Abstract
Vitamin D is a steroid hormone with pleiotropic effects. The association between serum 25-hydroxyvitamin D level [25(OH) D] and lupus nephritis are not clearly known. We aim to determine serum 25(OH) D levels in patients with inactive SLE, active SLE without lupus nephritis (LN) and active SLE with LN and to identify clinical predictor of vitamin D deficiency. One hundred and eight SLE patients were included. Patients were classified as Group (Gr) 1, 2 and 3 if they had SLE disease activity index (SLEDAI) <3, ≥3 but no LN and ≥3 with LN. Important baseline characteristics were collected. 25(OH) D was measured by high performance liquid chromatography (HPLC). SLEDAI in Gr1, Gr2 and Gr3 was 0.7 (0.9), 5.6 (2.3) and 9.2 (5.2), respectively. 43.5 % had vitamin D insufficiency and 29.6 % had vitamin D deficiency. Mean 25(OH) D in each groups was 28.3 (8.0), 26.7 (9.5) and 19.9 (7.6) ng/ml (p < 0.001 comparing Gr1 and 3) (p = 0.003 comparing Gr2 and 3). Vitamin D deficiency was found in 11.1, 22.2 and 55.6 % of Gr1, 2 and 3. Linear regression analysis found that 25(OH) D was significantly correlated with serum albumin (r = 0.28, p = 0.004), inversely correlated with SLEDAI (r = −0.22, p = 0.03) and urinary protein creatinine index (UPCI) (r = −0.28, p = 0.005), but not with sun exposure score, body mass index and estimated GFR. Only UPCI was significantly inversely correlated with 25(OH) D (p = 0.02) from multiple linear regression. LN was a significant predictor of vitamin D deficiency from multivariate logistic regression (OR 5.97; p = 0.006). Vitamin D deficiency and insufficiency was found in 93 and 86 % of LN with proteinuria ≥ and <500 mg/day. We conclude that SLE patients with LN have significantly lower vitamin D level than inactive SLE and active SLE without LN. Hence, nephritis is a significant predictor of vitamin D deficiency in SLE patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Investigations about the effect of vitamin D beyond bone health are increasing. These include the immunological effect of vitamin D on B lymphocyte, antigen presenting cell [1, 2] and cardiovascular effects [3]. The association between chronic kidney disease and vitamin D deficiency was demonstrated by the previous studies [4, 5]. Two recent randomized, controlled studies had demonstrated the benefit of vitamin D for reduction in proteinuria in diabetic nephropathy [6] and IgA nephropathy [7]. Previous studies had demonstrated lower vitamin D level in patients with SLE than age-match control [8]. Vitamin D deficiency is defined as serum 25(OH) D level less than 20 ng/ml [9]. The factors that may be associated with low vitamin D level in SLE patients are not clearly known. Previous studies showed that low vitamin D level in SLE patients was associated with high body mass index [10] and ethnic with dark skin color [11]. The association between SLE disease activity (SLEDAI) and serum 25(OH) D levels is one of the controversial issues according to inconsistent data from the earlier studies [8, 11, 12] which may be due to the unsolved confounding factors. Information regarding vitamin D level in SLE patients with lupus nephritis (LN) is limited. This study has focused on the association between 25(OH) D and SLE disease activity and the presence of lupus nephritis. The primary objective of this study was to determine serum 25(OH) D levels among inactive SLE, active SLE without LN and active SLE with LN. The secondary objective was to determine clinical predictors that had significant correlation with vitamin D deficiency.
