of malignant STT was made in 46 cases (38%). They are listed in Table 8.
Discussion
Soft tissues are defined as the subcutaneous and cutaneous tissues or compartments, muscles and tendons, fatty tissue, the soft parts of the joints (joint capsule, synovium, and ligaments) and peripheral neurovascular bundles. In our series, the retroperitoneal lesions were excluded.
Tumors of these soft tissues (STT) include benign and malignant ones and tumor-like lesions. The commonly used histological classification of STT refers to the standard book of Enzinger and Weiss (Weiss and Goldblum classification) or to the recent WHO histological typing adapted by Fletcher et al. [21]. We adjusted the classification of Weis and Goldblum in order to include metastasis, lymphoma and tumor-like lesions in our register.
Overall prevalence of malignant STT is estimated between 5.1 and 15.5% [34, 44]. In our study the relatively high number (n=123, 22%) of malignant lesions was due to a selection bias caused by the referral policy including only patients who had had an MR examination, excluding a large number of (superficial) lesions treated without imaging and of typically benign “do not touch” lesions. Our figures better reflect the prevalence of STT in contrast with the prospective studies of Ma and Berquist in which a prevalence of malignancy of 50 and 47%, respectively, was reported. This is probably due to the fact that the referring centers are requested to send all STT (benign and malignant) to the national registry. However, the prevalence of sarcoma in a radiological population (referred to MR) is more relevant than the prevalence in the entire population where the relatively high number of benign STT dwarfs the prevalence of sarcoma. The latter loses importance since a “radiological” population will always be a selected one.
Although some authors [7, 13, 32] state that MRI is not useful for differentiating malignant from benign lesions and characterization [41], Sundaram stressed the importance of “naming” soft tissue masses based on MR imaging criteria, working on the premise that one’s inability to “name” or provide a succinct differential diagnosis requires that the lesion has to be considered “indeterminate” and biopsied. The approach to such indeterminate lesions is that they are sarcomas until proven otherwise [50].
It was expected that MR imaging would have great potential for the histological diagnosis of STT because of its high intrinsic contrast resolution. Unfortunately, the initial enthusiasm has not entirely been fulfilled. Because MR images only provide indirect information about tumor histology by showing signal intensities related to some physicochemical properties of tumor components (e.g., fat, blood, water and collagen) and probably to well-known histological grading parameters, such as cellularity, cellular pleomorphism, mitotic rate, matrix and presence of necrosis, they reflect gross morphology of the lesion rather than underlying histology.
The second reason for the limited ability of MRI in tissue-specific characterization is the time-dependent changes of some tumors during natural evolution or as a consequence of therapy [16].
Although signal characteristics of both benign and malignant tumors frequently overlap, a number of reliable parameters for MR differentiation of malignant from benign tumors are described, including size, shape, margins, signal homogeneity, changing pattern of homogeneity (T1–T2), contrast enhancement (static studies and dynamic studies), low SI septations, intra-lesional hemorrhage, peri-tumoral edema, distribution (intra-compartmental and extra-compartmental), neurovascular bundle displacement and/or encasement, bone involvement and growth rate.
Retrospective studies on the differentiation of malignant from benign STT by MR imaging largely outnumber prospective ones [13, 25, 29, 42, 63]. De Schepper et al. performed retrospectively a multivariate statistical analysis to determine the accuracy of ten parameters, individually and in combination, for predicting malignancy. A sensitivity and specificity of 81% was achieved when a combination of parameters was used [17].
To date, only three prospective studies have been published. In the studies of Ma et al. [37], Berquist et al. [8] and Moulton et al. [43], respectively, a sensitivity of 100, 94 and 78% and a specificity of 17, 90 and 89% for predicting malignancy were reported.
