Abstract
To examine the morphological changes of the medial meniscus in advanced knee osteoarthritis (OA) we examined 167 knee joints of 106 patients who subsequently underwent total knee joint arthroplasty from January to May, 2007. All 106 patients were females and their ages ranged from 57 to 83 years (mean 68.7 ± 5.6 years). For patients with complete loss of medial joint space by weight-bearing radiography, the meniscal position was assessed by measuring meniscal subluxation and meniscal height. Meniscal morphology was assessed using a modified WORMS MRI-based method. Description of the prevalence of different meniscal morphologies and their respective positions are presented. The predominant type (32.2, 64.1 and 83.8% in anterior horn, mid-body and posterior horn, respectively) of meniscal morphology abnormality was a hypertrophied displaced tear. Medial meniscus height was found to be higher than lateral meniscus height. In persons with an hypertrophied meniscus the height of the medial meniscus was 8.06 ± 1.15, 10.03 ± 1.79, and 8.61 ± 1.57 mm at anterior horn, mid-body and posterior horn, respectively, compared to those in other categories whose height was 6.04 ± 0.92, 5.08 ± 1.68 and 6.43 ± 1.26 mm. A large proportion of persons with end stage varus knee OA have a paradoxically hypertrophied medial meniscus. This new finding of hypertrophied menisci highlights that not all menisci in persons with end stage OA are macerated or destroyed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis (OA) frequently affects the knee and is characterized by significant morphological changes of the whole joint including cartilage loss, subchondral sclerosis and cyst formation, osteophytosis, and meniscal degeneration [1–3]. With advanced disease plain radiographs depict large osteophytes, marked joint space narrowing, severe sclerosis, and definite deformity of bone contour. In contrast to plain radiography, MRI can directly depict changes in soft tissues of the synovial joint. One of the soft tissues prominently involved in OA etiopathogenesis and readily visualized on MRI is the meniscus.
Recent years have seen dramatic advances in our understanding of the integral role of the meniscus for knee function and the characterization of the frequency of meniscal abnormality and its consequences on disease progression. An intact and functional meniscus is integral to loadbearing, shock absorption, stability enhancement, and lubrication in the knee [4, 5]. The absence of a functioning meniscus increases peak and average contact stresses in the medial compartment of the knee in a range of 40–700% [6–8].
Degenerative meniscal lesions such as horizontal cleavages, oblique or complex tears are associated with older age [9], and by the time radiographic OA develops the overwhelming majority of persons will have meniscal lesions [9, 10]. Both meniscal subluxation and meniscal tears are common in knees with OA and appear related to the degree of joint space narrowing on plain radiographs [11–13]. Although meniscal subluxation is found in the absence of tears, generally meniscal subluxation occurs after tearing, and increasing tear magnitude increases the extent of meniscal subluxation and malposition [13]. Moreover, multiple tears and subluxation may ultimately lead to complete maceration or complete resection. The consequence of this damage is a markedly increased rate of disease progression [13–15].
Based on prior reports [13] and existing dogma if OA of the knee has progressed to an advanced stage with complete loss of the medial compartment joint space on radiographs, the medial meniscus and hyaline cartilage may have been completely macerated/destroyed. However, we suspected that not all diseased medial menisci are completely destroyed due to the mobility of the subluxed meniscus itself. At present it remains unknown whether the entire medial meniscus is completely macerated/destroyed, as would be expected to parallel radiographic findings in advanced medial compartment OA. To date, little is known of the morphological changes of the medial meniscus in advanced medial compartment OA. The present study aimed at examining the morphological and positional changes of the medial meniscus in advanced OA.
Materials and methods
Study participants
154 potential participants were screened of whom 106 were deemed eligible. All potential patients presented with varus osteoarthritis. A series of knee radiographs (weight bearing posteroanterior radiographs, weight bearing 30 degrees posteroanterior, lateral, and skyline views) were obtained for each patient to determine whether advanced radiographic OA was present. The radiographs were graded using the Kellgren-Lawrence (K&L) grading scale [16] and scored for medial joint space narrowing (JSN) on a scale of 0 (normal)—3 (total joint space narrowing) with the help of the Osteoarthritis Research Society International (OARSI) atlas [17] by two experienced observers (KAJ, SHH) reading in consensus. If patients had complete medial joint space obliteration (K&L = 4 and JSN = 3) by weight-bearing posteroanterior radiograph, they were eligible for this study.
