Abstract
Purpose
Prolonged postoperative pain is a frequent problem after uncomplicated total knee replacement (TKR). The purpose of this study was to evaluate the effect of anxiety and pain catastrophizing on postoperative pain after TKR.
Methods
A total of 150 patients were enrolled in this prospective study. Preoperatively, anxiety was assessed using the State-Trait Anxiety Inventory (STAI) and pain catastrophizing was assessed using the Pain Catastrophizing Scale (PCS). The primary outcome measure was postoperative pain on a numerical rating scale (NRS). The secondary outcome parameters were the different Knee Osteoarthritis Outcome Score (KOOS) subscales and patient satisfaction. Intergroup differences were tested with an independent t test. The odds ratio was calculated to determine the probability of an unsatisfactory outcome.
Results
Preoperatively and at 6 and 12 months postoperatively, patients with anxiety and particularly patients with pain catastrophizing usually had a higher NRS score, lower knee function before and after surgery, and higher dissatisfaction. These intergroup differences were significant preoperatively and at 6 months postoperatively.
Conclusions
Psychopathologic factors, particularly pain catastrophizing, have an impact on postoperative pain after TKR. Preoperative screening and concurrent treatment of the diagnosed psychological disorder may improve patient-perceived outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bicondylar total knee replacement (TKR) is a common treatment for end-stage osteoarthritis. More than 168,000 TKR surgeries were performed in Germany in 2011 [33]. In most patients, this intervention results in improved knee joint function, reduced joint pain, and increased quality of life [13, 18]. However, 15–25% of patients are unsatisfied with the result [5, 7, 13, 25]. One cause of this dissatisfaction may be continuing knee joint pain after apparently uncomplicated TKR [4, 24].
A high prevalence of residual pain has been reported after uncomplicated TKR, particularly during the first year [2, 4, 7, 13, 25]. Forsythe et al. [13] showed that the pain level at 3 and 12 months postoperatively was still approximately 50% of the preoperative pain level. Brander et al. [6, 7] demonstrated that the mean pain level measured on a visual analog scale was 52 preoperatively, 25 at 3 months postoperatively, and 17 at 12 months postoperatively.
The predictors of postoperative pain after TKR can be divided into modifiable and non-modifiable factors [2, 21]. The non-modifiable predictors include young age, female sex, and severe preoperative pain [6, 7, 13]. Of clinical interest are the modifiable psychological factors [21].
Several studies have shown that psychopathologic distress is negatively associated with patient outcomes after surgery [2, 14, 16]. It was further reported that depression and somatization dysfunction are associated with prolonged pain after TKR [2]. Other psychological predictors of postoperative pain are anxiety and pain catastrophizing [11, 26, 27]. There is controversy regarding the role of anxiety on the level of postoperative pain [7, 16, 27, 31]. However, we are not aware of any studies that have examined the effect of anxiety on postoperative pain after TKR. There is also limited information in the literature about the influence of pain catastrophizing on postoperative pain and satisfaction after TKR [13]. Pain catastrophizing describes a response style to painful experiences that is likely to be associated with negative pain outcomes [30].
The aim of the present study was to analyze the effect of anxiety and pain catastrophizing on postoperative pain and patient satisfaction after knee arthroplasty. The primary outcome measures were pain evaluated by a numeric rating scale (NRS) and total Knee Osteoarthritis Outcome Score (KOOS), an instrument responsive to changes in knee symptoms, including pain. The hypothesis of the present study is that anxiety and pain catastrophizing have an effect on the level of postoperative pain and patient satisfaction during the first year after surgery.
Materials and methods
Study population
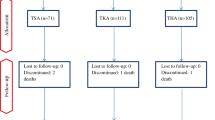
Patient recruitment took place in 2012 and 2013. Several inclusion and exclusion criteria were used to identify patients who were eligible for this prospective study (Table 1). All eligible patients were informed about the study design by one of the authors. After performing a statistical estimation of the number of cases, of 150 patients who were eligible, 138 were willing to participate. These 138 patients were enrolled after providing written informed consent (Fig. 1). The study design was approved by the local ethics committee.