Materials and methods
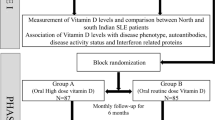
SLE patients fulfilling the 1997 revised ACR criteria for the diagnosis of SLE [13] who were currently followed up at the outpatient department were enrolled. All patients were older than 18 years and had provided informed consent for the study. Exclusion criteria were. (1) Patients who were taking vitamin D supplementation. (2) Patients who had chronic liver diseases. (3) Patients who had metabolic bone diseases. (4) Patients who had granulomatous diseases. (5) Patients who had malabsorption syndrome. (6) Patients who were currently taking drugs that might affect vitamin D level except for corticosteroid. The Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI2K) [14] was used to assess the disease activity. Lupus nephritis (LN) was diagnosed by: (a) the presence of proteinuria >0.5 g per 24 h or urine protein dipstick 3+ if quantitation was not performed or (b) the presence of any cellular casts [13]. Enroll patients were classified into 3 groups according to disease activity and the presence of lupus nephritis. Group 1 was the patients who had low disease activity (defined by SLEDAI2K <3) without LN. Group 2 was the patients who had moderate to high disease activity (defined by SLEDAI2K ≥3) without LN. Group 3 was the patients who had moderate to high disease activity (defined by SLEDAI2K ≥3) with LN. Important baseline characteristics were collected. These included age, sex, disease duration, body mass index (BMI), current and cumulative dose of corticosteroid. All participants were tested for urinalysis, urine protein creatinine index (UPCI), serum albumin, serum cholesterol, serum creatinine, estimated GFR (calculated by MDRD formula), serum complement and anti-dsDNA. All patients had to fill the questionnaire (modified from Hanwell et al.) [15] asking about duration of sun exposure and dressing style during the previous 7 days before enrollment. There were four choices for the time duration spending outdoor each day (1 ≤ 5 min, 2 = 5–10 min, 3 = 10–20 min, 4 ≥ 20 min) and four choices for skin exposure while staying outdoor (1 = face, 2 = face and hands, 3 = face, hands and arms, 4 = face, hands, arms and legs). The product of time spending outdoor multiplies by amount of skin exposure to sunlight for each day was calculated to create daily sun exposure score. The mean sun exposure score was determined with minimum score equal to 1 and maximum score equal to 16. Serum 25(OH) D level was measured by high performance liquid chromatography technique (HPLC) available from National Healthcare System Co., Ltd. Serum samples, calibrator and control materials were precipitated and extracted following the instruction manual of ClinRep® HPLC complete kit for serum 25(OH) D (RECIPE, Germany). 25(OH) D in extracted samples were analyzed by using high performance liquid chromatography (HPLC) equipped with UV detector (HPLC 1260, Agilent Technologies, USA). Both target compounds and internal standard were separated examined on the specific analytical column. For the quality control of testing, serum control materials in two different concentrations were used to control the accuracy of the analytical measurements. The technician who run test for 25(OH) D was kept blind from the patients’ history and clinical data. Vitamin D sufficiency, insufficiency and deficiency were defined as serum 25(OH) D level between 30–100, 20–29 and <20 ng/ml, respectively [9]. Severe vitamin D deficiency was defined as 25(OH) D < 10 ng/ml [16]. This study was approved by the institutional review boards of the investigating hospital.
Statistical analysis
We postulated that vitamin D level in patients with active SLE and lupus nephritis was lower than patients with inactive SLE and active SLE without LN. According to the previous study, mean difference of vitamin D level between patients with inactive SLE and active SLE was −27.2 ng/ml [11]. Hence, the estimated sample size of 108 patients would have 80 % power to detect mean difference among each group at 10 ng/ml [17]. Mean difference of vitamin D level among three groups was determined by using ANOVA with post hoc test or Kruskal–Wallis test as appropriated for comparing all pair of mean. Continuous variables were expressed by mean and standard deviation (SD). Proportion of SLE patients in each group classified by vitamin D status was shown in percent. The correlation between 25(OH) D level and predicted variable was examined by Pearson’s correlation coefficient (r) and regression analysis. Potential confounder was adjusted by multiple linear regression. Univariate logistic regression was used to determine potential predictors of vitamin D deficiency. Those variables that were significant at p value ≤0.20 on univariate were included in the multivariate logistic regression analysis to identify final predictor of vitamin D deficiency.
