Abstract
Objectives: To investigate the potential of a new osteogeometric technology based on digital X-ray radiogrammetry (DXR) as a diagnostic tool for quantification of severity-dependent osteoporosis, and to distinguish between inflammation-mediated and corticoid-induced variations of bone mineralisation in patients suffering from rheumatoid arthritis. Methods: Ninety-six patients (duration of disease: <18 months) underwent retrospective calculations of bone mineral density (DXR-BMD) and metacarpal index (MCI) by DXR, which were calculated from plain radiographs of the non-dominant hand. For comparison, pQCT-calculated BMD (total, cortical-subcortical and trabecular partition of bone tissue) was done on the distal radius. Severity was classified using Ratingen Score by two independent radiologists, and divided into three main groups. In addition, the patients were separated into those with corticoid medication (n=44; 5 mg/day over a half year period) and a control group (n=52) without any corticoid therapy. Results: Correlations between DXR-BMD and MCI versus pQCT parameters were all significant (0.36<R<0.71; p<0.01), independent of corticoid therapy. Only in the group without corticoid application, the correlation between DXR-BMD and pQCT-BMD (cortical) showed no significant association. For patients with corticoid therapy, our data revealed the lowest correlation coefficient between DXR parameters and pQCT-BMD (trabecular). Without a difference in comparison to corticoid therapy, the significant relative decrease of BMD estimated by DXR between the highest and lowest score was between 11.1% and 14.3% and for MCI between 15.8% and 17.8%. The also significant relative decrease of trabecular BMD using pQCT varied from 10.3% to 16.9%, whereas no significant results could be verified for pQCT-BMD (cortical and total). Conclusions: Digital radiogrammetry can precisely estimate severity-dependent cortical reduction of bone mineral density in patients suffering from rheumatoid arthritis both with and without corticoid therapy, and seems to be able to distinguish the side effects of antirheumatic treatment from the disease-related periarticular bone loss. The detection and quantification of periarticular osteoporosis by DXR could be an important diagnostic tool in early rheumatoid arthritis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is a systemic inflammatory disease [1]; in 80% of patients with RA the small joints of the hand are affected leading to destruction of periarticular tissue, including juxta-articular bone [2]. Osteoporosis is a major clinical complication in RA and occurs in two forms: periarticular osteopenia in near proximity to inflamed joints, which is a typical phenomenon in early RA, and generalised osteoporosis affecting the axial and appendicular bones occurring during the course of rheumatoid disease [3–5]. Generalised bone loss may be influenced by immobility, the inflammatory process itself and treatments such as steroids, whilst periarticular demineralisation is probably due to local release of inflammatory agents [6]. Many studies have revealed the influence of different cytokines with respect to the dysregulation of bone and cartilage remodelling [7]. Recently, receptor activators of nuclear κB ligand (RANKL) and osteoprotegerin (OPG), a decoy receptor for RANKL, have been identified as central regulators of osteoclast recruitment and activation. OPG and RANKL production is modulated by various cytokines, growth factors and hormones. In affected synovium, both fibroblasts and activated T cells express RANKL and maintain osteoclast recruitment and activation. Thus, OPG and RANKL are important molecular agents which appear to systemically influence bone resorption in the juxta-articular bone [8].
Osteoporosis in RA, which results in low bone mineral density and microarchitectural deterioration of bone tissue and leads to diminished biomechanical competence of the skeleton, commonly causes low-trauma or atraumatic fractures, particularly at the spine, hip and wrist [9–11]. The high fracture risk of patients suffering from RA contributes substantially to morbidity, mortality and health care costs [12–14].
Because the hand shows the earliest manifestation of RA [1], radiographs of the hands are regularly necessary to verify the success of the antirheumatic therapy as well as the progression of the disease during the course of rheumatoid arthritis [15, 16]. Despite the fact that onset of RA begins frequently in the small joints of the hand, hand X-rays of most patients are characterised by absence of erosions or joint-space narrowing, whereas periarticular bone loss is a typical phenomenon in early RA [17, 18]. Kalla et al. [19] postulate a high prevalence of metacarpal osteopenia (55%) in young patients with RA.
The periarticular (i.e. metacarpal) demineralisation, a qualitative parameter regarding Steinbroker and Larsen scoring, may precede erosions [17]. Yet osteopenia is only very imprecisely verified using hand X-rays at a reduction of more than 35% [20].