Ten of the original 154 patients screened were males, and six of these patients were excluded because they failed to meet the above inclusion criteria. As a result, the other four men were also excluded to prevent possible bias due to the low frequency of men in this sample. Another 38 patients were excluded due to secondary OA (i.e., OA associated with trauma, prior surgery, or another disease process), simultaneous lateral compartment OA with lateral joint space narrowing, or a history of previous meniscus-associated surgery. Patients without contraindications for MRI underwent MRI of eligible knee joints. Thus after applying the exclusion criteria above the final sample size was 106 persons (167 knees). We examined 167 knee joints of the 106 eligible patients, who subsequently underwent total knee joint arthroplasty due to symptomatic end-staged osteoarthritis between January and May, 2007.
The hospital ethics committee of Himchan hospital approved the study.
MRI acquisition
Meniscus changes were assessed using a 1.5 T MRI system in sagittal and coronal planes using spin-echo (proton density weighted acquisition) and fast scan (T2-weighted images) techniques. Sagittal and coronal spin-echo proton density weighted acquisition images were acquired using the following parameters: 1800/15/2(TR/TE/NEX), slice thickness 4 mm, inter-slice gap 0.4 mm for coronal images and 0.3 mm for sagittal images, slice thickness 3 mm, and matrix 256 × 256. T2-weighted images were also acquired using the following parameters: 3700/100/2(TR/TE/NEX), slice thickness 4 mm, inter-slice gap 0.4 mm for coronal images, and a slice thickness of 3 mm with an inter-slice gap of 0.3 mm for sagittal images.
MRI interpretation
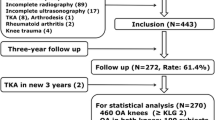
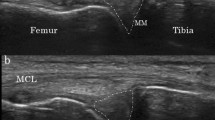
Anterior and posterior horns and mid-bodies of menisci were examined for (1) meniscal morphology, and (2) meniscal position (Figs. 1, 2). During the assessment, the readers were blinded to radiographic results, patient symptoms, patient age, and other clinical data.
Morphology at meniscal portions was assessed using a modification of Peterfy’s whole-organ magnetic resonance imaging score (WORMS) scoring system, where Schematic drawing (a) and MRI finding (b) are representative of the global meniscal scoring system. Grade 0 = intact, 1 = minor radial tear or parrot-beak tear, 2 = nondisplaced tear, 3 = displaced but no tear, 4 = displaced tear or partial resection, 5 = hypertrophied displaced, 6 = hypertrophied displaced tear, and 7 = complete maceration/destruction or complete resection
Meniscal position and dimension was assessed by measuring meniscal subluxation and height for each knee. To determine meniscal height, anterior and posterior horns of menisci were measured in the sagittal plane, which allowed for optimal visualization of greatest meniscal size. Mid-body height was measured in the coronal plane, where medial tibial spine volume was maximal. Meniscal height was measured at the most peripheral edge of each meniscus, regardless of whether the meniscus was “in-place”, subluxed or extruded. To determine meniscal subluxation, anterior subluxation of the anterior horn of the medial and lateral meniscus was assessed in the area where the subluxation was most prominent through multiple sagittal slices. Medial subluxation of the mid-body of lateral and medial meniscus was measured where the volume of the medial tibial spine was greatest. Posterior subluxation of the posterior horn was not measured, because this could not be performed accurately in the sagittal plane. Menisci that were completely macerated or destroyed did not generate measurable subluxation
Meniscal morphology (integrity) was measured independently by two experienced raters (KHY, SCL, respectively, 15 and 10 years of MSK radiology experience), and overall ratings were determined by consensus when necessary. Morphology at each portion of the meniscus was assessed, using a modification of the whole-organ magnetic resonance imaging score (WORMS) assessment method [18]. According to our modification 0 = intact, 1 = minor radial tear or parrot-beak tear, 2 = non-displaced tear, 3 = displaced but no tear, 4 = displaced tear or partial resection, 5 = hypertrophied displaced, 6 = hypertrophied displaced tear, 7 = complete maceration/destruction or complete resection (Fig. 1). The meniscal integrities of anterior and posterior horns of menisci were measured in sagittal and coronal planes, in which meniscal morphology was best observed. Mid-body height was measured where medial tibial spine volume was maximal [13, 19, 20]. “Hypertrophy” was defined to be present when medial meniscus height was >2 mm greater than that of the lateral meniscus, regardless of medial meniscus width, using reference values of normal meniscus size [20]. The inter-rater reliability of meniscal morphology ratings was 0.75 (kappa) for meniscal morphology at the anterior horn of the medial meniscus, 0.79 at the mid-body of the medial meniscus, and 0.77 at the posterior horn of the medial meniscus.
