Abstract
Vitamin D is a pleiotrophic hormone with immunoregulatory properties. Low levels of vitamin D have been discovered in various autoimmune diseases. Here, we investigated serum vitamin D levels in Koreans with systemic lupus erythematosus (SLE) and examined whether levels correlate with disease activity of SLE. Blood samples were prospectively collected from patients with SLE (n = 104) and normal controls (NC, n = 49) during the spring from March to May 2008. The level of serum 25-hydroxyvitamin D (25(OH)D3) was measured by radioimmunoassay. The serum 25(OH)D3 levels of patients with SLE (42.49 ± 15.08 ng/ml) were significantly lower than NC (52.72 ± 15.19 ng/ml, P < 0.001). Additionally, 17 patients with SLE (16.3%) had vitamin D insufficiency, while two NC had vitamin D insufficiency (4.1%). The risk of vitamin D insufficiency was 4.6-fold increased in SLE (P = 0.032). The serum 25(OH)D3 levels, adjusted with BMI, were positively correlated only with hemoglobin (β = 0.256, P = 0.018) and serum complement 3 (β = 0.365, P = 0.002). Serum vitamin D levels were lower, and vitamin D insufficiency was more common in Korean patients with SLE, however, our study demonstrated that vitamin D levels might not be a good marker of disease activity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vitamin D is a steroid hormone that plays a crucial role in calcium metabolism and bone homeostasis. Although vitamin D is contained in food, dietary intake alone supplies only 20% of the body’s requirements. The primary source of vitamin D is de novo synthesis in the skin, and the conversion of 7-dehydrocholesterol to pre-vitamin D3 by means of solar ultraviolet B radiation. Vitamin D3 undergoes a 25-hydroxylation in the liver, with the resulting product, 25-OH-vitamin D3 [25(OH)D3], being the primary circulating form of vitamin D. The fully active form, 1,25(OH)2D3, is synthesized in the kidneys by the 25(OH) vitamin D-1α hydroxylase [1].
The primary metabolic effects of 1,25(OH)2D3 are mediated through interaction with vitamin D receptors (VDRs). The identification of VDRs on immune cells, and the discovery that activated dendritic cells produce 1,25(OH)2D3 suggested that vitamin D could exert immunoregulatory effects [2]. Quiescent CD4+T cells express VDRs at low concentration, which increases fivefold after their activation. The effects of 1,25(OH)2D3 on acquired antigen-specific immune responses are characterized by inhibition of T-lymphocyte proliferation, particularly of the Th1 arm [3–5]. The addition of 1,25(OH)2D3 leads to decreased secretion of IL-2 and IFN-γ by CD4 T cells and promotes IL-5 and IL-10 production, which further shifts the T cell response toward Th2 dominance [2]. Interestingly, vitamin D has been shown to inhibit antibody secretion and autoantibody production in B cells [6].
The evidence linking vitamin D status as a potential environmental factor involved in autoimmune disease continues to accumulate. Indeed, there is a known link between vitamin D and insulin-dependent diabetes mellitus, multiple sclerosis, inflammatory bowel diseases, and rheumatoid arthritis [7, 8]. In patients with systemic lupus erythematosus (SLE), the prevalence of vitamin D deficiency/insufficiency has been reported to vary widely from 8 to 67% [9–12]. Some studies have documented an association between higher disease activity and a low level of vitamin D [12, 13]. Moreover, a significant negative correlation between 25(OH)D3 and Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) was noted in European patients [13]. However, no association between disease activity and 25(OH)D3 was observed in other studies [14–16].
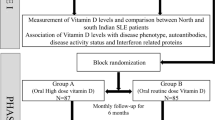
Previous studies have suggested a relationship between low serum levels of vitamin D and SLE; however, the association between vitamin D and disease activity in SLE remains controversial. Therefore, we conducted a prospective study to evaluate vitamin D levels and the prevalence of vitamin D deficiency/insufficiency in Korean patients with SLE. In addition, we examined the potential relationship between vitamin D levels with known markers of disease activity in SLE.