In 1960 Barnett and Nordin [21] developed a new technique to assess bone status from radiographs. The sum of the two cortical thicknesses of the middle metacarpal was calculated, and then divided by the width (i.e. Barnett and Nordin index or metacarpal index). Recently, clinical application of radiogrammetry has been significantly improved with refinement, computerisation and the use of algorithms for automatic image analysis [22, 23]. Our study is performed with the Pronosco X-Posure System (Version 2.0; Pronosco-Sectra, Sweden), which provides metacarpal index and bone mineral density by analysing plain radiographs of the non-dominant hand.
Peripheral quantitative computed tomography is an osteodensitometric technique, which allows independent quantification of trabecular and cortical bone at the distal radius in close proximity to the carpus [24, 25]. As the carpus is frequently involved in RA, and periarticular bone loss is a characteristic feature, pQCT seems an ideal method to study periarticular bone variations related to RA and to compare these measurements with the cortical DXR calculations. Accordingly, the cortical pQCT measurements can be more precisely compared to cortical DXR-BMD calculations, in contrast to DXA-BMD data measured as combined trabecular and also cortical bone partition without the possibility of differentiation between the different bone partitions [24, 25]. For these reasons we chose the precise pQCT as the reference method for quantification of bone loss in RA.
In this study, we have evaluated the potential of DXR to quantify disease-related cortical demineralisation, as compared to pQCT, and to differentiate between severity-dependent, RA-specific bone loss and generalised osteoporosis mainly caused by corticoid influence.
Patients and methods
Patients
Ninety-six Caucasian patients (75 female/21 male) were enrolled in this retrospective cross-sectional study. Mean age was 58 years (SD±13.4 years) with a range of 20–83 years.
All patients had suffered from RA (as defined by the American College of Rheumatology, [26]) for at least 6 months (duration of disease: <18 months) and were recruited from our out-patient department. No pre-selection regarding severity of rheumatoid arthritis or the individual therapy protocol was performed. Twenty-two patients were treated with methotrexate and 61 subjects with NSAIDs. Fourty-four patients had been on long-term low-dose prednisolone therapy (5 mg/day over a 6-month period). The remaining 52 patients had received neither systemic corticosteroids and DMARDs nor immune-modulating drugs. Subjects with abnormal renal function (serum creatinine >130 μmol/l), or who were on hormone replacement therapy/biphosphonates, or who had other conditions known to affect bone metabolism were excluded. Informed consent was obtained, and the study received local ethical committee approval. As a special note, the authors emphasise that all radiographs used for DXR calculations and all pQCT-measurements were routinely performed, without exception based on clinical considerations. No patient additionally underwent both pQCT-measurements and the transaction of X-ray imaging (for DXR calculation) for research purposes.
Each individual underwent digitally-prepared radiographs of the non-dominant hand (using standardised technical parameters) for the assessment of RA-related progression, and measurements of pQCT-BMD on the ultra-distal radius were performed within the study time-plan of 3 days provided for clinical purposes. Exclusion criteria were signs of fracture and visible osteosynthetic material in the right and left upper extremities (including ulna, radius and hand).
Each X-ray was independently scored by two separate observers using the Ratingen Score [27], which considers 38 affected joints of the feet and hands (total sum of points: 190). In cases of ambiguity, a third radiologist reviewed the radiographs; then the individual sum of scoring points is divided by the 38 evaluated joints and the patients were subdivided into the following groups:
-
Grade 1: minor changes (equivalent to Ratingen Score 1: few small erosions, <20% of the joint surface is destroyed)
-
Grade 2: moderate changes (equivalent to Ratingen Scores 2 and 3: 21–60% of the joint surface is destroyed)
-
Grade 3: severe changes (equivalent to Ratingen Scores 4 and 5: >61% of the joint surface is destroyed)
Methods
The pQCT of the ultradistal radius of the non-dominant forearm was performed using the Stratec XCT-900 scanner (Version 3.3; Stratec Medizintechnik GmbH, Pforzheim, Germany). The CT bone scanner used an X-ray tube as source of radiation. Following a coronal computed radiograph (scout scan), the distal end of the radius was marked with a reference line. A 2.5 mm-thick axial measurement CT scan occurred at a distance proximal to the ulna styloid process of 4% of the total ulnar length, thus clearly differentiating the radius from the cubitus [25]. Radial measurements were made automatically, resulting in a minor effective radiation dose (<0.1 mSv). The software calculated the BMD as truly volumetric measurements in mg/cm3 for total (overall radial BMD), trabecular (the central 45% of the radius), subcortical (cortical envelope with a small rim of subcortical trabecular bone) and cortical BMD (cortical envelope). The XCT-900 was calibrated daily with a bone standard supplied by Stratec. In our study, in vivo short-term precision of pQCT, expressed as the coefficient of variation, is 1.18% (BMD total), 1.29% (BMD trabecular) and 1.67% (BMD cortical), and thus shows similar values to those in published data [25].
