Abstract
The aim of this study was to investigate the role of psychological factors in the development of complex regional pain syndrome (CRPS) type I following the fracture of the distal radius. Fifty patients (average age 57.70 ± 13.43 years) with a distal radius fracture were enrolled in the present study. All of the patients were treated by closed reduction and cast immobilization. The Toronto Alexithymia Scale-20, Anxiety Sensitivity Index, State-Trait Anxiety Inventory, and Beck Depression Inventory were used to determine the patients’ psychological features 2 days after the fracture. The patients were followed for 2 months after cast immobilization was completed using the International Association for the Study of Pain criteria to diagnose CRPS type I. CRPS type I developed in 13 (26%) patients of the 32 (34.4%) female patients and 18 (11.1%) male patients. The risk of CRPS type I was significantly increased in patients with high trait anxiety scores (P = 0.038). The results show that, after fracturing the distal radius, patients who have an anxious personality have a higher risk of developing CRPS type I. Following these patients closely for the development of CRPS type I may be advantageous for early preventative and therapeutic interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Complex regional pain syndrome (CRPS) type I is a clinical syndrome with complex symptoms and findings that include pain, allodynia, hyperalgesia, edema, trophic changes, and vasomotor instability [1–3]. Reflex sympathetic dystrophy syndrome, Sudeck’s atrophy, and algodystrophy are the most used synonyms. CRPS type I is clinically separated into acute, dystrophic, and atrophic periods, but the value of this phasing is controversial because the duration of each phase is highly variable, and the phases cannot always be separated in every patient [4].
CRPS type I most commonly develops after trauma, but it may develop in hemiplegia, coronary heart disease, or after surgery. An inciting event cannot be determined in nearly one-fourth of patients. Upper extremity involvement is frequent, and fractures of the distal radius are one of the most common inciting events. The incidence of CRPS after distal radius fracture has been reported in several studies to be 1–37% [5–13].
The pathophysiology of CRPS type I is unclear, and the question of why CRPS type I develops only in some patients is still unanswered. Several theories exist, including an irregular sympathetic system, increased neurogenic inflammation, genetic predisposition, and immobilization [14–16]. Many factors have been proposed to play a role in the development of CRPS type I after fracture of the distal radius [17]. Physical factors, including trauma intensity, tight cast application, pain during cast immobilization, and the number of repositions needed are all thought to be causative factors [6, 8, 18]. Psychological factors are also an area of interest due to the observation that some CRPS type I patients present with enigmatic features and emotional and behavioral characteristics. Some studies have shown that emotional imbalance, anxiety, somatization, tendency for depression, and a lack of confidence are prominent features in patients with CRPS type I. CRPS type I has been hypothesized to be psychosomatic in origin, and some special psychological features predispose an individual to developing CRPS type I and accelerate progression [19–23]. Many authors have advised that treatment of the disease must include psychological support and treatment [23–25]. On the other hand, some other studies have reported that CRPS type I is a chronic pain condition, and behavioral and emotional changes can be due to chronic pain. Therefore, psychological abnormalities observed in CRPS type I patients may be the result, not the cause [7, 26], but all of the studies mentioned previously were retrospective, and psychological features were examined in late-phase patients. A few prospective studies have evaluated the psychological factors for CRPS type I development after fracture of the distal radius [8, 27, 28]. In these studies, the direct relationship between CRPS and psychological factors was controversial.
CRPS type I has different clinical profiles. The pathophysiology of this disorder is still unclear, and a variety of criteria exist for diagnosis. Most retrospective, and a few prospective, studies have determined the role of psychological factors in patients with CRPS type I. However, most of these studies had poor methodological quality; the association between psychological factors and CRPS type I should be investigated with higher methodological quality [29].
The aim of this prospective study is to investigate the role of multiple dimensions of psychological features on the development of CRPS type I in patients with a fracture of the distal radius.
Materials and methods
The study protocol was approved by the Ethics Committee of Dokuz Eylul University Faculty of Medicine in Turkey. All patients provided written informed consent.
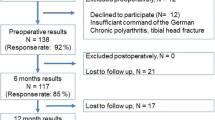
Seventy-four patients who visited the Emergency Unit of University Hospital with a fracture of the distal radius during the period of January 2006 to May 2007 were screened for inclusion in the study. All patients were treated by closed reduction and 6 weeks of cast immobilization. Patients who were operated on or failed to come to follow-up appointments were excluded.
