Abstract
We assessed potential predictors of sustained remission for 2 years according to the Disease Activity Score in 28 joints (DAS28)-CRP in patients with rheumatoid arthritis (RA). We obtained data for 290 RA outpatients, from July 2009 to September 2012. Sociodemographic data and answers to questionnaires were collected in face-to-face interviews. Remission was defined according to DAS28-CRP. Sustained remission was defined as meeting criteria for remission in the annual assessment for two consecutive years. Predictive factors of sustained remission according to DAS28-CRP were assessed by univariate and multivariate analyses. Of the 290 RA patients, the baseline remission level, according to DAS28-CRP, was 54.5%. During 2 years of follow-up, the sustained remission rate was 24.5%. RA patients who achieved sustained remission, according to DAS28-CRP, were younger, and had a shorter duration of symptoms, longer period of education, higher monthly income, lower Health Assessment Questionnaire (HAQ) score, lower physician global assessment, lower patient global assessment, lower patient pain assessment, and higher EQ-5D at baseline. Multivariate analyses showed that the baseline HAQ score was independently associated with sustained remission for 2 years according to DAS28-CRP (OR 0.298, 95% CI 0.115–0.770; p = 0.012). A lower HAQ score at baseline was an independent predictor of sustained remission at 2 years, according to DAS28-CRP. Thus, HAQ scores could be useful when stratifying patients according to risk for flare-ups in the clinic.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Remission in rheumatoid arthritis is considered an essential goal, because patients in remission show better physical function, higher health-related quality of life, and work productivity, even when compared with those who have low disease activity [1,2,3]. Also, it is clinically important to identify predictors of remission so that physicians can individualize treatment plans and educate patients on their expected prognoses. Several studies have sought to identify predictors of remission in patients with RA, as summarized in a systematic review by Katchamart et al. [4]. They identified several independent predictors of remission, including clinical factors (male, young age, late-onset RA, short disease duration, non-smoker, low baseline disease activity, mild functional impairment, low baseline radiographic damage), laboratory factors (seronegative status, low levels of acute-phase reactants), genetic markers, initial type and combination of therapeutic agents, and moderate or good response to treatments within the first 6 months.
While achieving remission is the first goal, maintaining remission is also important. The significance of sustained remission is evident from previous studies demonstrating that joint damage progresses more slowly and functional capacity continues to improve over time if remission is sustained, resulting in better outcomes than with more active disease [5,6,7]. Understanding which manifestations of patient may influence on sustained remission will provide more important data and guideline for physicians and patients. Recently, Hamann et al. [8] performed a meta-analysis to identify factors associated with sustained remission in patients with RA treated with TNF inhibitors. Greater baseline disease activity, a higher tender joint count, older age, longer disease duration, baseline functional impairment, and female sex were associated with a reduced likelihood of sustained remission; concomitant methotrexate use was associated with an increased likelihood of sustained remission. Although few reports of predictors of sustained remission in RA from longitudinal, observational cohorts were reported [9,10,11,12], there is still no established consensus. Thus, we assessed the frequency of sustained remission according to DAS28-CRP and investigated potential predictors of sustained remission in RA patients over 2 years of follow-up.
Methods
Study design and participants
We collected baseline and prospectively annual follow-up data for 290 RA outpatients from July 2009 to September 2012, who were ≥ 18 years old and met the 1987 revised criteria for the classification of RA [13]. The study protocol was approved by the institutional review board of Chonnam National University Hospital (I-2009-05-049), Republic of Korea. All patients provided written informed consent.
