Abstract
Purpose
To determine the maximum tolerated dose (MTD) of BEZ235, an oral inhibitor of class I PI3K and mTOR complexes 1 and 2.
Methods
We performed a phase I/Ib, multicenter, open-label study of oral BEZ235 administered in a continuous daily schedule. The study consisted of two parts: dose-escalation part and safety-expansion part. BEZ235 was administered as a single agent to patients with solid tumors or in combination with trastuzumab for HER2+ advanced breast cancer (aBC). Primary end points were MTD, safety, and tolerability. The secondary end point was pharmacokinetics. Other formulations of BEZ235, solid dispersion system (SDS) sachet, and SDS capsules were also assessed.
Results
One hundred and eighty-three patients were enrolled; single-agent BEZ235 was administered as hard gelatin capsule (n = 59), SDS capsules A and B (n = 33), and SDS sachet (n = 61), amongst which SDS sachet was chosen as the preferred formulation. The monotherapy MTD for capsule A and SDS sachet was determined to be 1000 and 1200 mg/day, respectively. Thirty patients with HER2+ aBC received BEZ235 in combination with trastuzumab. The MTD of BEZ235 in combination with trastuzumab was 600 mg/day. A total of four patients (13.3%) achieved partial response across the different groups. Most frequent AEs in single agent and combination cohorts included nausea (80.3 and 93.3%), diarrhea (75.4 and 80.0%), and vomiting (63.9 and 63.3%).
Conclusions
The MTD of BEZ235 as single agent was 1200 and 600 mg/day with trastuzumab. Pharmacokinetic profiles showed low-to-moderate variability at low dose (10 mg) and high variability at high doses (100 mg and above). Gastrointestinal AEs were frequent at high doses.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The phosphatidylinositol-3-kinase (PI3K)/AKT/mammalian target of rapamycin (mTOR) pathway is frequently activated in cancer [1, 2]. PI3K pathway activation occurs during malignant growth in many ways, including aberrant activation of upstream receptor tyrosine kinases (RTKs), mutation of the gene encoding the class I PI3K catalytic subunit p110α (PIK3CA) or genes encoding downstream effectors, as well as functional disruption of the negative regulator phosphatase and tensin homolog (PTEN) [3]. The PI3K pathway plays a major role in tumor growth and progression, and resistance to anticancer therapies [3, 4] and is, therefore, a promising therapeutic target in patients with solid tumors, including HER2+ aBC, due to its central role in cancer development and resistance to therapy [5].
Dual inhibitors of both PI3K and mTORC1/2 suppress the PI3K pathway signaling both upstream and downstream of AKT. This comprehensive inhibition has been proposed to be more effective than inhibitors targeting a single node in the signaling pathway. In addition, specificity for both mTORC1 and mTORC2 has been shown to overcome feedback signaling arising from abolition of the mTORC1–S6K–IRS1 negative feedback loop, such as that typically observed in preclinical models with mTORC1 inhibitors [6].
BEZ235 (Novartis Pharmaceuticals Corporation, East Hanover, New Jersey, USA) is a potent, oral, ATP-competitive dual inhibitor of class I PI3K and its downstream effectors mTOR complex 1 and 2 (mTORC1/2) [7]. In cellular assays, BEZ235 is a more potent inhibitor of mTOR than PI3K [8]. mTOR inhibition predominates at a low concentration(< 100 nmol/L), but dual PI3K/mTOR blockade is observed at relatively higher concentrations (≈ 500 nmol/L) [8]. Many preclinical studies demonstrated that BEZ235 has antiproliferative, proapoptotic, and antiangiogenic activity [8,9,10,11].
In HER2+ breast cancer models, single-agent inhibition of the PI3K/AKT/mTOR pathway caused significant antiproliferative activity in HER2+ cell lines harboring PI3K mutations. It also overcame both de novo and acquired trastuzumab resistance in vitro and in vivo [12]. Furthermore, combined targeting of HER2 and PI3K/mTOR led to increased apoptosis in vitro and induction of tumor regression in trastuzumab-resistant xenograft models [12, 13]. These data support targeting of the PI3K/AKT/mTOR pathway in combination with trastuzumab in trastuzumab-resistant breast cancer.
BEZ235 has antitumor activity (both in monotherapy and in combination with other anticancer agents) in multiple preclinical cancer models including breast, colorectal, non-small cell lung cancer (NSCLC), ovarian and prostate cancer, and sarcomas [14,15,16,17,18,19]. Here, we report the results of the first-in-human, open-label, phase I/Ib study to determine the maximum tolerated dose (MTD) of BEZ235 when administered to adult patients with advanced solid tumors including patients with advanced breast cancer, as a single agent and in combination with trastuzumab (CBEZ235A2101/NCT00620594). We also describe the preliminary clinical exploration of BEZ235 formulations and dosage forms.