Indications for TKR existed in these patients with radiological end-stage osteoarthritis (Kellgren and Lawrence grade IV) and a minimum of three of the following four clinical symptoms: crepitation, deformation, knee pain, and loss of function.
Surgical technique
In all patients, a prosthesis was implanted through a medial parapatellar approach with the patient under general anesthesia. The detailed surgical technique used for TKR was described previously [2]. The same TKR model (Genesis™ II Knee Replacement System; Smith & Nephew Inc., Andover, MA, USA) was used in all patients. All patients received femoral and sciatic nerve blocks for postoperative pain management.
Psychological scores
At baseline, anxiety and pain catastrophizing were evaluated with standardized psychological scores.
The State-Trait Anxiety Inventory (STAI) was used to evaluate the influence of anxiety on pain and function after TKR. In this study, the German STAI modified by Spielberger et al. [29] was used. This modified STAI is composed of two scales, each containing 20 items. The first scale describes anxiety as a state, reflecting a temporary emotional condition with high variance. The second scale characterizes anxiety as a trait, describing relative stabilized individual conditions to estimate situations as menacing. The aim of the questionnaire is to describe the relationship between anxiety as a state (temporary emotional) and a trait (stable interindividual differences in grade to estimate situations as drastic) [29]. The two scales were evaluated separately, and the values were converted with the help of norm tables.
The Pain Catastrophizing Scale (PCS) was developed in 1995 to explore how catastrophizing affects pain experiences [30]. Catastrophizing means to overrate the probability of a negative event. The questionnaire contains three different elements: rumor, helplessness, and enhancement [20]. The PCS includes 13 items, comprising four for rumor, six for helplessness, and three for enhancement. Each item has a five-level scale, and the score can range from 0 to 52 points. It has been suggested that a threshold of 30 points reflects clinically relevant catastrophizing.
Primary and secondary outcome measures
The primary outcome measure were pain, measured by an NRS at rest and after 15 min of daily living activities and the knee function, measured with the total KOOS. The validated German version of the KOOS is self-explanatory and comprises five subscales: pain, symptoms, activities of daily living, sports, and quality of life [23]. Standardized answer options are presented on a five-point Likert scale, and each question is assigned a score from 0 to 4. For the present study, the sports subscale was excluded because 30 and 25% of the patients did not fill out this category preoperatively and postoperatively, respectively.
The secondary outcome measures were the different KOOS subscales and patient satisfaction with the surgery. Patient satisfaction with the surgery was evaluated by the following question: “How satisfied are you with the outcome after TKR?” Answers were given on a five-point Likert scale (1: very satisfied; 2: satisfied; 3: mediocrely satisfied; 4: unsatisfied; and 5: very unsatisfied). Patients were deemed satisfied if they rated themselves ‘very satisfied’ or ‘satisfied’ and deemed unsatisfied if they rated themselves ‘unsatisfied’ or ‘very unsatisfied’.
All outcome measures were evaluated by self-administered questionnaires at baseline (preoperatively) and at 6 and 12 months postoperatively.
Statistical analysis
Before investigation, we estimate the number of cases to see how many patients were needed to see statistically relevant differences in the KOOS as the primary endpoint next to the NRS. Normal distributions of the primary endpoints (KOOS and NRS score) were tested with the Kolmogorov–Smirnov test. Significant intergroup differences were tested with an independent t test. If data were not normally distributed, the non-parametric Mann–Whitney U test was used. The odds ratio was calculated to determine the probability of an unsatisfactory outcome in patients with and without preoperative symptoms of depression and somatization.
Results
Patients
Of 150 eligible patients, 12 met the exclusion criteria (Table 1). Therefore, a total of 138 patients participated in the study. The flowchart in Fig. 1 shows the distribution of patients during the study. The patient characteristics are shown in Table 2. During the follow-up period, no recurring effusions were aspirated and no other surgical procedures were performed.