Meniscal position was measured independently by two experienced raters (KAJ, SHH, respectively, 7 and 5 years of experience), and mean values were used for analysis.
Meniscal position was assessed by measuring meniscal subluxation and height for each knee [20]. To determine meniscal height, anterior and posterior horns of menisci were measured in the sagittal plane, which allowed best visualization of greatest meniscal size. Mid-body height was measured in the coronal plane, where medial tibial spine volume was maximal. Meniscal height was measured at the most peripheral edge of each meniscus, regardless of whether the meniscus was “in-place”, subluxed or extruded. To determine meniscal subluxation, anterior subluxation of the anterior horn of the medial and lateral meniscus was assessed in the area where the subluxation is most prominent through multiple sagittal slice. Medial subluxation of the mid-body of lateral and medial meniscus was measured where the volume of the medial tibial spine was greatest. Posterior subluxation of the posterior horn was not measured, because this could not be performed accurately in the sagittal plane. Menisci that were completely macerated or destroyed did not generate measurable subluxation (Fig. 2). The inter-rater reliabilities of meniscal position measurements were determined by calculating intraclass correlation coefficients (ICCs). The ICCs for meniscal height and meniscal subluxation were medial meniscal height at the anterior horn 0.77, mid-body 0.78, and posterior horn 0.81; anterior subluxation at the anterior horn 0.75, and medial subluxation at mid-body 0.79.
Limb alignment assessment
The degree of varus deformity was measured as the femorotibial angle (FTA) by two experienced raters (KAJ, SHH) using a standing long limb radiograph. Femorotibial angles (FTA) were measured by drawing a line along the axis of the femoral shaft to intersect the corresponding line drawn through the tibial shaft. During the assessment, the readers were blinded to MRI results. The reliabilities of femorotibial angle measurements were determined by calculating inter-rater reliabilities using intraclass correlation coefficients (ICCs). ICC for FTA was 0.83.
Histologic examination
Based on preoperative MRI findings, we selected meniscal samples with definite hypertrophy with more than 10 mm height in meniscus body portion. Among the selected hypertrophic menisci samples the first ten consecutive hypertrophied menisci were histologically analyzed by an experienced pathologist. The specimens obtained at surgery were fixed in 10% neutral-buffered formalin and embedded in paraffin wax. The formalin-fixed, paraffin-embedded tissue blocks were cut in 4-μm sections, and then they were stained with hematoxylin and eosin (H-E) for histologic examination.
Statistical analysis
We first described the frequency of mensical integrity for each portion of the meniscus. The medial meniscus heights and medial meniscal subluxation were compared with those of lateral meniscus using the paired sample t test at each meniscal portion, comprised of the anterior horn, mid-body, and posterior horn. Meniscal height and subluxation of hypertrophied meniscus (Grade 5 and Grade 6) at each medial meniscal portion were also compared with those of non-hypertrophied meniscus, using an independent t test. Varus alignment in patients with hypertrophied meniscus at each meniscal portion was also compared with those of non-hypertrophied meniscus, using an independent t test. Correlations between BMI, FTA with meniscus parameters, such as meniscal height and meniscal subluxation were made using correlation coefficients (r) for each knee. All analyses were performed using SPSS 12.0 (SPSS Inc., Chicago, IL, USA). p values of 0.05 or less were considered significant.