Patients and methods
Study design
We performed a phase I/Ib, multicenter, open-label study of oral BEZ235 administered in a continuous daily dosing schedule. The study consisted of two parts: a dose-escalation part and a safety-expansion part at the MTD. In both, BEZ235 was evaluated as a single agent in a cohort of solid tumors and in combination with trastuzumab in patients with HER2+ aBC.
Patient population
Patients with histologically confirmed advanced unresectable solid tumors failing standard therapy or for whom no standard therapy existed were eligible for the single-agent dose-escalation part of the study. Archival or fresh tumor biopsies for prescreening of molecular alterations affecting PIK3CA and/or PTEN expression were required for the single-agent safety expansion. For the combination part of the study, patients with histologically confirmed metastatic HER2+ aBC after failure of trastuzumab treatment (disease progression during trastuzumab maintenance given as adjuvant treatment or for metastatic disease) and with tumors carrying molecular alterations of PIK3CA and/or PTEN were eligible.
For all the study arms, patients were required to have ≥ 1 lesion as defined by Response Evaluation Criteria in Solid Tumors (RECIST) v1.0 [20]; age ≥ 18 years; World Health Organization (WHO) performance status ≤ 2; life expectancy ≥ 12 weeks. Adequate bone marrow, cardiac, hepatic, and renal functions were required. Key exclusion criteria included treatment with corticosteroids ≤ 2 weeks prior to starting study drug, diagnosis of diabetes mellitus or history of gestational diabetes, and prior treatment with a PI3K inhibitor.
The study was approved by the ethics committees of participating institutions and regulatory authorities, and all participating patients provided written informed consent and agreed to comply with the protocol. The study was conducted in accordance with the Declaration of Helsinki and guidelines for Good Clinical Practice as defined by the International Conference on Harmonization.
Study objectives
The objective of the dose-escalation part of the study was to establish the MTD of oral BEZ235 as a single agent or in combination with trastuzumab. The primary objective of the safety-expansion part of the study was to assess the safety and tolerability of BEZ235 (either as a single agent or in combination with trastuzumab) at the MTD. The safety expansion was conducted using a sachet formulation of BEZ235.
Secondary objectives of the safety expansion included assessment of safety and tolerability of BEZ235, pharmacokinetics (PK) profile of BEZ235 (either as a single agent or in combination with trastuzumab), and preliminary antitumor activity.
Study treatment
Patients received oral BEZ235 once daily, in continuous 28-day cycles until disease progression, unacceptable toxicity, or withdrawal of consent. For the combination arm, commercially available trastuzumab (Herceptin®; 2 mg/kg/week) was used. The initial BEZ235 service form was a hard gelatin capsule (HGC) formulation. The first dose level with this service form was 10 mg/day.
Four different BEZ235 formulations and service forms were assessed: BEZ235-tosylate in HGC formulation or BEZ235-vitamin E TPGS [d-α-tocopheryl polyethylene glycol 1000 succinate; capsule A (size 000), capsule B (size 0), sachet], also referred to as SDS formulation (solid dispersion system). Either HGC (single-agent arm of the study only) or SDS formulations (both the single-agent and combination arms) were administered orally once daily with the same schedule.
Maximum tolerated dose determination
Dose escalation was guided by the escalation with overdose control (EWOC) principle and modeled by an adaptive Bayesian logistic regression model (BLRM) [21, 22]. Cohorts of three-to-six patients were planned to be enrolled at each dose level. Cohorts could be expanded at any dose level below MTD for further elaboration of safety and PK parameters as required.
The final recommendation of dose and formulation was based on the BLRM and an overall assessment of safety. Estimation of MTD was based upon the probability of DLT in cycle 1 in patients in the dose-determining set (DDS). The objective of this design was to find the dose maximizing the probability that the true DLT rate lies in the interval of 16–33%. Any dose of BEZ235, which had > 25% chance of being in the excessive (DLT rate between 33 and 60%) or unacceptable (DLT rate of ≥ 60%) toxicity categories was excluded.
Safety and efficacy assessments
All patients who received ≥ 1 dose of study drug and had ≥ 1 post baseline safety assessment were eligible for safety evaluation. Routine clinical and laboratory assessments were conducted at baseline, weekly until day 22 of cycle 2, and then on days 1 and 15 of subsequent cycles.
Adverse events (AEs) were collected continuously from first dose of study treatment to at least 4 weeks following the last dose of study treatment, and graded using the National Cancer Institute’s Common Terminology Criteria for Adverse Events (NCI-CTCAE) v3.0.
Assessments of preliminary antitumor activity were performed in all patients who had received at least 1 dose of BEZ235. Radiologic response was assessed according to RECIST v1.0 after two cycles and every other cycle thereafter.
The metabolic antitumor activity of BEZ235 was assessed by positron emission tomography (PET) at baseline (≤ 14 days prior to study drug administration) and at the end of cycle 1 and cycle 2 (day 28, ± 2 days) according to the recommendations of the EORTC [23].
Pharmacokinetic assessments
Plasma levels of BEZ235 were determined from blood samples using validated liquid chromatography tandem mass spectrometry assay with a lower limit of quantification of approximately 1 ng/mL.