Results
One hundred and eight patients were included in the analysis, 103 patients were female. Mean age (SD) and disease duration was 35.2 (11.09) and 7.74 (8.07) years, respectively. Demographic data of patients in each group were shown in Table 1. Median and range of cumulative prednisolone dosage of all patients were 10,950 mg and 150–54,750 mg, respectively. Mean serum 25(OH) D level in Gr1, Gr2 and Gr3 were 28.25 (8.00), 26.74 (9.54) and 19.96 (7.6) ng/ml, respectively (Fig. 1). Mean serum 25(OH) D in each group was compared by using ANOVA with post hoc test. The result showed that the mean difference of 25(OH) D levels between Gr 1 and Gr 3 was 8.29 (2.00); 95 % CI (3.53, 13.05): p < 0.001. The mean difference of 25(OH) D between Gr 2 and Gr 3 was 6.79 (1.99); 95 % CI (2.06, 11.51): p = 0.003.
Only 29 of 108 patients (26.85 %) had vitamin D adequacy. Thirty-three of 36 (91.66 %) SLE patients with lupus nephritis had vitamin D insufficiency or deficiency. Table 2 showed proportion of vitamin D status in three study groups. Pearson’s correlation showed that serum 25(OH) D level was significantly correlated with serum albumin (r = 0.28, p = 0.004), inversely correlated with SLEDAI (r = −0.22, p = 0.03) and inversely correlated with UPCI (r = −0.28, p = 0.005) (Fig. 2a–c). The adjusted SLEDAI score was calculated by deduction of scores attributed from nephritis, specifically: urinary cast, proteinuria, hematuria and pyuria from original SLEDAI. Subsequently, we found no correlation between 25(OH) D and adjusted SLEDAI score (r = 0.139, p = 0.155). 25(OH) D was poorly correlated with sun exposure score (r = 0.008, p value 0.93), BMI (r = 0.015, p = 0.90), eGFR (r = 0.04, p = 0.70). Multiple linear regression was used for adjusting the potential confounders including current prednisolone dosage, serum albumin, SLEDAI, eGFR and UPCI. The result showed that only UPCI was significantly inversely correlated with serum 25(OH) D level with a standardized coefficient beta of −0.31 (p = 0.015).
Plot of simple linear regression. a Serum 25(OH) D level was significantly correlated with serum albumin (r = 0.28, p = 0.004). b Serum 25(OH) D level was significantly inversely correlated with SLEDAI (r = −0.22, p = 0.03). c Serum 25(OH) D level was significantly inversely correlated with UPCI (r = −0.28, p = 0.005)
Logistic regression was used to identify potential and final predictors of vitamin D deficiency. From univariate analysis, serum albumin was found to be protective of vitamin D deficiency [OR 0.29; 95 % CI (0.14, 0.61): p = 0.001]. In contrast, lupus nephritis was found to be a hazard predictor of vitamin D deficiency [OR 6.25: 95 % CI (2.53, 15.43): p ≤ 0.001]. Cumulative prednisolone dosage more than 4,562 mg (interquartile range of median cumulative prednisolone dosage) was associated with the composite end point of vitamin D insufficiency, vitamin D deficiency or severe vitamin D deficiency [OR 4.50; 95 % CI (1.14,17.73): p = 0.032]. In addition, we have found that prednisolone usage was a predictor of severe vitamin D deficiency as defined by 25(OH) D < 10 ng/ml [OR 10.0; 95 % CI (1.24, 80.88): p = 0.03]. However, multivariate logistic regression analysis showed that only lupus nephritis was a significant predictor of vitamin D deficiency [OR 5.97; 95 % CI (1.68, 21.26): p = 0.006] (Table 3).
Subgroup analysis was done in SLE patients with lupus nephritis (group 3) to determine the vitamin D status among patients with different amount of proteinuria. Table 4 showed the percentage of patients who had vitamin D deficiency, vitamin D insufficiency and vitamin D adequacy among patients with several level of proteinuria. Vitamin D deficiency and vitamin D insufficiency were common in LN patients with all level of proteinuria. Overall, vitamin D deficiency and insufficiency were found in 93 % of LN patients with proteinuria ≥500 mg per day and 86 % of LN patients with proteinuria <500 mg per day, respectively.