The Pronosco X-Posure System (Version 2.0, Sectra, Sweden) was used to determine bone mineral density (DXR-BMD) and metacarpal index (MCI) based on radiogrammetry, requiring radiographs of the non-dominant hand. All plain radiographs of the hand were acquired by a Polydoros SX 80 (Siemens, Erlangen, Germany) under the following standardised conditions: FFD 1 m filter 1.0, aluminium 80, tube voltage 42 kV, exposure 4 mAs, AGFA Scopix Laser 2 B 400.
The digital radiographs were printed and subsequently scanned into the system. The system itself checked the quality of the scanned images, and interrupted the examination in case of inadequate quality. The computer algorithms automatically defined regions of interest (ROIs) around the narrowest bone parts of the metacarpalia II, III and IV, and subsequently determined the outer and inner cortical edges of the studied cortical bone parts. Apart from placing the radiography on the CCD-based desktop flatbed scanner, there was otherwise no operator interaction connected to the DXR calculations. The analysed images and their ROIs were displayed on the computer monitor.
The mean of the cortical thickness and overall bone cortical thickness of the second, third and fourth metacarpal were calculated. Subsequently, the cortical volume per area (VPA) was calculated for each bone. DXR-BMD—based on the mean VPA—was computed with a correction for the estimated porosity index. The porosity index is a technical parameter given as a value between 1 and 19, which is derived from the area percentage of local intensity minima found in the cortical part of the bone relative to the entire cortical area. The MCI obtains the mean cortical thickness normalised with the mean outer bone diameter [23]. In a study by Black et al. [28] the short-term precision accounted for 0.65% (Version 1.0), and in our own study accounted for 0.24% (MCI) versus 0.19% (DXR-BMD).
Statistical analysis
Results were expressed as mean and standard deviation. Correlation analyses of BMD results between DXR and pQCT were calculated using Spearman’s test; values of p<0.05 were considered as significant. The significance of severity-dependent reduction of BMD was calculated with Pearson’s correlation coefficient. The statistical analysis was performed using SPSS Version 10.13.
Results
Comparison between DXR and pQCT
It was possible to estimate BMD and MCI using DXR and to measure the different pQCT-BMD values in all patients.
All correlations between the different parameters of both techniques were significantly positive, independent of corticoid application (see Table 1). For all patients, the highest correlation was observed between MCI and total pQCT-BMD (R=0.69, p<0.01).
No significant association could be found between DXR-BMD and cortical pQCT-BMD in patients without corticoid intake (R=0.20); also a comparatively minor association was observed between MCI and cortical pQCT-BMD (R=0.40; p<0.05). Furthermore, the association between DXR parameters and trabecular pQCT revealed lower results for the steroid group in comparison to patients without corticoid therapy, as shown in Table 1.
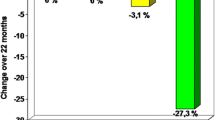
Severity-dependent reduction of periarticular bone mineral density
For all individuals, mean DXR-BMD was reduced from 0.49 g/cm2±0.05 (grade 1) to 0.42 g/cm2±0.08 (grade 3, see Table 2), and MCI shows a reduction from 0.45±0.08 (grade 1) to 0.37±0.07 (grade 3). In this context, Pearson’s correlation coefficients for DXR-BMD and MCI were R=−0.36 vs −0.47; p<0.01, and for pQCT-BMD (trabecular) the Pearson correlation coefficient was R=−0.31; p<0.01. For all patients, the relative reduction of MCI (17.8%) and the DXR-BMD (14.3%, see Table 2) showed a significant association between the severity of the RA and the periarticular reduction of cortical bone mass (p<0.01) independent of corticoid therapy (see Tables 3, 4). Our findings indicate a reduction of the DXR parameter with increasing severity of the rheumatoid arthritis.
