Abstract
Poor immune recovery is characteristic of bone marrow transplantation and leads to high levels of morbidity and mortality. The primary underlying cause is a compromised thymic function, resulting from age-induced atrophy and further compounded by the damaging effects of cytoablative conditioning regimes on thymic epithelial cells (TEC). Several strategies have been proposed to enhance T cell reconstitution. Some, such as the use of single biological agents, are currently being tested in clinical trials. However, a more rational approach to immune restoration will be to leverage the evolving repertoire of new technologies. Specifically, the combined targeting of TEC, thymocytes and peripheral T cells, together with the bone marrow niches, promises a more strategic clinical therapeutic platform.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fungal, viral and bacterial infections contribute significantly to patient morbidity and mortality during the prolonged immunosuppressive states that follow bone marrow transplantation (BMT) or, now more commonly, mobilised haematopoietic stem cell transplantation (HSCT). Strategies to enhance immune reconstitution have thus become an important area of clinical investigation. Robust cell-mediated immunity also provides a primary means of minimising disease relapse either directly or via cancer vaccines. T cells, particularly the CD4+ subset, are critical to these immune protective functions for reducing transplant-related morbidity and significantly improving clinical outcome in terms of overall survival, opportunistic infections and non-relapse mortality [1]. Not surprisingly, therefore, the kinetics of T cell recovery is of great significance, with the faster return of CD4+ T cell numbers correlating with better survival outcomes [2].
The cytoreductive regimes of chemotherapy and radiation therapy are, by necessity, often applied in such high levels that they evoke the need for HSCT because of the profound collateral destruction of the haematopoietic compartment. Associated damage to the thymic and bone marrow (BM) niche stromal cells can delay immune recovery because it compromises engraftment of donor haematopoietic stem cells (HSCs) and the development of all haematopoietic and lymphopoietic lineages. The age of the patient also influences the rate of haematopoietic and immune recovery [3]. More specifically and certainly paradoxically, the thymus naturally involutes with age, particularly noticeable during the early teenage years. Hence, damage by chemotherapy to an already age-induced atrophied thymus further compounds delays in immune reconstitution.
What induces the involution of the thymus and this age-correlated shift from an activated state to a atrophic milieu? Whilst the mechanisms of ageing are not well understood, implications for changes in the neuroendocrine-immune axis are suggested by either increases or losses in the production of particular hormones and growth factors. Can we utilise this knowledge to develop strategies to increase the rate of T cell recovery following HSCT? Furthermore, as the thymus relies throughout life on the continual seeding of BM derived haematopoietic precursors in order to produce T cells, any alterations in the BM that compromises the number or quality of lymphoid precursors can directly impact on thymic function and naïve T cell output. Deciphering the physiology of stem cell niches in the BM and effects thereon of age or damage from conditioning regimes thus becomes highly relevant to achieve long-term T cell reconstitution.
This review will briefly introduce thymic development, ageing and the problems associated with the damage to the BM and thymic stromal cell micro-environments by HSCT conditioning regimes. The mechanisms underlying thymic atrophy and decreased immune function with age will also be discussed, as well as how this information can be exploited to form therapeutic strategies to enhance T cell reconstitution for immune recovery.
Development and degeneration of the thymus
Understanding the processes that occur during thymic organogenesis should provide a logical basis to enabling a more focussed approach to targeting particular molecules or stem cell populations that may have potential in rejuvenating a damaged thymus for immune reconstitution. It will also be of importance to develop strategies for more complex applications, such as steering embryonic stem (ES) cells down a thymic epithelial cell (TEC) lineage.
The common thymic epithelial primordium develops from an outpocketing of the third pharyngeal pouch endoderm around embryonic day 10 in mice (E10) and is marked by the expression of Foxn1, a member of the forkhead-box family of transcription factors [4]. Foxn1 is functionally required for the differentiation and proliferation of immature TECs into cortical and medullary subsets and for subsequent thymocyte infiltration [5, 6]. Homozygous deletions in Foxn1 give rise to a nude phenotype, which is characterised by congenital athymia and results in severe immunodeficiency secondary to the absence of T cells. Although previously thought to contain ectodermal contributions, many studies have now demonstrated a sole, endodermal origin of the thymic epithelium that contributes to both functional components—cortex and medulla (see review [7]). Other transcriptional networks involved in thymic organogenesis include the Hox, Pax, Six families, the eyes absent (Eya) protein tyrosine phosphatases and T-box transcription factor TBX1 (see reviews [8, 9]).
Whilst these early stages of epithelium differentiation are thymocyte independent, they do involve essential interactions with mesenchyme that provide for example, bone morphogenic proteins which play a major role in cell signalling. The primitive thymic epithelial primordium recruits pharyngeal mesenchymal cells as it differentiates. Around E10 to E12, mesenchymal cells derived from the neural crest and mesoderm of the pharyngeal arches initially encapsulate the thymic epithelial rudiment before they migrate inwards to establish an intra-thymic network of fibroblasts [10, 11], which in turn facilitates later vascular invagination via the formation of trabeculae. The mesenchyme provides critical molecules such as fibroblast growth factor (Fgf)-7 and Fgf-10, which regulate proliferation of FgfR2IIIb-expressing epithelium [12, 13].
The avascular thymic primordium is seeded at E11 in mice and week 7–8 gestation in humans by liver-derived haematopoietic progenitors [14, 15]. Once the thymus is vascularised later in gestation, the haematopoietic component is continually replenished by circulating BM-derived lymphoid progenitors migrating into the thymus at the corticomedullary junction. Upon entering, the lymphoid progenitors closely interact with specialised thymic stromal cells, which supply growth factors and other signalling molecules important for the in situ T lineage commitment, migration, development and selection of haematopoietic cells. In turn, the committed T cell precursors supply the signals for the maturation and differentiation of TECs in a continual interplay known as thymic ‘crosstalk’ [16].
The ageing thymus
The thymus involutes with age, a process that becomes apparent as early as the first year of life in humans and is most pronounced in puberty. By 25 years of age, the thymus has decreased to approximately 50% of its size at birth and to 10% by mid-life (50 years) [17]. Parallel with these changes, there is not only a decline in the frequency of early T lineage progenitors (ETP) but their differentiation capacity is also diminished [18]. Functional thympoietic tissue is replaced over time by peri-vascular spaces and adipose tissue, which disrupt the thymic architecture [19]. A gradual loss in the production and export of thymus-derived naïve T cells results. Homeostatic mechanisms subsequently counteract this loss by expanding the existing peripheral T cell pool (Fig. 1). As a consequence, an increase in the ratio of memory to naïve T cells and a decrease in the CD4 to CD8 T cell subset ratio develops, leading to an increased susceptibility to microbial and viral infections. Furthermore, the resultant T cell receptor (TcR) repertoire is more limited and has hence a reduced capacity to recognise and respond to new antigens when compared to that of younger individuals. Paralleling the reduced output of thymus-derived naïve T cells with age, the remaining naive peripheral TcR repertoire becomes even further skewed due to progressive contact with environmental pathogens, further limiting the capacity to mount an effective immune response to new infections. Mortality rates are often two to three times higher in older patients due to infections; somewhat paradoxically, there is an increased prevalence of auto-immune diseases probably due to a loss of Treg cells or breakdown in thymus-based central tolerance, or both [20].
Impacts of age and regeneration by sex steroid ablation on lymphopoiesis and peripheral lymphocytes. a Lymphopoiesis in the BM and thymus progresses through developmental steps that result in the formation of mature B and T cells for export. This leads to a combination of naïve and memory cells in the periphery ready to ward off infection. b With age, there is an increase in HSCs—particularly in CD34− Flt3− LT-HSC and a corresponding decrease in CD34+ Flt3+ MPP. In the BM, this leads to a reduction in the number and function of LCP and subsequent decline in B-lymphopoiesis. In the thymus, there is a decline in the differentiation capacity of ETP and architectural disruption leading to a reduced output of naïve T cells, intrinsically altering the function of the thymus with age. These changes in BM and thymic lymphopoiesis lead to a reduction in the peripheral B and T cell receptor repertoires, thereby reducing the ability to fight new infections and impairing immune recovery following immunodepletion. The decrease in export of naïve lymphocytes from the BM and thymus results in a clonal expansion of pre-existing memory cells. Many of these processes in lymphoid degeneration with age have been associated with the negative regulation of sex steroids on the micro-environment; however, they have also been shown to directly impact on the earliest lymphoid progenitors in the BM. c Removal of sex steroids, by either chemical or surgical means, has been shown to regenerate thymic and BM function to levels observed in the young. LT-HSC Long-term repopulation HSCs, MPP multi-potent progenitors, LCP lymphoid committed progenitors, ETP early T cell progenitors
A number of cytokines, chemokines and growth factors produced by the thymus have been found to alter with age (Table 1). Some of these have been implicated in age-induced thymic atrophy, such as the reduction in growth hormone (GH) and its mediator insulin-like growth factor-1 (IGF-1; see review [21]) and increases in oncostatin M, stem cell factor, interleukin (IL)-6 and leukaemia inhibitory factor [22]. TGFβ has also been suggested to play a suppressive role with quantitative genetic variation in thymic involution being associated with variable levels of TGFβ2 production [23]. Hauri-Hohl et al. further showed that the specific deletion of TGFβRII in TECs led to reduced thymic atrophy with age [24], supporting a contributing role of TGFβ in thymic involution. These changes in levels of soluble mediators may be cell intrinsic but they are also likely to be due to shifts in the status of the relevant stromal cell sub-type producing them—not all components of the thymic micro-environment age equally.
It is not clear whether the overall loss of thymic tissue results from an intrinsic ageing defect in epithelial stem cells such as poor self-renewal and thus a gradual loss in cellularity or that an ageing micro-environment can no longer fully sustain efficient thymopoiesis. Whilst a more precise understanding of this ageing process is yet to be elucidated, the success of any long-term T cell reconstitution strategies will need to address the age and integrity of the thymic micro-environment.
Cytoreductive cancer treatment regimes affect thymic stromal cells
High-dose BMT conditioning regimes, such as chemotherapy and radiation, result in the severe depletion of virtually all haematopoietic and immune system cells. Both alkylating chemotherapeutics and irradiation target highly proliferative cells [65–67], including developing and naïve lymphocytes [68]. Immune recovery, particularly of the fundamentally important naïve CD4+ T cells, is critically dependent on the functional status of the two primary lymphoid organs—the thymus and bone marrow. However, the overall cellularity of the thymic stromal cell population and architectural organisation of the micro-environment are affected by the damaging conditioning regimes (Goldberg, submitted manuscript). As a consequence, the restoration of heterogeneous T cell populations and re-establishment of immune competence is often slow and incomplete. Of particular importance is a recently discovered major loss in major histocompatibility complex (MHC) class II high expressing medullary epithelial cells (mTEChi) following cyclophosphamide treatment (Fletcher, submitted manuscript). These cells express the auto-immune regulator (Aire) gene which regulates the expression of peripheral self-antigens in the thymus (see review [70]). In young mice, the population of mTEC that express high amounts of Aire (designated mTEChi) recovers within 10 days after cessation of treatment, alongside development of CD4+ and CD8+ thymocytes. Depending on the level of contact required with these specialised mTECs for tolerance induction, developing auto-reactive thymocytes may escape negative selection, leading to a pre-disposition to auto-immunity. Immunosuppressive treatments such as cyclosporine A have also been found to reduce thymic Aire expression due to the damaging effects on mTEChi cells. This may well explain the associated increase in clinical susceptibility to some auto-immune diseases following CsA treatment [71]. Thymic damage can also inhibit the development and function of T regulatory cells (Tregs), inducing another tier in compromised tolerance [72]. Graft versus host disease (GvHD) in the allogeneic HSC transplant setting can further diminish thymic mass [69]. How quickly and completely the atrophied aged thymus can regenerate after further treatment-related damage, particularly this specialised mTEC subset, is currently under investigation and will be important in re-assessing conditioning protocols.
A number of thymic cytokines, chemokines and growth factors are altered after chemotherapy and irradiation (Table 2). Depending on the time point analysed post-treatment, these will include direct changes due to the damaging effects on the stromal cells, as well as changes induced by the lymphopenic state and therefore form part of the recovery process. For instance, in young mice following immune depletion, there is an up-regulation in growth factors and chemokines such as IL-7, stromal derived factor-1 alpha (SDF1α; CXCL12), thymus-expressed chemokine (TECK; CCL25) and secondary lymphoid tissue chemokine (SLC; CCL21) [49]. How effectively the stromal micro-environment recovers in the aged setting after damage, however, will be more clinically relevant. Indeed, adults, whose thymi have involuted, are significantly impaired in their ability to recover immune capacity following chemotherapy, compared to children [3, 73, 74]. Whilst CD8+ T cell recovery in both young and aged patients is quite rapid [75], they are predominantly derived extra-thymically by clonal expansion [76]. Although delayed, substantial immune recovery is possible up until middle-age, however, in older patients, the peripheral naïve T cell receptor repertoire is never fully restored [77].