Discussion
The high prevalence of vitamin D deficiency in SLE mostly came from temperate zone which range between 62.2 and 67.7 % [8, 18]. Thailand is situated near equator area where sun shines almost all year round causing less seasonal fluctuation compares with countries in temperate area. The average duration of the day time in Bangkok is 4.7–8.3 hours per day (Thai Meteorological Department, 2008). The result from our study had demonstrated that the prevalence of vitamin D insufficiency or deficiency from our population is also high (73.1 %). This finding indicated that vitamin D deficiency is the global problem. Even though, the ethnic with dark skin color was claimed to be one of the risk factors of vitamin D deficiency [11]. The skin color of Thai population was categorized into skin type IV (brown) to type V (dark brown) by Fitzpatrick classification scale. The high prevalence of vitamin D deficiency in Thai population may indicate that vitamin D deficiency can also be found in patients with brown and dark brown skin color. The causes of vitamin D deficiency in SLE patients are not clearly known. Some contributing factors of vitamin D deficiency in SLE patients included sun avoidance [19], obesity [16], ethnic with dark skin color [11], use of glucocorticoids, anti-malarials and the presence of anti-vitamin D antibodies [20, 21]. The inversely association between SLE disease activity index (SLEDAI) and low 25(OH) D level is another interested topic. Borba et al. conducted a cross-sectional study of 36 SLE patients comparing mean vitamin D level between three different groups according to SLEDAI categorized by SLEDAI <3, SLEDAI >12, and normal control which aimed to determine effect of disease activity on bone metabolism in patients with SLE. The results showed that 25(OH) D levels were significantly lower in patients with active disease group (SLEDAI >12). 25(OH) D level was also shown to be inversely related with SLEDAI (r = −0.65, p < 0.001) [11]. Mok et al. [22] found that 25(OH) D level was inversely correlated with clinical SLE activity (r = −0.26, p < 0.001) and anti-dsDNA level (r = −0.13, p = 0.02). A recent study of Bonakdar et al. [23] reported that high disease activity index (British Isles Lupus Assessment Group; BILAG) in new cases of SLE patients was inversely correlated with serum 25(OH) D (r = −0.486, p = 0.001). However, another study reported from Toloza et al. [8] showed no correlation between vitamin D level and disease activity. In addition, from a recent study of Bogaczewicz et al. [24], which aim to identify relationships between serum vitamin D and vitamin D auto antibodies in 49 SLE patients found that SLE patients with renal disease had lower 25(OH) D level than SLE patients who had no renal disease. Since nephritis is one of the major organ involvement of SLE. The presence of nephritis can lead to high SLEDAI either by the presence of proteinuria, several type of casts or cellular sediment. We hypothesize that disparities of the correlation between 25(OH) D and SLEDAI among prior investigations may be attributed from the presence of lupus nephritis. We found that SLE patients with lupus nephritis had significantly lower mean serum 25(OH) D level than inactive SLE and active SLE without lupus nephritis which had confirmed our hypothesis. Interestingly, we have found no significant difference of mean serum 25(OH) D between inactive SLE and active SLE without lupus nephritis. Hence, the impact of lupus nephritis on low 25(OH) D levels has been shown from our study.
Our study found that serum 25(OH) D level is inversely correlated with SLEDAI. This supports the findings from Borba et al. and Mok et al. We have then examined the relative impact of systemic disease activities versus nephritis on the occurrence of vitamin D deficiency. This was done by calculating adjusted SLEDAI score (see definition in Table 3). We found no correlation between adjusted SLEDAI score and serum 25(OH) D. In addition, after, we had compared adjusted SLEDAI score with other factors including nephritis by multivariate logistic regression. The results showed that adjusted SLEDAI was not a significant predictor of vitamin D deficiency (Table 3).