Pharmacokinetic plasma samples were collected before dosing on day 1 of every other cycle, starting on cycle 1 day 1 (C1D1). On the days which involved full PK sampling and fasting insulin/glucose monitoring (C1D1, C1D8, and C1D28), blood was collected before dosing and 1-, 2-, 4-, 6-, 8-, and 24-h post dose. After all patients had potentially completed at least 6 cycles of treatment, PK samples were no longer collected.
For the single-agent MTD expansion, a subset of ten patients fasted overnight for 10–12 h prior to the administration of BEZ235 on the days which involved full PK blood sampling (day 1 and 28 of cycle 1).
Biomarker and pharmacodynamic assessments
Fresh tumor biopsy samples were collected at baseline, day 28 of cycle 1 and at disease progression or end of study treatment. Biopsies were used for central assessment (single-agent dose escalation) and/or local assessment (single-agent safety and combination dose escalation and safety expansion) of the presence of PIK3CA activating mutation in exons 9 or 20 as determined by SNaPshot genotyping assay; and low or null PTEN expression, as defined by an immunohistochemistry H-score < 50. The effect of BEZ235 on Ki67, pAKT, pS6, PARP, p4EBP1, cyclin D1, and pERK levels was also assessed.
Statistical analysis
Descriptive statistics was used to summarize demographic characteristics and frequency counts for categorical variables. The DLT data from all patients enrolled in the dose-escalation part for estimation of MTDs and eligible for the dose-determining set were modeled via an adaptive BLRM. The dose escalation was guided by the EWOC principle. Analysis of variance (ANOVA) test was performed on log-transformed area under curve (AUC) and maximum concentration (Cmax) (cycle 1 days 1, 8, and 28) using a linear mixed-effect model to assess day effect, food intake status effect, and dose proportionality. Inter-individual and intraindividual variability in systemic exposures was assessed.
Results
A total of 183 patients were treated with BEZ235, as a single agent (n = 153) or in combination with trastuzumab (n = 30) between 2006 and 2013.
Pharmacokinetics and exploration of the BEZ235 formulation
Fifty-nine patients received single-agent BEZ235 as an HGC. The HGC formulation was explored either under fasted (BEZ235 Fast, N = 41) or fed (BEZ235 Fed, N = 18) conditions. Pharmacokinetic parameters of patients on BEZ235 HGC formulation are summarized in Supplementary Table 1A. At doses < 25 mg, BEZ235 exhibited low–moderate variability (CV% = 24.8 for the 10-mg dose), while at doses ≥ 100 mg, high variability was observed (CV% > 100 for most doses). The administration of food increased the exposure to BEZ235 at 300–400 mg/day vs fasted conditions at same dose levels. Under fed condition, on day 8 and day 28, the adjusted geometric mean ratio also showed a trend towards higher exposure. However, firm conclusions could not be drawn for high doses ≥ 100 mg owing to large variability in the data with no statistically significant differences. Further investigation of the HGC formulation for doses ≥ 100 mg was discontinued due to low exposure and high inter-patient and intra-patient variability in PK profiles (Supplementary Table 1A), and safety issues related to a lack of absorption and precipitation. The MTD of the HGC formulation was not reached (Table 1).
MTD was declared for single-agent BEZ235, for both the SDS capsule A and SDS sachet dosage forms at 1000 and 1200 mg/day, respectively. MTD of the SDS capsule B was not reached, as dose escalation of the SDS capsule B was terminated due to low drug exposure (Table 1).
Pharmacokinetic profiles for SDS capsule A showed a high inter-individual variability with a coefficient of variation greater than 100% on both AUC0–24 and Cmax at doses ≥ 400/day mg at steady state (Supplementary Table 1B). Tmax ranged between 4 and 6 h. The estimated accumulation, based on the ratio of AUC0–24 on day 8/day 28 over the AUC0–24 on day 1, 3.53 on day 8 and 4.78 on day 28, for the dose of 1000 mg/day.
Pharmacokinetic profiles for the single-agent BEZ235 SDS sachet (n = 61) showed decreased absorption rate with a delayed Tmax, but the inter-patient variability in exposure remained high in the SDS sachet formulation on the exposure at steady state (Supplementary Table 1B) for doses of ≥ 800 mg/day. For instance, a CV of 129% around the geometric mean was observed at the dose of 1200 mg/day on day 28, and no clear dose exposure relationship could be observed in the Cmax and AUC0–24. The inter-patient variability on Cmax was less pronounced with a corresponding variability of 81%.
In the cohort administered BEZ235 as SDS capsule B, the variability in exposure remained high, and the absorption was relatively slow with a Tmax of approximately around 4 h similar to that of the previous formulations (Supplementary Table 1B). As the variability did not improve, it was considered that this dosage form did not bring additional value, and was, therefore, not investigated further. Overall, despite low-to-moderate variability of BEZ235 at a dose of 10 mg/day, the PK profiles of all formulations for doses ≥ 100 mg displayed a high degree of inter-patient and intra-patient variability, and were found to be similar across all the single-agent formulations (Supplementary Table 1A and 1B).