Materials and methods
Subjects
One hundred four female patients with SLE were enrolled in this study. All participants met the revised criteria of the American College of Rheumatology (ACR) for classification of SLE [17] and were being followed by the Department of Rheumatology at Ajou University Hospital in Suwon, Korea. In addition, 49 healthy females were recruited as normal controls (NC). Serum samples were prospectively collected for the measurement of 25(OH)D3 and antichromatin antibodies. All blood samples were kept at −20°C immediately upon collection until analysis.
To exclude factors influencing vitamin D level, our study obtained samples from female patients with SLE and female NC during the spring from March to May, 2008. Patients with SLE, who were pregnant, had serum aspirate aminotransferase levels or serum alanine aminotransferase levels that were elevated by more than twofold of the upper limit of normal, had serum creatinine level >1.4 mg/ml, or were taking medicine influencing vitamin D level were excluded. Also, the 25(OH)D3 levels were adjusted with BMI.
Information regarding the medical history, clinical symptoms, and physical examinations were registered in a database at the time of serum sampling. Each patient was also assayed for blood cell count, routine chemistry, urinalysis, complement, and anti-dsDNA antibody. Disease activity of SLE was evaluated according to the SLEDAI score [18]. In addition, the disease damage was assessed according to the Systemic Lupus International Collaborating Clinics/American College of Rheumatology (SLICC/ACR) damage index [19]. All subjects provided informed consent prior to participation, and the study was regulated by the Institutional Review of Board of our hospital.
25(OH)D3 and antichromatin antibodies assay
The 25(OH)D3 levels were determined by the Bio-Line 25(OH)D3-Ria CT kit (Bio-Line S.A., Belgium), a immunoradiometric assay, according to the manufactures’ instructions. Serum 25(OH)D3 levels <30 and <10 ng/ml were defined as vitamin D insufficiency and vitamin D deficiency, respectively. The interassay coefficient of variation (CV) of 25(OH)D3 was 3.3%, and the intraassay CV of 25(OH)D3 was 5.2%.
The level of antichromatin antibodies was measured by in-house enzyme-linked immunosorbent assay (ELISA) previously described and levels expressed as arbitrary unit (AU) [20].
Statistical analysis
The statistical analysis was conducted using the software SPSS, version 13.0 (Chicago, IL). The data were expressed as mean ± SD. A P value of <0.05 was regarded as significant. Serum 25(OH)D3 results of patients and NC were tested for differences by an independent sample t-test. Power of 93% was calculated in 25(OH)D3 between two groups. Chi-square test was used for comparison of the frequency of vitamin D deficiency/insufficiency between patients with SLE and NC. Mann–Whitney U test was used for comparison of serum 25(OH)D3 levels according to the clinical manifestations in SLE. Correlation between disease activity markers and serum 25(OH)D3 levels was calculated with logistic regression analysis by controlling BMI.
Results
Serum 25(OH)D3 levels in study groups
Table 1 summarizes the clinical features of the two study groups. The mean age of the patients with SLE was 36.21 ± 10.21, while that of the NC was 35.33 ± 6.18. There were no significant differences in age, weight, height, and body mass index (BMI) between groups.
The serum 25(OH)D3 levels in the SLE and the NC are shown in Fig. 1. The 25(OH)D3 was 42.49 ± 15.08 ng/ml in the patients with SLE and 52.72 ± 15.19 ng/ml in the NC. The serum 25(OH)D3 was lower in the SLE than the NC (P < 0.001).
Seventeen of the patients with SLE (16.3%) had vitamin D insufficiency, while only two NC had vitamin D insufficiency (4.1%) (Table 2). One of the patients with SLE (1.0%) had vitamin D deficiency, but none of the NC had vitamin D deficiency. The frequency of vitamin D insufficiency was significantly higher in the patients with SLE than in the NC (P = 0.032). Furthermore, the risk of vitamin D insufficiency was increased in Korean SLE when compared to the NC (relative risk (RR) 4.6, 95% confidence interval (CI) 1.0–20.7).
