Summary
Introduction The PI3 kinase (PI3K) pathway is a commonly dysregulated pathway in cancers and is an attractive target for antitumor therapy. BEZ235 is a potent, highly specific and selective dual PI3K/mTOR inhibitor. Methods Patients were enrolled in a 3 + 3 dose escalation design to determine the maximum tolerated dose (MTD), toxicities, and pharmacokinetics (PK) of BEZ235 when administered twice-daily as an oral sachet. For intrapatient PK comparison, patients were to receive a lead in of the total daily dose in a QD schedule for the first 8 days of the initial 28 day cycle. Patients continued treatment until unacceptable toxicity or disease progression occurred. Results Thirty-three patients received BEZ235. Initial dose levels of 200 and 400 mg BID had no DLTs. At the 600 mg BID dose level with 1200 mg QD lead in dose two DLTs of grade 3 mucositis occurred early in the first treatment cycle, the lead-in QD dosing was eliminated. Fatigue and mucositis limited dosing at 600 mg BID in subsequent patients. The 400 mg BID dose level was re-explored, with DLTs of grade 3 hyperglycemia, dehydration, fatigue, and grade 3 thrombocytopenia. Twelve patients were enrolled at an intermediate dose of 300 mg BID; a grade 3 mucositis DLT was reported in 1 patient, and this dose was declared the MTD. Preliminary PK data demonstrate a consistent increase in PK parameters (Cmax and AUC) with dose level compared to QD dosing. Fifteen patients experienced stable disease as their best response, including 10 (colorectal [4 patients], endometrial [3 patients], carcinoid NOS, pancreas, and melanoma) who had disease control for ≥16 weeks. Conclusions The recommended dose of BEZ235 administered BID as an oral sachet formulation is 300 mg BID. Toxicities seen have been reported for other dual PI3K/mTOR inhibitors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The PI3K/Akt/mTOR pathway is important in the regulation of cellular growth, proliferation, survival, and apoptosis. With aberrant activation observed in approximately 30–50 % of tumors, the PI3K/Akt/mTOR pathway is likely the most frequently activated pathway in human cancer [1–3]. PI3K mutations are frequently described in breast, ovarian, brain, stomach, and colorectal cancers, while loss of PTEN mutations, which also cause PI3K activation, are seen in melanoma, prostate, brain, and endometrial cancers [4–6].
As this pathway is an attractive target for cancer treatment, numerous agents have been developed. BEZ235 (Novartis) is a potent, highly specific and selective inhibitor of class I PI3K, which also inhibits both mTORC complexes (mTORC1 and mTORC2). The first-in-human study of BEZ235 utilized a hard gelatin capsule formulation for daily dosing [7]. There were no dose-limiting toxicities (DLTs), the safety profile was acceptable, and partial responses were seen. However, inter-patient pharmacokinetic (PK) variability and low bioavailability lead to the development of other formulations. Several formulations of BEZ235 were evaluated in the subsequent phase 1/1b trial: hard gelatin capsule, two special drug delivery system (SDS) capsule formulations (A and B, which varied by size and BEZ235 content), and an SDS sachet [8]. The hard gelatin capsule and SDS capsule A showed very high inter-patient variability, while PK of the SDS sachet was more consistent across patients. The MTD for once-daily administration of the SDS sachet formulation was 1600 mg/day, with dose-limiting grade 3 fatigue and grade 3 thrombocytopenia.
The poor solubility of BEZ235 is attributed to its pH higher than 4, which limits dissolution and absorption in the gastrointestinal tract. Splitting the SDS sachet dose into a twice daily (BID) regimen was anticipated to allow for improved daily exposures, thereby maximizing target inhibition. The purpose of this phase 1 study was to determine the maximum tolerated dose (MTD), safety and pharmacokinetic (PK) profiles, and clinical activity of BEZ235 when administered BID as the SDS sachet formulation to patients with advanced solid tumors.
Methods
This study (NCT#01343498) was conducted in accordance with applicable regulatory guidelines, the International Conference on Harmonization Guidelines for Good Clinical Practice, and the Declaration of Helsinki. Institutional review boards at both participating sites (Tennessee Oncology, PLLC, Nashville, TN; Stephenson Cancer Center, Oklahoma City, OK) approved the study, and all patients provided written informed consent.