The patients were psychologically evaluated within 2 days after cast application. Thirteen patients refused psychological evaluation. A total of 61 patients were included in the study. Four of these patients were operated on for poor reduction, and seven patients did not come to follow-up visits during the observation period. Therefore, the study was completed by 50 patients (Fig. 1).
Demographic data, including age, gender, educational level, habits, and history of psychiatric and other systemic diseases, were recorded.
The psychological assessment was performed using four different tools: Anxiety Sensitivity Index (ASI), Toronto Alexithymia Scale-20 (TAS–20), State-Trait Anxiety Inventory (STAI), and the Beck Depression Inventory (BDI). The Turkish versions of these tests were evaluated by two authors from the Department of Psychiatry.
The ASI is a 16-item self-reported measure of anxiety sensitivity, a fear of anxiety-related symptoms based on beliefs about their potential harmful consequences. Items are rated on scale of 0 (very little) to 5 (very much). The total score range is 0–64 [46].
The TAS–20 has 20 items to assess alexithymic features and provides scores for three empirically derived factors: difficulty identifying feelings, difficulty communicating feelings, and externally oriented thinking. Items are rated on a 5-point Likert scale. Higher scores on each of the subscales indicate higher levels of alexithymic traits. Factor analyses of the scale with clinical and nonclinical samples have shown these factors to be congruent with the theoretical characteristics of the alexithymia construct [30]. The TAS-20 scores of clinical populations have been found to be significantly higher than those of nonclinical populations [31, 45]. The scale is free from social desirability responses and has been shown to have a high level of internal consistency (Cronbach α = .81), good test–retest reliability over a 3-week period (r = 0.77), and convergent and divergent validity [31].
The STAI is a self-reported scale for evaluating anxiety levels and includes separate measures of state (STAI-I) and trait (STAI-II) anxiety. Each dimension is assessed with a 20-item scale, with each item scored on a 4-point scale. Respondents are asked to indicate how they are feeling “at the moment” on the state version and how they feel “generally” on the trait version [32].
The BDI is a self-reported scale consisting of 19 items to assess the severity of depressive symptoms. Items are scored on a scale of 0–3, yielding a score range of 0–57 in which higher scores indicate greater depression severity [33].
All patients were treated in a long arm cast for 2 weeks and then in a short arm cast for 4 weeks. Patients were advised to elevate the arm and perform a range of motion exercises for the fingers to protect from edema. After the cast was removed, the patients were followed for symptoms and signs of CRPS type I for 2 months. Patients were examined weekly during the first month of the follow-up period and bi-weekly during the second month. A standardized home exercise program was given to all patients during this 2-month period.
The diagnosis of CRPS type I was based on clinical findings and International Association for the Study of Pain (IASP) criteria (Table 1) [3].
Statistical analyses were performed with SPSS version 11.0 (SPSS, Chicago, IL, USA). Descriptive statistics were used for demographic data. The χ2 and Mann–Whitney U tests were used to compare two groups of patients that developed and did not develop CRPS type I in terms of demographic data and psychological test scores. All data are presented as mean ± SD. A two-tailed criterion of P < 0.05 was used as the cutoff for significance in all analyses.
Results
Fifty patients with an average age of 57.70 ± 13.43 years (range 18–81 years) completed the study. Thirty-two (64%) patients were women and 18 (36%) were men. Twenty-six (48%) patients had a right side fracture, 28 (52%) patients had a left side fracture. Forty-eight (96%) patients had right-sided dominance. The mean time interval from cast removal to CRPS type I diagnosis was 1.92 ± 0.86 weeks (1–4 weeks). CRPS type I developed in 13 (26%) patients according to IASP criteria. Eleven (86%) of the patients with CRPS were women and 2 (14%) were men. Stated differently, 2 (11%) of the 18 male patients and 11 (34%) of the 38 female patients developed CRPS type I. The gender difference was not significant (χ2 = 3.24, P > 0.05). Other demographic data comparing the two groups of patients are shown in Table 2.
Age (P = 0.15), gender (P = 0.07), marital status (P = 0.15), smoking (P = 0.65), and educational level (P = 0.90) distributions among patients with and without CRPS type I were not statistically different. Seven (54%) of the CRPS type I patients and 9 (24%) of the non-CRPS type I patients had a history of psychiatric disorders (panic disorder, depression, personality disorders, etc.). The difference between the two groups was not significant (P = 0.05).
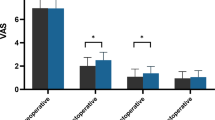
The STAI-II scores were higher for CRPS type I patients than non-CRPS type I patients (P = 0.038), but no difference was found between the two groups in terms of ASI, TAS -20, STAI-I, and BDI scores (Table 3).
