Abstract
The objective of this study is to determine whether meniscal extrusion (ME) of the medial meniscus on ultrasonography affects knee osteoarthritis (KOA) progression during 3-year follow-up. Two hundred seventy volunteers (70 men, 200 women; mean age 60.5 years) participated. Weight-bearing radiographs were evaluated. All subjects had medial radiographic KOA (Kellgren-Lawrence grade [KLG], ≥ 2) in at least one knee at baseline (BL). KLG 2 was defined as moderate KOA (MKOA); KLG 3 and 4 were defined as severe KOA (SKOA). Medial and lateral joint space width (MJSW and LJSW) were measured at the minimum width of femoro-tibial compartment. The medial and lateral osteophyte area (MOPA and LOPA) were measured. Rapid joint space narrowing progression (RP) was defined as ≥ 25% loss of JSW from BL. ME was measured at the medial knee joint space on the medial collateral ligament with ultrasonography. The optimal ME cut-off for RP was determined by ROC curve. The relationship between ME and the longitudinal change of radiographic parameters was elucidated by linear and logistic regression analysis. In the 460 OA knees at BL, both MOPA and LOPA increased, while only MJSW narrowed after 3 years. RP occurred in 25 knees among 281 MKOA knees and 42 among 179 SKOA knees. ME was associated with medial joint space narrowing only in the SKOA group, while the ME was associated with MOPA in the MKOA and SKOA groups. The cut-off value to detect RP was 5.5 mm only in the SKOA group. Ultrasonographic evaluation of medial ME was useful to detect radiographic KOA progression.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Knee osteoarthritis (KOA) is a common disease that compromises multiple joint structures, including cartilage, meniscus, bone, and synovial membrane. KOA is a multi-factorial disease, and patient age, sex, body mass index (BMI), and genetic predisposition; and meniscal lesions and joint malalignment [1,2,3] affect its severity. Radiographic changes associated with KOA, such as osteophytes and narrowed joint spaces, are present in approximately 42.6% of male and 62.4% of female Japanese people over the age of 40; similar rates of OA are seen globally [4]. Patients suffering from KOA experience symptoms including knee pain and stiffness, and disability, which reduce their quality of life. Thus, KOA is a crucial health problem in large-scale older populations.
Menisci have several important functions in the knee, including load distribution, shock absorption that prevents load stress on the articular cartilage, and lubrication and stabilization of the joint during movement. The outer third of the meniscus consists of circumferentially oriented collagen fibers that strongly insert into the tibial plateau and contribute to the generation of hoop stresses [5, 6]. Injury of the meniscus and associated collagen fiber damage can disrupt the hoop strain mechanism and result in biomechanical dysfunction of the meniscus [7, 8]. Recently, meniscal extrusion (ME) of the medial meniscus has been reported in studies using magnetic resonance imaging (MRI) or ultrasonography to investigate the degree of meniscal function [9, 10]. ME is measured as the degree of bulging of the medial meniscus from the medial edge of the tibial plateau at the midpoint of the medial femoral condyle or medial collateral ligament seen on coronal MRI images [11]. ME impairs the mechanical ability of the meniscus, decreases the contact area of the medial compartment of the knee, and increases the load stress on the medial femorotibial joint surface [12]. However, almost all of these previous studies have focused on the cross-sectional correlation between ME and the radiographic severity or pain status of KOA. A limited number of studies have mentioned how ME longitudinally affects OA changes. The current study aimed to elucidate whether ME correlates with joint space narrowing, and we observed a cohort of patients with radiographic KOA who were followed up for 3 years. Our hypothesis was that ME of the medial meniscus affects medial joint space narrowing on plain radiographs due to meniscal impairment.
Methods
The Iwaki Health Promotion Project
The Iwaki Health Promotion Project is a community-based program designed to improve the average life expectancy through regular general health checks. This program began in 2005 and was conducted for a 10-year period. About 1000 adult people aged 20 years or older and living in the Iwaki area of Hirosaki City, located on the west side of Aomori, Japan, participate annually. Physicians, general surgeons, gynecologists, urologists, psychiatrists, dermatologists, dentists, and an orthopedic specialist are involved in this project. We collected epidemiological data related to OA as one aspect of the project [13,14,15,16,17].