Results
All 106 patients were women (ages ranged from 57 to 83 years, mean 68.7 ± 5.6 years). Average patient weight was 63.0 ± 10.2 kg (range; 42–94), average body mass index (BMI) was 27.3 ± 4.5 (range; 18.2–47.4), and average height was 151.1 ± 6.1 cm (range; 137–167).
Meniscal morphology
The meniscal morphology for our study sample is summarized in Table 1. The most frequent morphology observed was a hypertrophied displaced tear (Grade 6), which was the most common morphology in the anterior horn (32.2%), mid-body (64.1%), and in the posterior horn (83.8%) of the medial meniscus.
Meniscal position
The dimensions of subluxation and height of the medial and lateral meniscus for whole sample are summarized in Table 2. The height of the medial meniscus was significantly greater than that of the lateral meniscus in all three locations of measurement (p < 0.05). The subluxation of the medial meniscus was also significantly greater than that of the lateral menisus (p < 0.05).
The data regarding meniscal height and subluxation of hypertrophied meniscus (Grade 5 and Grade 6), and non-hypertrophied meniscus at each medial meniscal portion are summarized in Table 3. In persons with hypertrophied meniscus, the subluxation of the medial meniscus was 6.0 ± 1.86 and 6.26 ± 1.77 mm at anterior horn and mid-body, respectively, compared to those in other categories whose subluxation was 4.21 ± 2.49 and 5.72 ± 1.67 mm. Persons with hypertrophied and non-hypertrophied meniscus showed similar subluxation at mid-body.
Meniscal height in persons with hypertrophied meniscus was significantly greater than those with non-hypertrophied meniscus. In persons with an hypertrophied meniscus the height of the medial meniscus was 8.06 ± 1.15, 10.03 ± 1.79 and 8.61 ± 1.57 mm at anterior horn, mid-body and posterior horn, respectively, compared to those in other categories whose height was 6.04 ± 0.92, 5.08 ± 1.68 and 6.43 ± 1.26 mm. The medial meniscus hypertrophy occurred irrespective of lateral meniscal status which showed similar height of lateral meniscus both in persons with hypertrophied meniscus and other categories. Limb alignment in persons with hypertrophied meniscus did not show significant difference from those of non-hypertrophied meniscus. Limb alignment (FTA) and BMI were not found to be correlated with meniscal position.
Histologic analysis
In all ten consecutive hypertrophied menisci, histologic analysis showed increased non-organized collagen matrix and increased chondroid metaplasia without edematous change (Fig. 3).
Low-power view of hypertrophied meniscus demonstrates increased non-organized collagen matrix without edematous change. (Hematoxylin-eosin stain, ×100) (a) High-power view of hypertrophied meniscus shows increased non-organized collagen matrix without edematous change. (Hematoxylin-eosin stain, ×400) (b). Low-power view of meniscus shows multifocal metaplastic cartilaginous tissue (arrows) in collagenous stroma. (Hematoxylin-eosin stain, ×100) (c) High-power view of meniscus shows metaplastic cartilaginous tissue containing proliferating chondrocytes (arrows) in collagenous stroma. (Hematoxylin-eosin stain, ×400) (d)
Remaining hypertrophied menisci were not analyzed because the first ten consecutive patients showed consistent findings.
Discussion
In the present study, we examined medial meniscal morphology and position in advanced knee OA. We found that the majority of persons had a hypertrophied displaced tear of the meniscus with well-preserved meniscal height. In contrast to other studies we did not find a predominance of macerated/destroyed menisci in persons with knee OA [13].
Radiographically, loss of joint space in OA knees reflects changes in both hyaline articular cartilage and meniscus [19]. Structural changes in the meniscus have been previously described using global meniscal grading and WORMS scores [13, 18, 21, 22]. Based on prior studies one might assume that if OA of the knee progresses to the advanced stage with complete loss of the medial compartment joint space that whole or partial segments of the medial meniscus may be completely macerated or destroyed. However, in the present study the majority of menisci were hypertrophied. MR images depict an apparent increase in meniscal height with overall increased mensical volume and preservation of characteristic meniscal shape. The position of the meniscus, however, is subluxed or extruded accounting for the reduction in joint space (Fig. 4). Our data showed that the mean subluxation was 6.26 ± 1.77 mm at mid-body in persons with hypertrophied meniscus. 108 out of 110 hypertrophied meniscus at mid-body (98.18%) showed subluxation with various values. Remaining 2 meniscus (1.82%) showed dislocation. “Meniscus-in-place” within joint was not found in this study.