Variables
Sociodemographic data, including age, age at symptom onset, age at disease diagnosis, symptom duration, treatment duration, gender, body mass index (BMI), history of smoking, waist-to-hip ratio, period of education, monthly income, and laboratory factors, such as rheumatoid factor (RF), anti-cyclic citrullinated peptide (anti-CCP), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP), were assessed. Information on types and amounts of drugs at the time of study enrollment was also collected. An experienced rheumatologist assessed clinical disease status, including the presence and duration of morning stiffness, and a physical examination of the 28 joints for the tender and swollen joint counts. Comorbidity was defined as a patient having ever had a medical history of coronary heart disease, heart failure, hypertension, stroke, diabetes mellitus, asthma, hepatitis, chronic kidney disease, thyroid disease, or cancer. For each patients, we collected answers to questionnaires in face-to-face interviews assessing functional capacity, as measured by the Korean version of the health assessment questionnaire (HAQ) scores [14], and health-related quality of life, as measured by the EQ-5D [15]. Patient global and patient pain assessments were made using a 100-mm visual analog scale (VAS) [16]. Physician global assessment of disease activity was assessed by an experienced rheumatologist also on a 100-mm VAS.
Definitions of remission
We assessed the remission status at each study visit based on the Disease Activity Score in 28 joints (DAS28)-CRP (remission defined as < 2.6) [17]. Sustained remission was defined as the patient continuing in remission at two consecutive annual assessments until the last observation, with no obvious evidence of flare-up, such as several joints with coincident inflammation, with a high level of ESR or CRP, or any need to change treatment to control disease activity.
Statistical methods
Demographic, laboratory, and clinical manifestations were summarized using medians and interquartile ranges for continuous variables and numbers and percentages for categorical variables. Comparisons for variables between the sustained remission group and flare-up group were performed using the Mann–Whitney U test for continuous variables and χ 2 tests for categorical data. Predictors of sustained remission, according to the DAS28-CRP, were assessed by univariate and multivariate analyses using a binary logistic regression model with step-wise backward elimination. Univariate regressions were performed to identify baseline individual variables and indices that were potential predictors of sustained remission. Variables with p values < 0.05 were entered stepwise into the multivariate model; variables with significance levels > 0.1 were removed, as they did not contribute to the model. The results are presented as multivariate ORs with 95% CIs. Statistical analyses were performed using SPSS software (ver. 18; SPSS Inc., Chicago, IL, USA). p values < 0.05 were considered to indicate statistical significance.
Results
In total, 290 patients with RA were enrolled and ultimately 224 patients with RA completed the 2-year follow-up study. At baseline, 158 patients were in remission. We divided them into two groups: one for patients who achieved sustained remission for 2 years and the other for patients who were not in remission at any study visit. After 1 year of follow-up, 111 patients were still in remission, 37 were not in remission, 8 were lost to follow-up, and 2 patients withdrew consent. After the 2-year follow-up of the 111 patients who were in remission at the 1-year follow-up, 71 were still in remission, 30 were not, 6 were lost to follow-up, and 4 patients withdrew consent. In the 37 patients who were not in remission at the 1-year follow-up, 28 completed the 2-year follow-up, 5 were lost to follow-up, and 4 withdrew consent. Ultimately, 129 patients who were in remission at baseline, according to DAS28-CRP, completed the 2-year follow-up and were divided into two groups: the ‘sustained remission group’ and the ‘flare-up group’ (Fig. 1). The percentage of patients in remission, by DAS28-CRP, at the time of enrollment was 54.5% (158/290). After the 2-year follow-up, the percentage of patients in sustained remission, by DAS28-CRP, was 24.5% (71/290). Baseline characteristics at the first assessment of remission are described in Table 1. Patients who achieved sustained remission, according to DAS28-CRP, were younger (53 vs. 58 years, p = 0.033) and had a shorter duration of symptoms (6.13 vs. 8.66 years, p = 0.038), a longer period of education (12 vs. 9 years, p = 0.050), and a higher monthly income (1650 vs. 825 USD, p = 0.012) at baseline. Gender, smoking, body mass index, positivity for RF and anti-CCP, ESR, CRP, and type and amount of drug at baseline did not differ between the groups.