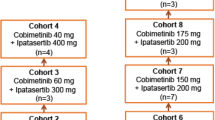
Dose escalation of BEZ235 in combination with trastuzumab began with the SDS capsule A dosage form (3 patients) and was continued with the SDS sachet formulation following the results of the single-agent dose escalation. The safety-expansion part of the combination arm of the study was completed with the SDS sachet at the declared MTD (Table 1). Mean PK profiles for the tested doses of 400–800 mg/day showed slow absorption rates and were highly variable, and no substantial differences were found among the doses tested (Supplementary Table 1C). Therefore, the results of the combination arm of the study included aggregate data of SDS capsule A and SDS sachet in combination with trastuzumab (Fig. 1).
Patients and treatments (to be re-drawn in high-res closer to submission). *Dose escalation started with SDS capsule A, and continued with SDS sachet. †MTD reached; however, the SDS capsule formulation was discontinued as it was difficult to swallow. HGC hard gelatin capsule, MTD maximum tolerated dose, SDS solid dispersion system
Safety and efficacy of single-agent BEZ235 arm
Patient characteristics
Eighty-three patients were treated with BEZ235 SDS capsule A (n = 22) and SDS sachet (n = 61). The most commonly represented tumor types were colon cancer and breast cancer. Most patients had received multiple prior lines of antineoplastic therapy (Table 2).
Dose escalation and maximum tolerated dose
BEZ235 HGC was administered at 9 dose levels (between 10 and 1200 mg/day) (Supplementary Table 1A). No DLT was observed and the MTD was not reached (Table 1).
BEZ235 SDS capsule A was administered at 3 doses between 400 and 1000 mg/day (Table 1). DLTs were observed in three patients: 1 at 800 mg/day and 2 at 1000 mg/day (Table 1). The MTD for the BEZ235 SDS capsule A was declared at 1000 mg/day based on the results of the BLRM and review of safety and tolerability (Supplementary Table 2).
BEZ235 SDS sachet was administered at 5 dose levels between 800 and 1600 mg/day, under fed conditions (Table 1). The SDS sachet treatment group included patients enrolled in the dose-escalation part and the MTD expansion part of the study (61 patients). Fifty patients met the criteria for inclusion in the DDS and were evaluable for MTD determination. Initially, the 800 mg/day dose was tested, and the BLRM allowed dose escalation to 1400 mg/day. One DLT was reported in the first cohort of four patients at 1400 mg/day, leading to a dose increase to 1600 mg/day (7 patients) in parallel with an extension of the 1400 mg/day cohort (3 additional patients). In these cohorts, one DLT was reported at 1400 mg/day and one DLT at 1600 mg/day.
To further understand the PK profile and safety near the MTD, subsequent enrollment of four patients at 1000 mg/day and six additional patients at 1400 mg/day revealed several additional DLTs: 1 at 1000 mg/day and 4 at 1400 mg/day (for a total of 6 at 1400 mg/day; Table 1), surpassing the criteria for MTD declaration. The recommendation of the BLRM was to reduce the dose back to 1000 mg/day; six patients were enrolled with no DLT reported. Dose escalation was continued with seven patients at 1200 mg/day, where two DLTs were reported (grade 3 vomiting and grade 2 nausea). According to the results of the BLRM and review of safety and tolerability, the MTD was estimated to be 1200 mg/day (Supplementary Table 2).
The SDS sachet was chosen as the preferred single-agent dosage form based on convenience of administration for oncology indications. In addition, there was no apparent difference in PK profiles between the capsule A and the sachet dosage forms.
Safety and tolerability of BEZ235 at doses near the MTD
BEZ235 HGC at doses > 25-mg daily was poorly tolerated due to gastrointestinal side effects most likely related to a lack of absorption and precipitation of the drug substance at high doses. BEZ235 HGC, SDS capsule A and B and SDS sachet had similar safety profiles, and as the SDS sachet was selected as the preferred formulation for further study (Table 3), safety and efficacy data focused on the 61 patients treated with BEZ235 SDS sachet. The most frequently reported AEs with BEZ235 SDS sachet were nausea (80.3%), diarrhea (75.4%), and vomiting (63.9%) (Table 3). Of the 24 patients treated with BEZ235 at the MTD level of 1200 mg/day, 2 patients (8.3%) experienced AEs leading to treatment discontinuation. Grade 3 or 4 AEs regardless of study drug relationship were experienced by 68.9% of patients (Table 3). The median duration of BEZ235 SDS sachet exposure was 8.0 weeks (range 1.9–48.0). At the data cutoff (January 8, 2013), all 61 patients had discontinued treatment, primarily due to disease progression (72.1% of patients; Supplementary Table 3). Three patients died within 28 days of last study treatment (Supplementary Table 3), all due to disease progression. No deaths were suspected to be related to study drug.