In case I, the meniscus shown in the medial compartment of the MR images in both knees was hypertrophied (b), even though a loss of medial joint space was evident in the anteroposterior radiograph with the knee in 30 degrees of flexion (a). In case II, The meniscus shown in MR image of right knee was hypertrophied (d) compared with those of left knee, even though a loss of medial joint space of right knee was evident in the anteroposterior radiograph with the knee in 30 degrees of flexion (c)
This hypertrophied type of morphologic abnormality does not exist in current scoring systems [13, 18, 21, 22]. In the present study, 62.2% (104 knees) of anterior horns, 65.9% (110 knees) of mid-bodies, and 83.8% (140 knees) of posterior horns, meniscal heights were more than 2 mm greater than those of corresponding lateral menisci. Also the mean anterior horn, mid-body, and posterior horn heights in hypertrophied menisci were; 8.06 ± 1.15, 10.03 ± 1.79, and 8.61 ± 1.57 mm, respectively. These height measures are substantially more than what our review of the literature revealed; average meniscus heights in normal knees of 3 and 5 mm [20, 23–25]. Erbagci et al. [20] also reported a mean normal height for the anterior horn of the medial meniscus of 5.32 ± 0.95 mm, a mid-body height of 5.03 ± 0.91 mm, and a posterior horn height of 5.53 ± 0.99 mm. While a hypertrophied meniscus may not be materially and mechanically viable [25] existing dogma appears to be incorrect in suggesting that in the vast majority of persons with end-stage OA the meniscus is destroyed/macerated. The issue, whether this represents a reparative response of the joint or degeneration of the extracellular matrix with myxomatous or edematous changes remains to be determined [26, 27].
Meniscal coverage and meniscal height diminish with increasing meniscal subluxation [13]. However, this prior study revealed that meniscal height was only measured from the non-subluxed edges of medial menisci to edges of the medial tibial plateau, whereas in the present study, meniscal height was measured at the most peripheral edge of hypertrophied medial menisci, and this measurement was affected by meniscal subluxation and joint space widening due to cartilage loss. Therefore, in their study, meniscal heights may have been lower than previously reported.
The present study has several limitations that require consideration. First, all subjects were referred to the hospital for total knee arthroplasty due to severe symptoms; thus the findings may not be generalizable to all persons with knee OA. In addition, as they represent persons with severe deformity they may also not be generalizable to the typical pre-surgical population. Second, although joint spaces were obliterated on weight bearing radiographs, there were some patients that did not complain of knee pain. These patients did not undergo total knee arthroplasty and were excluded from this study. Third, the cohort size (167 knees) was relatively small, and thus, different results may have been obtained had we enrolled a larger community-based sample that included both symptomatic and asymptomatic subjects. Fourth, there is a possibility that menisci in our subjects could change further into complete destruction or maceration, which could affect our findings. Fifth, it is unclear whether the etiology reflects a reparative response, or alternatively if discoid menisci (which are more common in Korea [28, 29]) may portend to the development of hypertrophied displaced tears. Sixth, as our study has enriched the sample with “endogenous or primary OA” by excluding subjects with previous knee injury, surgery, secondary OA and systemic disease, menisci in these specific situations was not investigated. Seventh, because only ten consecutive menisci were included in our histologic study, we cannot rule out the possibility of volume increase of meniscus secondary to the edematous change. Although all ten cases showed consistent histologic findings, further histologic study with a larger number of cases might be needed for this issue in the future. However, we think that MRI findings and consistent histologic findings in ten consecutive menisci might suggest that enlarged meniscus was a form of hypertrophy, rather than form of edematous change, and we also think that paradoxical hypertrophied meniscus should be considered as the form of meniscus change in the end-staged varus osteoarthritis of the knee.