Study subjects
A total of 1016 volunteers (385 men and 631 women) out of approximately 12,000 eligible people participated in the Iwaki Health Promotion Project in 2012 (baseline [BL]). The severity of KOA was evaluated by two trained orthopedic surgeons (YI and ES) according to the Kellgren-Lawrence grade (KLG) [18]; KLG 2 or more was defined as definitive radiographic KOA. KLG 2 was defined as moderate KOA (MKOA), and KLG 3 and 4 were defined as severe KOA (SKOA). Of the participants, 452 who did not have radiographic findings of KOA in both knees (KLG 0 and 1) were excluded so that we could focus only on people with definite KOA. In addition, 106 participants declined to undergo radiographic or ultrasonographic examinations, and 15 were excluded due to a history of knee surgery (total knee arthroplasty or arthrodesis), rheumatoid arthritis, or severe knee trauma (meniscal or ligament injury). After 3 years (3Y) of follow-up, 272 participants completed the final follow-up (follow-up rate, 61.4%); of these, two participants were excluded because they underwent total knee arthroplasty. Finally, 270 participants (70 men and 200 women) were included in the analysis; 190 participants had bilateral medial radiographic KOA. Thus, a total of 460 knees were analyzed in the current study (Fig. 1). The ethics committee of our institution approved this study, and all subjects gave written informed consent before participation.
Radiographic evaluation of joint space narrowing and osteophyte formation
At both BL and 3Y, experienced radiologic technicians obtained weight-bearing posteroanterior radiographs of both knees of all participants. The beam was aligned relative to the joint space and positioned parallel to the floor with no angle. The subject bent both knees until the anterior knee surface touched the front of a film cassette to coordinate with a 20–30° semi-flexed position, and the participant rotated the knee with 10° external rotation, supported by foot maps and a goniometer.
All radiographic images of both knees were converted into Joint Photographic Experts Group format files and automatically analyzed using software (KOACAD, Inotech, Ltd., Hiroshima, Japan). After defining a region of interest (ROI) in the KOACAD system that included the tibiofemoral joint space, a vertical neighborhood difference filter was applied to identify locations with high absolute values of difference of scales. Within the ROI, the outline of the femoral condyle was defined as the upper rim of the joint space. The outlines of the anterior and posterior margins of the tibial plateau were similarly drawn, and the middle line between the two outlines was defined as the lower rim of the joint space. The minimum joint space width ([JSW], mm) was further determined as the minimum vertical distance in the joint space area. To measure the osteophyte area, the outlines of the tibia and femur from the inflection point were extended upward to the joint level, and the area that became prominent over the smoothly extended outline was designated as the osteophyte area ([OPA], mm2) [19].
The medial and lateral JSW (MJSW and LJSW) were measured based on the minimum width of the femorotibial compartment. In addition, the medial and lateral osteophyte area (MOPA and LOPA) were measured based on the sum of the area of both the femur and tibia. To compare radiographic knee parameters at both BL and 3Y, we measured the progression of joint space narrowing (JSN) as ΔJSW by subtracting the BL value from the 3Y value; osteophyte formation was consistently measured as ΔOPA by subtracting BL from 3Y. A previous systematic review reported that the annual rate of medial JSN was 0.13 ± 0.15 mm/year [20]. Similarly, progression of more than 0.5 mm/3 years was considered radiographic KOA progression [21]. According to these reviews, rapid JSN progression (RP) in the medial femorotibial joint was defined as ≥ 25% loss of JSW from BL through the 3Y follow-up.
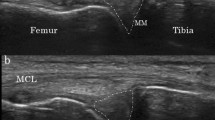
Ultrasonographic evaluation of medial ME
Two examiners (DC, 3-year career; SM, 6-year career) performed ultrasonography of all knees. During the examination, the subjects lay on their back with both knees fully extended and the feet set in the position of natural lateral rotation. Longitudinal ultrasonographic images were obtained as previously described [10]. A linear transducer (12-MHz, Viamo™; Toshiba Medical Systems Corp., Otawara, Japan) was placed over the medial joint space, where the medial collateral ligament could be clearly visualized. A line was drawn to connect the femoral and tibial cortices on the display, and ME was defined as the length of a perpendicular line drawn from that connecting line to the outermost edge of the medial meniscus (Fig. 2). For ME, the inter-rater reliability, expressed as intraclass correlation coefficients [ICC] (2.1), was 0.859 (95% confidence interval [CI] 0.668–0.944), the ICC of DC (1.1) was 0.977 (95% CI 0.942–0.991), and that of SM (1.1) was 0.982 (95% CI 0.953–0.993).