Discussion
CRPS type I is a severely disabling clinical entity for patients and a difficult treatment problem for clinicians. Trauma is one of the inciting events for the development of CRPS type I. Why some patients develop CRPS type I and others do not after almost the same trauma is still being investigated:
The incidence of CRPS type I has been reported to be 1–37% after distal radius fracture [5, 6, 8–13]. In this study, 13 of the 50 (26%) patients with a fracture of the distal radius, who were treated conservatively by closed reduction and cast immobilization, developed CRPS type I. Several reviews, including case studies, and a small number of studies on the relationship between psychological factors and CRPS type I have been published, but the literature on this issue is mixed [17, 19, 34–38]. Some retrospective studies demonstrated that emotional, behavioral, and personality abnormalities are prominent in CRPS type I patients [16, 19, 39, 40]. Pollack et al. [19] proposed Sudeck A type personality, which is characterized by emotional imbalance, increased anxiety, decreased self confidence, tendency for depression, and somatization, and suggested that these personality traits predispose an individual to CRPS type I development. On the other hand, personality disorders and major depression are observed at similar frequencies in CRPS type I and other chronic pain syndromes, such as low back pain and local neuropathy [7, 41, 42]. Chronic and intense pain may result in psychological abnormalities that represent an exaggeration of maladaptive personality traits and coping styles [41]. Retrospective studies have demonstrated that CRPS type I patients display psychological abnormalities but do not provide whether these abnormalities were present prior to the inciting event [43].
A few studies of the relationship between psychological factors and CRPS type I prospectively investigated patients with a fracture of the distal radius [8, 28, 43]. Field and Gadner (1997) used the General Health Questionnaire (GHQ), which has 30 questions about the level of psychological distress, in 100 patients with a Colles fracture who received conservative treatment. Twenty-four patients (24%) were diagnosed with CRPS type I at the 9-week evaluation. The first week GHQ scores were not significantly different between patients with or without CRPS type I. The authors concluded that CRPS type I patients had no increased distress before the onset of the disease [28]. Psychological distress was evaluated with a unidimensional test; therefore, interpretation of the results is difficult.
Puchalski and Zyluk examined 64 patients with distal radius fractures who underwent operations, finding no significant differences between patients with or without CRPS type I in terms of depression scores and personality [27]. Similar to that study, we found that our patients who developed CRPS type I did not differ from patients who did not develop CRPS in terms of BDI scores before the onset of disease.
The alexithymia construct was formulated to identify a group of affective and cognitive characteristics observed in patients with so-called ‘classical’ psychosomatic diseases [44] and has been found to be strongly related to many types of psychosomatic disorders. We used the TAS-20 to identify alexithymic features in patients and did not find any difference between patients with or without CRPS type I. To the best of our knowledge, this is the first study that prospectively investigated the alexithymic features of CRPS.
The role of anxiety in the development of CRPS has been investigated in two prospective studies [15, 44]. Feldman et al. [44] studied the relationships between daily pain, anxious mood, and social support in 109 people with reflex sympathetic dystrophy syndrome, finding that increased pain caused increases in anxious mood, but increased anxiety did not lead to increased pain. Harden et al. [15] found that a greater level of preoperative trait anxiety predicts the development of CRPS in patients undergoing total knee arthroplasty. In the present study, we used STAI-I and STAI-II to evaluate the presence and level of anxiety. The STAI-II scores (i.e. general anxiety level) were significantly high in patients with CRPS type I, but not the STAI-I scores, which indicate the state anxiety level just after fracture. These results indicate that, instead of the anxiety level immediately following fracture (state anxiety), the patient’s general anxiety level (trait anxiety) is predictive of CRPS development. In other words, an anxious personality is a risk factor for CRPS. We know that peripheral and central sensitization play primary roles in the CRPS disease process [1, 16, 24]. Psychological distress is often associated with increased catecholamine activity. In a pilot study, increased systemic catecholamines were found in CRPS with a relationship to psychological factors. The level of circulating norepinephrine was significantly higher than normal control levels or the contralateral limb in that study. Also, catecholamine levels have been correlated with scores on psychometric measures of depression, anxiety, and personality [16]. We think that an increased general anxiety level may correlate with permanent catecholamine levels.
Anxiety sensitivity refers to the tendency to fear anxiety-related sensations and is thought to arise from beliefs about their harmful physical, cognitive, or social consequences. In this study, we used the ASI to evaluate anxiety sensitivity, finding no difference between patients with or without CRPS type I.