Antitumor activity
Best overall response per investigator assessment of BEZ235 as a single agent and in combination with trastuzumab is represented in Table 5. Stable disease (SD) was the best overall response achieved in 19 patients (31.1%; Table 5) in the SDS sachet cohort. At the MTD (1200 mg/day), 10 patients had a best overall response of SD (Fig. 2a), and disease control was observed in 10 patients (41.7%; 90% CI 24.6–60.3). Of these 10 patients, 3 had PTEN null/low expression, and 7 did not show any PI3K pathway alteration in the tumor tissue, based on central assessment (Fig. 2a).
Best percentage change and best overall response by investigator assessment. a Single-agent BEZ235 SDS sachet (to be re-drawn in high-res closer to submission). Patients with missing best percentage change from baseline and unknown overall response are not included. Missing line denotes a missing best percent change from baseline. UNK indicates patients not qualifying for confirmed CR or PR and without SD after more than 6 weeks or early progression within the first 12 weeks. b BEZ235 in combination with trastuzumab (to be re-drawn in high-res closer to submission). Patients with missing best percentage change from baseline and unknown overall response are not included. UNK indicates patients not qualifying for confirmed CR or PR and without SD after more than 6 weeks or early progression within the first 12 weeks
Biomarker studies
Data from paired tumor biopsies at cycle 1 day 28, in three patients treated with HGC formulation showed a decrease in pS6 levels from baseline with a median decrease of − 23.08% (range − 59.2 to − 15.0). None of the analyzed biomarkers from paired biopsies showed any correlation to response (Supplementary Table 4).
Safety and efficacy of BEZ235 in combination with trastuzumab arm
Patient characteristics
In the combination cohort, 30 patients with HER2+ breast cancer were treated with BEZ235 SDS capsule A (n = 3) and SDS sachet (n = 27) in combination with trastuzumab (Table 2). These patients were heavily pretreated with a median number of 7 (range 4–14) prior antineoplastic regimens.
Dose escalation and maximum tolerated dose
The first three patients were treated with SDS capsule A, and the following cohorts of patients were treated with BEZ235 SDS sachet based on findings from the single-agent arm of the study. Therefore, MTD of the BEZ235 capsule A in combination with trastuzumab was not determined.
The SDS sachet treatment group included patients who were enrolled in the dose-escalation part and the MTD expansion part of the study (Table 1). DLTs were observed in 4 patients: 3 of 6 patients at 800 mg/day and 1 of 16 patients at 600 mg/day. The MTD for BEZ235 sachet in combination with trastuzumab (2 mg/kg/week) was declared at 600 mg/day based on the BLRM and review of safety and tolerability (Supplementary Table 2). The safety expansion of BEZ235 SDS sachet in combination with trastuzumab was completed at this dose level without further DLT.
Safety and tolerability
Safety and tolerability data for the combination cohort are presented in Table 4. The most frequently reported AEs included nausea (93.3%), diarrhea (80.0%), and vomiting (63.3%). Of the 17 patients treated with BEZ235 at the MTD of 600 mg/day, the median duration of exposure was 8.3 weeks (range 1.4–48.0). All 30 patients in the combination cohort discontinued treatment, primarily due to disease progression (73.3% of patients; Supplementary Table 3). A total of three deaths were reported; two of which occurred within 28 days of last study treatment (Supplementary Table 3). All deaths were assessed to be due to disease progression.
Antitumor activity
Response outcome as per investigator review was available for all 30 patients who received BEZ235 in combination with trastuzumab. Partial response (PR) was the best overall response observed, achieved by four patients (13.3%; Table 5). Of the 17 patients treated at the MTD (600 mg/day), 2 patients had a PR and 6 had SD as best response (Fig. 2b). The disease control rate was 47.1% (90% CI 26.0–68.9). Brain scans of a patient with 400-mg/day SDS capsule A in combination with trastuzumab showed a reduction in two brain metastatic lesions of 34.2 and 36.4% (Supplementary Fig. 2).
All patients enrolled in the combination arm were required to have tumors with a PI3K pathway alteration, identified by either local or central assessment. However, local results were not confirmed by central assessment of tumor tissue from four patients with a PR (Fig. 2b). Two of these patients were enrolled based on locally assessed PTEN null/low expression, and two based on locally assessed PIK3CA mutation.
Pharmacokinetic studies
As in BEZ235 single-agent cohorts, pharmacokinetics of BEZ235 SDS at 400–800 mg/day in combination with trastuzumab displayed high inter-patient variability, and there was no substantial difference in Cmax between the doses tested. Absorption rate was slow with a delayed Tmax (Supplementary Table 1C).