Example of an ultrasound image showing the technique for ME measurement. a The medial meniscus is centrally located and surrounded by the cortices of the femur and tibia. b A line was drawn connecting the cortices of the femur and tibia, and (mm) was defined as the length of a line arising from and perpendicular to the connecting line and ending at the outermost edge (domed dotted line) of the medial meniscus (arrow). ME: meniscal extrusion
Statistical analysis
Data were analyzed using SPSS ver. 22.0 J (SPSS Inc., Chicago, IL, USA). The mean continuous values were compared using a Mann-Whitney U test between (1) patients who dropped out and those who were completely followed up, (2) MKOA and SKOA, and (3) the RP and non-RP group in each KOA group at BL. Categorical values were compared with a χ2 test. The mean radiographic values at BL and 3Y were compared with Wilcoxon’s rank test. To evaluate the relationship between (1) ME and JSN and (2) ME and osteophyte formation, we applied two multiple linear regression models. In one model, ΔJSW was the dependent variable and ME was the independent variable; in the other, ΔOPA was the dependent variable and ME was the independent variable. Both regression models were adjusted for age, sex, height, BMI, Knee Injury and Osteoarthritic Outcome Score (KOOS) pain scale, and radiographic parameters (JSW and OPA) at BL. To evaluate the risk of ME for RP, a receiver operating curve (ROC) was drawn to obtain the optimal cut-off value. Additionally, multiple logistic regression analysis was applied with the prevalence of RP as the dependent variable and with the ME cut-off as the independent variable. This logistic model was also adjusted by age, sex, height, BMI, KOOS pain scale, and radiographic parameters at BL.
Results
Change of radiographic and ultrasonographic parameters during the 3-year follow-up
At BL, the patients who underwent complete follow-up were younger compared with those who dropped out. The mean age and BMI in the SKOA group were significantly higher than in the MKOA group, whereas the mean height and KOOS scale in the SKOA group were lower than those in the MKOA group (Table 1). Among participants with MKOA, the mean MJSW in the RP group was larger than that in the non-RP group. In those with SKOA, the mean ME, MOPA, LJSW, and LOPA in the RP group were larger than those in the non-RP group (Table 2).
At 3Y follow-up, the mean MJSW decreased from 3.79 ± 0.91 mm at BL to 3.57 ± 1.02 mm at 3Y (P < 0.001); the mean OPA increased from BL (MOPA: 16.84 ± 35.38 mm2; LOPA: 7.55 ± 18.25 mm2) to 3Y (MOPA: 23.92 ± 41.59 mm2; LOPA: 10.80 ± 24.13 mm2; P < 0.001 for both; Table 2). However, LJSW did not change.
In the RP group, the mean MJSW decreased from BL to 3Y in both the MKOA (4.67 ± 0.78 to 2.80 ± 0.83 mm; P < 0.001) and SKOA (3.32 ± 1.06 to 1.85 ± 0.92 mm; P < 0.001) groups. Compared with the non-RP group, in the RP group, MOPA significantly increased at 3Y follow-up in both the MKOA (8.24 ± 13.63 to 18.39 ± 13.63 mm2; P = 0.005) and SKOA groups (45.37 ± 43.71 to 73.17 ± 56.04 mm2; P < 0.001, Table 2).
Linear regression analysis for the interrelationship between medial ME at baseline and radiographic changes
According to the linear regression analysis, the ME value at BL significantly correlated with ΔMJSW, ΔMOPA, and ΔLOPA. The adjusted linear regression model showed that ME correlated with ΔMJSW only in the SKOA group, ΔLOPA only in the MKOA group, and ΔMOPA in both the MKOA and SKOA groups (Table 3).
In ΔMJSW, the adjusted regression model showed that a 1-mm increase of ME at BL correlated with a 0.164-mm decrease of MJSW at 3Y follow-up in the SKOA group (B = −0.164; β = −0.349; P = 0.001). In ΔMOPA, a 1-mm increase of ME at BL correlated with a 5.241-mm2 increase of MOPA after 3Y follow-up in the MKOA group (B = 5.421; β = 0.346; P < 0.001) and a 7.033-mm2 increase in the SKOA group (B = 7.033; β = 0.388; P < 0.001; Table 3).