Psychiatric history is also an important factor to investigate in CRPS studies. Two retrospective studies reported that people with a history of psychiatric disorders are more prone to developing CRPS type I than others [19, 23]. On the other hand, Dijkstra et al. [8] concluded in their prospective study that past psychiatric history has no effect on CRPS development. We found that a history of psychiatric disorders is more prevalent in CRPS type I patients, but not significant.
In summary, this was a prospective study investigating the effects of a broad spectrum of psychological factors on the development of CRPS type I after distal radius fracture. After the fracture, patients who have a high level of general anxiety are more prone to develop CRPS type I. Close follow-up of such patients may offer an advantage for prevention, early diagnosis, and treatment.
References
Dommerholt J (2004) Complex regional pain syndrome-1: history, diagnostic criteria and etiology. J Bodywork Mov Ther 8:167–177
Eisenberg E, Melamed E (2003) Can complex regional pain syndrome be painless. Pain 106:263–267
Merskey H, Bogduk N (1994) Classification of chronic pain: definitions of chronic pain syndromes and definition of pain terms. IASP Press, Seattle, WA, pp 40–43
Walker SM, Cousins MJ (1997) Complex regional pain syndromes: including reflex sympathetic distrophy and causalgia. Anaesth Intens Care 25:113–125
Veldman PHJM, Reynen HM, Arntz IE, Goris RJA (1993) Signs and symptoms of reflex sympathetic dystrophy: prospective study of 829 patients. Lancet 342:1012–1016
Bickerstaff DR, Kanis JA (1994) Algodystrophy: an under-recognized complication of minor trauma. Br J Rheumatol 33:240–248
Bruehl S, Husfeldt B, Lubenow TR, Nath H, Ivankovich AD (1996) Psychological differences between reflex sympathetic dystrophy and non RSD chronic pain patients. Pain 67:107–114
Dijktstra PU, Groothoff JW, Duis HJ, Geertzen JHB (2003) Incidence of complex regional pain syndrome type I after fracturas of the distal radius. Eu J Pain 7:457–462
Atkins RM, Duckworth T, Kanis JA (1989) Algodystrophy following Colles’ fracture. J Hand Surg Br 14:161–164
De Brujin HP (1987) Functional teratment of colles fracture. Acta Orthop Scand 223:1–95
Dressing K, Peterson T, Schimit NK (1994) Compartment pressure in the carpal tunnel in distal fracture of the radius. A prospective study. Arch Orthop Trauma Surg 113:285–289
Roumen RM, Hesp WL, Bruggink ED (1991) Unstable Colles’ fractures in elderly patients. A randomised trial of external fixation for redisplacement. J Bone Joint Surg Br 73:307–311
Zollinger PE, Tuinebreijer WE, Kreis RW, Breederveld RS (1999) Effect of vitamin C on frequency of reflex sympathetic dystrophy in wrist fractures: a randomised trial. Lancet 354:2025–2028
Doro C, Hayden JR, Louis SD (2006) Complex regional pain syndrome type I in the upper extremity. Clin Occup Environ Med 5:445–454
Harden RN, Bruehl S, Stanos S, Brander VI et al (2003) Prospective examination of pain- related and psychological predictors of CRPS-like phenomena following total knee arthroplasty: a preliminary study. Pain 106:393–400
Harden RN, Rudin NJ, Bruehl SI et al (2004) Increased systemic catecholamines in complex regional pain syndrome and relationship to psychological factors: a pilot study. Anesth Analg 99:1478–1485
Zyluk A (2004) Complex regionel pain syndrome type I: risk factors, prevention and recurrence. J Hand Surg 29:334–337
Field J, Protheroe DL, Atkins RM (1994) Algodystrophy after colles fractures is associated with secondary tightness of casts. J Bone Joint Surg Br 76:901–905
Pawl RP (2000) Controversies surrounding reflex sympathetic dystrophy. Curr Rev Pain 4:259–267
Pushalski P, Zyluk A (2005) Complex regional pain syndrome type 1 after fractures of the distal radius: a prospective study of psychological factors. J Hand Surg 6:574–580
Bruehl S, Carlson CR (1992) Predisposing psychological factors in the development of reflex sympathetic dystrophy. A review of the empirical evidence. Clin J Pain 8:287–299