Clinical manifestations and the results of functional disability, quality of life, and clinical assessment at the first assessment of remission by DAS28-CRP are shown in Table 2. Patients who achieved sustained remission for 2 years, according to DAS28-CRP, had a lower median (IQR) baseline HAQ score (0.12; 0.00–0.38) vs. 0.38 (0.13–0.78) in patients who were not in sustained remission (p < 0.001). Compared to patients in the flare-up group at baseline, those in sustained remission had a lower median (IQR) physician global assessment (12.0; 0.00–0.38 vs. 17.0; 10.5–36.3), a lower patient global assessment (11.0; 5.0–33.0 vs. 24.5; 11.0–70.3), a lower patient pain assessment (26.0; 16.0–49.0 vs. 36.0; 20.5–52.3) (p < 0.05 for all comparisons). The sustained remission group showed a higher median (IQR) baseline EQ-5D (0.85; 0.73–1.00 vs. 0.79; 0.68–0.85) in the flare-up group (p = 0.003). Morning stiffness, tender joints, swollen joints, and comorbidities did not differ between the groups at baseline.
We also evaluated potential predictive factors of sustained remission, according to DAS28-CRP, by univariate and multivariate analyses (Table 3). By univariate logistic regression, period of education (OR 1.083, 95% CI 1.007–1.164; p = 0.032), HAQ score (OR 0.223, 95% CI 0.085–0.583; p = 0.002), physician global assessment (OR 0.961, 95% CI 0.935–0.988; p = 0.005), patient global assessment (OR 0.982, 95% CI 0.970–0.994; p = 0.004), patient pain assessment (OR 0.982, 95% CI 0.965–0.998; p = 0.049), and EQ-5D (OR 13.76, 95% CI 1.969–96.23; p = 0.008) at baseline were significant. These variables were then subjected to multivariate logistic regression. Ultimately, baseline HAQ score (OR 0.257, 95% CI 0.067–0.980; p = 0.047) was found to be independently associated with sustained remission for 2 years, according to DAS28-CRP.
Discussion
In this study of 290 patients with RA, the remission level at baseline, according to DAS28-CRP, was 54.5%. During follow-up over 2 years, the sustained remission level was 24.5%. RA patients who achieved such sustained remission were younger and had a longer period of education, higher monthly income, lower HAQ score, lower physician global assessment, lower patient global assessment, lower patient pain assessment, and higher EQ-5D at baseline than patients who experienced flare-ups. A multivariate analysis revealed that low HAQ score at baseline was independently associated with sustained remission for 2 years, according to DAS28-CRP.
In terms of clinical status, patients in our study population who had lower HAQ scores, lower physician and patient global assessments, lower patent pain assessments, and higher EQ-5D at baseline achieved sustained remission for 2 years. From the multivariate analysis, our results showed that only a low HAQ score at baseline was an independent predictor of sustained remission at 2 years, according to DAS28-CRP. Jayakumar et al. reported that male gender, short duration of symptoms, and fewer tender joints at baseline were predictors of sustained remission by DAS, but baseline HAQ score was not included as an independent predictor [11]. Another recent cohort study that defined remission as no tender or swollen joints showed that female gender, higher tender joint count, higher HAQ, obesity, and hypertension or depression at baseline were independent predictors of being less likely to achieve remission at the 5-year follow-up [10]. Unlike these studies, which mentioned many predictors, our results clearly showed only low HAQ score at baseline to be associated with sustained remission, highlighting the importance of HAQ. HAQ is a commonly used instrument for measuring physical function in RA and predicting disability and mortality. The prevention of functional disability, reflecting the cumulative effects of the disease, is an important problem in RA treatment. Functional disability in RA affects the patient’s well-being and correlates with long-term disease consequences, from loss of employment to mortality [18,19,20]. Moreover, higher baseline HAQ scores have been shown to be associated with mortality [21] and lower HAQ scores to be associated with favorable responses to treatment [12]. We suggest that our results add weight to the importance of HAQ in RA, not only as a predictor of functional outcomes, mortality, and treatment response, but also as a predictor of sustained remission.