Discussion
Preclinical data from in vivo and in vitro studies [14,15,16,17,18,19] supported the development of BEZ235 as a promising candidate to assess in a phase I clinical trial in patients with advanced solid tumors. The MTD was reached for capsule A and SDS sachet, and the sachet dosage form was chosen based on ease of administration. The single-agent safety expansion was completed with BEZ235 SDS sachet at the MTD (1200 mg/day), and the safety expansion for the combination arm of the study was completed with BEZ235 SDS sachet at the MTD (600 mg/day + trastuzumab). The RP2D of single-agent BEZ235 SDS sachet was chosen to be 1000 mg/day. Although the 10-mg/day dose of BEZ235 exhibited low–moderate variability, with the caveat that the cohort size was small (Supplementary Table 1A), there was a high degree of PK variability in the systemic exposure profile of BEZ235 at doses ≥ 100-mg/day BEZ235. This variability in the PK data led to the exploration of different modes of administration of BEZ235 for doses ≥ 100 mg/day in relation with food and different formulations. Preclinical PK studies in dogs had indicated that administration of BEZ235 with food increased systemic exposure. A food effect study in healthy male volunteers also showed a slight improvement of variability and degree of exposure to BEZ235 under fed conditions [24]. In addition, data from a previous trial showed that administration of BEZ235 with a high-fat meal slightly improved the variability and degree of exposure compared with fasting conditions. For these reasons, patients in our study were administered HGC under both fasted and fed conditions to examine whether food affected the exposure to BEZ235. However, no firm conclusions could be drawn from the analyses. Thus, investigation of the HGC formulation for BEZ235 doses ≥ 100 mg/day was discontinued due to PK variability. Furthermore, the formulation of BEZ235 evolved during the trial in response to observed PK data and based on the results of a healthy volunteers study conducted in parallel. Solid dispersion system (SDS) is a type of special delivery approach designed to improve the bioavailability of poorly water-soluble drugs. This method involves formation of eutectic mixtures of drugs with water-soluble carriers by the melting of their physical mixtures [25]. Different formulations of BEZ235 employing the SDS technique also were studied in patients with advanced solid tumors. However, across all formulations and dosage forms ≥ 100 mg tested, BEZ235 displayed low bioavailability, with a moderate absorption rate, a less than proportional increase in exposure, and large inter-patient and intra-patient variability. In contrast, doses < 25 mg formulated in HGC exhibited PK properties potentially acceptable for further development in non-oncology indications, where full target inhibition would not be necessary.
Adverse effects in the single-agent arm and in the combination treatment arm were similar to each other and to those observed with the different formulations in the single-agent arm of the study. The most frequently reported events for BEZ235 ≥ 400 mg/day in both the single-agent and the combination treatment arms, were nausea, diarrhea, and vomiting. The onset of these AEs was typically reported within a short period of time after dosing, suggesting that these were caused by low absorption and precipitation of the drug at high doses, and not by mechanism-based toxicities. Notably, hyperglycemia and rash, AEs that are typically associated with PI3K inhibition, and pneumonitis, an mTOR-related toxicity, were not prevalent in this study; however, the incidence of stomatitis, another mTOR-related toxicity, was near to that seen with the allosteric mTOR inhibitor everolimus (59–71%) in solid tumors [26].
Clinical activity of BEZ235 was observed, both as a single agent and in combination with trastuzumab. Despite exposure variability at doses ≥ 100-mg/day BEZ235, 5 patients (2.7%) experienced PR and 62 patients (33.9%) achieved SD as best overall response. The lack of robust antitumor effect may have been due to the fact that BEZ235 is a more potent inhibitor of mTOR than PI3K in vivo [8]. Therefore, sufficient BEZ235 exposure to consistently inhibit PI3K may not have been achieved in patients due to exposure variability at doses ≥ 100 mg/day. In addition, definitive conclusions could not be drawn about the role of PI3K pathway alterations (ie, PIK3CA and PTEN status) as predictive markers of sensitivity to BEZ235. Limitations were due to sample size, discrepancies in local vs central assessment of PI3K pathway activation status, and inconsistencies in tumor sample amount and quality. The challenges observed in the translational aspects of this study underscored the need for a robust companion diagnostic assay if pathway alterations were proven to correlate with drug responses and dual PI3K/mTOR inhibitors were to gain regulatory approval.
In summary, although robust preclinical data supported development of BEZ235, the more potent inhibition of mTOR than PI3K in cellular assays, and the highly variable PK profile of BEZ235 at doses ≥ 100 mg/day led to discontinuation of further development in oncology indications. The results of the present study indicate that PI3K/mTOR inhibition by BEZ235 in advanced solid tumors, including breast cancer, was not sufficient to achieve an adequate antitumor effect with a favorable safety profile.