The high sensitivity (100%) in the study of Ma et al. coincides with a very low specificity (17%) caused by a rigorous threshold of parameters that differentiates benign form malignant lesions, avoiding all false negatives. The additional value of MRI for differentiating benign from malignant lesions in these circumstances is doubtful. Their rigorous calculated threshold disregards subjective recognition of typical lesions with well-known MR imaging characteristics, but conflicts with their definition of malignancy and benignity. The limitations of their study are twofold. First, their list of lesions with well-known conflicting imaging characteristics such as hemangioma, lipoma, leiomyosarcoma and low grade liposarcoma is incomplete, lacking desmoid, lymphadenitis in cat scratch disease, synovial chondromatosis, pigmented villonodular synovitis and nodular fasciitis. Another drawback is the low number (36) of cases with equal malignant/benign (18/18) distribution, not reflecting the prevalence in the general population.
In the study of Berquist et al., a sensitivity of 94% and a specificity of 90% with an accuracy of 90% for diagnosing malignancy were obtained. Three radiologists were asked to evaluate cases according to several specific criteria: size, location, margins, SI and/or homogeneity on T1-WI and T2-WI images, neurovascular encasement or displacement, hemorrhage and/or edema in or around the lesions and bone involvement. Then they were asked to categorize lesions as malignant or benign and, when possible, to provide a specific diagnosis. Their study uses not a quantitative, but a subjective method for discrimination of malignant from benign lesions. This study also suffered from the same limitations as the previous one, e.g., a relatively low number of included cases (95) and a benign-malignant distribution that did not conform to the prevalence in the general population. Consequently, results of both studies are not comparable with ours.
Moulton et al. obtained a specificity of 89%, PPV of 65%, NPV of 94% and a sensitivity of 78%. Exclusion of the benign lesions decreased the specificity and NPV to 76% and 86%, respectively. A subjective analysis of each case was done prospectively in 95 cases and retrospectively but blinded in 127 cases. The observers were asked to determine the specific histological diagnosis of the lesion and whether they believed it to be benign of malignant. Because of the great number of lesions (225) and segmentation more in accordance with epidemiology, i.e., 179 (79.5%) benign and 46 (20.5%) malignant tumors, this study is comparable with ours.
In most previous studies, the accuracy of MRI was evaluated by using (a combination of) quantitative parameters. In a retrospective study of 44 cases, however, Teo et al. concluded that malignant soft tissue masses are reliably distinguished from hemangioma by subjective analysis combining lesion morphology, SI and enhancement after gadolinium chelate injection [52]. The subjective method for the differentiation of malignant from benign STT is also supported by Berquist et al. [8]. They could not identify any quantitative criterion or combination of criteria that could differentiate benign from malignant STT with greater accuracy than on subjective evaluation.
In our study, this non-quantitative analysis of different imaging characteristics was also performed in order to obtain a specific diagnosis or differential diagnosis with a maximum of three possibilities. The patient’s age, sex and clinical presentation were available to the radiologist. The radiologist was using imaging characteristics as described in the methods section, but also considering tumor prevalence, location, age of the patient and concomitant diseases. We classified lesions on MRI according to their phenotypes as defined by Weiss and Goldblum. By grouping lesions by grade and similar histology in which discrimination is often only possible on histochemical grounds, differentiation of malignant from benign tumors with phenotype classification better reflects the performance of characterization by MRI. The advantages of a multi-center approach for unusual histology are numerous if the methodology is rigorously followed. The additional expertise acquired in a short time by reviewing a large number of cases with up-to-date and uniform MRI technique proved to be highly useful. In regard to the wide range of possible diagnoses in STT (n=198 according to the list of Weiss and Goldblum), a representative sample containing the majority of diagnoses is needed; subsequently, even in our study, the peculiar diagnoses are not numerous enough to evaluate. All these arguments support the need for a centralized imaging registration of STT.