Comparison of serum 25(OH)D3 levels according to the clinical manifestations in SLE
The primary clinical manifestations of SLE observed at the time of serum sampling included photosensitivity (17.3%), arthritis (21.2%), and malar rash (13.5%). The level of anti-dsDNA antibody was 14.1 ± 23.5 IU/ml, and the level of complement 3 was 100.9 ± 28.5 mg/dl. The level of antichromatin antibody was 40.9 ± 33 AU. The SLEDAI was 2.82 ± 2.82, and the SLICC/ACR DI was 0.09 ± 0.32. Their daily glucocorticoids dose was 4.21 ± 4.65 mg prednisolone equivalent. The comparisons of serum 25(OH)D3 levels according to the clinical manifestations of SLE revealed no significant differences (data not shown). In addition, there were no significant differences in the clinical manifestations of patients with SLE on the basis of vitamin D insufficiency (data not shown).
It has been suggested that corticosteroids and hydroxychloroquine could influence the serum 25(OH)D3 levels. The 25(OH)D3 was 37.38 ± 12.02 ng/ml in the patients with SLE taking corticosteroids and 44.10 ± 15.65 ng/ml in those who were corticosteroid free. However, we found no significant differences of 25(OH)D3 levels between patients with SLE taking corticosteroids and those not. Finally, there was no significant correlation between 25(OH)D3 level and the dose of corticosteroids (data not shown). Also, the serum 25(OH)D3 levels were not different between patients with SLE taking hydroxychloroquine (41.67 ± 14.09 ng/ml) and those not (52.26 ± 23.11 ng/ml).
Correlation between disease activity markers and serum 25(OH)D3 level in SLE
The correlation between disease activity markers and the serum 25(OH)D3 levels is shown in Table 3. A positive correlation was found between the 25(OH)D3 level and the hemoglobin (β = 0.256, P = 0.018). Also, the serum 25(OH)D3 levels were correlated positively with complement 3 (β = 0.365, P = 0.002). However, no correlation was found between 25(OH)D3 and other disease activity markers such as antichromatin antibody, anti-dsDNA antibody, and SLEDAI.
Discussion
To examine potential relationships between vitamin D and disease activity in Korean patients with SLE, we evaluated the levels of vitamin D and compared them with clinical features and markers of disease activity. The serum 25(OH)D3 levels of patients with SLE were significantly lower than the levels of NC. Seventeen patients with SLE (16.3%) had vitamin D insufficiency, indicating that the risk of vitamin D insufficiency may be 4.6-fold higher in patients with SLE compared to NC (RR 4.6, 95% CI 1.0–20.7, P = 0.032). However, the comparisons of serum 25(OH)D3 levels according to the clinical manifestations of SLE revealed no significant differences. The serum 25(OH)D3 levels were positively correlated only with hemoglobin and serum complement 3.
The first study conducted to measure levels of vitamin D in patients with SLE reported a deficiency of 1,25(OH)2D3 levels in seven of 12 adolescents receiving corticosteroids [21]. Thereafter, several studies were conducted to evaluate the association between serum vitamin D levels and SLE. These studies revealed a high prevalence of vitamin D insufficiency in patients with SLE [10, 11, 15, 22]. A case–control study of 25(OH)D3 and 1,25(OH)2D3 in patients with SLE, patients with rheumatoid arthritis (RA), patients with osteoarthritis (OA), and controls revealed that the 25(OH)D3 levels in patients with SLE were significantly lower than in patients with OA and controls, but that there was no difference in 1,25(OH)2D3 levels [10]. A recent study showed 25(OH)D3 levels in a number of autoimmune diseases including multiple sclerosis, myositis, RA, autoimmune thyroid disease, and SLE [15]. Patients with SLE had a significantly lower 25(OH)D3 level than that of European controls. These results are consistent with the results of the present study, although the mean 25(OH)D3 level in our patients with SLE was higher than previous studies. The reason for the higher 25(OH)D3 levels in the present study is not clear; however, the difference may be explained by sampling during different seasons as well as ethnic background. All sampling in our study was conducted during spring, whereas sampling was conducted throughout the year in some previous studies. Indeed, one study revealed that higher levels of vitamin D were measured in the summer and fall than in the winter and spring [23]. Finally, a previous report demonstrated that vitamin D levels varied according to ethnicity [12].