The recovery of B cells and NK cells is also severely impaired in aged compared to young patients [77]. Furthermore, much like the TcR repertoire, the B cell repertoire is severely diminished after chemotherapy and suffers a prolonged recovery [78]. Quiescent HSCs are largely numerically spared from many chemotherapeutic and low-dose radiation regimes [79]; however, their haematopoietic function appears to be significantly impaired [80, 81]. Importantly, this was also shown with human CD34+ HSCs [82] suggesting that the standard clinical practice of collecting autologous HSCs from patients in remission, often after prolonged chemotherapy treatment, may lead to poorer transplant outcomes. Furthermore, radiation or chemotherapy was shown to cause enhanced senescence in HSCs that was coupled with an up-regulation in p19Arf and p16ink4A [81, 83], mimicking some of the effects seen with age.
The BM niche and development of T cell precursors
Maintaining the integrity of the BM niche is critical for the survival and continued production of HSCs throughout life. This minimises undesired differentiation cues and apoptotic stimuli and promotes the homeostatic differentiation into circulating blood and immune cells that include lymphocytes and myeloid cells. In this regard, the BM has direct relevance to the thymus in the quality and quantity of T cell precursors available for thymic uptake and T cell development. Whilst the mechanisms involved in HSC survival, renewal, differentiation and migration have been well studied, the complex BM stromal environments adjacent to the endosteum or within the central more vascularised regions are not precisely understood. A critical study by Nilsson et al. found that transplanted carboxyfluorescein succinimidyl ester labelled LT-HSCs lodge and engraft in the endosteal region, whilst more committed HSCs lodge in the vascular niche, indicating a quiescent stem cell niche at the endosteal surface [105, 106]. However, using the signalling lymphocyte attractant molecule markers for identification of HSCs in steady-state BM, Kiel et al. found that whilst there was localisation of LT-HSCs in the endosteum, there was also significant association with sinusoidal (vascular) endothelium in the BM [107]. Taken together, these studies suggest that there are at least two stem cell niches in the BM—the endosteal and sinusoidal niches. However, these are not necessarily distinct; secreted factors may diffuse into adjacent niches (see review [108]) and so the HSC ‘niche’ could be a continuum between these regions. Within these niches, two major types of stromal cells—bone forming osteoblasts and CXCL12 abundant reticular (CAR) cells, have been identified as playing critical roles in maintaining HSC quiescence, self-renewal, adhesion and differentiation. Osteoblastic cells are located at the endosteal surface and are an essential regulatory component of the HSC niche [109–111]. They produce proteins that not only can both inhibit and stimulate HSC proliferation and therefore exquisitely regulate their fate but also can effect HSC homing, trans-marrow migration and engraftment. Osteopontin, produced by osteoblasts, acts to negatively regulate HSC activity by maintaining stem cell quiescence [112, 113]. Alterations in its production can lead to an imbalance in self-renewal and inadequately regulated activation of stem cells [109–111]. Bone formation and re-modelling can also play a role in regulating the endosteal niche. The dynamic equilibrium between bone-forming osteoblasts and bone resorbing osteoclasts can influence the regulation of haematopoietic progenitors near the endosteum (see review [108]). The reticular (CAR) stromal cells and endothelial cells produce growth factors for differentiation and proliferation such as IL-7 and chemokines such as CXCL12—important for stem cell homing (see review [114]). These detailed studies regarding the micro-environmental interactions with developing HSCs reveal a complex scenario that is still evolving.
Declining bone marrow function with age
As for the thymus, age-related changes in the BM can directly impact on HSC maintenance, proliferation and differentiation. Donor HSC trans-marrow migration and attachment to the stem cell niche following transplant is also reduced. Not surprisingly, a loss in osteoblasts can result in a direct reduction in HSC production (see review [115]). Increased infiltration of adipocytes associated with age can also lead to a dysregulated cytokine and growth factor milieu, impacting upon HSC production, survival and differentiation. A number of age-related alterations have been proposed, such as reduced adhesion of HSC and progenitor cells to the stroma [116], attenuation of the homing and engraftment potential of aged HSCs [117], decreased responsiveness to IL-7 [118] and skewing in lineage differentiation away from lymphoid cells [119]. However, the full impact of age-induced alterations on HSC number and function [120] and overall immunosenescence remains to be elucidated. Nevertheless, BM ageing appears to occur at both an intrinsic level in HSCs as well as extrinsic alterations in the HSC niche (see review [115, 121]). Hence, ideally, regeneration of both the BM and thymus environments should be considered in long-term immune reconstitution strategies.
Restoration of bone marrow niche and function
Regeneration of the BM niche would obviously have particular relevance following the damaging cytoablative conditioning regimes of HSC transplantation. Treatment with human parathyroid hormone (PTH) stimulates osteoblast cells leading to enlargement of the HSC pool, protection from chemotherapy and enhanced engraftment following BMT. Collectively, this offers significant therapeutic potential [115]. Another strategy has been to co-transplant donor BM cells of non-haematopoietic origin, including stromal cells and osteoblast progenitors, together with the HSC into non-ablated hosts. This has led to improved HSC engraftment, possibly by increasing the number of competent osteoblasts lining the endosteum [122, 123]. Another BM stromal cell population gaining importance in regenerative medicine is the mesenchymal stem cell (MSC). These cells have the important property of being naturally immunosuppressive and have been shown to successfully diminish graft versus host disease in cancer patients receiving an allogeneic HSC transplant [124]. They also prolong the acceptance of allografts [125] and, importantly, may facilitate the induction of mixed donor–host HSC chimerism (see review [126]). However, whether sustained engraftment potential can be achieved in the clinical setting, particularly in the aged or damaged BM niche, is a current point of contention.
Strategies for thymic regeneration post-HSCT
Can we apply our knowledge of the mechanisms leading to thymic involution, to reverse the aging process and to induce thymic regeneration? Several theories have been proposed for thymic atrophy. These include reduced production of important growth factors such as IL-7 and GH, increase in atrophic factors such as the TGFβ family of cytokines and reduced levels of chemokines or adhesion molecules that attract and facilitate entry of precursors into the thymus. Changes in the neuroendocrine-immune axis have evolved as a likely trigger to promote thymopoiesis, but it will most likely be a multi-faceted process involving both BM-derived haematopoietic progenitors and the thymic stromal cell niches that convert them to T cells.
Targeting endocrine influences
Sex steroid ablation therapy
It is well established that immune cells are inhibited by adrenal and gonadal steroids and an increased rate of thymic atrophy has been associated with the onset of sexual maturation (see review [127]). Hence, endocrine-based strategies were developed in animal models in an attempt to regenerate the ageing, atrophied thymus. The results were dramatic. Sex steroid ablation (SSA) resulted in a rapid (within 2 weeks) reversal of this degenerative state. Castrate levels of sex steroids can be achieved via surgical removal of the gonads or bio-chemically by using a luteinising hormone-releasing hormone analogue (LHRH-A) which is reversible and, as such, more clinically applicable. LHRH-A has been widely used in the clinic to treat endocrine-related disorders such as endometriosis [128], prostate cancer [129], precocious puberty [130] and breast cancer [131]. Pre-treatment with LHRH-A has also been used to protect against high-dose chemotherapy-induced sterility in females undergoing HSCT [132].
Both surgical and chemical SSA effect a delayed onset of thymic atrophy in young mice—and its reversal in the aged—in both male and female rodents, albeit to a lesser extent in females [133–139]. Morphologically, SSA rejuvenated the atrophic thymic micro-environment of aged mice, including reappearance of well-defined corticomedullary boundaries and decreased peri-vascular spaces, to similar levels observed in the thymus of young mice [140, 141]. Functionally, SSA restored defective thymopoiesis and enhanced export of naïve T cells, leading to an expanded TcR Vβ repertoire and augmented function of the peripheral T cell pool [141, 142] (Fig. 1).
In pre-clinical models of lymphopenia induced by anti-neoplastic therapy such as cyclophosphamide, SSA restored T cell-mediated immunity [142, 143]. Within the thymus, SSA increased the recovery of all thymocyte and TEC populations ([143]; Goldberg, submitted manuscript). Importantly, SSA enhanced restoration of the Aire expressing mTEChi population, compared to sham-treated control animals (Goldberg, submitted manuscript), which would facilitate the appropriate negative selection of re-emerging thymocyte populations [144, 145]. Furthermore, in studies of HSCT, SSA led to enhanced cellular recovery of both the thymus and BM following immunoablative conditioning in animal models of autologous and allogeneic BMT [146, 147]. In addition, SSA therapy increased both engraftment and function of donor T cells post-allogeneic transplant and did not exacerbate GVHD [146].
In line with the murine data, we found SSA induced increases in naïve T cell output; however, the recovery in humans was much slower due to the obvious physiological differences between mouse and human and the impact of aging on the thymus. In a cohort of elderly patients (>60 years) receiving routine LHRH-A therapy for the treatment of prostate cancer, thymic regeneration was apparent with increased numbers of TcR excision circles (TREC) in T cells observed by 4 months after onset of the drug. This indicates some efficacy of SSA to improve human thymic function [141]. It was also associated with an increase in T cell infiltration of the prostate gland, adding another dimension to the positive impact of SSA on prostate cancer patients. These data collectively contributed to the development of a protocol for a pilot phase II clinical trial for LHRH-A therapy in patients with haematologic malignancies (acute leukemia, chronic leukemia, lymphoma, multiple myeloma) or non-malignancies (myelodysplasia, aplastic anemia) undergoing BMT/HSCT [148]. A total of 80 male and female patients (40 LHRH-A treated, 40 control, non-randomised) ranging in age from 17–69 years were given LHRH-A over 4 months starting treatment 3 weeks prior to transplant such that sex steroids would be at castrate levels at the time of transplant. Despite the fact that being an agonistic LHRH variant, which causes a profound initial surge in sex steroid production over the first 7–10 days, within the first month of treatment LHRH-A treated patients showed increased neutrophil levels and decreased time taken to engraft. Most significantly, LHRH-A treated patients demonstrated enhanced recovery of naïve CD4+ T cells from 5–6 months, confirmed by increased TRECs and increased TcR diversity [148]. These patients also showed a significant increase in their T cell response to direct-TcR stimulation.
Despite its efficacy in restoring thymic function, the exact mechanisms underpinning sex-steroid removal remain ill defined. In mice, SSA-mediated thymic regeneration is abolished via re-administration of testosterone [134]. The target cells may include both the thymocyte and thymic stromal cell populations since both express the androgen receptor [146, 149]. Androgen administration induced thymocyte apoptosis in thymic organ culture [150], and conversely, removal of androgen resulted in increased proliferation of thymocytes both in vivo and following in vitro stimulation, indicating a direct influence on thymocyte development [143, 151, 152]. It is likely, however, that androgen removal also indirectly affects thymocyte development via modulation of the thymic stromal cell niche. Indeed, chimeric studies using AR-deficient mice have demonstrated that thymic atrophy only occurs when functional ARs are expressed by non-haematopoietic stromal cells, but not when only on thymocytes [153], indicating a fundamental role for the thymic stromal compartment in SSA-mediated thymic regeneration.
ARs are expressed on both TEC and non-TEC populations, including cortical epithelial cells, mTEC and subsets therein defined by MHCII high or low expression, as well as MTS-15+ fibroblasts ([146] and Search, unpublished observations). Whilst still speculative, it is possible that removal of the suppressive influence of sex steroids initiates functional changes within thymic stromal populations, such as increasing the production of thymopoiesis promoting chemokines and growth factors. These in turn can enhance the uptake and/or proliferation of T cell progenitors, apparent early following SSA [143, 151]. The subsequent expansion of mature thymocyte subsets may then feed back to the thymic stroma, particularly the neighbouring mTEC, increasing their proliferation and cell number via mechanisms of thymic cross talk [16]. On the other hand, LHRH itself can have a direct effect on cell types that express its receptor, such as thymocytes and splenocytes, inducing an upregulation of IL-2 receptor expression and potentially improving their proliferative capacity [154]. To enhance this potential and diminish the initial LHRH agonist-induced flare in sex steroid production, combined treatment with androgen or estrogen receptor blockers could be used in the first week of LHRH-A therapy [127]. Alternatively, LHRH antagonists could be administered to prevent the damaging initial flare in sex steroids, but they would not embrace the potential direct stimulatory capacity of LHRH on the thymus.