Logistic regression analysis for the interrelationship between medial ME at BL and rapid progression in medial JSN
According to the ROC, there was no optimal ME cut-off to detect RP in the MKOA group. On the other hand, 5.5 mm was the optimal ME cut-off value to detect RP in the SKOA group (area under the curve = 0.730; odds ratio: 3.708; P < 0.001; Fig. 3). The adjusted logistic regression analysis showed that the odds of RP was 3.542 times higher in those having an extruded medial meniscus that extended by 5.5 mm or more, compared with protrusion less than 5.5 mm in the SKOA group (Table 4).
Discussion
The current study evaluated ME in the meniscus using ultrasonography, and it elucidated the longitudinal relationship between ME and radiographic OA changes, comparing both at BL and at 3Y follow-up. In participants with radiographic KOA at BL, a more medially extruded medial meniscus at baseline affected medial JSN and osteophyte formation at 3Y follow-up, even after adjusting for the covariates of age, sex, physique, knee symptoms, and radiographic parameters at BL.
The natural history of JSN in patients with KOA is known to be relatively slow. Mazzuka et al. reported that the medial knee joint space narrows less than 0.10 mm/year on plain radiographs in the general population with KOA, whereas more than 0.20 mm/year was the rate of medial JSN in patients with KOA who suffered from any symptom and visited a hospital [22]. Consistent with this, a more recent systematic review reported that the annual rate of medial JSN was 0.13 ± 0.15 mm/year [20]. Moreover, progression of more than 0.5 mm/3Y was considered to be radiographic KOA progression [21]. Thus, the JSN rate in the medial femorotibial joint of the RP group relatively and rapidly progresses, considering the natural course of medial JSN. There is considerable evidence showing that narrower medial joint space seen on radiographs correlates with the progression of articular cartilage degeneration or loss [23,24,25,26,27,28,29,30,31]. The current study supported the idea that a more extruded meniscus significantly affected rapid OA progression.
Many previous studies have mentioned the longitudinal association between ME and joint degeneration, evaluated not by ultrasonography but by MRI. Felson et al. reported that in their study with an 84-month follow-up period, any ME graded using the whole-organ magnetic resonance imaging score (WORMS) showed a significant risk for the incidence of radiographic KOA (KLG 0/1 to grade 2) [32]. Similarly, Guermazi et al. reported that in their study with 30 months of follow-up, participants having any ME graded using WORMS had significant loss of joint cartilage in both the medial and lateral femorotibial compartments, surveyed by MRI [33]. Emmanuel et al. elucidated whether quantitative ME correlated with the incidence of radiographic KOA, and they concluded that the earlier incidence group (1–2 years from BL) had a more extruded medial meniscus, compared with those in the non-incident group [34]. These recent studies supported that ME correlates with the impairment of meniscal function, and with the longitudinal risk of developing or progressive OA changes in the knee joint.
Unfortunately, there is less evidence to support ultrasonography’s superior ability to detect OA progression in the knee joint compared with MRI. Bevers et al. were the first to report the longitudinal relationship between ultrasonographic ME and the progression of radiographic KOA [35]. They concluded that in their 2-year follow-up period, the cut-off of 3.0 mm was not correlated with the progression of more than two grade changes according to the Osteoarthritic Research Society International atlas, or conversion to total knee arthroplasty. There were definite differences between that study and ours, including (1) the current study had a 3-year follow-up period, (2) radiographic evaluations were not categorical but quantitative (medial JSW and osteophyte area), and (3) the study elucidated the cut-off value for rapid KOA progression without conforming to the conventional cut-off of 3.0 mm [36,37,38]. Since the degree of ME varies according to the radiographic severity of KOA at BL [10], a different cut-off is desirable to survey the risk of OA progression using ultrasonography. In addition, the ME had different associations with the degree of medial JSN between moderate and severe KOA. Future studies will show in detail how meniscal impairment affects the pathology of KOA.