Compared to the study of Moulton published in 1994, our study, with the largest number of cases (548), best population representation and a comparable study population, showed that MRI reliably identifies malignancy in STT with a higher sensitivity (93 vs. 78%) with high NPV (98%) and comparable specificity (82 vs. 87%), but with rather low PPV (60%). Better sensitivity was probably the result of a methodology adapted to clinical radiological practice (three diagnostic possibilities in our study and only one MRI diagnosis in Moulton’s study), progress in radiological science with inclusion of newly described parameters, description of larger series of tumors with specific imaging characteristics and the diagnostic skill of radiologists [22, 31]. Indeed, in several recent studies, distinctive or suggestive imaging characteristics have been described in relatively large series of specific STT, including lesions adjacent to the superficial fascia, clear cell sarcoma, desmoid tumors, hemangiomas, liposarcoma and dermatofibrosarcoma protuberans [6, 14, 15, 30, 53]. If a biopsy is done in all lesions with rather benign but non-specific MRI appearance, FNs (n=8) are almost completely avoided. False negative cases without biopsy proposition (n=4) may go undiagnosed and untreated, and their number has to be as low as reasonably achievable. This technique is proposed by Sundaram to manage indeterminate lesions. He also states that the number of soft-tissue conditions that can be diagnosed on MRI will continue to grow [50]. In our study, FN cases without biopsy proposition included one lymphoma, one soft tissue metastasis and four sarcomas. The number of undiagnosed cases will decrease if the policy of performing a biopsy in all atypical lesions on MRI, especially in patients with known malignancies, is respected.
On the other hand, in 76 cases false positivity resulted in “over-treatment” by performing a biopsy that otherwise showed the benign character. The high NPV therefore will avoid misdiagnosis of malignant tumors as benign ones and inappropriate treatment.
In addition to the differentiation of malignant from benign lesions, tissue-specific diagnosis was also statistically evaluated in our series and compared to the data in the literature. In an early retrospective study on characterization, Balzarini reported that most lesions have a non-specific MRI appearance, except for lipomatous and fibrous lesions [6]. On the other hand, in a retrospective study of 134 masses and pseudo-masses of the hand and wrist, Capelastegui et al. reported an accurate diagnosis with differentiation of tumor-like lesions from genuine tumors [10]. As stated before, the need for preoperative characterization will grow in the future because of the diagnosis-dependent prognosis and diagnosis-dependent therapeutic approach to STT. Concerning characterization, we used the modified classification of Enzinger and Weiss. For characterization, the same parameters as for grading are used together with age, location, multiplicity and concomitant diseases. In a recent publication, we emphasized the value of SI characteristics on SE T1-WI with and without FS. Decisions regarding biopsy and treatment could be simplified if a specific diagnosis or limited differential diagnosis could be provided by clinical or imaging evaluation.
In their prospective study on differentiation of malignant from benign lesions and characterization of 95 lesions (50 benign and 45 malignant), Berquist et al. predicted the exact histology of the lesion in 22 and in 58% of the benign group. Predicting the histology of malignant lesions was not successful at all. In the largest partially prospective study of Moulton et al. (n=225, 179 benign and 46 malignant), the exact histology of the lesions was predicted in 44%, while specificity and NPV decreased for malignant lesions.
In our study the exact histology of all lesions was predicted in 50% (versus 22% in the study of Berquist et al). A correct histological diagnosis was included in the proposed diagnostic possibilities in 55% of cases.
Phenotype classification of all lesions revealed a sensitivity of 67% and a specificity of 98%. The best sensitivity (≥75%) and specificity (≥95%) was found in vascular, fatty, neural and synovial phenotypes. An intermediate sensitivity (71%) with high specificity (96%) was found in tumor-like lesions (Table 4). STT (benign and malignant) were confidently differentiated from tumor-like lesions.
In malignant lesions the exact histology was predicted in 47 (38%) cases. Best results were found for sarcomas NOS (6/6/100%), and malignant peripheral nerve sheath tumors (5/5/100%). The non-diagnosis “sarcoma NOS” was proposed in all malignant-looking lesions on MRI that could not be further differentiated; thus, it is expected that the prediction of histology will score well.