Effect of pain catastrophizing and anxiety on primary outcome measures
Pain catastrophizing symptoms were seen in 27.5% of patients. Trait anxiety was observed in 14.5% of patients.
The primary outcome measures were pain (NRS) and knee function (total KOOS). There was a significant improvement in pain, both at rest and during activities of daily living, as well as in total KOOS from baseline to both 6 and 12 months postoperatively. No significant differences in pain level or KOOS were observed between 6 and 12 months postoperatively.
At each time point, patients with pain catastrophizing (PCS > 30 points) had a higher pain level both at rest and with activity. However, this intergroup difference was only significant for rest and activity preoperatively and at 6 months postoperatively (Fig. 2a, b).
The influence of anxiety is shown in Fig. 3a, b. Patients with anxiety had a higher pain level both at rest and with activity. However, the difference was not significant for pain assessment with activity before surgery.
Patients’ opinions about their knees and knee-associated problems were assessed by the KOOS. The total KOOS improved from 33.0 ± 22.7 points preoperatively to 63.0 ± 23.4 points at 6 months postoperatively and 67.0 ± 23.4 points at 12 months postoperatively.
Pain catastrophizing had a significant effect on the total KOOS at baseline and at 6 months postoperatively (Fig. 4, Table 3). Patients with anxiety also had a poor assessment of their knee function, the effect on the total KOOS was significant at baseline (preoperatively) and after surgery (Fig. 5, Table 4).
Effect of pain catastrophizing and anxiety on secondary outcome measures
The influence of pain catastrophizing and anxiety on the KOOS subscales is shown in Tables 3 and 4. Patients with pain catastrophizing tended to have a poorer outcome in all five subscales, but significant intergroup differences between patients with and without pain catastrophizing among the subscales were only found preoperatively and at 6 months postoperatively for the subscales “pain” and “QOL”. For anxiety, significant intergroup differences for the subscales “pain” and “ADL” were found at baseline (preoperatively) and after surgery.
At 6 months postoperatively, 13% of all patients were dissatisfied with their postoperative outcome, while at 12 months postoperatively, 11% were dissatisfied. The dissatisfaction rate was correlated with lower function in the total KOOS. The patients with pain catastrophizing tended to be more dissatisfied at 6 and 12 months postoperatively, but these differences were only significant at 6 months, and not at 12 months (Table 5). The mean dissatisfaction scores were also higher in patients with anxiety at 6 and 12 months postoperatively (Table 5), but the differences were not significant.
The odds ratio for patients with pain catastrophizing was 1.73 and that for patients with anxiety was 1.81 (Table 6).
Discussion
The results of the present study show that psychological factors such anxiety and pain catastrophizing affected the outcome after TKR, thus confirming our hypothesis. Patients with signs of anxiety and pain catastrophizing had significantly more pain, experienced significantly more knee symptoms, and were more dissatisfied with their outcome, but the influence of pain catastrophizing was stronger than the influence of anxiety, especially at 6 months after TKR.
As pain is the most disabling symptom of osteoarthritis, it is one of the most important outcome measures after TKR [25], and it is meaningful to use non-elaborate questions like the NRS [12]. Therefore, pain was chosen as the primary outcome measure in the present study along with the KOOS. Increased pain, especially during the first postoperative year, is a well-known phenomenon, and memory of pain was also reported to play a role in pain chronicity [1].
Several studies have shown that psychopathology is associated with poorer patient-perceived outcomes after elective surgery [6, 7, 28]. It has been estimated that 25% of patients who have undergone TKR complain of psychological factors, which can potentially worsen pain and functional outcomes [19]. Other studies investigated the influence of physical symptoms like low back pain (LBP). LBP usually remains after TKR and this may impair satisfaction and patient-reported outcomes [9].