The current study includes several limitations. First, meniscal injury was not fully investigated with MRI, or even by ultrasonography, although certain types of meniscal injury, particularly those that disrupt the circumferential fibers that maintain the shape of the meniscus, are more likely to result in meniscal displacement [11, 39, 40]. It is important to understand the relationship between meniscal injury and ME, but the usefulness of ultrasonography to diagnose meniscal tears remains controversial [41]. Ultrasonographic examination of the menisci is limited by the presence of artifacts that originate from adjacent bone surfaces, which makes it difficult to detect the inner meniscal margins [42]. Thus, the development of a novel and concise method to diagnose OA by ultrasonographic examination would be very useful in clinical practice. Evaluation of ME by ultrasonography is easier than that of the entire meniscus for detecting injury because ME can be determined by visualizing one portion of the medial meniscus, which is close to the skin and easy to visualize [43, 44]. Second, two examiners performed the current ultrasonographic evaluations, and there may be concerns about interclass reliability. However, a previous report suggested that the inter-rater reliability of ME severity using ultrasonography is good, even for inexperienced examiners [45]. The inter-rater reliability for evaluating ME was also good in this study. Third, the current study had short-term follow-up. ME was not associated with the medial JSN, although it was associated with medial osteophyte formation in MKOA (those having KLG 2 knees). Future long-term cohort studies will clarify in detail the association between ME and radiographic medial JSN. Despite these limitations, the current study showed that ultrasonography has the potential to survey the risk of OA progression in the knee joint.
In summary, using ultrasonography, more medially extruded medial menisci affected medial JSN in patients with KOA when the BL and 3Y follow-up were compared. Ultrasonography is useful to evaluate the rapid progression of OA change in patients with OA seen on radiographs.
References
Ledingham J, Regan M, Jones A, Doherty N (1995) Factors affecting radiographic progression of knee osteoarthritis. Ann Rheum Dis 54:53–58
Felson DT, Lawrence RC, Dieppe PA, Hirsch R, Helmick CG, Jordan JM et al (2000) Osteoarthritis: new insights. Part 1: the disease and its risk factors. Ann Intern Med 133:635–646
Hunter DJ (2011) Osteoarthritis. Best Pract Res Clin Rheumatol 25:801–814
Yoshimura N, Muraki S, Oka H, Mabuchi A, En-Yo Y, Yoshida M et al (2009) Prevalence of knee osteoarthritis, lumbar spondylosis, and osteoporosis in Japanese men and women: the research on osteoarthritis/osteoporosis against disability study. J Bone Miner Metab 9:620–628
Bullough PG, Munuera L, Murphy J, Weinstein AM (1970) The strength of the menisci of the knee as it relates to their fine structure. J Bone Joint Surg Br 52:564–567
Levy IM, Torzilli PA, Warren RF (1982) The effect of medial meniscectomy on anterior-posterior motion of the knee. J Bone Joint Surg Am 64:883–888
Jones RS, Keene GC, Learmonth DJ, Bickerstaff D, Nawana NS, Costi JJ et al (1996) Direct measurement of hoop strains in the intact and torn human medial meniscus. Clin Biomech (Bristol, Avon) 11:295–300
Messner K, Gao J (1998) The menisci of the knee joint. Anatomical and functional characteristics, and a rationale for clinical treatment. J Anat 193:161–178
Gale DR, Chaisson CE, Totterman SM, Schwartz RK, Gale ME, Felson D (1999) Meniscal subluxation: association with osteoarthritis and joint space narrowing. Osteoarthr Cartil 7:526–532
Kawaguchi K, Enokida M, Otsuki R, Teshima R (2012) Ultrasonographic evaluation of medial radial displacement of the medial meniscus in knee osteoarthritis. Arthritis Rheum 64:173–180
Ohishi T, Suzuki D, Yamamoto K, Banno T, Shimizu Y, Matsuyama Y (2014) Medial extrusion of the posterior segment of medial meniscus is a sensitive sign for posterior horn tears. Knee 21:112–118