Initial molecular analysis of whole thymic stromal cells from SSA-treated mice revealed little change in the production of thymic growth factors or cytokines pertinent to thymopoiesis [141, 147]. More specific and sensitive analysis of defined stromal cell sub-populations, however, has indicated that removal of sex steroids may initiate molecular changes as early as 48 h post-SSA. This was reflected in the differential expression patterns of various transcription factors, cytokines, chemokines and growth factors involved in thymopoietic regulation (Chidgey, manuscript in preparation). In addition to influences on the thymic stroma, SSA also impacts upon BM function, as evidenced by increased circulating B cells and early pro-B cells in the BM [155]. Increased haematopoietic engraftment, B cell differentiation and T cell progenitor number were found following combined SSA and HSCT in mice [146]. Possible side effects of SSA treatment may include an increase in osteoporosis, however, this would not be an issue with short-term SSA therapy. SSA may thus contribute to thymic regeneration at multiple levels (Fig. 1). To this end, investigations are ongoing to assess the impact of sex steroid removal on the haematopoietic compartment of the BM and, importantly, the supporting stromal cell niches.
Growth hormone/IGF1
GH is predominantly produced by the anterior pituitary gland, but of relevance in the context of thymic function and possibly regeneration, GH is also produced by thymocytes and thymic epithelial cells [21]. Its receptor (GHR) is present on both TEC and thymocytes, suggesting that GH can function in an autocrine and paracrine fashion [156]. The decreased production with age of GH and its mediator, IGF1, has implicated GH as a contributory factor to thymic involution (reviewed in [21]). Prior studies have shown administration of GH restores thymic function in aged rodents [157] and improves immune reconstitution after allogeneic, T cell depleted, BMT [59]. However, the level and duration of thymic recovery and the effective translation from animal models to the clinic has been unclear. Napolitano et al. recently performed clinical trials on HIV-1-positive patients that were simultaneously undergoing anti-retroviral treatment and carrying a low viral load [158]. A 2-year cross-over study was performed on 22 HIV-1-positive male patients (age ranging 40–76 years in GH arm and 37–65 years in control arm) in a randomised, prospective, open-labelled study. GH-treated patients showed significant increases above baseline levels in proportion and absolute number of circulating naïve CD4+ T cells and in TRECs of unfractionated PBMCs at 6 months. Whilst this study provided encouraging results towards the potential for GH to replenish a polyclonal population of CD4+ T cells, there were major safety issues. There was the necessity for daily injections of GH and there were multiple adverse side effects such as arthralagias, abnormal glucose metabolism, edema and carpal tunnel syndrome, causing nine patients to discontinue the treatment. This is likely to hinder broad acceptance of GH as a therapy; however, the outcome from this study warrants further investigations into reducing the frequency and dose of administration. GH may also find important clinical utility as an adjuvant for other thymic regrowth strategies.
Administration of growth factors
Interleukin-7
IL-7 is a pleiotropic cytokine produced by stromal cells in the BM, thymus, gut and by keratinocytes. It is a non-redundant cytokine important for T and B cell development, promoting cell survival, differentiation and proliferation. Signalling is regulated through the IL7Rα and in the context of T cells, is expressed in a stage specific manner on developing thymocytes and on resting peripheral T cells and is down-regulated once cells are activated—possibly due to IL-2 signalling [159]. IL7Rα expression is highest on immature triple negative thymocytes and mature single positive thymocytes. The post-thymic expression is highest on recent thymic emigrants (RTE), naïve and memory cells and least on effector cells and late memory/senescent populations. Pre-clinical studies in rodents and primates have shown that IL-7 administration following BMT [160, 161] can enhance peripheral T cell reconstitution without aggravating GVHD [162], although some studies have demonstrated an IL7 induced bone loss [163]. Expansion of naïve CD4+ and CD8+ T cells, increased TREC levels per T cell and improved functional response to influenza vaccine, collectively suggest both thymic and peripheral effects [164].
The first clinical trial using human recombinant IL-7 (rhIL-7; Cytheris) was performed on four sequential cohorts of three patients (11 metastatic melanoma and one metastatic sarcoma; age range 20–59 years), each receiving graded doses of rhIL7 delivered subcutaneously every 3 days for eight doses [165]. The administration of IL7 was well tolerated. Increases in both CD4 and CD8 lymphocytes were evident in a dose dependent manner, with a trend towards increased CD45RA+ naïve cells. No increases in Foxp3 expressing Tregs were evident and there was no impact on circulating B cells or NK cells, although some, but not all, patients showed an increase in B progenitor cells in a BM biopsy.
Recently, in a phase 1 dose-escalation clinical trial administering rhIL-7, 16 patients with non-haematological, non-lymphoid cancer refractory to standard therapy (age range 20–71 years) [166] were subcutaneously administered every other day a total of eight doses. rhIL7 did not appear to induce thymic regrowth, although this is not surprising given the short duration of the treatment. However, the rhIL-7 preferentially expanded peripheral RTEs, naïve T cells and central memory CD4+ T cells and unlike rhIL2 therapy, the T regulatory cells were not expanded disproportionately. The increased TcR receptor diversity appears to have derived from the expansion of pre-existing RTEs, potentially restoring balance to an otherwise skewed ageing repertoire. Only two patients withdrew from the trial due to dose limiting toxicity, namely elevations of transaminases and hypertension and chest pain.
This important study suggests that rhIL-7 has the potential to enhance T cell reconstitution following BMT. Whether this treatment can induce long-term effects by enhancing thymopoiesis has yet to be clarified, however, as for GH, it could be used as an important adjuvant to other more robust therapies that target TEC regeneration.
Keratinocyte growth factor
Keratinocyte growth factor (KGF; also known as Fgf-7), is a member of the fibroblast growth factor family and is a potent mitogen for many epithelial cell types, regulating their growth, differentiation and morphogenesis [167–175]. In the thymus, mesenchyme-dependent production of Fgf-7 and Fgf-10 regulate the development and proliferation of thymic epithelium expressing a specific isoform of the Fgf receptor 2, FgfR2IIIb. Mature SP thymocytes may also provide a source of KGF [12, 40, 176]. Removal of the thymic mesenchyme at day 12 of embryogenesis (E12), as well as a deficiency of FgfR2IIIb or its ligand Fgf-10, significantly impaired development of the thymic epithelial compartment, resulting in a functional, but severely hypoplastic thymus [12, 13]. In contrast, the function of KGF appears redundant in the steady-state thymus, which is of normal size in KGF deficient mice. However, KGF appears to play a crucial role in aiding thymic recovery in situations of thymic damage [177].
Systemic administration of KGF has been shown to significantly increase both thymic weight and function in young mice and reverse age-associated thymic atrophy of 15-month-old mice for up to 8 weeks following a single KGF time course (5 mg/kg per day administered subcutaneously over 3 days). Repeated monthly injections were able to sustain thymus growth for 12 weeks [178]. In pre-clinical studies, KGF significantly enhanced thymic recovery and function following radiation—and chemotherapy—conditioning for allogeneic BMT in mice [41] and autologous HSCT in rhesus macaques [179]. It increased the peripheral reconstitution of naïve T cells and subsequent immune response to T cell-dependent neo-antigens. TECs are directly damaged by irradiation therapy [90] and KGF may provide their cytoprotection, similar to that reported for epithelial tissue of the lung [175, 180], gastrointenstinal tract [168] and mouth [181, 182]. KGF treatment has also shown potential to reduce the severity of GVHD induced in mice receiving allogeneic BMT [183, 184] and following adoptive allogeneic T cell transfer [185] and may do so by reducing the production of inflammatory cytokines. Whilst basic thymic structure and normal thymopoiesis were seemingly restored in models of chronic GVHD, KGF treatment failed to preserve the expression of Aire in mTEC [185], raising the potential for escape of auto-reactive T cells.
Recently, the combined treatment of KGF and LHRH-A was demonstrated to enhance thymic recovery and peripheral reconstitution of naïve T cells in an additive fashion following total body irradiation (TBI) and allogeneic BMT in mice [186]. This included recovery of the thymic stromal compartment and importantly, restoration of the mTEChi Aire expressing subset, above that of either LHRH-A or KGF treatment alone. Interestingly, this study demonstrated an equivalent loss of TEC number post-transplant, regardless of KGF treatment, indicating that accelerated TEC recovery, rather than a generalised cytoprotection of the epithelial compartment, may be responsible for enhanced thymopoietic recovery, at least in this setting of TBI for allogeneic BMT.
Clinically, combination therapy of KGF and LHRH-A may reduce the dosage of each yet still enhance the restoration of T cell-mediated immunity in situations of severe thymic atrophy or dysfunction following intensive conditioning regimes. Recombinant human KGF (palifermin) treatment has shown clinical effectiveness in reducing the duration and severity of chemotherapy-induced mucositis in patients with haematological malignancies [181]. However, its application in other malignant disorders, in particular those of epithelial origin, needs to be addressed with some caution, due to potential protection or proliferation of FgfR2-expressing tumorigenic cells [187].
Flt3 ligand
Fms-like tyrosine kinase 3 (Flt3; also termed Fetal liver kinase 2) is a tyrosine kinase receptor with homology to c-kit, c-fms and platelet-derived growth factor receptors and plays a well-reported role in the regulation of haematopoiesis and to a lesser extent thymopoiesis [188]. In the BM, Flt3 is not expressed in self-renewing HSCs but is enriched on haematopoietic progenitor cells, including lymphoid progenitors. It regulates homeostasis of multi-potent and early lineage committed progenitors via interaction with Flt3 ligand (Flt3L) expressed by the local BM niche environment [189–194]. Examination of the BM of Flt3-deficient mice revealed reduced numbers of haematopoietic progenitor cells and an impaired ability to competitively reconstitute lethally irradiated recipients, most significantly in the generation of T and myeloid lineages [195, 196]. Conversely, pre-treatment of mice with progenipoietin (a dual receptor agonist of Flt3 and granulocyte colony-stimulating factor; G-CSF) prolonged survival of lethally irradiated mice via radioprotection of the haematopoietic compartment [197] and is superior to G-CSF treatment alone, in the prevention of GVHD following allogeneic HSCT [198].
Murine T cell reconstitution studies have indicated that treatment with Flt3L can enhance recovery of the peripheral T cell pool via both thymic-dependent and -independent means [95, 199, 200]. In such situations, it may indirectly influence homeostatic expansion and function of the peripheral T cell pool, by mediating the expansion and availability of dendritic cell (DC) populations [199]. In addition, Flt3L treatment increased the number of naïve, donor T cells following irradiation and HSCT, indicating direct modulation of thymic function [199]. Furthermore, the expression of Flt3 receptor on a sub-population of T cell progenitors in the BM—the common lymphoid progenitor, as well as on the earliest intra-thymic progenitors [201, 202], suggests its action may also occur at the very early stages of haematopoietic and T lymphopoietic recovery. Indeed, enhanced thymopoiesis and peripheral T cell generation following Flt3L treatment and BMT was preceded by an increase in BM lymphoid progenitor cells [200, 203]. The thymic autonomous nature of Flt3L was recently demonstrated by its expression on thymic stromal cells, particularly the mesenchymal cells, early in thymopoietic reconstitution following lethal irradiation and HSCT [95]. Interestingly, whilst Flt3L strongly enhanced peripheral T cell recovery following BMT, co-administration of Flt3L and IL-7 showed no additive effects [200].
In humans, Flt3 expression appears in both the BM and cord blood HSC populations capable of long-term reconstitution, extending to progenitors of the lymphoid and granulocyte/macrophage lineages [204]. Flt3 signalling prevents spontaneous apoptotic cell death, suggesting an important role in cell survival [205]. Whilst Flt3L appears to effect T cell recovery at multiple levels, the different distribution of Flt3 in mouse and human haematopoiesis warrants further investigation in disease specific models.
Adult stem cell therapy
The appeal of stem cells for therapeutic application lies in their unique ability to replenish themselves as well as their capacity to differentiate into multiple cell lineages. These characteristic properties are fundamental to not only tissue organogenesis during development but also in tissue replenishment, maintenance and repair in the adult. The need for specialised tissues and organs progressively restricts the development of stem cells to being either multi-potent or uni-potent, such that post-natally, specialised niches in various tissues serve as reservoirs for stem cells. The importance of such niches is their protective micro-environment for stem cell survival, regulating asymmetric versus symmetric division and protection of the stem cell genetic profile [206, 207]. Constant dialogue between the stem cells, niche cells—including mesenchyme and extra-cellular matrix and cues from the surrounding tissue—are crucial to the maintenance of cellular homeostasis, balancing quiescence and activity (see review [115]).
There is now a growing list of tissue-specific markers for adult stem cells and their specialised niche micro-environments are increasingly being characterised (see review [114]). Being able to specifically target these for focal tissue regeneration would be ideal clinically, minimising the risk of systemic, invariably detrimental, side effects. In turn, this requires a detailed knowledge of the complex signalling pathways directing stem cell differentiation and these are now slowly being unravelled. An important consideration for such therapies to be effective is the age of the patient. Recent work has demonstrated age-related alterations in stem cell niches that could contribute to deficient stem cell number and/or activity including cell fate plasticity, expansion capacity, telomere length and lifespan (for example [121, 208–211]), leading to a decline in regenerative potential—a hallmark of ageing.