Finally, only women were enrolled in this study. Male patients were excluded because of limited numbers and low prevalence of total knee replacements amongst men in Korea [30]. Accordingly, the extrapolation of our results to male populations is uncertain. Further studies are needed on this topic.
An additional limitation of this study is that we have used a modification of an existing instrument to grade meniscal morphology. As hypertrophied menisci with increased meniscal heights were commonly found in surgical practice, it was evident that the meniscal morphology aspect of existing global meniscal grading system at each meniscal portion would require modification. This modified grading system was devised after a thorough examination of 167 knee joints, and all menisci studies were gradable using this system.
Given the above limitations, we cannot definitively conclude that degenerative menisci in knees with advanced OA are primarily hypertrophied rather than macerated/destroyed. Nevertheless, our data suggest that the medial meniscus is paradoxically hypertrophied in a large proportion of persons with advanced knee OA. The hypertrophied meniscus with increased meniscal height was the predominant form of meniscal abnormality identified in our sample. Therefore, we consider that the existing knee osteoarthritis evaluation methods require modification with respect to determining meniscal morphology scores to include the hypertrophied meniscus [18, 21, 22].
To our knowledge, this is the first description of the prevalence of different meniscal morphologies in persons with end-stage OA and the high prevalence of hypertrophied displaced tears of the meniscus. The role of the hypertrophied meniscus in disease progression, its position within the stage of evolution of meniscal morphologic abnormality, and the etiology of the hypertrophied meniscus remain to be determined.
References
Chan WP, Lang P, Stevens MP, Sack K, Majumdar S, Stoller DW et al (1991) Osteoarthritis of the knee: comparison of radiography, CT, and MR imaging to assess extent and severity. AJR 1991. Am J Roentgenol 157:799–806
Brandt KD, Dieppe P, Radin EL (2008) Etiopathogenesis of osteoarthritis. [Review] [113 refs]. Rheum Dis Clin North Am 34:531–559
Kindynis P, Haller J, Kang HS, Resnick D, Sartoris DJ, Trudell D et al (1990) Osteophytosis of the knee: anatomic, radiologic, and pathologic investigation. Radiology 174:841–846
Seedhom BB, Dowson D, Wright V (1974) Proceedings: functions of the menisci. a preliminary study. Ann Rheum Dis 33:111
Verstraete KL, Verdonk R, Lootens T, Verstraete P, De Rooy J, Kunnen M (1997) Current status and imaging of allograft meniscal transplantation. [Review] [32 refs]. Eur J Radiol 26:16–22
Baratz ME, Fu FH, Mengato R (1986) Meniscal tears: the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee: a preliminary report. Am J Sports Med 14(4):270–275
Fukubayashi T, Kurosawa H (1980) The contact area and pressure distribution pattern of the knee: a study of normal and osteoarthrotic knee joints. Acta Orthopaedica Scandinavica 51(6):871–879
Kurosawa H, Fukubayashi T, Nakajima H (1980) Load-bearing mode of the knee joint: physical behavior of the knee joint with or without menisci. Clin Orthop Related Res 149:283–290
Englund M, Guermazi A, Gale D, Hunter DJ, Aliabadi P, Clancy M et al (2008) Incidental meniscal findings on knee MRI in middle-aged and elderly persons. N Engl J Med 359:1108–1115
Bhattacharyya T, Gale D, Dewire P, Totterman S, Gale ME, McLaughlin S et al (2003) The clinical importance of meniscal tears demonstrated by magnetic resonance imaging in osteoarthritis of the knee. [comment]. J Bone Joint Surg Am 85-A:4–9
Adams JG, McAlindon T, Dimasi M, Carey J, Eustace S (1999) Contribution of meniscal extrusion and cartilage loss to joint space narrowing in osteoarthritis. Clin Radiol 54:502–506