Phenotype classification of all malignant lesions revealed a sensitivity of 37% and a specificity of 96%. The highest sensitivity (71%) and specificity (91%) were reached for neural phenotype lesions (Table 6).
On the contrary, in benign lesions the exact histological diagnosis was made in 50% of lesions if only the first diagnosis was taken into account versus 58% in the study of Berquist et al.
Benign STT were accurately categorized into phenotypes (sensitivity 75%, specificity 98%, PPV 76%, NPV 98%, and accuracy 97%). Sensitivities of 75% or more and specificities of 95% or more were reached for vascular, fatty, neural, synovial and lymphoid phenotypes. Results of both differentiation of malignant from benign lesions and characterization were better in the group of benign STT and tumor-like lesions.
The methodology used to classify lesions as true positive and true negative was different in our study compared to the other prospective studies. In the other prospective studies, the radiologist could only give one diagnosis. If MR findings were not entirely specific, the radiologist in our study was allowed to give a differential diagnosis with a maximum of three possibilities; this methodology better reflects clinical radiological practice.
In conclusion, the results of our large, prospective (multi-institutional) study were better than those reported in previous studies, reflecting the progress not only in technology and technical skill, but also in the methodology and diagnostic flair of experienced radiologists.
The obtained results allowed the conclusion that rare pathologies such as STT are best centralized and studied by experts for diagnosis as well as probably for treatment. It was not our purpose to study all diagnostic parameters in a quantitative way and to provide the radiologist with a statistically based diagnostic formula. This could be a drawback to this study.
Another drawback to our study focused on MRI is the lack of data and comparison with other imaging examinations (standard radiography, ultrasound, CT scan, nuclear medicine). It is evident that these examinations, as well as evolving molecular biology studies, can provide complementary information. Together with proliferation markers, histological and immunohistochemical examination, MRI will be a cornerstone method in diagnosis, avoiding non-suited invasive therapy for many patients with benign STT and optimizing the treatment, prognosis and outcome. Moreover, optimal differentiation of malignant from benign lesions, phenotyping and histology will be mandatory for the development of therapeutic regimens in the near future.
References
Aisen AM, Martel W, Braunstein EM, McMillin KI, Phillips WA, Kling TF (1986) MRI and CT evaluation of primary bone and soft-tissue tumors. Am J Roentgenol 146:749–756
Alexander A, Nazarian L, Feld R (1997) Superficial soft tissue masses suggestive of recurrent malignancy: sonographic localization and biopsy. Am J Roentgenol 169:1449–1451
Andrassy RJ (2002) Advances in the surgical management of sarcomas in children. Am J Surg 184:484–491
Arrivé L, Renard R, Carrat F, Belkacem A, Dahan A, Le Hir P, Monnier-Cholley L, Tubiana J-M (2000) A scale of methodological quality for clinical studies of radiologic examinations. Radiology 217:69–74