Thymic epithelial stem or progenitor cells: TEC maintenance and damage recovery
The epithelial and structural complexity of the thymus and the importance of its integrity for generating normal T cells represents a particular challenge for regenerative medicine. Do all the epithelial subsets derive from a single stem cell or are there region-specific progenitors? The existence of resident bi-potent thymic epithelial stem cells has been demonstrated in the mouse embryo [212–214] and indirectly in the young adult through reversion of a conditional Foxn1 mutation in TECs [215], with single cells able to generate both cortical and medullary TEC phenotypes.
Thymic epithelial stem cell studies have mostly been functionally confirmed in rodents by grafting putative progenitor epithelial cells isolated from the embryonic thymus, re-aggregated ex vivo, then grafted under the kidney capsule of athymic mice. By 4 weeks, clear formation of functional vascularised thymic tissue can be achieved with the necessary micro-environments to attract haematopoietic precursors, sustain full T cell differentiation and present self-peptides for negative selection. MTS24, an antibody developed from thymic stromal cells [216] identifies the antigen Plet-1 [217] and binds to putative thymic epithelial progenitor cells in the embryo. MTS24 is expressed in the emerging E10.5 mouse thymic anlage in the endodermal layer of the third pharyngeal pouch and is gradually restricted in expression as the thymus develops and expands such that by E15.5 it is expressed on less than 50% of TECs [212, 213]. Grafting of only 5,000 E15.5 MTS24 expressing cells under the kidney capsule forms a complete thymus by 4 weeks. However, equivalent grafting experiments using the post-natal thymus as a source have been unsuccessful, prompting the question of whether the MTS24 identifies thymic progenitor capacity at the completion of development. Furthermore, if larger quantities of embryonic cells are re-aggregated (such as 100,000 cells), both MTS24+ and MTS24− populations can form a thymus [218], questioning the uniqueness of Plet1 in identifying true progenitor TECs.
In the adult, Plet1 (identified by MTS24 expression) is preferentially expressed on a subset of mTECs, the majority of which represent a more quiescent population expressing low levels of MHCII (Fletcher, submitted manuscript). In addition, the expression of molecules characteristic of pluripotential cells (Oct4, Nanog, Sox2, Ehox, DPPa3) and developmental regulators of TEC differentiation (FoxN1, Pax1, Eya1, Hoxa3, Pax9, lymphotoxin β receptor) have been found to be expressed in sub-populations of mTECs [219]. Thus, whilst the precise identity of a single thymic epithelial stem cell (TESC) type is as yet unresolved in the adult, there is increasing evidence for its functional presence, given the capacity of the young adult thymus to rebound following severe injury, although theoretically this could also occur through self-renewal of pre-existing mature TEC subsets. Whether TESC reduce in number or function with age and contribute to age-induced involution also needs resolving if they are to be a target for regenerative strategies and thymus-based tolerance induction. Unfortunately, the human equivalent of TESCs is yet to be identified.
Developing a de novo thymus
Understanding the precise phenotype of TESCs would provide a means of potentially developing a thymus de novo, both in vivo and also in vitro. Seeding three-dimensional (3D) bio-matrices with patient or donor TESC, in combination as appropriate with mesenchyme, donor haematopoietic precursors (T cell and DC precursors) and requisite growth factors to encourage growth and vascularisation, may create a thymus. The ensuing T cells would not only restore immune competence, but they would also be donor (and host)-tolerant (Fig. 2). Such an artificial thymus could then be implanted into the host, providing a means of both overcoming graft rejection and enhancing T cell reconstitution. Although a number of issues remain with regard to safety and development of non-pathological T cells, human skin epidermal keratinocytes in combination with HSC have been reported to create human T cells [220] ex vivo. Murine thymic stromal 3D ‘organoids’ were also able to support human T cell development from CD34+ HSCs [221], albeit at very low efficiency. An interesting alternative to the provision of growth factors to encourage angiogenesis and overcome the problems of ischemic growth limitations is the use of a novel in vivo tissue engineering construct in which a macro-vascular arteriovenous shunt loop is enclosed in a poly-carbonate chamber in which cell populations, growth factors, matrices and other essential factors can be seeded [222, 223]. Whilst these strategies are unlikely to be translated into the clinic for some time, they do serve as a proof of concept. Working in parallel with the host thymus, enhanced T cell reconstitution and tolerance to both donor and host antigens may be achieved.
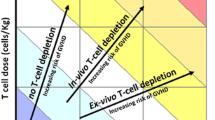
Strategies to enhance T-lymphoid reconstitution. Cytoablative regimes can severely damage the BM and thymic stromal micro-environments, delaying immune reconstitution after BMT. Exogenous factors such as LHRH-A, KGF, GH, Flt3L and IL-7 can be used to target either the TEC or thymocyte components for thymic and peripheral T cell regeneration. PTH, IL-7 and mesenchymal stem cells could enhance BM niche recovery and HSC engraftment. In combination, these could substantially enhance T cell reconstitution. Future therapies may include transplanting ESC or iPS-derived TECs and ex vivo expanded donor-derived TECs. LHRH-A luteinising hormone-releasing hormone analogue, KGF keratinocyte growth factor, GH growth hormone, Flt3L FMS-like tyrosine kinase 3-ligand, IL-7 interleukin-7, TEC thymic epithelial cell, PTH parathyroid hormone, ESC embryonic stem cell, iPS induced pluripotent cell
Future applications: embryonic stem cell therapy
There is enormous potential in regenerative therapies from ES cell approaches; however, there are controversial ethical and safety issues surrounding their use. Because ES cells can form teratomas when implanted, some in vitro lineage commitment will initially be required. Tolerance issues will therefore need to be addressed to ensure the foreign transplant will not be rejected (see review [224]). Alternative sources of pluripotential cells have recently emerged. Epithelial stem cells derived from amnion [225], if stored at birth, can be a source of self stem cells without the associated ethical controversy. These human amnion epithelial cells have been demonstrated to retain pluripotency that is being able to form cell derivatives from all three germ layers (endoderm, ectoderm, mesoderm); they therefore have enormous clinical potential. Furthermore, the developing technology around induced pluripotential stem cells (iPS), which involves re-programming of somatic cells to become ESC-like cells by transducing with ESC-associated factors—including Sox2, Oct3/4, Nanog and Klf-4 [226], offers potential for autologous cell-based regenerative therapies, therefore avoiding the obvious issues of immune rejection. Not withstanding their potential importance as diagnostic or drug testing tools, given the enormity of genetic and epigenetic modification involved in iPS, there are still various safety concerns for their clinical utility.
The tissue specific morphogenetic cues required to trigger the activation of specific differentiation signalling pathways is quite complex, requiring directed differentiation of ESCs initially into definitive endoderm and then thymic epithelium. It is likely to be some time before this can be achieved for clinical application.
Can stem cell therapies be practically applied to the clinic?
Given that most diseases are multi-factorial in aetiology, it would be predicted that their therapeutic management would involve combination treatments. Whilst major advances are being made in the derivation of tissue-specific cell types from ESCs and the identification of other allogeneic stem cells, their clinical utility will be hampered by the confrontation of such cells with a normally hostile host immune system, as for any transplanted non-self cell, tissue or organ. This is certainly the case with many degenerative diseases. They will require tissue-specific stem cells or their immediate derivatives, retardation of the immune response to prevent rejection and subsequently rebuilding of a donor tolerant immune system. In the case of auto-immune disease, it is also necessary to silence the pathological arm of the immune system. To overcome the rejection problem and for long-term low morbidity graft acceptance, it would be ideal to utilise the body’s normal thymus-based mechanisms for inducing self-tolerance, rather than rely on long-term immunosuppressive regimes. Strategies for developing appropriate Tregs are now emerging but it is unclear how long they can last in vivo. As discussed in this review, the pre-clinical and clinical studies on the restoration of thymic function in adults, such as using reversible, hormonally (LHRH)-based sex steroid reduction, have thus provided fundamentally new therapeutic platforms for addressing T cell-based deficiencies and disorders, paramount amongst which are enhancement of T cell reconstitution and induction of transplantation tolerance.
Protocols for stem cell-based thymic regenerative therapies (Fig. 2) could proceed with:
-
(a)
Endogenous thymus: combined administration of LHRH-A and other therapeutic agents such as KGF, GH, Flt3L to initiate in situ thymus recovery and reduce damage from cytoablative regimes. PTH and MSCs could be included to improve BM function to facilitate subsequent HSC engraftment and IL-7 administration to enhance T cell development and naïve T cell proliferation.
-
(b)
‘De novo’ thymus production: transplantation of ESC or iPS derived TEC or ex vivo expanded TEC biopsy.
-
(c)
Creation of donor tolerance: transplantation of donor HSCT to create a chimeric thymus and peripheral immune system.
-
(d)
Further expansion of naïve T cells if necessary by IL-7 administration and possibly Flt3L.
Conclusion
HSCT stands as one of the pivotal breakthroughs in the clinical management of disseminated haematological malignancies. Despite its global acceptance as a standard of care, however, the legacy of HSCT is profound immune deficiency resulting from age-related thymic atrophy, which is further exacerbated by the necessary cytoreductive conditioning. The immune deficiency leads to high levels of morbidity and often mortality and also underlies the inability to retard cancer relapse either directly or via response to cancer vaccination regimes. Hope that this immune deficiency can be overcome has recently stemmed from a combined research platform incorporating knowledge of the cellular and molecular basis to thymic organogenesis and its age-related atrophy. The rapidly emerging science of stem cell biology has also provided an important new impetus to these studies, facilitating the ability to reconstruct a thymus in vitro, or induce regeneration of the atrophic thymic remnant.
Currently, the most logical, clinically feasible approach would be to use agonist variants of LHRH to remove the inhibitory effects of sex steroids, which induce thymic atrophy (particularly post-puberty) and compromise BM function. LHRH-A may also provide a direct stimulatory effect on thymocytes cells. LHRH-A would be combined with one or more of KGF and GH, to promote TEC restoration and Flt3L and IL-7 to enhance T lymphoid progenitors. Chimeric thymic re-growth through allogeneic HSCT also induces donor tolerance. It is clear, however, that both the kinetics and degree of T cell recovery need improvement. The integration of strategies targeting thymic epithelial stem cells is emerging as the most rational and progressively feasible approach to achieve this.