Our additional findings that 25(OH) D was inversely correlated with UPCI need to be addressed. Robinson et al. had evaluated the relationships between vitamin D, proteinuria and disease activity in 37 pediatric systemic lupus erythematosus patients. They found the correlation between serum 25(OH) D level and serum albumin and inversely correlated with UPCI (r = −0.60, p < 0.001). In addition, they had found an inverse correlation between serum 25(OH) D level and urinary vitamin D binding protein (VDBP) (r = −0.63, p < 0.001) [25]. This lead to a possibility that low serum vitamin D level might be related with loss of urinary VDBP. Our result, however, showed that low serum 25(OH) D was found in 86 % of lupus nephritis patients with low grade proteinuria (urine protein <0.5 g per day). Low 25(OH) D in SLE with lupus nephritis can thus be attributed from factor other than losing of VDBP via proteinuria. Agarwal et al. [27] found that vitamin D deficiency could cause reduction in urine creatinine generation in patients with chronic kidney disease. This could lead to high urine protein to creatinine (UPCI) ratio in our lupus nephritis patient who had vitamin D deficiency. On the other hand, low serum 25(OH) D level may be a marker of active disease and a cause of proteinuria. A recent study had demonstrated that vitamin D supplement could lead to reduction in proteinuria via suppression of renin angiotensin aldosterone system [26]. In addition, reduction in proteinuria had been demonstrated by vitamin D supplementation from previous randomized, controlled trial in model of diabetic nephropathy [6] and IgA nephropathy [7]. Further studies are required to identify the causal relationship between low serum 25(OH) D level and proteinuria in SLE patients with lupus nephritis.
The presence of nephritis in patients with SLE may be associated with low vitamin D level. This notion is supported by our findings that SLE patients with lupus nephritis had almost 6 times more risk of vitamin D deficiency than SLE patients without lupus nephritis (Table 3). The high prevalence of vitamin D insufficiency and deficiency in SLE patients with proteinuria lower than 0.5 g per day suggested that low vitamin D level may be associated with the presence of nephritis through immunological pathway and not proteinuria per se. Various immune cells including monocyte, macrophages, dendritic cells, B lymphocyte and T lymphocyte had been reported to express vitamin D receptors [28]. The direct impact of active SLE diseases on the changes of 25(OH) D metabolisms still remains to be further investigated.
Unlike the previous study, we found no association between 25(OH) D and obesity. This may be related with the low prevalence of obese patients in our study (6.5 %). Skversky et al. [16] had conducted a cross-sectional study using the National Health and Nutrition Examination Survey (NHANES): 2001–2006 data that aimed to evaluate the association between severe vitamin D deficiency and oral steroid usage. Our study had confirmed that vitamin D insufficiency, vitamin D deficiency or severe vitamin D deficiency were significantly associated with high cumulative prednisolone dosage. We had also shown that severe vitamin D deficiency was ten times more common in steroid users compared with steroid nonusers. Regarding the sun exposure, Hanwell et al. [15] found that high sun exposure score in summer was correlated with elevated 25(OH) D level in healthy individuals. In contrast, our study in SLE patients, however, has found no correlation between sun exposure score and 25(OH) D level. This suggested that the impact of sun exposure on serum 25(OH) D levels in SLE patients is weaker than other critical factors. Other important factor that was shown to be important predictor of low serum 25(OH) D is the baseline renal function (estimated GFR). LaClair et al. had studied in 201 subjects from 12 geographically diverse locations across the US and aimed to find the prevalence of calcidiol deficiency in chronic kidney disease patients. The authors reported low mean calcidiol level in the subjects with moderate and severe CKD (mean eGFR 27 ± 11 ml/min) [5]. Our study found no correlation between serum 25(OH) D and eGFR. This may be related with the fact that almost all of our studied population had eGFR >30 ml/min. In fact, there was only one patient with eGFR lower than 30 ml/min and the serum 25(OH) D level in this patient was found to be low (data not shown).
Our study had some limitation. From the questionnaire, we found that 48.6 % of our SLE patients frequently used sunscreen as sun protection. However, we could not determine the proportion of patients who used SPF >30 and proportion of patients who applied adequate amount of sunscreen (more than 2 mg of cream per square centimeter of skin surface). Hence, we could not determine the precise effect of sunscreen use and vitamin D deficiency in our patients.