The results of the present study confirm the findings of previous studies showing that anxiety is associated with suboptimal improvement in knee function after primary TKR [11, 26]. However, trait anxiety, which describes relative stabilized individual conditions to estimate situations as menacing, had a significant influence of pain and function especially at baseline and 6 months postoperatively. At 12 months postoperatively, the groups had converged. The reason for this finding may be that the surgery as the menacing event and the prosthesis as a new unknown part of the body are moved into the background. Otherwise, it can be postulated that patients with anxiety decide to have surgery at a later time with more severe knee symptoms.
Satisfaction at 12 months postoperatively measured by the odds ratio was 1.81, meaning that patients with anxiety have an approximately twofold increased risk for dissatisfaction.
Brander et al. [7] described a significant relationship between anxiety measured by the STAI and the NRS at 12 months after TKR. Hirschmann et al. [16] determined only a low correlation between the two scales of the STAI and the Knee Society Score (KSS) and Womac score. It is notable that the study by Hirschmann and colleagues used the endpoints from the STAI, and not the normed reference values. A great influence of anxiety, measured by the Hospital Anxiety and Depression Scale (HADS), was shown by Hanusch et al. [14] for the KSS at 12 months postoperatively, but not for the “range of motion” (ROM) at 6 and 12 months postoperatively. No relationship between the HADS and pain at 12 months postoperatively was found by Utrillas-Compaired et al. [31]. Other studies examine the patient’s perception of their inpatient hospital experience after TKR, it showed an important modifiable predictor of functional outcome and satisfaction with TKR after 5 years [8].
Blackburn et al. [3] tried to determine whether anxiety and depression are responsible for poor outcomes or persistent knee pain. They indicated the complexity of the interpretation, but described that if anxiety and depression are accompanied by high pain levels, knee pain can be accountable for anxiety and depression.
It is striking that approximately 50% of the patients had a trait anxiety in the appropriate questionnaire. Another study showed a prevalence of 27.9% measured by the “Hospital Anxiety and Depression Scale” (HADS) [10].
Few studies have evaluated the effect of pain catastrophizing on TKR outcomes. In the present study, pain catastrophizing was associated with a significantly higher pain level and lower knee function (KOOS) at baseline and 6 months postoperatively. Associated with this, patients with anxiety were significantly more dissatisfied at 6 months postoperatively. At 12 months postoperatively, the differences were assimilated. Apparently, the real clinical knee pain preoperatively and the healing process immediately after implantation play a strong role to increase pain catastrophizing. Patients with pain catastrophizing had a 1.73-fold higher risk for dissatisfaction at 12 months after TKR than patients without pain catastrophizing. Keefe et al. [17] described that catastrophizing leads to modified central nervous system handling of pain, increased claims on healthcare, and reduced function.
Forsythe et al. [13] showed that a high preoperative level on the PCS is a predictor for persistent knee pain, as measured by the McGill Pain Questionnaire (MPQ), at 12 and 24 months after TKR. Furthermore, they found that the psychological variable of the PCS did not significantly change after TKR. The fact that the “rumination” part of the PCS is a stronger predictor than the whole PCS could not be confirmed in the present study. In a review, Bonnin et al. [4] described pain catastrophizing as one of five predictors for persistent knee pain after TKR. Riddle et al. [22] showed a significant influence of the Womac pain score at 6 months postoperatively. The reasons for the different findings may be partially the short study periods and the different cut-off points of the PCS (15 or 30 points) between the studies. In particular, investigations with the shorter period of 12 months show higher influence.
Wallis and Tayler [32] highlighted that pain catastrophizing is modifiable. Intervention possibilities can be coping skills, improvement of preoperative knowledge on outcomes, and participation in the decision-making [18, 22]. Hirikawa et al. [15] described that sensory training during rehabilitation can reduce persistent pain. The need for an intervention is underlined by the present study.