Photosynthesis of vitamin D is dependent on the intensity of ultraviolet radiation and is affected by altitude, season, and time of day. Reduced exposure to sunlight, aging, heavy clothing, darker skin color, and the use of sunscreen also limit the cutaneous generation of vitamin D [24]. In patients with SLE, photosensitivity is a key feature of SLE, and the resultant avoidance of sun exposure may result in impaired vitamin D metabolism. Two previous studies reported that photosensitivity predicted vitamin D insufficiency [12, 16]. In the present study, there was no difference of 25(OH)D3 level according to photosensitivity. This result can be explained by the education of sun protection in all patients with SLE, enrollment of patients with mild disease activity, and sampling in spring; however, the patients were not asked about their sun exposure time or use of sunscreen.
One-hydroxylation is essential to activate 25(OH)D3 vitamin D, a step carried out by the kidney that can be potentially compromised by the development of significant renal disease in patients with SLE. In addition, it has been suggested that there is an association between vitamin D deficiency and lupus nephritis [12]. However, no association between 25(OH)D3 and renal disease was observed in our study. We suggest that this discrepancy is due to the exclusion of patients with SLE who had serum creatinine level >1.4 mg/ml.
Chronic corticosteroids use may result in altered metabolism of vitamin D, although there is contradictory evidence [25, 26]. One study demonstrated that the daily dose of corticosteroids was negatively correlated with the level of 25(OH)D3 [25]. However, another study reported that the maintenance of normal serum levels of 25(OH)D3 was not altered by chronic moderate dose corticosteroids therapy [26]. In the present study, there were no significant differences of 25(OH)D3 levels between patients taking corticosteroids and those who were not taking corticosteroids, probably because of our patients taking low-dose corticosteroids (4.21 mg/d prednisolone equivalent).
Patients with SLE often take hydroxychloroquine, which has been suspected to reduce the conversion of 25(OH)D3 to the more biologically active 1,25(OH)2D3 [27]. Lower 1,25(OH)2D3 levels was reported in patients with lupus treated with hydroxychloroquine, although circulating 25(OH)D3 levels did not differ. However, a recent study found that patients receiving anti-malarial treatment had higher levels of 25(OH)D3 and were less likely to have critically low vitamin D levels [16]. Serum 25(OH)D3 levels of our patients with lupus taking hydroxychloroquine were not different from those who were not. However, there is a need of further study because of the majority of our patients taking hydroxychloroquine.
A recent study investigated the prevalence of vitamin D deficiency/insufficiency in patients with undifferentiated connective tissue disease (UCTD). During 2.3 years follow-up, 21.7% of patients with UCTD developed into well-established connective tissue disease (CTD) including SLE. Patients who progressed into CTDs had lower vitamin D levels [28]. These results suggest that vitamin D deficiency in patients with UCTD may play a role in the subsequent progression into well-defined CTDs. However, a large epidemiological study involving >180,000 women from the Nurses’ Health Study did not find any association between vitamin D intake and the risk of developing either SLE or RA [29]. Therefore, the role of vitamin D deficiency/insufficiency in the pathogenesis of SLE is far from clear.