In summary, we have shown the high prevalence of vitamin D deficiency in SLE patients. SLE patients with lupus nephritis had significantly lower vitamin D level than inactive SLE and active SLE without lupus nephritis. This low level of 25(OH) D was inversely correlated with UPCI. However, high prevalence of low 25(OH) D levels was also found in lupus nephritis with proteinuria lower than 0.5 g per day. We conclude that lupus nephritis is a significant predictor of vitamin D deficiency in SLE patients. Further studies are required to clarify the causal relationship between low vitamin D level and lupus nephritis. In addition, the impact of low 25(OH) D levels on cardiovascular diseases and other immunological function in SLE patients needs to be determined. Still, the effect of vitamin D supplement on certain interested outcomes such as proteinuria and SLE disease activities remains to be further investigated.
References
Chen S, Sims GP, Xiao XC, Yue YG, Lipsky PE (2007) Modulatory effects of 1,25-dihydroxyvitamin D3 on human B cell differentiation. J Immunol 179(3):1634–1647
Haroon M, Fitzgerald O (2012) Vitamin D and its emerging role in immunopathology. Clin Rheumatol 31(2):199–202
Kamen D, Aranow C (2008) Vitamin D in systemic lupus erythematosus. Curr Opin Rheumatol 20(5):532–537
de Boer IH, Ioannou GN, Kestenbaum B, Brunzell JD, Weiss NS (2007) 25-Hydroxyvitamin D levels and albuminuria in the third national health and nutrition examination survey (NHANES III). Am J Kidney Dis 50(1):69–77
LaClair RE, Hellman RN, Karp SL, Kraus M, Ofner S, Li Q, Graves KL, Moe SM (2005) Prevalence of calcidiol deficiency in CKD: a cross-sectional study across latitudes in the United States. Am J Kidney Dis 45(6):1026–1033
de Zeeuw D, Agarwal R, Amdahl M, Audhya P, Coyne D, Garimella T, Parving HH, Pritchett Y, Remuzzi G, Ritz E, Andress D (2010) Selective vitamin D receptor activation with paricalcitol for reduction of albuminuria in patients with type 2 diabetes (VITAL study): a randomised controlled trial. Lancet 376(9752):1543–1551
Liu LJ, Lv JC, Shi SF, Chen YQ, Zhang H, Wang HY (2012) Oral calcitriol for reduction of proteinuria in patients with IgA nephropathy: a randomized controlled trial. Am J Kidney Dis 59(1):67–74
Toloza SMA, Cole DEC, Gladman DD, Ibañez D, Urowitz MB (2010) Vitamin D insufficiency in a large female SLE cohort. Lupus 19(1):13–19
Holick MF (2007) Vitamin D deficiency. N Engl J Med 357(3):266–281
Wright TB, Shults J, Leonard MB, Zemel BS, Burnham JM (2009) Hypovitaminosis D is associated with greater body mass index and disease activity in pediatric systemic lupus erythematosus. J Pediatr 155(2):260–265
Borba VZC, Vieira JGH, Kasamatsu T, Radominski SC, Sato EI, Lazaretti-Castro M (2009) Vitamin D deficiency in patients with active systemic lupus erythematosus. Osteoporos Int 20(3):427–433
Kim HA, Sung JM, Jeon JY, Yoon JM, Suh CH (2011) Vitamin D may not be a good marker of disease activity in Korean patients with systemic lupus erythematosus. Rheumatol Int 31(9):1189–1194
Hochberg MC (1997) Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40(9):1725
Uribe AG, Vila LM, McGwin G Jr, Sanchez ML, Reveille JD, Alarcon GS (2004) The systemic lupus activity measure-revised, the Mexican systemic lupus erythematosus disease activity index (SLEDAI), and a modified SLEDAI-2K are adequate instruments to measure disease activity in systemic lupus erythematosus. J Rheumatol 31(10):1934–1940