An assessment of disease activity is essential in treating patients appropriately, but various definitions of disease activity have different stringencies; DAS28-CRP is considered the least stringent and may underestimate disease activity, compared with other definitions [22,23,24,25]. This indicates that patients with residual joint inflammation may be considered as in remission when assessments are based only on DAS28-CRP and progress in joint damage and functional disability despite ongoing treatment. Although previous studies have shown that low HAQ scores are associated with remission [26,27,28], they only considered inflammation status at a single time point. In this study, we found that low baseline HAQ scores were associated with the maintenance of remission, which may indicate the longitudinal significance of the HAQ score. We suggest that a low HAQ score at any point in remission may show that the disease process has subsided in response to therapy; thus, the HAQ score may complement DAS28-CRP in assessing disease status precisely in practice.
In terms of socioeconomic factors, RA patients who achieved sustained remission according to DAS28-CRP, were younger and had a longer period of education and higher monthly income at baseline than those who did not. Although socioeconomic status has been shown to be associated with delayed treatment, higher disease activity, increased joint damage, and disability in RA [29], there has been no previous report demonstrating an association between sustained remission and socioeconomic status. Our results suggest that social determinants of health, including longer education and higher monthly income, may be associated with maintaining remission, which may result from patient compliance with medical treatment and/or capacity for supplementary non-pharmacological treatments.
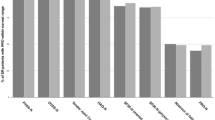
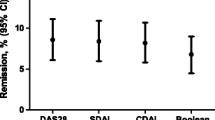
In this study, the frequencies of patients in remission at all time points were relatively high. Thus, we assessed remission rates using various definitions of remission. The RA remission rates varied from as low as 5.9% by the Boolean measure, to 10.0% on the CDAI, 10.3% on the SDAI, 18.0% on the DAS28-ESR, and 54.5% on the DAS28-CRP. Similarly, others have reported that various definitions of disease activity yield different remission rates; the DAS28-CRP measure is the least stringent and the Boolean criteria are considered to be the most restrictive of all disease activity measures [22,23,24,25]. In our study, the difference between the highest and lowest values was greater than in previous studies, showing that the DAS28 definition identifies about fourfold more patients in remission than does the Boolean definition [30, 31]. This variability was less pronounced on annual follow-ups, but the Boolean test still yielded the lowest scores and the DAS28-CRP the highest. During follow-up over 2 years, the sustained RA remission rates were 55.0% (DAS28-CRP), 46.5% (DAS28-ESR), 37.5% (SDAI), 32.0% (CDAI), and 30.8% (Boolean). We found higher proportions of sustained remission over 2 years than reported by Shahouri et al. [8.1% (Boolean), 6.0–13.5% (CDAI), and 13.3% (SDAI)] [32]. This difference may reflect the fact that patients who agreed to inclusion were more compliant with physicians’ instructions and relatively undemanding in terms of satisfaction. Although this issue may reduce the generalizability of the findings, we believe that the study results were not significantly affected. Also, clinicians need to carefully interpret disease activity in terms of appropriate treatment because any discrepancy may cause confusion when assessing the therapeutic response.
A strength of this study is that we designed a longitudinal observational cohort, whereas most previous studies considered only a cross-sectional evaluation of remission. Additionally, we included subjects who underwent treatment in ordinary clinical settings with not only early RA but also established RA, which may better reflect real practice.
Several limitations of our study also need to be considered. First, it was a single-center study and our findings might not be generalizable to all RA populations. Selection bias may potentially be in play because we excluded patients who were not in remission at baseline. However, when we compared patients in remission with those not in remission at baseline, we found no difference in age, sex, symptom or treatment duration, BMI, or any sociodemographic parameter between groups. Patients who were not in remission exhibited higher ESRs, higher CRP and DAS28-CRP levels, more frequent and longer-lasting morning stiffness, more tender joints, higher HAQ scores, lower physician and patient global assessments, lower patient pain assessments, and lower EQ-5D scores. We suggest that these clinical results could reasonably be associated with disease status, which would not affect the generalizability of the results. Second, the visit interval was 1 year and we cannot rule out the possibility of insidious fluctuation of disease activity, which may have resulted in some patients being deemed to be in sustained remission when they were not. However, we excluded patients from the sustained remission group if they had obvious evidence of a flare-up, such as several joints with inflammation together with a high level of ESR or CRP or any need to change treatment to control disease activity. Third, we did not assess radiographic damage, which has also been found to be significant. In addition, predictors of sustained remission may vary depending on the various definitions used to measure disease activity, which have different stringencies.