References
Kim DH, Sohn SK, Won DI, Lee NY, Suh JS, Lee KB (2006) Rapid helper T-cell recovery above 200 × 10 6/l at 3 months correlates to successful transplant outcomes after allogeneic stem cell transplantation. Bone Marrow Transplant 37:1119–1128
Berger M, Figari O, Bruno B, Raiola A, Dominietto A, Fiorone M, Podesta M, Tedone E, Pozzi S, Fagioli F, Madon E, Bacigalupo A (2008) Lymphocyte subsets recovery following allogeneic bone marrow transplantation (BMT): CD4+ cell count and transplant-related mortality. Bone Marrow Transplant 41:55–62
Mackall CL, Fleisher TA, Brown MR, Andrich MP, Chen CC, Feuerstein IM, Horowitz ME, Magrath IT, Shad AT, Steinberg SM et al (1995) Age, thymopoiesis, and CD4+ T-lymphocyte regeneration after intensive chemotherapy. N Engl J Med 332:143–149
Gordon J, Bennett AR, Blackburn CC, Manley NR (2001) Gcm2 and Foxn1 mark early parathyroid- and thymus-specific domains in the developing third pharyngeal pouch. Mech Dev 103:141–143
Blackburn CC, Augustine CL, Li R, Harvey RP, Malin MA, Boyd RL, Miller JF, Morahan G (1996) The nu gene acts cell-autonomously and is required for differentiation of thymic epithelial progenitors. Proc Natl Acad Sci U S A 93:5742–5746
Nehls M, Kyewski B, Messerle M, Waldschutz R, Schuddekopf K, Smith AJ, Boehm T (1996) Two genetically separable steps in the differentiation of thymic epithelium. Science 272:886–889
Manley NR, Blackburn CC (2003) A developmental look at thymus organogenesis: where do the non-hematopoietic cells in the thymus come from? Curr Opin Immunol 15:225–232
Blackburn CC, Manley NR (2004) Developing a new paradigm for thymus organogenesis. Nat Rev Immunol 4:278–289
Hollander G, Gill J, Zuklys S, Iwanami N, Liu C, Takahama Y (2006) Cellular and molecular events during early thymus development. Immunol Rev 209:28–46
Jenkinson WE, Rossi SW, Jenkinson EJ, Anderson G (2005) Development of functional thymic epithelial cells occurs independently of lymphostromal interactions. Mech Dev 122:1294–1299
Suniara RK, Jenkinson EJ, Owen JJT (2000) An essential role for thymic mesenchyme in early T cell development. J Exp Med 191:1051–1056
Jenkinson WE, Jenkinson EJ, Anderson G (2003) Differential requirement for mesenchyme in the proliferation and maturation of thymic epithelial progenitors. J Exp Med 198:325–332
Revest JM, Suniara RK, Kerr K, Owen JJ, Dickson C (2001) Development of the thymus requires signaling through the fibroblast growth factor receptor R2-IIIb. J Immunol 167:1954–1961
Blom B, Res PC, Spits H (1998) T cell precursors in man and mice. Crit Rev Immunol 18:371–388
Itoi M, Kawamoto H, Katsura Y, Amagai T (2001) Two distinct steps of immigration of hematopoietic progenitors into the early thymus anlage. Int Immunol 13:1203–1211
van Ewijk W, Shores EW, Singer A (1994) Crosstalk in the mouse thymus. Immunol Today 15:214–217
Gruver AL, Hudson LL, Sempowski GD (2007) Immunosenescence of ageing. J Pathol 211:144–156
Min H, Montecino-Rodriguez E, Dorshkind K (2004) Reduction in the developmental potential of intrathymic T cell progenitors with age. J Immunol 173:245–250
George AJ, Ritter MA (1996) Thymic involution with ageing: obsolescence or good housekeeping? Immunol Today 17:267–272
Yung RL, Julius A (2008) Epigenetics, aging, and autoimmunity. Autoimmunity 41:329–335
Taub DD, Longo DL (2005) Insights into thymic aging and regeneration. Immunol Rev 205:72–93
Sempowski GD, Hale LP, Sundy JS, Massey JM, Koup RA, Douek DC, Patel DD, Haynes BF (2000) Leukemia inhibitory factor, oncostatin M, IL-6, and stem cell factor mRNA expression in human thymus increases with age and is associated with thymic atrophy. J Immunol 164:2180–2187
Kumar R, Langer JC, Snoeck HW (2006) Transforming growth factor-beta2 is involved in quantitative genetic variation in thymic involution. Blood 107:1974–1979
Hauri-Hohl MM, Zuklys S, Keller MP, Jeker LT, Barthlott T, Moon AM, Roes J, Hollander GA (2008) TGF-beta signaling in thymic epithelial cells regulates thymic involution and postirradiation reconstitution. Blood 112:626–634
Thoman ML, Weigle WO (1981) Lymphokines and aging: interleukin-2 production and activity in aged animals. J Immunol 127:2102–2106
Chang MP, Utsuyama M, Hirokawa K, Makinodan T (1988) Decline in the production of interleukin-3 with age in mice. Cell Immunol 115:1–12
Flurkey K, Miller RA, Harrison DE (1992) Cellular determinants of age-related decrements in the T-cell mitogen response of B6CBAF1 mice. J Gerontol 47:B115–120
Kubo M, Cinader B (1990) Polymorphism of age-related changes in interleukin (IL) production: differential changes of T helper subpopulations, synthesizing IL 2, IL 3 and IL 4. Eur J Immunol 20:1289–1296
Ernst DN, Hobbs MV, Torbett BE, Glasebrook AL, Rehse MA, Bottomly K, Hayakawa K, Hardy RR, Weigle WO (1990) Differences in the expression profiles of CD45RB, Pgp-1, and 3G11 membrane antigens and in the patterns of lymphokine secretion by splenic CD4+ T cells from young and aged mice. J Immunol 145:1295–1302
Hobbs MV, Weigle WO, Noonan DJ, Torbett BE, McEvilly RJ, Koch RJ, Cardenas GJ, Ernst DN (1993) Patterns of cytokine gene expression by CD4+ T cells from young and old mice. J Immunol 150:3602–3614
Paganelli R, Scala E, Quinti I, Ansotegui IJ (1994) Humoral immunity in aging. Aging (Milano) 6:143–150
Sempowski GD, Gooding ME, Liao HX, Le PT, Haynes BF (2002) T cell receptor excision circle assessment of thymopoiesis in aging mice. Mol Immunol 38:841–848
Andrew D, Aspinall R (2002) Age-associated thymic atrophy is linked to a decline in IL-7 production. Exp Gerontol 37:455–463
Aspinall R, Andrew D (2000) Thymic atrophy in the mouse is a soluble problem of the thymic environment. Vaccine 18:1629–1637
Aspinall R, Andrew D (2000) Thymic involution in aging. J Clin Immunol 20:250–256
Ortman CL, Dittmar KA, Witte PL, Le PT (2002) Molecular characterization of the mouse involuted thymus: aberrations in expression of transcription regulators in thymocyte and epithelial compartments. Int Immunol 14:813–822
Li L, Hsu HC, Stockard CR, Yang P, Zhou J, Wu Q, Grizzle WE, Mountz JD (2004) IL-12 inhibits thymic involution by enhancing IL-7- and IL-2-induced thymocyte proliferation. J Immunol 172:2909–2916
Leclercq G, Plum J (1996) Thymic and extrathymic T cell development. Leukemia 10:1853–1859
Bloom ET, Horvath JA (1994) Cellular and molecular mechanisms of the IL-12-induced increase in allospecific murine cytolytic T cell activity. Implications for the age-related decline in CTL. J Immunol 152:4242–4254
Erickson M, Morkowski S, Lehar S, Gillard G, Beers C, Dooley J, Rubin JS, Rudensky A, Farr AG (2002) Regulation of thymic epithelium by keratinocyte growth factor. Blood 100:3269–3278
Min D, Taylor PA, Panoskaltsis-Mortari A, Chung B, Danilenko DM, Farrell C, Lacey DL, Blazar BR, Weinberg KI (2002) Protection from thymic epithelial cell injury by keratinocyte growth factor: a new approach to improve thymic and peripheral T-cell reconstitution after bone marrow transplantation. Blood 99:4592–4600
Jiang Q, Coffield VM, Kondo M, Su L (2007) TSLP is involved in expansion of early thymocyte progenitors. BMC Immunol 8:11
Kecha O, Brilot F, Martens H, Franchimont N, Renard C, Greimers R, Defresne MP, Winkler R, Geenen V (2000) Involvement of insulin-like growth factors in early T cell development: a study using fetal thymic organ cultures. Endocrinology 141:1209–1217
Van der Ven LT, Roholl PJ, Reijnen-Gresnigt MG, Bloemen RJ, van Buul-Offers SC (1997) Expression of insulin-like growth factor II (IGF-II) and histological changes in the thymus and spleen of transgenic mice overexpressing IGF-II. Histochem Cell Biol 107:193–203
Lamberts SW, van den Beld AW, van der Lely AJ (1997) The endocrinology of aging. Science 278:419–424
Kecha O, Martens H, Franchimont N, Achour I, Hazee-Hagelstein MT, Charlet-Renard C, Geenen V, Winkler R (1999) Characterization of the insulin-like growth factor axis in the human thymus. J Neuroendocrinol 11:435–440
Bruunsgaard H, Andersen-Ranberg K, Jeune B, Pedersen AN, Skinhoj P, Pedersen BK (1999) A high plasma concentration of TNF-alpha is associated with dementia in centenarians. J Gerontol Ser A Biol Sci Med Sci 54:M357–364
Paolisso G, Rizzo MR, Mazziotti G, Tagliamonte MR, Gambardella A, Rotondi M, Carella C, Giugliano D, Varricchio M, D'Onofrio F (1998) Advancing age and insulin resistance: role of plasma tumor necrosis factor-alpha. Am J Physiol 275:E294–E299
Zubkova I, Mostowski H, Zaitseva M (2005) Up-regulation of IL-7, stromal-derived factor-1 alpha, thymus-expressed chemokine, and secondary lymphoid tissue chemokine gene expression in the stromal cells in response to thymocyte depletion: implication for thymus reconstitution. J Immunol 175:2321–2330
Gui J, Zhu X, Dohkan J, Cheng L, Barnes PF, Su DM (2007) The aged thymus shows normal recruitment of lymphohematopoietic progenitors but has defects in thymic epithelial cells. Int Immunol 19:1201–1211
Fabris N, Mocchegiani E (1985) Endocrine control of thymic serum factor production in young-adult and old mice. Cell Immunol 91:325–335
Savino W, Dardenne M, Bach JF (1983) Thymic hormone containing cells. II. Evolution of cells containing the serum thymic factor (FTS or thymulin) in normal and autoimmune mice, as revealed by anti-FTS monoclonal antibodies. Relationship with Ia bearing cells. Clin Exp Immunol 52:1–6
Bach JF, Papiernik M, Levasseur P, Dardenne M, Barois A, Le Brigand H (1972) Evidence for a serum-factor secreted by the human thymus. Lancet 2:1056–1058
Fabris N, Mocchegiani E, Amadio L, Zannotti M, Licastro F, Franceschi C (1984) Thymic hormone deficiency in normal ageing and Down's syndrome: is there a primary failure of the thymus? Lancet 1:983–986
Bodey B, Bodey B Jr, Siegel SE, Kaiser HE (1997) Involution of the mammalian thymus, one of the leading regulators of aging. In Vivo 11:421–440
Hirokawa K, McClure JE, Goldstein AL (1982) Age-related changes in localization of thymosin in the human thymus. Thymus 4:19–29
Dixit VD, Yang H, Sun Y, Weeraratna AT, Youm YH, Smith RG, Taub DD (2007) Ghrelin promotes thymopoiesis during aging. J Clin Invest 117:2778–2790
Burgess W, Liu Q, Zhou J, Tang Q, Ozawa A, VanHoy R, Arkins S, Dantzer R, Kelley KW (1999) The immune-endocrine loop during aging: role of growth hormone and insulin-like growth factor-I. Neuroimmunomodulation 6:56–68
Chen BJ, Cui X, Sempowski GD, Chao NJ (2003) Growth hormone accelerates immune recovery following allogeneic T-cell-depleted bone marrow transplantation in mice. Exp Hematol 31:953–958
Aloe L, Micera A, Bracci-Laudiero L, Vigneti E, Turrini P (1997) Presence of nerve growth factor in the thymus of prenatal, postnatal and pregnant rats. Thymus 24:221–231
Turrini P, Zaccaria ML, Aloe L (2001) Presence and possible functional role of nerve growth factor in the thymus. Cell Mol Biol (Noisy-le-grand) 47:55–64
Maroder M, Bellavia D, Meco D, Napolitano M, Stigliano A, Alesse E, Vacca A, Giannini G, Frati L, Gulino A, Screpanti I (1996) Expression of trKB neurotrophin receptor during T cell development. Role of brain derived neurotrophic factor in immature thymocyte survival. J Immunol 157:2864–2872
Tokuda N, Hamasaki K, Mizutani N, Adachi Y, Sawada T, Funahashi H, Shioda S, Fukumoto T (2004) Expression of PAC1 receptor in rat thymus after irradiation. Regul Pept 123:167–172