Baliski CR, Temple WJ, Arthur K, Schachar NS (2002) Desmoid tumors: a novel approach for local control. J Surg Oncol 80:96–99
Balzarini L, Ceglia E, Petrillo R, Tesoro Tess JD, REitano A, Musumeci R (1989) Magnetic resonance in neoplasms of the adipose, fibrous and muscular tissues. Radiol Med 77:87–93
Beltran J, Simon DC, Katz W, Weis LD (1987) Increased MR signal intensity in skeletal muscle adjacent to malignant tumors: pathologic correlation and clinical relevance. Radiology 162:251–255
Berquist TH, Ehman RL, King BF, Hodgman CH, Ilstrup DM (1990) Value of MR imaging in differentiating benign from malignant soft-tissue masses: study of 95 lesions. Am J Roentgenol 155:1251–1255
Binkovitz LA, Berquist TH, Mc Leod RA (1990) Masses of the hand and wrist: detection and characterization with MR imaging. Am J Roentgenol 154:323–326
Capelastegui A, Astigarraga E, Fernandez-Canton G, Saralegui I, Larena JA, Merino A (1999) Masses and pseudomasses of the hand and wrist: MR findings in 134 cases. Skeletal Radiol 28:498–507
Cerofolini E, Landi A, Desantis G et al (1991) MR of benign peripheral nerve sheath tumors. J Comput Assist Tomogr 15:593–597
Chang AE, Matory YL, Dwyer AJ, Hill SC, Girton ME, Steinberg SM, Knop RH, Frank JA, Hyams D, Doppman JL et al (1987) Magnetic resonance imaging versus computed tomography in the evaluation of soft tissue tumors of the extremities. Ann Surg 205:340–348
Crim JR, Seeger LL, Yao L, Chandnani V, Eckardt J (1992) Diagnosis of soft tissue masses with MR imaging: can benign masses be differentiated from malignant ones? Radiology 185:581–586
Daldrup H, Shames DM, Wendland M, Okuhata Y, Link TM, Rosenau W, Lu Y, Brasch RC et al (1998) Correlation of dynamic contrast enhanced magnetic resonance imaging with histologic tumor grade: comparison of macromolecular and small-molecular contrast media. Pediatr Radiol 28:67–78
De Beuckeleer LH, De Schepper AM, Vandevenne JE et al (2000) MR imaging of clear cell sarcoma (malignant melanoma of the soft parts): a multicenter correlative MRI–pathology study of 21 cases and literature review. Skeletal Radiol 29:187–195
De Schepper AM (2001) Grading and characterization of soft tissue tumors. In: De Schepper AM, Parizel PM, De Beukeleer L, Vanhoenacker F (eds) Imaging of soft tissue tumors, 2nd edn. Springer, Berlin Heidelberg New York, pp 123–141
De Schepper A, Ramon F, Degryse H (1992) Statistical analysis of MRI parameters predicting malignancy in 141 soft tissue masses. Rofo Fortschr Geb Rontgenstr Neuen Bildgeb Verfahr 156:587–591
De Schepper A, De Beuckeleer L, Vandevenne J, Somville J (2000) Magnetic resonance imaging of soft tissue tumors. Eur Radiol 10:213–222
Duchateau F, Vande Berg BC (2002) MR imaging of the articular cartilage of the knee with arthroscopy as gold standard: assessment of methodological quality of clinical studies. Eur Radiol 12:2977–2981
Erlemann R, Reiser MF, Peters PE, Vasallo P, Nommensen B, Kusnierz-Glaz CR, Ritter J, Roessner A (1989) Musculoskeletal neoplasms: static and dynamic Gd-DTPA-enhanced MR imaging. Radiology 171:767–773
Fletcher CDM, Mertens KK, Mertens F (eds) (2002) Pathology and genetics. Tumours of soft tissue and bone, WHO classification of tumours. IARC, Lyon