References
Liu P, Cheng H, Roberts TM, Zhao JJ (2009) Targeting the phosphoinositide 3-kinase pathway in cancer. Nat Rev Drug Discov 8:627–644
Brachmann S, Fritsch C, Maira SM, Garcia-Echeverria C (2009) PI3K and mTOR inhibitors: a new generation of targeted anticancer agents. Curr Opin Cell Biol 21:194–198
Miller TW, Balko JM, Arteaga CL (2011) Phosphatidylinositol 3-kinase and antiestrogen resistance in breast cancer. J Clin Oncol 29:4452–4461
Burris HA III (2013) Overcoming acquired resistance to anticancer therapy: focus on the PI3K/AKT/mTOR pathway. Cancer Chemother Pharmacol 71:829–842
Huang WC, Hung MC (2009) Induction of Akt activity by chemotherapy confers acquired resistance. J Formos Med Assoc 108:180–194
O’Reilly KE, Rojo F, She QB, Solit D, Mills GB, Smith D, Lane H, Hofmann F, Hicklin DJ, Ludwig DL, Baselga J, Rosen N (2006) mTOR inhibition induces upstream receptor tyrosine kinase signaling and activates Akt. Cancer Res 66:1500–1508
Maira SM, Stauffer F, Brueggen J, Furet P, Schnell C, Fritsch C, Brachmann S, Chene P, De Pover A, Schoemaker K, Fabbro D, Gabriel D, Simonen M, Murphy L, Finan P, Sellers W, Garcia-Echeverria C (2008) Identification and characterization of NVP-BEZ235, a new orally available dual phosphatidylinositol 3-kinase/mammalian target of rapamycin inhibitor with potent in vivo antitumor activity. Mol Cancer Ther 7:1851–1863
Serra V, Markman B, Scaltriti M, Eichhorn PJ, Valero V, Guzman M, Botero ML, Llonch E, Atzori F, Di Cosimo D, Maira M, Garcia-Echeverria C, Parra JL, Arribas J, Baselga J (2008) NVP-BEZ235, a dual PI3K/mTOR inhibitor, prevents PI3K signaling and inhibits the growth of cancer cells with activating PI3K mutations. Cancer Res 68:8022–8030
Schnell CR, Stauffer F, Allegrini PR, O’Reilly T, McSheehy PM, Dartois C, Stumm M, Cozens R, Littlewood-Evans A, Garcia-Echeverria C, Maira SM (2008) Effects of the dual phosphatidylinositol 3-kinase/mammalian target of rapamycin inhibitor NVP-BEZ235 on the tumor vasculature: implications for clinical imaging. Cancer Res 68:6598–6607
Awasthi N, Yen PL, Schwarz MA, Schwarz RE (2012) The efficacy of a novel, dual PI3K/mTOR inhibitor NVP-BEZ235 to enhance chemotherapy and antiangiogenic response in pancreatic cancer. J Cell Biochem 113:784–791
Brachmann SM, Hofmann I, Schnell C, Fritsch C, Wee S, Lane H, Wang S, Garcia-Echeverria C, Maira SM (2009) Specific apoptosis induction by the dual PI3K/mTOR inhibitor NVP-BEZ235 in HER2 amplified and PIK3CA mutant breast cancer cells. Proc Natl Acad Sci USA 106:22299–22304
O’Brien NA, McDonald K, Tong L, von Euw E, Kalous O, Conklin D, Hurvitz SA, di Tomaso E, Schnell C, Linnartz R, Finn RS, Hirawat S, Slamon DJ (2014) Targeting PI3K/mTOR overcomes resistance to HER2-targeted therapy independent of feedback activation of AKT. Clin Cancer Res 20:3507–3520
Rexer BN, Chanthaphaychith S, Dahlman KB, Arteaga CL (2014) Direct inhibition of PI3K in combination with dual HER2 inhibitors is required for optimal antitumor activity in HER2+ breast cancer cells. Breast Cancer Res 16:R9
Roper J, Richardson MP, Wang WV, Richard LG, Chen W, Coffee EM, Sinnamon MJ, Lee L, Chen PC, Bronson RT, Martin ES, Hung KE (2011) The dual PI3K/mTOR inhibitor NVP-BEZ235 induces tumor regression in a genetically engineered mouse model of PIK3CA wild-type colorectal cancer. PLoS One 6(9):e25132
Santiskulvong C, Konecny GE, Fekete M, Chen KY, Karam A, Mulholland D, Eng C, Wu H, Song M, Dorigo O (2011) Dual targeting of phosphoinositide 3-kinase and mammalian target of rapamycin using NVP-BEZ235 as a novel therapeutic approach in human ovarian carcinoma. Clin Cancer Res 17:2373–2384
Piao J, Chen L, Quan T, Li L, Quan C, Piao Y, Jin T, Lin Z (2016) Superior efficacy of co-treatment with the dual PI3K/mTOR inhibitor BEZ235 and histone deacetylase inhibitor Trichostatin A against NSCLC. Oncotarget 7:60169–60180
Manara MC, Nicoletti G, Zambelli D, Ventura S, Guerzoni C, Landuzzi L, Lollini PL, Maira SM, García-Echeverría C, Mercuri M, Picci P, Scotlandi K (2010) NVP-BEZ235 as a new therapeutic option for sarcomas. Clin Cancer Res 16:530–540
Hong SW, Shin JS, Moon JH, Kim YS, Lee J, Choi EK, Ha SH, Lee DH, Chung HN, Kim JE, Kim KP, Hong YS, Lee JL, Lee WJ, Choi EK, Lee JS, Jin DH, Kim TW (2014) NVP-BEZ235, a dual PI3K/mTOR inhibitor, induces cell death through alternate routes in prostate cancer cells depending on the PTEN genotype. Apoptosis 19:895–904