Dissatisfaction after TKR varies from 11 to 25% in the literature [25]. In the present study, the dissatisfaction rate was 11% at 12 months postoperatively, but was not associated with any postoperative radiological abnormalities. However, patients with dissatisfaction had a lower knee function after surgery. The results of the present study suggest that patient endogenous psychological characteristics contribute to the dissatisfaction rate. This fact should be considered when healthcare providers and insurance companies discuss new strategies, such pay-per-performance models, to reimburse joint replacement costs.
This study has some limitations. First, the percentage of patients lost to follow-up was high (25%). However, this loss of follow up is comparable with the percentages in other studies evaluating the impact of psychological factors on outcomes after TKR. Second, there was a disparity between the sexes (87 female patients and 51 male patients). Again, this distribution is comparable with those in other studies.
In conclusion, anxiety and particularly pain catastrophizing can have a strong impact on outcomes after TKR. However, the impact appears slightly lower compared with the influence of somatization and depressive symptoms [2].
Nevertheless, such patients should not be withheld from helpful treatment. Based on the high prevalence of these factors, patients should be screened and additionally treated preoperatively by a psychologist.
References
Alvarado S, Tajerian M, Suderman M et al (2015) An epigenetic hypothesis for the genomic memory of pain. Front Cell Neurosci 9:88
Bierke S, Haner M, Petersen W (2016) Influence of somatization and depressive symptoms on the course of pain within the first year after uncomplicated total knee replacement: a prospective study. Int Orthop 40:1353–1360
Blackburn J, Qureshi A, Amirfeyz R et al (2012) Does preoperative anxiety and depression predict satisfaction after total knee replacement? Knee 19:522–524
Bonnin MP, Basiglini L, Archbold HA (2011) What are the factors of residual pain after uncomplicated TKA? Knee Surg Sports Traumatol Arthrosc 19:1411–1417
Bourne RB, Chesworth BM, Davis AM et al (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 468:57–63
Brander V, Gondek S, Martin E et al (2007) Pain and depression influence outcome 5 years after knee replacement surgery. Clin Orthop Relat Res 464:21–26
Brander VA, Stulberg SD, Adams AD et al (2003) Predicting total knee replacement pain: a prospective, observational study. Clin Orthop Relat Res 416:27–36
Clement ND, Macdonald D, Burnett R et al (2017) A patient’s perception of their hospital stay influences the functional outcome and satisfaction of total knee arthroplasty. Arch Orthop Trauma Surg 137:693–700
Collados-Maestre I, Lizaur-Utrilla A, Martinez-Mendez D et al (2016) Concomitant low back pain impairs outcomes after primary total knee arthroplasty in patients over 65 years: a prospective, matched cohort study. Arch Orthop Trauma Surg 136:1767–1771
Duivenvoorden T, Vissers MM, Verhaar JA et al (2013) Anxiety and depressive symptoms before and after total hip and knee arthroplasty: a prospective multicentre study. Osteoarthr Cartil 21:1834–1840
Ellis HB, Howard KJ, Khaleel MA et al (2012) Effect of psychopathology on patient-perceived outcomes of total knee arthroplasty within an indigent population. J Bone Jt Surg Am 94:e84
Fischer CA, Neubauer E, Adams HS et al (2014) Effects of multidisciplinary pain treatment can be predicted without elaborate questionnaires. Int Orthop 38:617–626
Forsythe ME, Dunbar MJ, Hennigar AW et al (2008) Prospective relation between catastrophizing and residual pain following knee arthroplasty: two-year follow-up. Pain Res Manag 13:335–341
Hanusch BC, O’connor DB, Ions P et al (2014) Effects of psychological distress and perceptions of illness on recovery from total knee replacement. Bone Jt J 96-B:210–216
Hirakawa Y, Hara M, Fujiwara A et al (2014) The relationship among psychological factors, neglect-like symptoms and postoperative pain after total knee arthroplasty. Pain Res Manag 19:251–256