In conclusion, a lower HAQ score at baseline was an independent predictor for sustained remission at 2 years, according to DAS28-CRP. Physicians should consider the possibility of flare-up when functional capacity decreases at any point, even if the patient has technically achieved remission.
References
Smolen JS, Aletaha D, Bijlsma JW, Breedveld FC, Boumpas D, Burmester G, Combe B, Cutolo M, de Wit M, Dougados M, Emery P, Gibofsky A, Gomez-Reino JJ, Haraoui B, Kalden J, Keystone EC, Kvien TK, McInnes I, Martin-Mola E, Montecucco C, Schoels M, van der Heijde D, Committee TTE (2010) Treating rheumatoid arthritis to target: recommendations of an international task force. Ann Rheum Dis 69(4):631–637. doi:10.1136/ard.2009.123919
Radner H, Smolen JS, Aletaha D (2014) Remission in rheumatoid arthritis: benefit over low disease activity in patient-reported outcomes and costs. Arthritis Res Ther 16(1):R56. doi:10.1186/ar4491
Ma MH, Scott IC, Kingsley GH, Scott DL (2010) Remission in early rheumatoid arthritis. J Rheumatol 37(7):1444–1453. doi:10.3899/jrheum.091131
Katchamart W, Johnson S, Lin HJ, Phumethum V, Salliot C, Bombardier C (2010) Predictors for remission in rheumatoid arthritis patients: a systematic review. Arthritis Care Res (Hoboken) 62(8):1128–1143. doi:10.1002/acr.20188
Combe B, Logeart I, Belkacemi MC, Dadoun S, Schaeverbeke T, Daures JP, Dougados M (2015) Comparison of the long-term outcome for patients with rheumatoid arthritis with persistent moderate disease activity or disease remission during the first year after diagnosis: data from the ESPOIR cohort. Ann Rheum Dis 74(4):724–729. doi:10.1136/annrheumdis-2013-204178
Radner H, Alasti F, Smolen JS, Aletaha D (2015) Physical function continues to improve when clinical remission is sustained in rheumatoid arthritis patients. Arthritis Res Ther 17:203. doi:10.1186/s13075-015-0719-x
Lillegraven S, Prince FH, Shadick NA, Bykerk VP, Lu B, Frits ML, Iannaccone CK, Kvien TK, Haavardsholm EA, Weinblatt ME, Solomon DH (2012) Remission and radiographic outcome in rheumatoid arthritis: application of the 2011 ACR/EULAR remission criteria in an observational cohort. Ann Rheum Dis 71(5):681–686. doi:10.1136/ard.2011.154625
Hamann P, Holland R, Hyrich K, Pauling JD, Shaddick G, Nightingale A, McHugh N (2017) Factors associated with sustained remission in rheumatoid arthritis in patients treated with anti-tumor necrosis factor. Arthritis Care Res (Hoboken) 69(6):783–793. doi:10.1002/acr.23016
Barnabe C, Homik J, Barr SG, Martin L, Maksymowych WP (2014) The effect of different remission definitions on identification of predictors of both point and sustained remission in rheumatoid arthritis treated with anti-TNF therapy. J Rheumatol 41(8):1607–1613. doi:10.3899/jrheum.131451
Cook MJ, Diffin J, Scire CA, Lunt M, MacGregor AJ, Symmons DP, Verstappen SM (2016) Predictors and outcomes of sustained, intermittent or never achieving remission in patients with recent onset inflammatory polyarthritis: results from the Norfolk Arthritis Register. Rheumatology 55(9):1601–1609. doi:10.1093/rheumatology/kew210
Jayakumar K, Norton S, Dixey J, James D, Gough A, Williams P, Prouse P, Young A, Early Rheumatoid Arthritis S (2012) Sustained clinical remission in rheumatoid arthritis: prevalence and prognostic factors in an inception cohort of patients treated with conventional DMARDS. Rheumatology 51(1):169–175. doi:10.1093/rheumatology/ker250