Taskaynatan MA, Balaban B, Karlidere T, Ozgul A, Tan AK, Kalyon TA (2005) Factitious disorders encountered in patients with the diagnosis of reflex sympathetic dystrophy. Clin Rheumatol 24:521–526
Rauis AL (1994) Psychological aspects: a series of 104 posttraumatic cases of reflex sympathetic dystrophy. Acta Orthop Belg 65:86–90
Ghai B, Dureja GP (2004) Complex regional pain syndrome: a review. J Postgrad Med 50:300–307
King JH, Nuss S (1993) Reflex sympathetic dystophy treated by ECT. Pain 55:393–396
Zyluk A (2003) A new clinical severity scoring system for reflex sympatetic dystrophy of the upper limp. J Hand Surg 3:238–241
Pollack HJ, Neumann R, Pollack E (1980) Sudeck und psyche. Beitr Orthop Traumatol 27:463–468
Field J, Gardner FV (1997) Psychological distress associated with algodystrophy. J Hand Surg 22:100–101
Beerthuizen A, Spijker A, Huygen FJPM, Klein J, Wit R (2009) Is there an association between psychological factors and the complex regional pain syndrome type 1(CRPS1) in adults? A systematic review. Pain 145:52–59
Bagby RM, Parker JD, Taylor GJ (1994) The twenty-item Toronto Alexithymia Scale-I. Item selection and cross-validation of the factor structure. J Psychosom Res 38:23–32
Bagby RM, Taylor GJ, Parker JD (1994) The twenty-item Toronto Alexithymia Scale-II. Convergent, discriminant, and concurrent validity. J Psychosom Res 38:33–40
Öner N (1978) Türkçeye uyarlanmış bir kaygı envanterinin geçerlik çalışması. Türk Psikoloji Dergisi 1:12–17
Hisli N (1989) Beck Depresyon Envanterinin üniversite öğrencileri için geçerliği ve güvenirliği. Psikoloji dergisi 7:3–13
Bruehl S (2001) Do psychological factors play a role in the onset and maintenance of CRPS-1? In: Harden N, Baron R, Janig W (eds) Complex regional pain syndrome, progress in pain research and management. IASP Press, Seattle
Bruehl S, Chung OY ( 2006) Psychological and behevioral aspects of complex regional pain syndrome managment. Clin J Pain 22:430–437
Greipp ME (2003) Complex regional pain syndrome- type 1: research relevance, practice realities. J Neurosci Nurs 35:16–20
Kasdan ML, Jhonson AL (1998) Reflex sympathetic dystrophy. Occup Med 13:521–531
Stanton-Hicks MD, Burton AW, Bruehl SP, Carr DB, Harden RN, Hassenbusch SJ, Lubenow TR, Oakley JC, Racz GB, Raj PP, Rauck RL, Rezai AR (2002) An updated interdisciplinary clinical pathway for CRPS: report of an expert panel. Pain Practice 2:1–16
Shiri S, Tsenter J, Livai R, Schwartz I, Vatine JJ (2004) Similarities between the psychological profiles of complex regional pain syndrome and conversion disorder patients. J Clin Psychol Med S 10:193–199
Grunert BK, Devine CA, Sanger JR, Matloub HS, Green D (1990) Thermal self-regulation for pain control in reflex sympathetic dystrophy. J Hand Surg 15:615–618
Monti DA, Herring CL, Schwartzman RJ, Marchese M (1998) Personality assessment of patients with complex regional pain syndrome type I. Clin J Pain 14:295–302
Ciccone DS, Bandilla EB, Wu W (1997) Psychological dysfunction in patients with reflex sympathetic dystrophy. Pain 71:323–333
Sifneos PE (1973) The prevalence of alexithymic characteristics in psychosomatic patients. Psychother Psychosom 22:255–262
Feldman SI, Downey G, Schaffer-Neitz R (1999) Pain, negative mood, and perceived support in chronic pain patients: a daily diary study of people with reflex sympathetic dystrophy syndrome. J Consult Clin Psychol 67:776–785
Sayar K, Gulec H, Ak I (2001) Validity and reliability of the twenty item Toronto Alexithymia Scale (Turkish version). Istanbul: 37th National congress of psychiatry abstract book
Ayvaşık HB (2000) Kaygı duyarlılığı indeksi: geçerlik ve güvenirlik çalışması. Türk Psikoloji Dergisi 15:43–57
Acknowledgments
We would like to thank all of the patients who participated in this study.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dilek, B., Yemez, B., Kizil, R. et al. Anxious personality is a risk factor for developing complex regional pain syndrome type I. Rheumatol Int 32, 915–920 (2012). https://doi.org/10.1007/s00296-010-1714-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-010-1714-9