However, only trabecular pQCT-BMD was significantly reduced, from 121.44 g/cm3±28.38 (grade 1) to 104.79 g/cm3±28.22 (grade 3) in all patients. The relative reduction of trabecular pQCT-BMD was 13.7% for all patients, accentuated in the group with corticoid therapy (see Table 4). Regarding pQCT-BMD (total and cortical) no significant correlation was obtained regarding severity of RA (Tables 2, 3, 4). In this context, cortical and total pQCT-BMD revealed a moderate reduction of BMD between grades 1 and 2, but astonishingly-higher BMD values could be verified from grade 2 to 3.
Discussion
In recent years, interest has increasingly grown regarding the differentiation between periarticular and generalised reduction of bone mineral density in patients suffering from RA. Some studies have verified the coexistence of periarticular (i.e. juxta-articular or appendicular) and systemic bone loss. Periarticular osteoporosis has been shown to have a close association to level of disease activity, but not to disease duration, even indicating a maximal demineralisation in early RA [29, 30]. Because of a frequent and severe involvement of metacarpal joints in the rheumatoid inflammatory process, Alenfeld et al. [31] observed a higher degree of bone loss in the subregions of phalanges and metacarpals in comparison with whole-hand BMD decrease. Kalla et al. [32] verified a significant reducing effect on metacarpal osteopenia in patients with antirheumatic therapy (SAARD), and emphasised that quantification of metacarpal bone mass could be a more useful criteria of early radiological changes in RA than erosions or joint space narrowing. The inflammatory process causes periarticular and systemic bone loss by various cytokine- and hormone-mediated mechanisms [33], particularly with respect to the imbalance between OPG and RANKL in patients with RA [8].
Against the background of these data, our retrospective study has demonstrated marked reductions in periarticular bone mass, depending on the severity of RA, using digital radiogrammetry (see Tables 2, 3, 4). Similiar findings have been published regarding an association of BMD loss and progression in radiological scores [34, 35]. In one of our own recent studies [36] we found comparable results concerning severity-dependent DXR-BMD reduction for another group of patients at different stages of RA, and could find no significantly reduced BMD as measured by DXA on the total femur and lumbar spine. In addition, this study demonstrated that DXR-BMD correlated significantly with DXA-BMD of the total femur and the lumbar spine, but a greater severity-dependent reduction in periarticular DXR-BMD was observed.
DXR is ideal for quantification of periarticular BMD-reduction without an influence of soft tissue (as documented in DXA), because this method utilises the metacarpals as the location of the osteogeometric estimation. The earliest and most extensive inflammatory activity occurs here in RA. The influence of disease-related bony defects and erosions on the DXR calculations can be minimised because of DXR calculations on the diaphyseal part of the metacarpal bones.
In addition the short-term precision of DXR with CV-values less than 0.65% (Version 1.0) and less than 0.25% (Version 2.0) is at a very low level [28], indicating that estimated bone loss is in fact disease-related and not based on the precision error of the technique itself. It should be mentioned that in our study it is not problematic for DXR to determine the contour of the metacarpal shaft during the procedure of ROI positioning, and also the operator dependency of the BMD calculation—as is generally known for DXA measurements—is irrelevant for DXR.
The limitation of DXR may be the estimation of only the cortical partition of BMD. Otherwise cortical thinning of periarticular bone, supported by the inflammation process, is a typical phenomenon of bone destruction in rheumatoid arthritis [22, 32], which can be assumed because of very high bone turnover on the inner bone surface [37]. It is well known that osteoporosis in postmenopausal women is characterised by both the reduction of cortical thickness and a decrease of trabecular bone volume [38]. Recently Dreher et al. [39] documented in a histopathological study that cortical and subchondral destruction is a common feature in early RA, whereas the origin of cortical destruction is not only the affected synovial tissue but also the inflammatorily-involved trabecular bone.