Hanwell HE, Vieth R, Cole DE, Scillitani A, Modoni S, Frusciante V, Ritrovato G, Chiodini I, Minisola S, Carnevale V (2010) Sun exposure questionnaire predicts circulating 25-hydroxyvitamin D concentrations in Caucasian hospital workers in southern Italy. J Steroid Biochem Mol Biol 121(1–2):334–337
Skversky AL, Kumar J, Abramowitz MK, Kaskel FJ, Melamed ML (2011) Association of glucocorticoid use and low 25-hydroxyvitamin D levels: results from the National Health and Nutrition Examination Survey (NHANES): 2001–2006. J Clin Endocrinol Metab 96(12):3838–3845
Haarburger D, Hoffman M, Erasmus RT, Pillay TS (2009) Relationship between vitamin D, calcium and parathyroid hormone in Cape Town. J Clin Pathol 62(6):567–569
Wu PW, Rhew EY, Dyer AR, Dunlop DD, Langman CB, Price H, Sutton-Tyrrell K, McPherson DD, Edmundowicz D, Kondos GT, Ramsey-Goldman R (2009) 25-Hydroxyvitamin D and cardiovascular risk factors in women with systemic lupus erythematosus. Arthritis Care Res 61(10):1387–1395
Norval M, Wulf HC (2009) Does chronic sunscreen use reduce vitamin D production to insufficient levels? Br J Dermatol 161(4):732–736
Le Goaziou MF, Contardo G, Dupraz C, Martin A, Laville M, Schott-Pethelaz AM (2011) Risk factors for vitamin D deficiency in women aged 20–50 years consulting in general practice: a cross-sectional study. Eur J Gen Pract 17(3):146–152
Carvalho JF, Blank M, Kiss E, Tarr T, Amital H, Shoenfeld Y (2007) Anti-vitamin D, vitamin D in SLE: preliminary results. Ann N Y Acad Sci 1109:550–557
Mok CC, Birmingham DJ, Ho LY, Hebert LA, Song H, Rovin BH (2012) Vitamin D deficiency as marker for disease activity and damage in systemic lupus erythematosus: a comparison with anti-dsDNA and anti-C1q. Lupus 21(1):36–42
Bonakdar ZS, Jahanshahifar L, Jahanshahifar F, Gholamrezaei A (2011) Vitamin D deficiency and its association with disease activity in new cases of systemic lupus erythematosus. Lupus 20(11):1155–1160
Bogaczewicz J, Sysa-Jedrzejowska A, Arkuszewska C, Zabek J, Kontny E, McCauliffe D, Wozniacka A (2012) Vitamin D status in systemic lupus erythematosus patients and its association with selected clinical and laboratory parameters. Lupus 21(5):477–484
Robinson AB, Thierry-Palmer M, Gibson KL, Rabinovich CE (2012) Disease activity, proteinuria, and vitamin D status in children with systemic lupus erythematosus and juvenile dermatomyositis. J Pediatr 160(2):297–302
Freundlich M, Quiroz Y, Zhang Z, Zhang Y, Bravo Y, Weisinger JR, Li YC, Rodriguez-Iturbe B (2008) Suppression of renin-angiotensin gene expression in the kidney by paricalcitol. Kidney Int 74(11):1394–1402
Agarwal R, Hynson JE, Hecht TJ, Light RP, Sinha AD (2011) Short-term vitamin D receptor activation increases serum creatinine due to increased production with no effect on the glomerular filtration rate. Kidney Int 80(10):1073–1079
Baeke F, Takiishi T, Korf H, Gysemans C, Mathieu C (2010) Vitamin D: modulator of the immune system. Curr Opin Pharmacol 10(4):482–496
Acknowledgments
This study was supported by The Research Fund of Rajavithi Hospital.
Conflict of interest
The authors have no disclosures or financial support relevance to this study to report.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sumethkul, K., Boonyaratavej, S., Kitumnuaypong, T. et al. The predictive factors of low serum 25-hydroxyvitamin D and vitamin D deficiency in patients with systemic lupus erythematosus. Rheumatol Int 33, 1461–1467 (2013). https://doi.org/10.1007/s00296-012-2537-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-012-2537-7