Mohammed RH, Farahat F, Kewan HH, Bukhari MA (2015) Predictors of European League Against Rheumatism (EULAR) good response, DAS-28 remission and sustained responses to TNF-inhibitors in rheumatoid arthritis: a prospective study in refractory disease. Springerplus 4:207. doi:10.1186/s40064-015-0979-6
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, Healey LA, Kaplan SR, Liang MH, Luthra HS et al (1988) The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheumatol 31(3):315–324
Bae SC, Cook EF, Kim SY (1998) Psychometric evaluation of a Korean Health Assessment Questionnaire for clinical research. J Rheumatol 25(10):1975–1979
Kim MH, Cho YS, Uhm WS, Kim S, Bae SC (2005) Cross-cultural adaptation and validation of the Korean version of the EQ-5D in patients with rheumatic diseases. Qual Life Res 14(5):1401–1406
Stucki G, Liang MH, Stucki S, Bruhlmann P, Michel BA (1995) A self-administered rheumatoid arthritis disease activity index (RADAI) for epidemiologic research. Psychometric properties and correlation with parameters of disease activity. Arthritis Rheumatol 38(6):795–798
Fransen J, Welsing PMJ, De Keijzer RMH, Van Riel PLCM (2003) Disease activity scores using C-reactive protein: CRP may replace ESR in the assessment of RA disease activity. Ann Rheum Dis 62(Suppl 1):151
Wolfe F (2000) A reappraisal of HAQ disability in rheumatoid arthritis. Arthritis Rheumatol 43(12):2751–2761. doi:10.1002/1529-0131(200012)43:12<2751:AID-ANR15>3.0.CO;2-6
Wolfe F, Kleinheksel SM, Cathey MA, Hawley DJ, Spitz PW, Fries JF (1988) The clinical value of the Stanford Health Assessment Questionnaire Functional Disability Index in patients with rheumatoid arthritis. J Rheumatol 15(10):1480–1488
Callahan LF, Bloch DA, Pincus T (1992) Identification of work disability in rheumatoid arthritis: physical, radiographic and laboratory variables do not add explanatory power to demographic and functional variables. J Clin Epidemiol 45(2):127–138
van Nies JA, de Jong Z, van der Helm-van Mil AH, Knevel R, Le Cessie S, Huizinga TW (2010) Improved treatment strategies reduce the increased mortality risk in early RA patients. Rheumatology 49(11):2210–2216. doi:10.1093/rheumatology/keq250
Fleischmann R, van der Heijde D, Koenig AS, Pedersen R, Szumski A, Marshall L, Bananis E (2015) How much does Disease Activity Score in 28 joints ESR and CRP calculations underestimate disease activity compared with the Simplified Disease Activity Index? Ann Rheum Dis 74(6):1132–1137. doi:10.1136/annrheumdis-2013-204920
Gaujoux-Viala C, Mouterde G, Baillet A, Claudepierre P, Fautrel B, Le Loet X, Maillefert JF (2012) Evaluating disease activity in rheumatoid arthritis: which composite index is best? A systematic literature analysis of studies comparing the psychometric properties of the DAS, DAS28, SDAI and CDAI. Jt Bone Spine 79(2):149–155. doi:10.1016/j.jbspin.2011.04.008
Shaver TS, Anderson JD, Weidensaul DN, Shahouri SH, Busch RE, Mikuls TR, Michaud K, Wolfe F (2008) The problem of rheumatoid arthritis disease activity and remission in clinical practice. J Rheumatol 35(6):1015–1022