Garcia-Suarez O, Perez-Perez M, Germana A, Esteban I, Germana G (2003) Involvement of growth factors in thymic involution. Microsc Res Tech 62:514–523
Brock N (1996) The history of the oxazaphosphorine cytostatics. Cancer 78:542–547
Trobaugh FE Jr, Husseini S (1973) Effects of radiation on hematopoietic tissue. Am J Med Technol 39:119–131
Zitvogel L, Apetoh L, Ghiringhelli F, Kroemer G (2008) Immunological aspects of cancer chemotherapy. Nat Rev Immunol 8:59–73
Mackall CL, Fleisher TA, Brown MR, Magrath IT, Shad AT, Horowitz ME, Wexler LH, Adde MA, McClure LL, Gress RE (1994) Lymphocyte depletion during treatment with intensive chemotherapy for cancer. Blood 84:2221–2228
Krenger W, Hollander GA (2008) The thymus in GVHD pathophysiology. Best Pract Res Clin Haematol 21:119–128
Rizzi M, Ferrera F, Filaci G, Indiveri F (2006) Disruption of immunological tolerance: role of AIRE gene in autoimmunity. Autoimmun Rev 5:145–147
Sakaguchi S, Sakaguchi N (1988) Thymus and autoimmunity. Transplantation of the thymus from cyclosporin A-treated mice causes organ-specific autoimmune disease in athymic nude mice. J Exp Med 167:1479–1485
Wang H, Zhao L, Sun Z, Sun L, Zhang B, Zhao Y (2006) A potential side effect of cyclosporin A: inhibition of CD4(+)CD25(+) regulatory T cells in mice. Transplantation 82:1484–1492
Storek J, Witherspoon RP, Storb R (1995) T cell reconstitution after bone marrow transplantation into adult patients does not resemble T cell development in early life. Bone Marrow Transplant 16:413–425
Weinberg K, Annett G, Kashyap A, Lenarsky C, Forman SJ, Parkman R (1995) The effect of thymic function on immunocompetence following bone marrow transplantation. Biol Blood Marrow Transplant 1:18–23
Mackall CL, Fleisher TA, Brown MR, Andrich MP, Chen CC, Feuerstein IM, Magrath IT, Wexler LH, Dimitrov DS, Gress RE (1997) Distinctions between CD8+ and CD4+ T-cell regenerative pathways result in prolonged T-cell subset imbalance after intensive chemotherapy. Blood 89:3700–3707
Fagnoni FF, Lozza L, Zibera C, Zambelli A, Ponchio L, Gibelli N, Oliviero B, Pavesi L, Gennari R, Vescovini R, Sansoni P, Da Prada G, Robustelli Della Cuna G (2002) T-cell dynamics after high-dose chemotherapy in adults: elucidation of the elusive CD8+ subset reveals multiple homeostatic T-cell compartments with distinct implications for immune competence. Immunology 106:27–37
Sfikakis PP, Gourgoulis GM, Moulopoulos LA, Kouvatseas G, Theofilopoulos AN, Dimopoulos MA (2005) Age-related thymic activity in adults following chemotherapy-induced lymphopenia. Eur J Clin Invest 35:380–387
Li F, Jin F, Freitas A, Szabo P, Weksler ME (2001) Impaired regeneration of the peripheral B cell repertoire from bone marrow following lymphopenia in old mice. Eur J Immunol 31:500–505
Gardner RV, McKinnon E, Astle CM (2001) Analysis of the stem cell sparing properties of cyclophosphamide. Eur J Haematol 67:14–22
Meng A, Wang Y, Brown SA, Van Zant G, Zhou D (2003) Ionizing radiation and busulfan inhibit murine bone marrow cell hematopoietic function via apoptosis-dependent and -independent mechanisms. Exp Hematol 31:1348–1356
Meng A, Wang Y, Van Zant G, Zhou D (2003) Ionizing radiation and busulfan induce premature senescence in murine bone marrow hematopoietic cells. Cancer Res 63:5414–5419
Offner F, Kerre T, De Smedt M, Plum J (1999) Bone marrow CD34 cells generate fewer T cells in vitro with increasing age and following chemotherapy. Br J Haematol 104:801–808
Wang Y, Schulte BA, LaRue AC, Ogawa M, Zhou D (2006) Total body irradiation selectively induces murine hematopoietic stem cell senescence. Blood 107:358–366
Mizutani N, Fujikura Y, Wang YH, Tamechika M, Tokuda N, Sawada T, Fukumoto T (2002) Inflammatory and anti-inflammatory cytokines regulate the recovery from sublethal X irradiation in rat thymus. Radiat Res 157:281–289
Greenberg DB, Gray JL, Mannix CM, Eisenthal S, Carey M (1993) Treatment-related fatigue and serum interleukin-1 levels in patients during external beam irradiation for prostate cancer. J Pain Symptom Manage 8:196–200
Abdul-Hai A, Ben-Yehuda A, Galsky H, Slavin S, Or R (2006) Interleukin 2 regulation following semi-allogeneic bone marrow transplantation in mice. Cancer Immunol Immunother 55:1330–1336
Xia YJ, Gao QP, Wan CC, Cheng FJ, Wang WM, Guo RC (2005) [Effects of HGF on GVHD and Th1/Th2-related cytokines in ALL mice after allo-BMT]. Zhongguo Shi Yan Xue Ye Xue Za Zhi 13:35–38
Yang YC, Wang KL, Su TH, Liao HF, Wu MH, Chen TC, Huang MC, Chen YJ (2006) Concurrent cisplatin-based chemoradiation for cervical carcinoma: tumor response, toxicity, and serum cytokine profiles. Cancer Invest 24:390–395
Gridley DS, Bonnet RB, Bush DA, Franke C, Cheek GA, Slater JD, Slater JM (2004) Time course of serum cytokines in patients receiving proton or combined photon/proton beam radiation for resectable but medically inoperable non-small-cell lung cancer. Int J Radiat Oncol Biol Phys 60:759–766
Chung B, Barbara-Burnham L, Barsky L, Weinberg K (2001) Radiosensitivity of thymic interleukin-7 production and thymopoiesis after bone marrow transplantation. Blood 98:1601–1606
Uchimura E, Watanabe N, Niwa O, Muto M, Kobayashi Y (2000) Transient infiltration of neutrophils into the thymus in association with apoptosis induced by whole-body X-irradiation. J Leukoc Biol 67:780–784
Garncarek D (1978) Short time and prolonged low dose X radiation in human immunity. Arch Immunol Ther Exp (Warsz) 26:905–911
Brennan BM, Rahim A, Mackie EM, Eden OB, Shalet SM (1998) Growth hormone status in adults treated for acute lymphoblastic leukaemia in childhood. Clin Endocrinol (Oxf) 48:777–783
Chen W, Frank ME, Jin W, Wahl SM (2001) TGF-beta released by apoptotic T cells contributes to an immunosuppressive milieu. Immunity 14:715–725
Kenins L, Gill JW, Boyd RL, Hollander GA, Wodnar-Filipowicz A (2008) Intrathymic expression of Flt3 ligand enhances thymic recovery after irradiation. J Exp Med 205:523–531
Chklovskaia E, Jansen W, Nissen C, Lyman SD, Rahner C, Landmann L, Wodnar-Filipowicz A (1999) Mechanism of flt3 ligand expression in bone marrow failure: translocation from intracellular stores to the surface of T lymphocytes after chemotherapy-induced suppression of hematopoiesis. Blood 93:2595–2604
Mantovani G, Madeddu C, Gramignano G, Lusso MR, Mocci M, Massa E, Ferreli L, Astara G, Maccio A, Serpe R (2003) Subcutaneous interleukin-2 in combination with medroxyprogesterone acetate and antioxidants in advanced cancer responders to previous chemotherapy: phase II study evaluating clinical, quality of life, and laboratory parameters. J Exp Ther Oncol 3:205–219
Tsavaris N, Kosmas C, Vadiaka M, Kanelopoulos P, Boulamatsis D (2002) Immune changes in patients with advanced breast cancer undergoing chemotherapy with taxanes. Br J Cancer 87:21–27
Sato M, Kasai C, Takeuchi S, Takemura M, Shimokawa K, Noma A (1992) [Changes in serum cytokine levels in patients with malignant bone and soft tissue tumors in the course of chemotherapy]. Gan To Kagaku Ryoho 19:1449–1452
Kanabrocki EL, Hermida RC, Haseman MB, Bettis K, Young RM, Mathew JP, Potkul R, Hrushesky WJ (2006) Chronotherapy of ovarian cancer: effect on blood variables and serum cytokines. A case report. Clin Ter 157:349–354
Wood LJ, Nail LM, Perrin NA, Elsea CR, Fischer A, Druker BJ (2006) The cancer chemotherapy drug etoposide (VP-16) induces proinflammatory cytokine production and sickness behavior-like symptoms in a mouse model of cancer chemotherapy-related symptoms. Biol Res Nurs 8:157–169
Pedersen LM, Klausen TW, Davidsen UH, Johnsen HE (2005) Early changes in serum IL-6 and VEGF levels predict clinical outcome following first-line therapy in aggressive non-Hodgkin's lymphoma. Ann Hematol 84:510–516
Benicchi T, Ghidini C, Re A, Cattaneo C, Casari S, Caimi L, Rossi G, Imberti L (2005) T-cell immune reconstitution after hematopoietic stem cell transplantation for HIV-associated lymphoma. Transplantation 80:673–682
Sirohi B, Powles R, Morgan G, Treleaven J, Kulkarni S, Horton C, Saso R, Rolfe D, Cook G, Shaw C, Wass J (2007) Use of physiological doses of human growth hormone in haematological patients receiving intensive chemotherapy promotes haematopoietic recovery: a double-blind randomized, placebo-controlled study. Bone Marrow Transplant 39:115–120
Haylock DN, Williams B, Johnston HM, Liu MC, Rutherford KE, Whitty GA, Simmons PJ, Bertoncello I, Nilsson SK (2007) Hemopoietic stem cells with higher hemopoietic potential reside at the bone marrow endosteum. Stem Cells 25:1062–1069
Nilsson SK, Johnston HM, Coverdale JA (2001) Spatial localization of transplanted hemopoietic stem cells: inferences for the localization of stem cell niches. Blood 97:2293–2299
Kiel MJ, Yilmaz OH, Iwashita T, Yilmaz OH, Terhorst C, Morrison SJ (2005) SLAM family receptors distinguish hematopoietic stem and progenitor cells and reveal endothelial niches for stem cells. Cell 121:1109–1121
Kiel MJ, Morrison SJ (2008) Uncertainty in the niches that maintain haematopoietic stem cells. Nat Rev Immunol 8:290–301
Calvi LM, Adams GB, Weibrecht KW, Weber JM, Olson DP, Knight MC, Martin RP, Schipani E, Divieti P, Bringhurst FR, Milner LA, Kronenberg HM, Scadden DT (2003) Osteoblastic cells regulate the haematopoietic stem cell niche. Nature 425:841–846
Visnjic D, Kalajzic Z, Rowe DW, Katavic V, Lorenzo J, Aguila HL (2004) Hematopoiesis is severely altered in mice with an induced osteoblast deficiency. Blood 103:3258–3264
Zhang J, Niu C, Ye L, Huang H, He X, Tong WG, Ross J, Haug J, Johnson T, Feng JQ, Harris S, Wiedemann LM, Mishina Y, Li L (2003) Identification of the haematopoietic stem cell niche and control of the niche size. Nature 425:836–841
Nilsson SK, Johnston HM, Whitty GA, Williams B, Webb RJ, Denhardt DT, Bertoncello I, Bendall LJ, Simmons PJ, Haylock DN (2005) Osteopontin, a key component of the hematopoietic stem cell niche and regulator of primitive hematopoietic progenitor cells. Blood 106:1232–1239
Stier S, Ko Y, Forkert R, Lutz C, Neuhaus T, Grunewald E, Cheng T, Dombkowski D, Calvi LM, Rittling SR, Scadden DT (2005) Osteopontin is a hematopoietic stem cell niche component that negatively regulates stem cell pool size. J Exp Med 201:1781–1791
Jones DL, Wagers AJ (2008) No place like home: anatomy and function of the stem cell niche. Nat Rev Mol Cell Biol 9:11–21
Scadden DT (2006) The stem-cell niche as an entity of action. Nature 441:1075–1079
Xing Z, Ryan MA, Daria D, Nattamai KJ, Van Zant G, Wang L, Zheng Y, Geiger H (2006) Increased hematopoietic stem cell mobilization in aged mice. Blood 108:2190–2197
Liang Y, Van Zant G, Szilvassy SJ (2005) Effects of aging on the homing and engraftment of murine hematopoietic stem and progenitor cells. Blood 106:1479–1487
Min H, Montecino-Rodriguez E, Dorshkind K (2006) Effects of aging on the common lymphoid progenitor to pro-B cell transition. J Immunol 176:1007–1012
Rossi DJ, Bryder D, Zahn JM, Ahlenius H, Sonu R, Wagers AJ, Weissman IL (2005) Cell intrinsic alterations underlie hematopoietic stem cell aging. Proc Natl Acad Sci U S A 102:9194–9199
Guerrettaz LM, Johnson SA, Cambier JC (2008) Acquired hematopoietic stem cell defects determine B-cell repertoire changes associated with aging. Proc Natl Acad Sci U S A 105:11898–11902
Morrison SJ, Wandycz AM, Akashi K, Globerson A, Weissman IL (1996) The aging of hematopoietic stem cells. Nat Med 2:1011–1016
El-Badri NS, Wang BY, Cherry, Good RA (1998) Osteoblasts promote engraftment of allogeneic hematopoietic stem cells. Exp Hematol 26:110–116