Dey N, Sun Y, Carlson JH, Wu H, Lin X, Leyland-Jones B, De P (2016) Anti-tumor efficacy of BEZ235 is complemented by its anti-angiogenic effects via downregulation of PI3K-mTOR-HIF1alpha signaling in HER2-defined breast cancers. Am J Cancer Res 6:714–716
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92:205–216
Babb J, Rogatko A, Zacks S (1998) Cancer phase I clinical trials: efficient dose escalation with overdose control. Stat Med 17:1103–1120
Neuenschwander B, Branson M, Gsponer T (2008) Critical aspects of the Bayesian approach to phase I cancer trials. Stat Med 27:2420–2439
Young H, Baum R, Cremerius U, Herholz K, Hoekstra O, Lammertsma AA, Pruim J, Price P (1999) Measurement of clinical and subclinical tumour response using [18F]-fluorodeoxyglucose and positron emission tomography: review and 1999 EORTC recommendations. European Organization for Research and Treatment of Cancer (EORTC) PET Study Group. Eur J Cancer 35:1773–1782
Rodon J, Infante J, Burris H, Tabernero J, Ranson MR, Rouyrre N, Duval V, Silva A, Hackl W, Baselga J (2010) A dose-escalation study with a special drug delivery system (SDS) of BEZ235, a novel dual PI3K/mTOR inhibitor, in patients with metastatic/advanced solid tumors SABCS. Abstract #.P6-15-07
Serajuddin AT (1999) Solid dispersion of poorly water-soluble drugs: early promises, subsequent problems, and recent breakthroughs. J Pharm Sci 88(10):1058–106626
Rugo HS, Hortobagyi GN, Yao J, Pavel M, Ravaud A, Franz D, Ringeisen F, Gallo J, Rouyrre N, Anak O, Motzer R (2016) Meta-analysis of stomatitis in clinical studies of everolimus: incidence and relationship with effciacy. Ann Oncol 27:519–525
Acknowledgements
We thank the patients who participated in this trial and their families, as well as staff members at individual trial centers who provided support; Amirtha Ganesh, PhD and Avinash Yerramsetti (Novartis Healthcare Pvt Ltd) for providing medical editorial assistance with this manuscript.
Funding
The study was initiated, funded, and sponsored by Novartis Pharmaceuticals Corporation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J. Rodon reports grants and personal fees from Novartis during the conduct of the study; grants from Bayer and personal fees from Peptomyc, Orion, and Servier outside the submitted work. I. Krop reports personal fees from Genentech/Roche, Daiichi/Sankyo and Macrogenics outside the submitted work; research grants from Genentech/Roche. H. Burris reports other fees Novartis during the conduct of the study. C. Britten reports grants from Novartis during the conduct of the study; grants from Amgen, Boston Biomedical, Eli Lilly, Five Prime, Plexxikon, Keystone Nano, EMD Serono, Roche, Tesaro, Regeneron, Pfizer and Halozyme outside the submitted work; non-financial support from Five Prime; personal fees from Cleave outside the submitted work. M. Schuler reports other fees from University Hospital Essen, University Duisburg-Essen and Ruhrlandklinik outside the submitted work; personal fees from AstraZeneca, Celgene, Roche, Abbvie, Eli Lilly, Alexion, and MSD outside the submitted work; personal fees and grants from Boehringer Ingelheim, Bristol-Myers Squibb, and Novartis outside the submitted work. M. Abu-Khalaf reports grants from Novartis during the conduct of the study and outside the submitted work. A. Silva is employee of Novartis Pharma AG and hold Novartis stock options. W. Hackl is employee of Novartis Pharma AG and hold Novartis stock options. C. Quadt is employee of Novartis Pharma AG and hold Novartis stock options. D. Demanse is employee of Novartis Pharma AG. V. Duval is employee of Novartis Pharma AG. A. Pérez-Fidalgo, A. Guerrero-Zotano, C. Becerra, sJ. Schellens, D. Richards, F. Johnson, M. Ranson, J. Edenfield and J. Baselga have nothing to disclose.
Ethical approval
This study was conducted in accordance with Good Clinical Practice guidelines and the Declaration of Helsinki. An independent ethics committee and institutional review boards approved the study protocol and any subsequent amendments at each participating center. A study steering committee monitored study conduct in line with the protocol.
Informed consent
Written informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rodon, J., Pérez-Fidalgo, A., Krop, I.E. et al. Phase 1/1b dose escalation and expansion study of BEZ235, a dual PI3K/mTOR inhibitor, in patients with advanced solid tumors including patients with advanced breast cancer. Cancer Chemother Pharmacol 82, 285–298 (2018). https://doi.org/10.1007/s00280-018-3610-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-018-3610-z