The findings in the studies of Jergas [37] and Dreher et al. [39] can explain the fact that the degree of reduction for MCI (−17.8, −15.8, and −17.4% respectively) is higher in comparison to the significant decrease of DXR-BMD (−14.3, −13.3, and −11.1% respectively) independent of corticoid therapy and especially documented in grades 1 and 2. Therefore, MCI seems to be an important diagnostic parameter in early RA, in addition to its osteogeometric value.
Our study compared DXR with pQCT, which measures BMD near the affected joints of the hand and can distinguish between cortical and trabecular bone.
However, the moderate correlations between the DXR and pQCT parameters for all patients, as well as for the cortisone group and for patients without cortic acid intake, are not surprising when compared to the results of Heilmann et al. [40], who compared five different BMD utensils (three DXA devices versus pQCT and SPA) on the distal radius in healthy young individuals. The coefficients of correlation between the five techniques show a nonhomogeneous result (0.31<R<0.97), depending on the measurement site as well as the osteodensitometric technique and the different devices used [40].
The pQCT calculations were at times problematic due to normal anatomical landmarks being distorted in patients with severe RA; in contrast to DXR, an accurate positioning of the pQCT-scanner is hindered [41]. Also the cortical pQCT-BMD measurement can be influenced by additional calcifications characteristic to secondary arthrosis and ankylosis in the measurement range for severe RA, which might be considered a limitation for using pQCT on patients with severe RA; our data demonstrate a consecutive increase of cortical and total pQCT-BMD from grade 2 to 3, whereas a significant reduction of trabecular pQCT-BMD and a moderate decrease of cortical pQCT-BMD (between grades 1 and 2) is verified. These results are consistent with previous studies examining radial trabecular bone reduction of up to 25% in patients with RA using pQCT [41, 42]; the rapid trabecular bone reduction measured by pQCT occurred early in the disease process with subsequent slowing [43], whereas—similarly to our study—no significant reduction of cortical bone via pQCT could be documented.
Furthermore, our results show lower correlation coefficients in the case of corticoid application (see Table 1) between DXR parameters and trabecular pQCT-BMD.
These findings are based on the common corticoid-related systemic bone loss of the radius [44], but DXR calculates predominantly the cortical bone partition of the metacarpals and therefore cannot detect and quantify the corticoid-induced trabecular reduction of BMD.
Here it should be noted that trabecular demineralisation can be enhanced by corticoid therapy; as the trabecular component is more metabolically active, it is more responsive to such medicamentous stimuli [45, 46]. Indeed our findings indicate that steroids are able to stabilise cortical destruction and cortical bone loss, because our results reveal poor associations between DXR parameters and cortical pQCT-BMD in patients without corticoid therapy (R=0.20 vs 0.40; see Table 1). In the case of systemic corticoid application (5 mg/day over a half year period) the association between cortical pQCT-BMD and DXR-BMD versus MCI presents a significant refinement (R=0.43 vs 0.71).
The influence of steroids on bone metabolism in RA remains a cause for concern. Recent studies indicate that the stabilising function of steroids is caused by anti-inflammatory effects and potential regarding bone remodelling [47]. In addition, the decrease of inflammation induced pain during corticoid therapy may increase the individual physical activity, and consequently prevent osteoporosis. In this context, our study reveals a minor reduction of trabecular pQCT-BMD in patients with corticoid therapy compared to the group without corticoid application (see Tables 3, 4).
Other studies have described that treatment with steroids reduces the rate of irreversible joint destruction, and delays the development of appendicular osteopenia, at the expense of a significant systemic bone loss [34, 48]. Cortical bone mineral density reveals only limited alteration under the influence of indirect or non-disease-related affecting factors, and consecutively represents the more RA-specific bone partition in the BMD calculations and bone structure analyses. It is commonly known that hormone effects, age and steroids have only a small influence with respect to alterations of cortical bone tissue [49]. Therefore, osteogeometric estimation of the cortical bone by DXR might provide a reliable quantification of periarticular BMD reduction induced by RA [50, 51].