Nilsson SK, Dooner MS, Weier HU, Frenkel B, Lian JB, Stein GS, Quesenberry PJ (1999) Cells capable of bone production engraft from whole bone marrow transplants in nonablated mice. J Exp Med 189:729–734
Le Blanc K, Rasmusson I, Sundberg B, Gotherstrom C, Hassan M, Uzunel M, Ringden O (2004) Treatment of severe acute graft-versus-host disease with third party haploidentical mesenchymal stem cells. Lancet 363:1439–1441
Bartholomew A, Sturgeon C, Siatskas M, Ferrer K, McIntosh K, Patil S, Hardy W, Devine S, Ucker D, Deans R, Moseley A, Hoffman R (2002) Mesenchymal stem cells suppress lymphocyte proliferation in vitro and prolong skin graft survival in vivo. Exp Hematol 30:42–48
Chen X, Armstrong MA, Li G (2006) Mesenchymal stem cells in immunoregulation. Immunol Cell Biol 84:413–421
Hince M, Sakkal S, Vlahos V, Dudakov J, Boyd R, Chidgey A (2008) The role of sex steroids and gonadectomy in the control of thymic involution. Cell Immunol 252(1–2):122–138
Wang J, Zhou F, Dong M, Wu R, Qian Y (2006) Prolonged gonadotropin-releasing hormone agonist therapy reduced expression of nitric oxide synthase in the endometrium of women with endometriosis and infertility. Fertil Steril 85:1037–1044
Dondi D, Festuccia C, Piccolella M, Bologna M, Motta M (2006) GnRH agonists and antagonists decrease the metastatic progression of human prostate cancer cell lines by inhibiting the plasminogen activator system. Oncol Rep 15:393–400
Vottero A, Pedori S, Verna M, Pagano B, Cappa M, Loche S, Bernasconi S, Ghizzoni L (2006) Final height in girls with central idiopathic precocious puberty treated with gonadotropin-releasing hormone analog and oxandrolone. J Clin Endocrinol Metab 91:1284–1287
Pritchard K (2005) Endocrinology and hormone therapy in breast cancer: endocrine therapy in premenopausal women. Breast Cancer Res 7:70–76
Blumenfeld Z (2002) Preservation of fertility and ovarian function and minimalization of chemotherapy associated gonadotoxicity and premature ovarian failure: the role of inhibin-A and -B as markers. Mol Cell Endocrinol 187:93–105
Fitzpatrick FT, Kendall MD, Wheeler MJ, Adcock IM, Greenstein BD (1985) Reappearance of thymus of ageing rats after orchidectomy. J Endocrinol 106:R17–R19
Greenstein BD, Fitzpatrick FT, Adcock IM, Kendall MD, Wheeler MJ (1986) Reappearance of the thymus in old rats after orchidectomy: inhibition of regeneration by testosterone. J Endocrinol 110:417–422
Greenstein BD, Fitzpatrick FT, Kendall MD, Wheeler MJ (1987) Regeneration of the thymus in old male rats treated with a stable analogue of LHRH. J Endocrinol 112:345–350
Marchetti B, Guarcello V, Morale MC, Bartoloni G, Farinella Z, Cordaro S, Scapagnini U (1989) Luteinizing hormone-releasing hormone-binding sites in the rat thymus: characteristics and biological function. Endocrinology 125:1025–1036
Nabarra B, Andrianarison I (1996) Ultrastructural study of thymic microenvironment involution in aging mice. Exp Gerontol 31:489
Utsuyama M, Hirokawa K (1989) Hypertrophy of the thymus and restoration of immune functions in mice and rats by gonadectomy. Mech Ageing Dev 47:175–185
Windmill KF, Meade BJ, Lee VW (1993) Effect of prepubertal gonadectomy and sex steroid treatment on the growth and lymphocyte populations of the rat thymus. Reprod Fertil Dev 5:73–81
Kendall MD, Fitzpatrick FT, Greenstein BD, Khoylou F, Safieh B, Hamblin A (1990) Reversal of ageing changes in the thymus of rats by chemical or surgical castration. Cell Tissue Res 261:555–564
Sutherland JS, Goldberg GL, Hammett MV, Uldrich AP, Berzins SP, Heng TS, Blazar BR, Millar JL, Malin MA, Chidgey AP, Boyd RL (2005) Activation of thymic regeneration in mice and humans following androgen blockade. J Immunol 175:2741–2753
Roden AC, Moser MT, Tri SD, Mercader M, Kuntz SM, Dong H, Hurwitz AA, McKean DJ, Celis E, Leibovich BC, Allison JP, Kwon ED (2004) Augmentation of T cell levels and responses induced by androgen deprivation. J Immunol 173:6098–6108
Heng TS, Goldberg GL, Gray DH, Sutherland JS, Chidgey AP, Boyd RL (2005) Effects of castration on thymocyte development in two different models of thymic involution. J Immunol 175:2982–2993
Anderson MS, Venanzi ES, Klein L, Chen Z, Berzins SP, Turley SJ, von Boehmer H, Bronson R, Dierich A, Benoist C, Mathis D (2002) Projection of an immunological self shadow within the thymus by the aire protein. Science 298:1395–1401
Liston A, Lesage S, Wilson J, Peltonen L, Goodnow CC (2003) Aire regulates negative selection of organ-specific T cells. Nat Immunol 4:350–354
Goldberg GL, Alpdogan O, Muriglan SJ, Hammett MV, Milton MK, Eng JM, Hubbard VM, Kochman A, Willis LM, Greenberg AS, Tjoe KH, Sutherland JS, Chidgey A, van den Brink MR, Boyd RL (2007) Enhanced immune reconstitution by sex steroid ablation following allogeneic hemopoietic stem cell transplantation. J Immunol 178:7473–7484
Goldberg GL, Sutherland JS, Hammet MV, Milton MK, Heng TS, Chidgey AP, Boyd RL (2005) Sex steroid ablation enhances lymphoid recovery following autologous hematopoietic stem cell transplantation. Transplantation 80:1604–1613
Sutherland JS, Spyroglou L, Muirhead JL, Heng TS, Prieto-Hinojosa A, Prince HM, Chidgey AP, Schwarer AP, Boyd RL (2008) Enhanced immune system regeneration in humans following allogeneic or autologous hemopoietic stem cell transplantation by temporary sex steroid blockade. Clin Cancer Res 14:1138–1149
Viselli SM, Olsen NJ, Shults K, Steizer G, Kovacs WJ (1995) Immunochemical and flow cytometric analysis of androgen receptor expression in thymocytes. Mol Cell Endocrinol 109:19–26
Olsen NJ, Viselli SM, Fan J, Kovacs WJ (1998) Androgens accelerate thymocyte apoptosis. Endocrinology 139:748–752
Olsen NJ, Viselli SM, Shults K, Stelzer G, Kovacs WJ (1994) Induction of immature thymocyte proliferation after castration of normal male mice. Endocrinology 134:107–113
Olsen NJ, Watson MB, Kovacs WJ (1991) Studies of immunological function in mice with defective androgen action. Distinction between alterations in immune function due to hormonal insensitivity and alterations due to other genetic factors. Immunology 73:52–57
Olsen NJ, Olson G, Viselli SM, Gu X, Kovacs WJ (2001) Androgen receptors in thymic epithelium modulate thymus size and thymocyte development. Endocrinology 142:1278–1283
Batticane N, Morale MC, Gallo F, Farinella Z, Marchetti B (1991) Luteinizing hormone-releasing hormone signaling at the lymphocyte involves stimulation of interleukin-2 receptor expression. Endocrinology 129:277–286
Ellis TM, Moser MT, Le PT, Flanigan RC, Kwon ED (2001) Alterations in peripheral B cells and B cell progenitors following androgen ablation in mice. Int Immunol 13:553–558
de Mello-Coelho V, Gagnerault MC, Souberbielle JC, Strasburger CJ, Savino W, Dardenne M, Postel-Vinay MC (1998) Growth hormone and its receptor are expressed in human thymic cells. Endocrinology 139:3837–3842
De Mello-Coelho V, Savino W, Postel-Vinay MC, Dardenne M (1998) Role of prolactin and growth hormone on thymus physiology. Dev Immunol 6:317–323
Napolitano LA, Schmidt D, Gotway MB, Ameli N, Filbert EL, Ng MM, Clor JL, Epling L, Sinclair E, Baum PD, Li K, Killian ML, Bacchetti P, McCune JM (2008) Growth hormone enhances thymic function in HIV-1-infected adults. J Clin Invest 118:1085–1098
Xue HH, Kovanen PE, Pise-Masison CA, Berg M, Radovich MF, Brady JN, Leonard WJ (2002) IL-2 negatively regulates IL-7 receptor alpha chain expression in activated T lymphocytes. Proc Natl Acad Sci U S A 99:13759–13764
Alpdogan O, Muriglan SJ, Eng JM, Willis LM, Greenberg AS, Kappel BJ, van den Brink MR (2003) IL-7 enhances peripheral T cell reconstitution after allogeneic hematopoietic stem cell transplantation. J Clin Invest 112:1095–1107
Bolotin E, Smogorzewska M, Smith S, Widmer M, Weinberg K (1996) Enhancement of thymopoiesis after bone marrow transplant by in vivo interleukin-7. Blood 88:1887–1894
Alpdogan O, Schmaltz C, Muriglan SJ, Kappel BJ, Perales MA, Rotolo JA, Halm JA, Rich BE, van den Brink MR (2001) Administration of interleukin-7 after allogeneic bone marrow transplantation improves immune reconstitution without aggravating graft-versus-host disease. Blood 98:2256–2265
Toraldo G, Roggia C, Qian WP, Pacifici R, Weitzmann MN (2003) IL-7 induces bone loss in vivo by induction of receptor activator of nuclear factor kappa B ligand and tumor necrosis factor alpha from T cells. Proc Natl Acad Sci U S A 100:125–130
Aspinall R, Pido-Lopez J, Imami N, Henson SM, Ngom PT, Morre M, Niphuis H, Remarque E, Rosenwirth B, Heeney JL (2007) Old rhesus macaques treated with interleukin-7 show increased TREC levels and respond well to influenza vaccination. Rejuvenation Res 10:5–17
Rosenberg SA, Sportes C, Ahmadzadeh M, Fry TJ, Ngo LT, Schwarz SL, Stetler-Stevenson M, Morton KE, Mavroukakis SA, Morre M, Buffet R, Mackall CL, Gress RE (2006) IL-7 administration to humans leads to expansion of CD8+ and CD4+ cells but a relative decrease of CD4+ T-regulatory cells. J Immunother 29:313–319
Sportes C, Hakim FT, Memon SA, Zhang H, Chua KS, Brown MR, Fleisher TA, Krumlauf MC, Babb RR, Chow CK, Fry TJ, Engels J, Buffet R, Morre M, Amato RJ, Venzon DJ, Korngold R, Pecora A, Gress RE, Mackall CL (2008) Administration of rhIL-7 in humans increases in vivo TCR repertoire diversity by preferential expansion of naive T cell subsets. J Exp Med 205:1701–1714
De Moerlooze L, Spencer-Dene B, Revest J, Hajihosseini M, Rosewell I, Dickson C (2000) An important role for the IIIb isoform of fibroblast growth factor receptor 2 (FGFR2) in mesenchymal–epithelial signalling during mouse organogenesis. Development 127:483–492
Farrell CL, Bready JV, Rex KL, Chen JN, DiPalma CR, Whitcomb KL, Yin S, Hill DC, Wiemann B, Starnes CO, Havill AM, Lu ZN, Aukerman SL, Pierce GF, Thomason A, Potten CS, Ulich TR, Lacey DL (1998) Keratinocyte growth factor protects mice from chemotherapy and radiation-induced gastrointestinal injury and mortality. Cancer Res 58:933–939
Finch PW, Cunha GR, Rubin JS, Wong J, Ron D (1995) Pattern of keratinocyte growth factor and keratinocyte growth factor receptor expression during mouse fetal development suggests a role in mediating morphogenetic mesenchymal–epithelial interactions. Dev Dyn 203:223–240
Finch PW, Rubin JS, Miki T, Ron D, Aaronson SA (1989) Human KGF is FGF-related with properties of a paracrine effector of epithelial cell growth. Science 245:752–755
Mason IJ, Fuller-Pace F, Smith R, Dickson C (1994) FGF-7 (keratinocyte growth factor) expression during mouse development suggests roles in myogenesis, forebrain regionalisation and epithelial-mesenchymal interactions. Mech Dev 45:15–30
Orr-Urtreger A, Bedford MT, Burakova T, Arman E, Zimmer Y, Yayon A, Givol D, Lonai P (1993) Developmental localization of the splicing alternatives of fibroblast growth factor receptor-2 (FGFR2). Dev Biol 158:475–486
Rubin JS, Bottaro DP, Chedid M, Miki T, Ron D, Cunha GR, Finch PW (1995) Keratinocyte growth factor as a cytokine that mediates mesenchymal–epithelial interaction. Exs 74:191–214
Rubin JS, Osada H, Finch PW, Taylor WG, Rudikoff S, Aaronson SA (1989) Purification and characterization of a newly identified growth factor specific for epithelial cells. Proc Natl Acad Sci U S A 86:802–806
Yi ES, Williams ST, Lee H, Malicki DM, Chin EM, Yin S, Tarpley J, Ulich TR (1996) Keratinocyte growth factor ameliorates radiation- and bleomycin-induced lung injury and mortality. Am J Pathol 149:1963–1970