Bloecker K, Guermazi A, Wirth W, Benichou O, Kwoh CK, Hunter DJ et al (2013) Tibial coverage, meniscus position, size and damage in knees discordant for joint space narrowing—data from the osteoarthritis initiative. Osteoarthr Cartil 21:419–427
Inoue R, Ishibashi Y, Tsuda E, Yamamoto Y, Matsuzaka M, Takahashi I et al (2011) Knee osteoarthritis, knee joint pain and aging in relation to increasing serum hyaluronan level in the Japanese population. Osteoarthr Cartil 19:51–57
Sasaki E, Tsuda E, Yamamoto Y, Iwasaki K, Inoue R, Takahashi I et al (2013) Serum hyaluronan levels increase with the total number of osteoarthritic joints and are strongly associated with the presence of knee and finger osteoarthritis. Int Orthop 37:925–930
Sasaki E, Tsuda E, Yamamoto Y, Maeda S, Inoue R, Chiba D et al (2014) Nocturnal knee pain increases with the severity of knee osteoarthritis, disturbing patient sleep quality. Arthritis Care Res (Hoboken) 66:1027–1032
Sasaki E, Tsuda E, Yamamoto Y, Maeda S, Inoue R, Chiba D et al (2015) Serum hyaluronic acid concentration predicts the progression of joint space narrowing in normal knees and established knee osteoarthritis—a five-year prospective cohort study. Arthritis Res Ther 17:283
Chiba D, Tsuda E, Maeda S, Sasaki E, Takahashi I, Nakaji S et al (2016) Evaluation of a quantitative measurement of suprapatellar effusion by ultrasonography and its association with symptoms of radiographic knee osteoarthritis: a cross-sectional observational study. Arthritis Res Ther 18:181
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteoarthrosis. Ann Rheum Dis 16:494–502
Oka H, Muraki S, Akune T, Mabuchi A, Suzuki T, Yoshida H et al (2008) Fully automatic quantification of knee osteoarthritis severity on plain radiographs. Osteoarthr Cartil 16:1300–1306
Emrani PS, Katz JN, Kessler CL, Reichmann WM, Wright EA, McAlindon TE et al (2008) Joint space narrowing and Kellgren-Lawrence progression in knee osteoarthritis: an analytic literature synthesis. Osteoarthr Cartil 16:873–882
Ornetti P, Brandt K, Hellio-Le Graverand MP, Hochberg M, Hunter DJ, Kloppenburg M et al (2009) OARSI-OMERACT definition of relevant radiological progression in hip/knee osteoarthritis. Osteoarthr Cartil 17:856–863
Mazzuca SA, Brandt KD, Katz BP (1997) Is conventional radiography suitable for evaluation of a disease-modifying drug in patients with knee osteoarthritis? Osteoarthr Cartil 5:217–226
Amin S, LaValley MP, Guermazi A, Grigoryan M, Hunter DJ, Clancy M et al (2005) The relationship between cartilage loss on magnetic resonance imaging and radiographic progression in men and women with knee osteoarthritis. Arthritis Rheum 52:3152–3159
Mazzuca SA, Brandt KD, Katz BP, Lane KA, Buckwalter KA (2006) Comparison of quantitative and semiquantitative indicators of joint space narrowing in subjects with knee osteoarthritis. Ann Rheum Dis 65:64–68
Nevitt MC, Peterfy C, Guermazi A, Felson DT, Duryea J, Woodworth T et al (2007) Longitudinal performance evaluation and validation of fixed-flexion radiography of the knee for detection of joint space loss. Arthritis Rheum 56:1512–1520
Pelletier JP, Raynauld JP, Berthiaume MJ, Abram F, Choquette D, Haraoui B et al (2007) Risk factors associated with the loss of cartilage volume on weight-bearing areas in knee osteoarthritis patients assessed by quantitative magnetic resonance imaging: a longitudinal study. Arthritis Res Ther 9:R74
Eckstein F, Wirth W, Hudelmaier MI, Maschek S, Hitzl W, Wyman BT et al (2009) Relationship of compartment-specific structural knee status at baseline with change in cartilage morphology: a prospective observational study using data from the osteoarthritis initiative. Arthritis Res Ther 11:R90
Eckstein F, Wirth W, Hunter DJ, Guermazi A, Kwoh CK, Nelson DR et al (2010) Magnitude and regional distribution of cartilage loss associated with grades of joint space narrowing in radiographic osteoarthritis—data from the osteoarthritis initiative (OAI). Osteoarthr Cartil 18:760–768
Wirth W, Buck R, Nevitt M, Le Graverand MP, Benichou O, Dreher D et al (2011) MRI-based extended ordered values more efficiently differentiate cartilage loss in knees with and without joint space narrowing than region-specific approaches using MRI or radiography—data from the OA initiative. Osteoarthr Cartil 19:689–699