Conclusion
As DXR is able to quantify disease-related demineralisation and reduction of cortical thickness independent from corticoid intake and also in a longitudinal study [50], the clinical use of digital radiogrammetry on patients suffering from rheumatoid arthritis seems to hold significant benefits [50–52]. Possible applications and clinical importance of DXR might include a BMD calculation in routinely performed follow-up radiographs for distinguishing the side effects of anti-rheumatic medicamentous therapy from the disease-related periarticular osteoporosis. In particular, the metacarpal index can detect the disease-related impairment of cortical thickness and can potentially also quantify the stabilising effect of steroids on cortical bone tissue in early RA. Therefore, DXR could be an important diagnostic tool in early rheumatoid arthritis, which is often characterised by periarticular osteoporosis in the absence of erosions or joint-space narrowing. Further prospective studies are necessary, which should focus on the quantitative and qualitative influence of anti-rheumatic therapy as documented by DXR estimations of BMD and MCI and also should consider both the reduced muscular strength and the limited physical activity in patients with RA.
References
Papadopoulos IA, Katsimbri P, Katsaraki A, Temekonidis T, Georgiadis A, Drosos AA (2001) Clinical course and outcome of early rheumatoid arthritis. Rheumatol Int 20:205–210
Blair WF (1996) An approach to complex rheumatoid arthritis hand and wrist problems. Hand Clin 12:615–628
Dequeker J, Geusens P (1990) Osteoporosis and arthritis. Ann Rheum Dis 49:276–280
Dequeker J, Maenaut K, Verwilghen J, Westhovens R (1995) Osteoporosis in rheumatoid arthritis. Clin Exp Rheumatol 13 (Suppl 12):21–26
Sambrook PN (2000) The skeleton in rheumatoid arthritis: common mechanism for bone erosion and osteoporosis? J Rheumatol 27:2541–2542
Dolan AL, Moniz C, Abraha H, Pitt P (2002) Does active treatment of rheumatoid arthritis limit disease-associated bone loss?. Rheumatology 41:1047–1051
Goldring SR (2003) Pathogenesis of bone and cartilage destruction in rheumatoid arthritis. Rheumatology 42:11–16
Hofbauer LC, Heufelder AE (2001) Role of receptor activator of nuclear factor-κB ligand and osteoprotegerin in bone cell biology. J Mol Med 79:243–253
Gough AK, Lilley J, Eyre S, Holder RL, Emery P (1994) Generalized bone loss in patients with early rheumatoid arthritis. Lancet 344:23–27
Lee YH, Rho YH, Choi SJ, Ji JD, Song GG (2003) Predictors of bone mineral density and osteoporosis in patients attending a rheumatology outpatient clinic. Rheumatol Int 23:67–69
Cetin A, Ertürk H, Celiker R, Sivri A, Hascelik Z (2001) The role of quantitative ultrasound in predicting osteoporosis defined by dual X-ray absorptiometry. Rheumatol Int 20:55–59
Celiker R, Gokce-Kutsal Y, Cindas A, Ariyurek M, Renda N, Koray Z, Basgoze O (1995) Osteoporosis in rheumatoid arthritis: effect of disease activity. Clin Rheumatol 14:429–433
Cooper C, Atkinson EJ, Jacobsen SJ, O’Fallon WM, Melton LJ (1993) Population-based study of survival after osteoporotic fractures. Am J Epidemiol 137:1001–1005
Peris P (2002) Stress fractures in rheumatological practice: clinical significance and localizations. Rheumatol Int 22:77–79
Berglin E, Lorentzon R, Nordmark L, Nilsson-Sojka B, Rantapaa Dahlqvist S (2003) Predictors of radiological progression and changes in hand bone density in early rheumatoid arthritis. Rheumatology 42(2):268–275
Larsen A, Thoen J (1987) Hand radiography of 200 patients with rheumatoid arthritis repeated after an interval of one year. Scand J Rheumatol 16:395–401
Brower AC (1990) Use of the radiograph to measure the course of rheumatoid arthritis. The gold standard versus fool’s gold. Arthritis Rheum 33:316–324