Galant J, Marti-Bonmati L, Soler R et al (1998) Grading of subcutaneous soft tissue tumors by means of their relationship with the superficial fascia on MR imaging. Skeletal Radiol 27:657–663
Galant J, Marti-Bonmati L, Saez F, Soler R, Alcala-Santaella R, Navarro M (2003) The value of fat-suppressed T2 or STIR sequences in distinguishing lipoma from well-differentiated liposarcoma. Eur Radiol 13:337–343
Gielen JL, De Schepper AM, Parizel PM, Wang XL, Vanhoenacker F (2003) Additional value of magnetic resonance with spin echo T1-weighted imaging with fat suppression in characterization of soft tissue tumors. J Comput Assist Tomogr 27:434–441
Greenspan A, McGahan JP, Vogelsang P, Szabo RM (1992) Imaging strategies in the evaluation of soft-tissue hemangiomas of the extremities: correlation of the findings of plain radiography, angiography, CT, MRI and ultrasonography in 12 histologically proven cases. Skeletal Radiol 21:11–18
Hanna SL, Fletcher BD (1995) MR imaging of malignant soft-tissue tumors. Magn Reson Imaging Clin North Am 3:629–650
Hasegawa T, Yamamoto S, Yokoyama R, Umeda T, Matsuno Y, Hirohashi S (2002) Prognostic significance of grading and staging systems using MIB-1 score in adult patients with soft tissue sarcoma of the extremities and trunk. Cancer 95:843–851
Hogeboom WR, Hoekstra HJ, Mooyaart EL, Freling NJ, Schraffordt Koops H (1991) MRI and CT in the preoperative evaluation of soft-tissue tumors. Arch Orthop Trauma Surg 110:162–164
Jelinek JS, Kransdorf MJ (1995) MR imaging of soft-tissue masses: mass-like lesions that simulate neoplasms. Magn Reson Imaging Clin North Am 3:727–741
Kransdorf MJ (1995) Malignant soft-tissue tumors in a large referral population. Am J Roentgenol 164:129–134
Kransdorf MJ (1995) Benign soft-tissue tumors in a large referral population. Am J Roentgenol 164:395–402
Kransdorf M, Jelinek JS, Moser RP et al (1989) Soft-tissue masses: diagnosis using MR imaging. Am J Roentgenol 153:541–547
Kreicbergs A, Tibukait B, Willems J, Bauer HC (1987) DNA flow analysis of soft tissue tumors. Cancer 59:128
Lattes R (1982) Tumors of the soft tissue, 2nd edn. Armed Forces Institute of Pathology, Washington
Levine EA, Holzmayer T, Bacus S et al (1997) Evaluation of newer prognostic markers for adult soft tissue sarcoma. J Clin Oncol 15:3249–3257
Lucas JD, O’Doherty MJ, Wong JC, Bingham JB, McKee PH, Fletcher CD, Smith MA (1998) Evaluation of fluorodeoxyglucose positron emission tomography in the management of soft-tissue sarcomas. J Bone Joint Surg Br 80:441–447
Ma LD, Frassica FJ, Scott WW Jr, Fishman EK, Zerbouni EA (1995) Differentiation of benign and malignant musculoskeletal tumors: potential pitfalls with MR imaging. Radiographics 15:349–366
Ma LD, Frassica FJ, McCarthy EF, Bluemke DA, Zerhouni EA (1997) Benign and malignant musculoskeletal masses: MR imaging differentiation with rim-to-center differential enhancement ratios. Radiology 202:739–744
Matsuno T, Gebhardt MC, Schiller AL et al (1988) The use of flow cytometry as a diagnostic aid in the management of soft-tissue tumors. J Bone Joint Surg 70:751
Mc Kenzie AF (1997) The role of magnetic resonance imaging. When to use it and what to look for. Acta Orthop Scand Suppl 273:21–24
Meis-Kindblom J, Enzinger F (1996) Color atlas of soft tissue tumors. Mosby-Wolfe, St Louis
Miller TT, Potter HG, LcCormack RR (1994) Benign soft tissue masses of the wrist and hand: MRI appearances. Skeletal Radiol 23:327–332