Wirth W, Nevitt M, Hellio Le Graverand MP, Lynch J, Maschek S, Hudelmaier M et al (2014) Lateral and medial joint space narrowing predict subsequent cartilage loss in the narrowed, but not in the non-narrowed femorotibial compartment—data from the osteoarthritis initiative. Osteoarthr Cartil 22:63–70
Maschek S, Wirth W, Ladel C, Hellio Le Graverand MP, Eckstein F (2014) Rates and sensitivity of knee cartilage thickness loss in specific central reading radiographic strata from the osteoarthritis initiative. Osteoarthr Cartil 22:1550–1553
Felson DT, Niu J, Neogi T, Goggins J, Nevitt MC, Roemer F et al (2016) Synovitis and the risk of knee osteoarthritis: the MOST study. Osteoarthr Cartil 24:458–464
Guermazi A, Eckstein F, Hayashi D, Roemer FW, Wirth W, Yang T et al (2015) Baseline radiographic osteoarthritis and semi-quantitatively assessed meniscal damage and extrusion and cartilage damage on MRI is related to quantitatively defined cartilage thickness loss in knee osteoarthritis: the multicenter osteoarthritis study. Osteoarthr Cartil 23:2191–2198
Emmanuel K, Quinn E, Niu J, Guermazi A, Roemer F, Wirth W et al (2016) Quantitative measures of meniscus extrusion predict incident radiographic knee osteoarthritis—data from the osteoarthritis initiative. Osteoarthr Cartil 24:262–269
Bevers K, Vriezekolk JE, Bijlsma JW, van den Ende CH, den Broeder AA (2015) Ultrasonographic predictors for clinical and radiological progression in knee osteoarthritis after 2 years of follow-up. Rheumatology (Oxford) 54:2000–2003
de Miguel ME, Cobo Ibáñez T, Usón Jaeger J, Bonilla Hernán G, Martín Mola E (2006) Clinical and ultrasonographic findings related to knee pain in osteoarthritis. Osteoarthr Cartil 14:540–544
Wu PT, Shao CJ, Wu KC, Wu TT, Chern TC, Kuo LC et al (2012) Pain in patients with equal radiographic grades of osteoarthritis in both knees: the value of gray scale ultrasound. Osteoarthr Cartil 20:1507–1513
Bevers K, Bijlsma JW, Vriezekolk JE, van den Ende CH, den Broeder AA (2014) The course of ultrasonographic abnormalities in knee osteoarthritis: 1 year follow up. Osteoarthr Cartil 22:1651–1656
Choi CJ, Choi YJ, Lee JJ, Choi CH (2010) Magnetic resonance imaging evidence of meniscal extrusion in medial meniscus posterior root tear. Arthroscopy 26:1602–1606
Hwang BY, Kim SJ, Lee SW, Lee HE, Lee CK, Hunter DJ et al (2012) Risk factors for medial meniscus posterior root tear. Am J Sports Med 40:1606–1610
Azzoni R, Cabitza P (2002) Is there a role for sonography in the diagnosis of tears of the knee menisci? J Clin Ultrasound 30:472–476
Lee D, Bouffard JA (2001) Ultrasound of the knee. Eur J Ultrasound 14:57–71
Naredo E, Cabero F, Palop MJ, Collado P, Cruz A, Crespo M (2005) Ultrasonographic findings in knee osteoarthritis: a comparative study with clinical and radiographic assessment. Osteoarthr Cartil 13:568–574
Friedman L, Finlay K, Jurriaans E (2001) Ultrasound of the knee. Skelet Radiol 30:361–377
Iagnocco A, Perricone C, Scirocco C, Ceccarelli F, Modesti F, Gattamelata A et al (2012) The interobserver reliability of ultrasound in knee osteoarthritis. Rheumatology (Oxford) 51:2013–2019
Acknowledgements
We are extremely grateful to all participants in the Iwaki Health Promotion Project and to the staff of our department who conducted interviews and collected the data.
Funding
This study is funded by the Ministry of Education, Culture, Sports, Science and Technology of Japan (No. 18200044), the Japanese Society for the Promotion of Science (No. 21500676), Karoji Memorial Fund for Medical Research (No. 5310139302), and JOA-Subsidized Science Project Research from the Japanese Orthopaedic Association.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Rights and permissions
About this article
Cite this article
Chiba, D., Maeda, S., Sasaki, E. et al. Meniscal extrusion seen on ultrasonography affects the development of radiographic knee osteoarthritis: a 3-year prospective cohort study. Clin Rheumatol 36, 2557–2564 (2017). https://doi.org/10.1007/s10067-017-3803-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-017-3803-6