Cortet B, Flipo RM, Duquesnoy B, Delcambre B (1995) Bone tissue in rheumatoid arthritis. Bone mineral density and fracture risk. Rev Rheum Engl Ed 62:197–204
Kalla AA, Meyers OL, Laubscher R (1995) Prevalence of metacarpal osteopenia in young rheumatoid arthritis patients. Clin Rheumatol 14:617–625
Jergas M, Uffmann M, Escher H, Gluer CC, Young KC, Grampp S, Koster O, Genant HK (1994) Interobserver variation in the detection of osteopenia by radiography and comparison with dual X-ray absorptiometry (DXA) of the lumbar spine. Skeletal Radiol 23:195–199
Barnett E, Nordin B (1960) The radiological diagnosis of osteoporosis: a new approach. Clin Radiol 11:166–174
Kalla AA, Meyers OL, Parkyn ND, Kotze TJ (1989) Osteoporosis screening—radiogrammetry revisited. Br J Rheumatol 28:511–517
Rosholm A, Hyldstrup L, Baeksgaard L, Grunkin M, Thodberg HH (2001) Estimation of bone mineral density by digital X-ray radiogrammetry: theoretical background and clinical testing. Osteoporos Int 12:961–969
Cardenas JL, Revilla M, Hernandez ER, Aguado F, Villa LF, Rico H (1997) Comparison of three bone densitometry methods in osteoporotic women. Osteoporos Int 61:358–361
Martin JC, Reid DM (1999) Radial bone mineral density and estimated rates of change in normal Scottish women: assessment by peripheral quantitative computed tomography. Osteoporos Int 64:126–132
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fies FJ, Cooper NS (1988) The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 31:315–324
Rau R, Wassenberg S, Herborn G, Stucki G, Gebler A (1998) A new method of scoring radiographic change in rheumatoid arthritis. J Rheumatol 25:2094–2107
Black DM, Palermo L, Sorensen T, Jorgensen JT, Lewis C, Tylavsky F, Wallace R, Harris E, Cummings SR (2001) A normative reference database study for Pronosco X-posure SystemTM. J Clin Densitom 4:5–12
Deodhar AA, Brabyn J, Jones PW, Davis MJ, Woolf AD (1995) Longitudinal study of hand bone densitometry in rheumatoid arthritis. Arthritis Rheum 38:1204–1210
Devlin J, Lilley J, Gough A, Huissoon A, Holder R, Reece R, Perkins P, Emery P (1996) Clinical associations of dual-energy X-ray absorptiometry measurement of hand bone mass in rheumatoid arthritis. Br J Rheumatol 35:1256–1262
Alenfeld FE, Diessel E, Brezger M, Sieper J, Felsenberg D, Braun J (2000) Detailed analyses of periarticular osteoporosis in rheumatoid arthritis. Osteoporos Int 11:400–407
Kalla AA, Meyers OL, Chalton D, Heath S, Brown GM, Smith PR, Burger MC (1991) Increased metacarpal bone mass following 18 months of slow-acting antirheumatic drugs for rheumatoid arthritis. Br J Rheumatol 30:91–100
Oelzner P, Hein G (1997) Inflammation and bone metabolism in rheumatoid arthritis. Pathogenetic viewpoints and therapeutic possibilities. Med Klin 92:607–614
Hansen M, P?denphant J, Florescu A, Stoltenberg M, Borch A, Kluger E, Sorensen SF, Hansen TM (1999) A randomised trial of differentiated prednisolone treatment in active rheumatoid arthritis. Clinical benefits and skeletal side effects. Ann Rheum Dis 58:713–718
Chan E, Pandith V, Towheed TE, Brouillard D, Zee B, Anastassiacles TP (1998) Comparison of the combined cortical thickness of the second metacarpal with Sharp’s method for scoring hand microradiographs in rheumatoid arthritis. J Rheumatol 25:1290–1294
Böttcher J, Malich A, Pfeil A, Petrovitch A, Lehmann G, Heyne JP, Hein G, Kaiser WA (2004) Potential clinical relevance of digital radiogrammetry for quantification of periarticular bone demineralization in patients suffering from rheumatoid arthritis depending on severity and compared with DXA. Eur Radiol 14:631–637
Jergas M (2003) Conventional radiographs and basic quantitative methods. In: Grampp S (ed) Radiology of osteoporosis. Springer, Berlin Heidelberg New York , pp 62–64
Barger-Lux MJ, Recker RR (2002) Bone microstructure in osteoporosis: transilial biopsy and histomorphometry. Top Magn Reson Imaging 13:297–305