Moulton JS, Blebea JS, Dunco DM, Braley SE, Bisset GS III, Emery KH (1995) MR imaging of soft-tissue masses: diagnostic efficacy and value of distinguishing between benign and malignant lesions. Am J Roentgenol 164:1191–1199
Myhre-Jensen O (1981) A consecutive 7-year series of 1331 benign soft tissue tumors: clinicopathologic data-comparison with sarcomas. Acta Orthop Scand 52:287–293
Okuno SH, Edmonson JH (2003) Combination chemotherapy for desmoid tumors. Cancer 97:1134–1135
Panicek DM, Gatsonis C, Rosenthal DI et al (1997) CT and MR imaging in the local staging of primary malignant musculoskeletal neoplasms: report of the radiology diagnostic oncology group. Radiology 202:237–246
Petasnick J, Turner D, Charters J, Gitelis Z, Zacharias C (1986) Soft-tissue masses of the locomotor system: comparison of MR imaging with CT. Radiology 160:125–133
Petterson H, Thurman G III, Hamlin D et al (1987) Primary musculoskeletal tumors: examination with MR imaging compared with conventional modalities. Radiology 164:237–241
Pisters PWT, Leung DHY, Woodruff J, She W, Brennan MF (1996) Analysis of prognostic factors in 1041 patients with localized soft tissue sarcomas of the extremities. J Clin Oncol 1:1679–1689
Sundaram M, Sharafudding M (1995) MR imaging of benign soft tissue masses. Magn Reson Imaging Clin North Am 3:609–627
Tacikowska M (2002) Dynamic MR imaging of soft tissue tumors with assessment of the rate and character of lesion enhancement. Med Sci Monit 8:31–35
Teo EL, Strousse PJ, Hernandez RJ (2000) MR imaging differentiation of soft-tissue hemangiomas from malignant soft-tissue masses. Am J Roentgenol 174:1623–1628
Terrier-Lacombe MJ, Guillou L, Maire G, Terrier P, Vince DR, De Saint Aubain Somerhausen N, Collin F, Pedeutour F, Coindre JM (2003) Dermatofibrosarcoma protuberans, giant cell fibroblastoma, and hybrid lesions in children: clinicopathologic comparative analysis of 28 cases with molecular data. A study from the French Federation of Cancer Centers Sarcoma Group. Am J Surg Pathol 27:27–39
Tung G, Davis L (1993) The role of magnetic resonance imaging in the evaluation of soft tissue mass. Crit Rev Diagn Imaging 34:239–308
Ueda T, Aozasa K, Tsujimoto M et al (1989) Prognostic significance of Ki-67 reactivity in soft tissue sarcomas. Cancer 63:1607
Vandevenne JE, De Schepper AM, De Beuckeleer L, Van Marck E, Aparisi F, Bloem JL, Erkorkmaz Z, Brijs S (1997) New concepts in understanding evolution of desmoid tumors: MR imaging of 30 lesions. Eur Radiol 7:1013–1019
Van der Woude HJ, Bloem JL, Schipper J, Hermans J Van Eck-Smit BLF, Van Oostayen J, Taminiau AHM, Holscher HJ, Hogendoorn PCW (1994) Changes of tumor perfusion in bone sarcomas induced by chemotherapy: color Doppler flow imaging and three phase bone scintigraphy. Radiology 191:421–431
Van der Woude H, Verstraete K, Taminiau A, Hogendoorn P, Vanzieleghem B, Bloem J (1995) Double slice dynamic contrast-enhanced subtraction MR images in 60 patients with musculoskeleletal tumors or tumorlike lesions. Eur Radiol 5:181
Van Rijswijk CS, Geirnaerdt MJ, Hogendoorn PC et al (2003) Dynamic contrast-enhanced MR imaging in monitoring response to isolated limb perfusion in high-grade soft tissue sarcoma: initial results. Eur Radiol 13:1849–1858