Sokka T, Hetland ML, Makinen H, Kautiainen H, Horslev-Petersen K, Luukkainen RK, Combe B, Badsha H, Drosos AA, Devlin J, Ferraccioli G, Morelli A, Hoekstra M, Majdan M, Sadkiewicz S, Belmonte M, Holmqvist AC, Choy E, Burmester GR, Tunc R, Dimic A, Nedovic J, Stankovic A, Bergman M, Toloza S, Pincus T, Questionnaires in Standard Monitoring of Patients With Rheumatoid Arthritis G (2008) Remission and rheumatoid arthritis: data on patients receiving usual care in twenty-four countries. Arthritis Rheumatol 58(9):2642–2651. doi:10.1002/art.23794
Forslind K, Hafstrom I, Ahlmen M, Svensson B, Group BS (2007) Sex: a major predictor of remission in early rheumatoid arthritis? Ann Rheum Dis 66(1):46–52. doi:10.1136/ard.2006.056937
Kristensen LE, Kapetanovic MC, Gulfe A, Soderlin M, Saxne T, Geborek P (2008) Predictors of response to anti-TNF therapy according to ACR and EULAR criteria in patients with established RA: results from the South Swedish Arthritis Treatment Group Register. Rheumatology 47(4):495–499. doi:10.1093/rheumatology/ken002
Castrejon I, Dougados M, Combe B, Fautrel B, Guillemin F, Pincus T (2016) Prediction of Remission in a French Early Arthritis Cohort by RAPID3 and other core data set measures, but not by the absence of rheumatoid factor, anticitrullinated protein antibodies, or radiographic erosions. J Rheumatol 43(7):1285–1291. doi:10.3899/jrheum.141586
Molina E, Del Rincon I, Restrepo JF, Battafarano DF, Escalante A (2015) Association of socioeconomic status with treatment delays, disease activity, joint damage, and disability in rheumatoid arthritis. Arthritis Care Res (Hoboken) 67(7):940–946. doi:10.1002/acr.22542
Thiele K, Huscher D, Bischoff S, Spathling-Mestekemper S, Backhaus M, Aringer M, Kohlmann T, Zink A, German Collaborative Arthritis C (2013) Performance of the 2011 ACR/EULAR preliminary remission criteria compared with DAS28 remission in unselected patients with rheumatoid arthritis. Ann Rheum Dis 72(7):1194–1199. doi:10.1136/annrheumdis-2012-201821
de Punder YM, Fransen J, Kievit W, Houtman PM, Visser H, van de Laar MA, van Riel PL (2012) The prevalence of clinical remission in RA patients treated with anti-TNF: results from the Dutch Rheumatoid Arthritis Monitoring (DREAM) registry. Rheumatology 51(9):1610–1617. doi:10.1093/rheumatology/kes078
Shahouri SH, Michaud K, Mikuls TR, Caplan L, Shaver TS, Anderson JD, Weidensaul DN, Busch RE, Wang S, Wolfe F (2011) Remission of rheumatoid arthritis in clinical practice: application of the American College of Rheumatology/European League Against Rheumatism 2011 remission criteria. Arthritis Rheumatol 63(11):3204–3215. doi:10.1002/art.30524
Acknowledgements
The authors thank the patients and their families for their participation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This research complied with the Helsinki Declaration. This study was approved by the Institutional Review Board of CNUH (I-2009-05-049) and informed consent was obtained at the time of registry enrollment.
Conflict of interest
The authors declare that they do not have conflict of interests.
Funding
This study was supported by Celltrion Korea and Bitgoeul Chonnam National University Hospital (BCRI16001-52).
Rights and permissions
About this article
Cite this article
Lee, KE., Choi, SE., Xu, H. et al. HAQ score is an independent predictor of sustained remission in patients with rheumatoid arthritis. Rheumatol Int 37, 2027–2034 (2017). https://doi.org/10.1007/s00296-017-3833-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-017-3833-z