Hirschmann MT, Testa E, Amsler F et al (2013) The unhappy total knee arthroplasty (TKA) patient: higher WOMAC and lower KSS in depressed patients prior and after TKA. Knee Surg Sports Traumatol Arthrosc 21:2405–2411
Keefe FJ, Lefebvre JC, Egert JR et al (2000) The relationship of gender to pain, pain behavior, and disability in osteoarthritis patients: the role of catastrophizing. Pain 87:325–334
Lewis GN, Rice DA, Mcnair PJ et al (2014) Predictors of persistent pain after total knee arthroplasty: a systematic review and meta-analysis. Br J Anaesth 114(4):551–561
Lingard EA, Riddle DL (2007) Impact of psychological distress on pain and function following knee arthroplasty. J Bone Jt Surg Am 89:1161–1169
Osman A, Barrios FX, Gutierrez PM et al (2000) The Pain Catastrophizing Scale: further psychometric evaluation with adult samples. J Behav Med 23:351–365
Petersen W, Rembitzki IV, Bruggemann GP et al (2014) Anterior knee pain after total knee arthroplasty: a narrative review. Int Orthop 38:319–328
Riddle DL, Keefe FJ, Ang D et al (2012) A phase III randomized three-arm trial of physical therapist delivered pain coping skills training for patients with total knee arthroplasty: the KASTPain protocol. BMC Musculoskelet Disord 13:149
Roos EM, Toksvig-Larsen S (2003) Knee injury and Osteoarthritis Outcome Score (KOOS)—validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes 1:17
Scott CE, Howie CR, Macdonald D et al (2010) Predicting dissatisfaction following total knee replacement: a prospective study of 1217 patients. J Bone Jt Surg Br 92:1253–1258
Seil R, Pape D (2011) Causes of failure and etiology of painful primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 19:1418–1432
Singh JA, Gabriel S, Lewallen D (2008) The impact of gender, age, and preoperative pain severity on pain after TKA. Clin Orthop Relat Res 466:2717–2723
Singh JA, Lewallen DG (2014) Depression in primary TKA and higher medical comorbidities in revision TKA are associated with suboptimal subjective improvement in knee function. BMC Musculoskelet Disord 15:127
Soohoo NF, Lieberman JR, Ko CY et al (2006) Factors predicting complication rates following total knee replacement. J Bone Jt Surg Am 88:480–485
Spielberger CD, O’neil Jr HF, Hansen DN (1972) Anxiety, drive theory, and computer-assisted learning. Prog Exp Pers Res 6:109–148
Sullivan MJ, D’eon JL (1990) Relation between catastrophizing and depression in chronic pain patients. J Abnorm Psychol 99:260–263
Utrillas-Compaired A, De La Torre-Escuredo BJ, Tebar-Martinez AJ et al (2014) Does preoperative psychologic distress influence pain, function, and quality of life after TKA? Clin Orthop Relat Res 472:2457–2465
Wallis JA, Taylor NF (2011) Pre-operative interventions (non-surgical and non-pharmacological) for patients with hip or knee osteoarthritis awaiting joint replacement surgery—a systematic review and meta-analysis. Osteoarthr Cartil 19:1381–1395
Wengler A, Nimptsch U, Mansky T (2014) Hip and knee replacement in Germany and the USA: analysis of individual inpatient data from German and US hospitals for the years 2005 to 2011. Dtsch Arztebl Int 111:407–416
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
There are no financial conflicts related to the study.
Ethical statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (ethic vote no. EA1/305/13) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
W. Petersen receives consultant fees form Karl Storz, Otto Bock and AAP implants. W. Petersen receives lecture fees form Plasmaconcept.
Rights and permissions
About this article
Cite this article
Bierke, S., Petersen, W. Influence of anxiety and pain catastrophizing on the course of pain within the first year after uncomplicated total knee replacement: a prospective study. Arch Orthop Trauma Surg 137, 1735–1742 (2017). https://doi.org/10.1007/s00402-017-2797-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-017-2797-5