Additionally, the relationship of vitamin D deficiency/insufficiency and disease activity that has been reported in previous studies is controversial. For example, a significant negative correlation between 25(OH)D3 serum levels and European Consensus Lupus Activity Measurement (ECLAM) and SLEDAI was demonstrated in European patients [13]. However, another study revealed no association between 25(OH)D3 levels and SLE disease activity [10]. Furthermore, a recent study reported that both SLEDAI and SDI scores were similar in patients with and without vitamin D deficiency [16]. In the present study, no significant differences of clinical manifestations according to serum 25(OH)D3 levels were found. Among disease activity markers, serum 25(OH)D3 levels were positively correlated only with hemoglobin (β = 0.256, P = 0.018) and serum complement level (β = 0.365, P = 0.002) after adjusted with BMI. It may be possible that the effects of vitamin D in disease activity are difficult to elucidate due to our patients with lupus being relatively well controlled (SELDAI 2.82) with-low dose corticosteroids (4.21 mg/d prednisolone equivalent). The role of vitamin D deficiency/insufficiency in the disease activity of SLE is far from clear, and further large prospective studies including more active patients with lupus are needed.
Our study is limited in that it was a cross-sectional study conducted without an associated questionnaire including questions designed to evaluate sun exposure time and the use of sunscreen. Additionally, our patients were relatively well controlled with low-dose corticosteroids. However, we included subjects prospectively that were evaluated only during the spring with matched controls. In addition, we evaluated multiple disease activity markers including antichromatin antibody, anti-dsDNA antibody, and SLEDAI.
Overall, the results indicate that the serum vitamin D levels are lower and vitamin D insufficiency is more common in Korean patients with SLE; however, our study demonstrates that vitamin D levels may not be a good marker of disease activity marker in SLE.
References
Holick MF (2007) Vitamin D deficiency. N Engl J Med 357:266–281
van Etten E, Mathieu C (2005) Immunoregulation by 1, 25-dihydroxyvitamin D3: basic concepts. J Steroid Biochem Mol Biol 97:93–101
Bhalla AK, Amento EP, Serog B et al (1984) 1,25-Dihydroxyvitamin D3 inhibits antigen-induced T cell activation. J Immunol 133:1748–1754
Lemire JM (1992) Immunomodulatory role of 1, 25-dihydroxyvitamin D3. J Cell Biochem 49:26–31
Mattner F, Smiroldo S, Galbiati F et al (2000) Inhibition of Th1 development and treatment of chronic-relapsing experimental allergic encephalomyelitis by a non-hypercalcemic analogue of 1, 25-dihydroxyvitamin D(3). Eur J Immunol 30:498–508
Linker-Israeli M, Elstner E, Klinenberg JR et al (2001) Vitamin D(3) and its synthetic analogs inhibit the spontaneous in vitro immunoglobulin production by SLE-derived PBMC. Clin Immunol 99:82–93
Holick MF (2004) Vitamin D: importance in the prevention of cancers, type 1 diabetes, heart disease, and osteoporosis. Am J Clin Nutr 79:362–371
Cantorna MT, Mahon BD (2004) Mounting evidence for vitamin D as an environmental factor affecting autoimmune disease prevalence. Exp Biol Med (Maywood) 229:1136–1142
Bultink IE, Lems WF, Kostense PJ et al (2005) Prevalence of and risk factors for low bone mineral density and vertebral fractures in patients with systemic lupus erythematosus. Arthritis Rheum 52:2044–2050
Muller K, Kriegbaum NJ, Baslund B et al (1995) Vitamin D3 metabolism in patients with rheumatic diseases: low serum levels of 25-hydroxyvitamin D3 in patients with systemic lupus erythematosus. Clin Rheumatol 14:397–400