Gale DR, Chaisson CE, Totterman SM, Schwartz RK, Gale ME, Felson D (1999) Meniscal subluxation: association with osteoarthritis and joint space narrowing. Osteoarthr Cartil 7:526–532
Hunter DJ, Zhang YQ, Niu JB, Tu X, Amin S, Clancy M et al (2006) The association of meniscal pathologic changes with cartilage loss in symptomatic knee osteoarthritis. Arthritis Rheum 54:795–801
Biswal S, Hastie T, Andriacchi TP, Bergman GA, Dillingham MF, Lang P (2002) Risk factors for progressive cartilage loss in the knee: a longitudinal magnetic resonance imaging study in forty-three patients. Arthritis Rheum 46:2884–2892
Berthiaume MJ, Raynauld JP, Martel-Pelletier J, Labonte F, Beaudoin G, Bloch DA et al (2005) Meniscal tear and extrusion are strongly associated with progression of symptomatic knee osteoarthritis as assessed by quantitative magnetic resonance imaging. Ann Rheum Dis 64:556–563
Kellgren JH, Lawrence JS (1963) Atlas of standard radiographs. Blackwell, Oxford
Altman RD, Hochberg M, Murphy WAJ, Wolfe F, Lequesne M (1995) Atlas of individual radiographic features in osteoarthritis. Osteoarthr Cartil 3(Suppl A):3–70
Peterfy CG, Guermazi A, Zaim S, Tirman PF, Miaux Y, White D et al (2004) Whole-organ magnetic resonance imaging score (WORMS) of the knee in osteoarthritis. Osteoarthr Cartil 12:177–190
Hunter DJ, Zhang YQ, Tu X, LaValley M, Niu JB, Amin S et al (2006) Change in joint space width: hyaline articular cartilage loss or alteration in meniscus? Arthritis Rheum 54:2488–2495
Erbagci H, Gumusburun E, Bayram M, Karakurum G, Sirikci Sirikci A (2004) The normal menisci: in vivo MRI measurements. Surg Radiol Anat 26:28–32
Hunter DJ, Lo GH, Gale D, Grainger AJ, Guermazi A, Conaghan PG (2008) The reliability of a new scoring system for knee osteoarthritis MRI and the validity of bone marrow lesion assessment: BLOKS (Boston-Leeds Osteoarthritis Knee Score). Ann Rheum Dis 67:206–211
Kornaat PR, Ceulemans RY, Kroon HM, Riyazi N, Kloppenburg M, Carter WO et al (2005) MRI assessment of knee osteoarthritis: Knee Osteoarthritis Scoring System (KOSS)–inter-observer and intra-observer reproducibility of a compartment-based scoring system. Skeletal Radiol 34:95–102
Crues JV III, Ryu R, Morgan FW Meniscal pathology: the expanding role of magnetic resonance imaging. Clin Orthop Relat Res 1990:80–87
Ferrer-Roca O, Vilalta C Lesions of the meniscus. Part I: macroscopic and histologic findings. Clin Orthop Relat Res 1980, 289–300
Fithian DC, Kelly MA, Mow VC Material properties and structure–function relationships in the menisci. [Review] [96 refs]. Clin Orthop Relat Res 1990:19–31
Tchetina EV, Squires G, Poole AR (2005) Increased type II collagen degradation and very early focal cartilage degeneration is associated with upregulation of chondrocyte differentiation related genes in early human articular cartilage lesions. J Rheumatol 32:876–886
Hennerbichler A, Moutos FT, Hennerbichler D, Weinberg JB, Guilak F (2007) Repair response of the inner and outer regions of the porcine meniscus in vitro. Am J Sports Med 35:754–762
Kim SJ, Lee YT, Kim DW (1998) Intraarticular anatomic variants associated with discoid meniscus in Koreans. Clin Orthop Relat Res 356:202–207
Seong SC, Park MJ (1992) Analysis of the discoid meniscus in Koreans. Orthopedics 15:61–65
Kim HA, Kim S, Seo YI, Choi HJ, Seong SC, Song YW et al (2008) The epidemiology of total knee replacement in South Korea: national registry data. Rheumatology 47:88–91
Acknowledgments
The authors wish to thank Ms. Eun Joo Hong and Mr. Kyung Deuk Yoon for collecting patient data.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jung, K.A., Lee, S.C., Hwang, S.H. et al. High frequency of meniscal hypertrophy in persons with advanced varus knee osteoarthritis. Rheumatol Int 30, 1325–1333 (2010). https://doi.org/10.1007/s00296-009-1153-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-009-1153-7