Verstraete KL, Vanzieleghem B, De Deene Y, Palmans H, De Greef D, Kristoffersen DT, Uyttendaele D, Roels H, Hamers J, Kunnen M (1995) Static, dynamic and first-pass MR imaging of musculoskeletal lesions using gadodiamide injection. Acta Radiol 36:27–36
Waldt S, Rechl H, Rummeny EJ, Woertler K (2003) Imaging of benign and malignant soft tissue masses of the foot. Eur Radiol 13:1125–1136
Weiss SH, Goldblum JR (2001) General considerations. In: Weiss SH, Goldblum JR (eds) Enzinger and Weiss’s soft tissue tumors, 4th edn. Mosby, St Louis, pp 1–19
Wetzel LH, Levine E (1990) Soft-tissue tumors of the foot: value of MR imaging for specific diagnosis. Am J Roentgenol 155:1025–1030
Wetzel L, Levin E, Murphey M (1987) A comparison of MR imaging and CT in the evaluation of musculoskeletal masses. Radiographics 7:851–874
Acknowledgments
We would like to thank the coinvestigators of the Belgian Soft Tissue Neoplasm Registry (BSTNR) and the members of the pathological peer review committee. Dr. Patrick Aerts, Jean Alexiou, Michel Baeyaert, Dario Bigattini, Eric Bijnens, Isabel Biltjes, Edith Bleus, Jean Bonnet, Peter Bracke, Stefaan Brijs, Jan Broeckx, Alain Broeders, Peter Brys, Lieve Buyl, Eric Bynens, Ben Caerts, Vincent Caucheteur, Bart Claikens, Clybouw, Ilse Crevits, Bénédicte Daenen, Adelard De Backer, Frank De Belder, Christophe de Bergeyck, Luc De Beuckeleer, Y. De Breuck, Damienne de la Kethulle, Michel De Maeseneer, N. De Saint Aubain, De Surgeloose, Guy De Vriendt, Dimitri De Vuyst, Geert Debakker, Filip Deckers, Hugo Declercq, Hendrik Degryse, Johan Dehem, Piet Dekimpe, Marc Deldinne, Luc Denis, J. Desimpelaere, L. Divano, Julien Djekic, Laurent Dorthu, J. Doyen, P. Flandroy, Jan Fraeyman, Eric Fumiere, Wim Geyskens, Ghijselings, Dirk Ghysen, Grignard, M. Guffens, A. Hacourt, Ester Hauben, Evert Heindryckx, Brat Hughes, Tjeerd Jager, Marie-Anne Labaisse, Anne Lampaert, H. Lauwers, Isabelle Layalle, Marc Lemort, Bart Maes, Menno Maes, Frederic Maisse, Jacques Malghem, Sam Mampaey, Peter Matthijs, Hendrik Mertens, Eva Mortelmans, Lieven Mortelmans, Tom Mulkens, Yolande Nackaerts, Jean-François Nisolle, Jacques Olette, P. Pauwels, Johan Peeters, Dirk Perdieus, Benoït Poucet, Kristof Ramboer, Léon Rausin, Willem Roelandt, Philippe Rosoux, Frederik Rosseel, Rodrigo Salgado, Karlien Schutyzer, Patrick Seynaeve, Maryam Shahabpour, William Simoens, Philip Simons, Dana Smolders, Roel Stappaerts, Rudi Stokmans, Linus Swinnen, Carlo Thywissen, M.R. Timmermans, K. Trap, Luc Van Breuseghem, Marc Van Campenhoudt, B. Van Den Bossche, Luc Van den Hauwe, Pieter Van Dyck, Johan Van Goethem, Filip Van Grimberge, Eddy Van Hedent, Eric Van Marck, R. Van Ratthinge, Walter Van Rompaey, Christian Van Ruyssevelt, Van Tournhoudt, Bruno Vande Berg, Jan Vandevenne, Frederik Vanrietvelde, Bart Vanzieleghem, Johan Vercruysse, Huguette Vereycken, Dieter Verhulst, Frans Vermaut, Koenraad Verstraete, S. Vyt, Jan Willems, C. Ziegels.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gielen, J.L.M.A., De Schepper, A.M., Vanhoenacker, F. et al. Accuracy of MRI in characterization of soft tissue tumors and tumor-like lesions. A prospective study in 548 patients. Eur Radiol 14, 2320–2330 (2004). https://doi.org/10.1007/s00330-004-2431-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-004-2431-0