Huisman AM, White KP, Algra A et al (2001) Vitamin D levels in women with systemic lupus erythematosus and fibromyalgia. J Rheumatol 28:2535–2539
Kamen DL, Cooper GS, Bouali H et al (2006) Vitamin D deficiency in systemic lupus erythematosus. Autoimmun Rev 5:114–117
Cutolo M, Otsa K (2008) Review: vitamin D, immunity and lupus. Lupus 17:6–10
Chen S, Sims GP, Chen XX et al (2007) Modulatory effects of 1, 25-dihydroxyvitamin D3 on human B cell differentiation. J Immunol 179:1634–1647
Orbach H, Zandman-Goddard G, Amital H et al (2007) Novel biomarkers in autoimmune diseases: prolactin, ferritin, vitamin D, and TPA levels in autoimmune diseases. Ann NY Acad Sci 1109:385–400
Ruiz-Irastorza G, Egurbide MV, Olivares N et al (2008) Vitamin D deficiency in systemic lupus erythematosus: prevalence, predictors and clinical consequences. Rheumatology (Oxford) 2047:920–923
Tan EM, Cohen AS, Fries JF et al (1982) The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 25:1271–1277
Bombardier C, Gladman DD, Urowitz MB et al (1992) Derivation of the SLEDAI.A disease activity index for lupus patients. The Committee on Prognosis Studies in SLE. Arthritis Rheum 35:630–640
Gladman DD, Goldsmith CH, Urowitz MB et al (2000) The systemic lupus international collaborating clinics/American college of rheumatology (SLICC/ACR) damage index for systemic lupus erythematosus international comparison. J Rheumatol 27:373–376
Kim HA, Jeon JY, Choi GS et al (2008) The antichromatin antibodies can be useful as a diagnostic tool and disease activity marker of systemic lupus erythematosus in Koreans. Clin Immunol 128:277–283
O’Regan S, Chesney RW, Hamstra A et al (1979) Reduced serum 1, 25-(OH)2 vitamin D3 levels in prednisone-treated adolescents with systemic lupus erythematosus. Acta Paediatr Scand 68:109–111
Borba VZ, Vieira JG, Kasamatsu T et al (2009) Vitamin D deficiency in patients with active systemic lupus erythematosus. Osteoporos Int 20:427–433
Thudi A, Yin S, Wandstrat AE et al (2008) Vitamin D levels and disease status in Texas patients with systemic lupus erythematosus. Am J Med Sci 335:99–104
Webb AR, Kline L, Holick MF (1988) Influence of season and latitude on the cutaneous synthesis of vitamin D3: exposure to winter sunlight in Boston and Edmonton will not promote vitamin D3 synthesis in human skin. J Clin Endocrinol Metab 67:373–378
Klein RG, Arnaud SB, Gallagher JC et al (1977) Intestinal calcium absorption in exogenous hypercortisonism. Role of 25-hydroxyvitamin D and corticosteroid dose. J Clin Invest 60:253–259
Hahn TJ, Halstead LR, Haddad JG Jr (1977) Serum 25-hydroxyvitamin D concentrations in patients receiving chronic corticosteroid therapy. J Lab Clin Med 90:399–404
O’Leary TJ, Jones G, Yip A (1986) The effects of chloroquine on serum 1, 25-dihydroxyvitamin D and calcium metabolism in sarcoidosis. N Engl J Med 315:727–730
Zold E, Szodoray P, Gaal J et al (2008) Vitamin D deficiency in undifferentiated connective tissue disease. Arthritis Res Ther 10:R123
Costenbader KH, Feskanich D, Holmes M et al (2008) Vitamin D intake and risks of systemic lupus erythematosus and rheumatoid arthritis in women. Ann Rheum Dis 67:530–535
Acknowledgments
This study was supported by the Brain Korea 21 project for Ajou University School of Medicine and a grant of the Korea Healthcare technology R&D Project, Ministry for Health, Welfare and Family Affairs, Republic of Korea (A080588).
Conflict of interest statement
We have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, HA., Sung, JM., Jeon, JY. et al. Vitamin D may not be a good marker of disease activity in Korean patients with systemic lupus erythematosus. Rheumatol Int 31, 1189–1194 (2011). https://doi.org/10.1007/s00296-010-1442-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-010-1442-1