Dreher R, Thabe H, Schill S, Schulz A (2003) Die Rheumatoide Arthritis aus osteologischer Sicht. Osteologie 11 (Suppl 1):52
Heilmann P, Wüster C, Prolingheuer C, Gotz M, Ziegler R (1998) Measurement of forearm bone mineral density: comparison of five different instruments. Calcif Tissue Int 62:383–387
Martin JC, Munro R, Campbell MK, Reid DM (1997) Effects of disease and corticosteroids on appendicular bone mass in postmenopausal women with rheumatoid arthritis: comparison with axial measurements. Br J Rheumatol 36:43–49
Sambrook PN, Ansell BM, Foster S, Gumpel JM, Hesp R, Reeve J (1985) Bone turnover in early rheumatoid arthritis. 2. Longitudinal bone density studies. Ann Rheum Dis 44:580–584
Sambrook PN, Shawe D, Hesp R, Zanelli JM, Mitchell R, Katz D, Gumpel JM, Ansell BM, Reeve J (1990) Rapid periarticular bone loss in rheumatoid arthritis.Possible promotion by normal circulating concentrations of parathyroid hormone or calcitriol (1,25-dihydroxyvitamin D3). Arthritis Rheum 33:615–622
Kalla AA, Bewerunge L, Langley A, Meyers OL, Fataar AB (2002) Trabecular bone density in premenopausal rheumatoid arthritis patients. S Afr Med J 92:62–68
Verhoeven AC, Boers M, te Koppele JM, van der Laan WH, Markusse HM, Geusens P, van der Linden S (2001) Bone turnover, joint damage and bone mineral density in early rheumatoid arthritis with combination therapy including high-dose prednisolone. Rheumatology 40:1231–1237
Trapani S, Civinini R, Ermini M, Paci E, Falcini F (1998) Osteoporosis in juvenile systemic lupus erythematosus: a longitundinal study on the effect of steroids on bone mineral density. Rheumatol Int 18:45–49
Jensen T, Klarlund M, Hansen M et al (2004) Bone loss in unclassified polyarthritis and early rheumatoid arthritis is better detected by digital radiogrammetry than dual X-ray absorptiometry: relationship with disease activity and radiographic outcome. Ann Rheum Dis 63:15–22
Kirwan JR (1995) The effect of glucocorticoids on joint destruction in rheumatoid arthritis. The Arthritis and Rheumatism Council Low-Dose Glucocorticoid Study Group. N Engl J Med 333:142–146
Sambrook PN, Eisman JA, Yeates MG, Pocock NA, Eberl S, Champion GD (1986) Osteoporosis in rheumatoid arthritis: safety of low dose corticosteroids. Ann Rheum Dis 45:950–953
Stewart A, Mackenzie LM, Black AJ, Reid DM (2004) Predicting erosive disease in rheumatoid arthritis. A longitudinal study of changes in bone density using digital X-ray radiogrammetry: a pilot study. Rheumatology 24 (online publication ahead of print)
Haugeberg G, Lodder MC, Lems WF, Uhlig T, Orstavik RE, Dijkmans BA, Kvien TK, Woolf AD (2004) Hand cortical bone mass and its associations with radiographic joint damage and fractures in 50–70 year-old female patients with rheumatoid arthritis: cross sectional Oslo-Truro-Amsterdam (OSTRA) collaborative study. Ann Rheum Dis 63:1331–1334
Ward KA, Cotton J, Adams JE (2003) A technical and clinical evaluation of digital X-ray radiogrammetry. Osteoporos Int 14:389–395
Acknowledgements
We would like to thank Pronosco-Sectra (Mr. A. Rosholm, PhD) and Arewus (Mrs. M. Arens) for the X-posure equipment. Finally the authors would also like to thank Mr. D. Felsenberg, PhD (Berlin, Germany), Mr. C.C. Gluer, PhD (Kiel, Germany), Mr. R. Rau, PhD (Ratingen, Germany), Mr. S. Grampp, PhD and Mr. H. Imhof, PhD (Wien, Austria) for their comments regarding our study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Böttcher, J., Pfeil, A., Heinrich, B. et al. Digital radiogrammetry as a new diagnostic tool for estimation of disease-related osteoporosis in rheumatoid arthritis compared with pQCT. Rheumatol Int 25, 457–464 (2005). https://doi.org/10.1007/s00296-004-0560-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-004-0560-z