Miki T, Bottaro DP, Fleming TP, Smith CL, Burgess WH, Chan AM, Aaronson SA (1992) Determination of ligand-binding specificity by alternative splicing:two distinct growth factor receptors encoded by a single gene. Proc Natl Acad Sci U S A 89:246–250
Alpdogan O, Hubbard VM, Smith OM, Patel N, Lu S, Goldberg GL, Gray DH, Feinman J, Kochman AA, Eng JM, Suh D, Muriglan SJ, Boyd RL, van den Brink MR (2006) Keratinocyte growth factor (KGF) is required for postnatal thymic regeneration. Blood 107:2453–2460
Min D, Panoskaltsis-Mortari A, Kuro OM, Hollander GA, Blazar BR, Weinberg KI (2007) Sustained thymopoiesis and improvement in functional immunity induced by exogenous KGF administration in murine models of aging. Blood 109:2529–2537
Seggewiss R, Lore K, Guenaga FJ, Pittaluga S, Mattapallil J, Chow CK, Koup RA, Camphausen K, Nason MC, Meier-Schellersheim M, Donahue RE, Blazar BR, Dunbar CE, Douek DC (2007) Keratinocyte growth factor augments immune reconstitution after autologous hematopoietic progenitor cell transplantation in rhesus macaques. Blood 110:441–449
Takeoka M, Ward WF, Pollack H, Kamp DW, Panos RJ (1997) KGF facilitates repair of radiation-induced DNA damage in alveolar epithelial cells. Am J Physiol 272:L1174–L1180
Spielberger R, Stiff P, Bensinger W, Gentile T, Weisdorf D, Kewalramani T, Shea T, Yanovich S, Hansen K, Noga S, McCarty J, LeMaistre CF, Sung EC, Blazar BR, Elhardt D, Chen MG, Emmanouilides C (2004) Palifermin for oral mucositis after intensive therapy for hematologic cancers. N Engl J Med 351:2590–2598
Stiff PJ, Emmanouilides C, Bensinger WI, Gentile T, Blazar B, Shea TC, Lu J, Isitt J, Cesano A, Spielberger R (2006) Palifermin reduces patient-reported mouth and throat soreness and improves patient functioning in the hematopoietic stem-cell transplantation setting. J Clin Oncol 24:5186–5193
Panoskaltsis-Mortari A, Lacey DL, Vallera DA, Blazar BR (1998) Keratinocyte growth factor administered before conditioning ameliorates graft-versus-host disease after allogeneic bone marrow transplantation in mice. Blood 92:3960–3967
Panoskaltsis-Mortari A, Taylor PA, Rubin JS, Uren A, Welniak LA, Murphy WJ, Farrell CL, Lacey DL, Blazar BR (2000) Keratinocyte growth factor facilitates alloengraftment and ameliorates graft-versus-host disease in mice by a mechanism independent of repair of conditioning-induced tissue injury. Blood 96:4350–4356
Rossi S, Blazar BR, Farrell CL, Danilenko DM, Lacey DL, Weinberg KI, Krenger W, Hollander GA (2002) Keratinocyte growth factor preserves normal thymopoiesis and thymic microenvironment during experimental graft-versus-host disease. Blood 100:682–691
Kelly RM, Highfill SL, Panoskaltsis-Mortari A, Taylor PA, Boyd RL, Hollander GA, Blazar BR (2008) Keratinocyte growth factor and androgen blockade work in concert to protect against conditioning regimen-induced thymic epithelial damage and enhance T-cell reconstitution following murine bone marrow transplantation. Blood 111(12):5734–5744
Finch PW, Rubin JS (2006) Keratinocyte growth factor expression and activity in cancer: implications for use in patients with solid tumors. J Natl Cancer Inst 98:812–824
Moore TA, Zlotnik A (1997) Differential effects of Flk-2/Flt-3 ligand and stem cell factor on murine thymic progenitor cells. J Immunol 158:4187–4192
Ceredig R, Rauch M, Balciunaite G, Rolink AG (2006) Increasing Flt3L availability alters composition of a novel bone marrow lymphoid progenitor compartment. Blood 108:1216–1222
Karsunky H, Merad M, Cozzio A, Weissman IL, Manz MG (2003) Flt3 ligand regulates dendritic cell development from Flt3+ lymphoid and myeloid-committed progenitors to Flt3+ dendritic cells in vivo. J Exp Med 198:305–313
Lyman SD, Jacobsen SE (1998) c-kit ligand and Flt3 ligand: stem/progenitor cell factors with overlapping yet distinct activities. Blood 91:1101–1134
Ramsfjell V, Borge OJ, Veiby OP, Cardier J, Murphy MJ Jr, Lyman SD, Lok S, Jacobsen SE (1996) Thrombopoietin, but not erythropoietin, directly stimulates multilineage growth of primitive murine bone marrow progenitor cells in synergy with early acting cytokines: distinct interactions with the ligands for c-kit and FLT3. Blood 88:4481–4492
Veiby OP, Lyman SD, Jacobsen SE (1996) Combined signaling through interleukin-7 receptors and flt3 but not c-kit potently and selectively promotes B-cell commitment and differentiation from uncommitted murine bone marrow progenitor cells. Blood 88:1256–1265
Wodnar-Filipowicz A (2003) Flt3 ligand: role in control of hematopoietic and immune functions of the bone marrow. News Physiol Sci 18:247–251
Mackarehtschian K, Hardin JD, Moore KA, Boast S, Goff SP, Lemischka IR (1995) Targeted disruption of the flk2/flt3 gene leads to deficiencies in primitive hematopoietic progenitors. Immunity 3:147–161
McKenna HJ, Stocking KL, Miller RE, Brasel K, De Smedt T, Maraskovsky E, Maliszewski CR, Lynch DH, Smith J, Pulendran B, Roux ER, Teepe M, Lyman SD, Peschon JJ (2000) Mice lacking flt3 ligand have deficient hematopoiesis affecting hematopoietic progenitor cells, dendritic cells, and natural killer cells. Blood 95:3489–3497
Streeter PR, Dudley LZ, Fleming WH (2003) Activation of the G-CSF and Flt-3 receptors protects hematopoietic stem cells from lethal irradiation. Exp Hematol 31:1119–1125
MacDonald KP, Rowe V, Filippich C, Thomas R, Clouston AD, Welply JK, Hart DN, Ferrara JL, Hill GR (2003) Donor pretreatment with progenipoietin-1 is superior to granulocyte colony-stimulating factor in preventing graft-versus-host disease after allogeneic stem cell transplantation. Blood 101:2033–2042
Fry TJ, Sinha M, Milliron M, Chu YW, Kapoor V, Gress RE, Thomas E, Mackall CL (2004) Flt3 ligand enhances thymic-dependent and thymic-independent immune reconstitution. Blood 104:2794–2800
Wils EJ, Braakman E, Verjans GM, Rombouts EJ, Broers AE, Niesters HG, Wagemaker G, Staal FJ, Lowenberg B, Spits H, Cornelissen JJ (2007) Flt3 ligand expands lymphoid progenitors prior to recovery of thymopoiesis and accelerates T cell reconstitution after bone marrow transplantation. J Immunol 178:3551–3557
Sambandam A, Maillard I, Zediak VP, Xu L, Gerstein RM, Aster JC, Pear WS, Bhandoola A (2005) Notch signaling controls the generation and differentiation of early T lineage progenitors. Nat Immunol 6:663–670
Sitnicka E, Bryder D, Theilgaard-Monch K, Buza-Vidas N, Adolfsson J, Jacobsen SE (2002) Key role of flt3 ligand in regulation of the common lymphoid progenitor but not in maintenance of the hematopoietic stem cell pool. Immunity 17:463–472
Schwarz BA, Sambandam A, Maillard I, Harman BC, Love PE, Bhandoola A (2007) Selective thymus settling regulated by cytokine and chemokine receptors. J Immunol 178:2008–2017
Bertho JM, Chapel A, Loilleux S, Frick J, Aigueperse J, Gorin NC, Gourmelon P (2000) CD135 (Flk2/Flt3) expression by human thymocytes delineates a possible role of FLT3-ligand in T-cell precursor proliferation and differentiation. Scand J Immunol 52:53–61
Kikushige Y, Yoshimoto G, Miyamoto T, Iino T, Mori Y, Iwasaki H, Niiro H, Takenaka K, Nagafuji K, Harada M, Ishikawa F, Akashi K (2008) Human Flt3 is expressed at the hematopoietic stem cell and the granulocyte/macrophage progenitor stages to maintain cell survival. J Immunol 180:7358–7367
Mitsiadis TA, Barrandon O, Rochat A, Barrandon Y, De Bari C (2007) Stem cell niches in mammals. Exp Cell Res 313:3377–3385
Moore KA, Lemischka IR (2006) Stem cells and their niches. Science 311:1880–1885
Carlson ME, Conboy IM (2007) Loss of stem cell regenerative capacity within aged niches. Aging Cell 6:371–382
Chidgey A, Dudakov J, Seach N, Boyd R (2007) Impact of niche aging on thymic regeneration and immune reconstitution. Semin Immunol 19:331–340
Mayhall EA, Paffett-Lugassy N, Zon LI (2004) The clinical potential of stem cells. Curr Opin Cell Biol 16:713–720
Ryu BY, Orwig KE, Oatley JM, Avarbock MR, Brinster RL (2006) Effects of aging and niche microenvironment on spermatogonial stem cell self-renewal. Stem Cells 24:1505–1511
Bennett AR, Farley A, Blair NF, Gordon J, Sharp L, Blackburn CC (2002) Identification and characterization of thymic epithelial progenitor cells. Immunity 16:803–814
Gill J, Malin M, Hollander GA, Boyd R (2002) Generation of a complete thymic microenvironment by MTS24(+) thymic epithelial cells. Nat Immunol 3:635–642
Rossi SW, Jenkinson WE, Anderson G, Jenkinson EJ (2006) Clonal analysis reveals a common progenitor for thymic cortical and medullary epithelium. Nature 441:988–991
Bleul CC, Corbeaux T, Reuter A, Fisch P, Monting JS, Boehm T (2006) Formation of a functional thymus initiated by a postnatal epithelial progenitor cell. Nature 441:992–996
Godfrey DI, Izon DJ, Tucek CL, Wilson TJ, Boyd RL (1990) The phenotypic heterogeneity of mouse thymic stromal cells. Immunology 70:66–74
Depreter MG, Blair NF, Gaskell TL, Nowell CS, Davern K, Pagliocca A, Stenhouse FH, Farley AM, Fraser A, Vrana J, Robertson K, Morahan G, Tomlinson SR, Blackburn CC (2008) Identification of Plet-1 as a specific marker of early thymic epithelial progenitor cells. Proc Natl Acad Sci USA 105(3):961–966
Rossi SW, Chidgey AP, Parnell SM, Jenkinson WE, Scott HS, Boyd RL, Jenkinson EJ, Anderson G (2007) Redefining epithelial progenitor potential in the developing thymus. Eur J Immunol 37:2411–2418
Gillard GO, Farr AG (2006) Features of medullary thymic epithelium implicate postnatal development in maintaining epithelial heterogeneity and tissue-restricted antigen expression. J Immunol 176:5815–5824
Clark RA, Yamanaka K, Bai M, Dowgiert R, Kupper TS (2005) Human skin cells support thymus-independent T cell development. J Clin Invest 115:3239–3249
Poznansky MC, Evans RH, Foxall RB, Olszak IT, Piascik AH, Hartman KE, Brander C, Meyer TH, Pykett MJ, Chabner KT, Kalams SA, Rosenzweig M, Scadden DT (2000) Efficient generation of human T cells from a tissue-engineered thymic organoid. Nat Biotechnol 18:729–734
Lokmic Z, Stillaert F, Morrison WA, Thompson EW, Mitchell GM (2007) An arteriovenous loop in a protected space generates a permanent, highly vascular, tissue-engineered construct. Faseb J 21:511–522
Mian R, Morrison WA, Hurley JV, Penington AJ, Romeo R, Tanaka Y, Knight KR (2000) Formation of new tissue from an arteriovenous loop in the absence of added extracellular matrix. Tissue Eng 6:595–603
Chidgey AP, Layton D, Trounson A, Boyd RL (2008) Tolerance strategies for stem-cell-based therapies. Nature 453:330–337
Ilancheran S, Michalska A, Peh G, Wallace EM, Pera M, Manuelpillai U (2007) Stem cells derived from human fetal membranes display multilineage differentiation potential. Biol Reprod 77:577–588
Takahashi K, Yamanaka S (2006) Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell 126:663–676
Acknowledgements
We acknowledge generous research support from the Australian Stem Cell Centre, the National Health and Medical Research Council of Australia and Norwood Immunology.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chidgey, A.P., Seach, N., Dudakov, J. et al. Strategies for reconstituting and boosting T cell-based immunity following haematopoietic stem cell transplantation: pre-clinical and clinical approaches. Semin Immunopathol 30, 457–477 (2008). https://doi.org/10.1007/s00281-008-0140-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00281-008-0140-5