Study design and drug administration
Using a 3 + 3 dose escalation design, cohorts of 3–6 patients were treated with escalating BID doses of BEZ235 in 28-day treatment cycles. For intrapatient PK comparison, patients received a lead in on days 1–8, in which the entire amount of drug was administered as one daily dose. This was followed by BID dosing beginning on day 9. The daily dose lead-in was later removed by protocol amendment due to dose-limiting toxicities as described in the Results section. Evaluation of at least 3 patients completing one cycle of treatment was required prior to dose escalation, and patients were required to receive at least 80 % of doses in cycle 1 to be considered evaluable for escalation decisions. Toxicities were graded using the National Cancer Institute Common Terminology Criteria for Adverse Events (CTCAE version 4) [9]. Grade 4 neutropenia for >7 days or febrile neutropenia, grade 4 thrombocytopenia or grade 3 thrombocytopenia with bleeding, grade 3 or 4 non-hematologic toxicity (excluding rash, nausea, diarrhea, and vomiting if controlled by supportive care), and treatment delays of ≥14 days due to unresolved toxicity were considered dose-limiting. The MTD was defined as the highest dose at which ≤1 of 6 or ≤33 % of patients experienced dose-limiting toxicity (DLT) during the first cycle of treatment.
BEZ235 was supplied by Novartis Pharmaceuticals, Inc as SDS sachets. Daily doses of BEZ235 were taken at approximately the same time each day within 30 min after a light meal. Patients were instructed to suspend one sachet in a glass of water or apple juice (approximately 50 mL), drink the content, and then rinse the glass using approximately one-fourth the volume of liquid to drink the remaining sachet content. After PK collection was completed on day 1 of cycle 2, patients were permitted to mix the sachet in chocolate milk, yogurt, or applesauce.
Patients could continue treatment until disease progression or intolerable toxicity. Dose reductions or holds and initiation of supportive care were allowed at the discretion of the treating physician. Patients who required delays in treatment could proceed with the next cycle when the toxicity improved to ≤ grade 1 or the baseline value. If a delay of more than 14 days was required due to treatment-related toxicity, patients discontinued treatment unless the treating physician and medical monitor agreed that continued treatment at a lower dose level was in the patient’s best interest.
Patient selection
Adult patients with advanced solid tumors and Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1 were eligible. A protocol amendment later limited the eligible tumor types to those that had shown preclinical and/or early clinical activity with PI3K/mTOR inhibitors, including: breast, renal cell, endometrial, carcinoid, and pancreatic neuroendocrine tumors (PNET). Adequate organ system function for study entry was defined as: absolute neutrophil count (ANC) ≥1.5 × 109/L; platelets ≥100 × 109/L; hemoglobin ≥9 g/dL; INR ≤2; fasting plasma glucose ≤140 mg/dL; total bilirubin ≤1.5 times the upper limit of normal (ULN); alanine aminotransferase (ALT) and aspartate aminotransferase (AST) ≤3 times ULN, or ≤5 times ULN with liver involvement; creatinine ≤1.5 times ULN or calculated or measured creatinine clearance ≥50 mL/min. Women of child-bearing potential were required to have a negative serum or urine pregnancy test within 72 h of starting treatment.
Patients with diabetes mellitus requiring insulin or those with a history of gestational diabetes mellitus were excluded, as were those who received an investigational drug within 21 days or 5 half-lives (whichever was shorter) prior to beginning treatment with BEZ235. Patients with previously untreated brain metastases were not allowed; however, patients who had received radiation or surgery for brain metastases could be enrolled if treatment was completed at least 2 weeks prior to study entry and there was no evidence of central nervous system (CNS) progression. Patients were not permitted to use enzyme-inducing antiepileptic drugs or chronic corticosteroid treatment for CNS metastases. Additional exclusion criteria were: left ventricular ejection fraction (LVEF) <50 % by multiple gated acquisition (MUGA) or echocardiogram; QTcF >480 msec; myocardial infarction within 6 months; New York Heart Association congestive heart failure III-IV; inadequately controlled hypertension (systolic >180 mmHg or diastolic >100 mmHg); use of strong CYP3A4 inhibitors; known human immunodeficiency virus (HIV), hepatitis B or hepatitis C.
Study assessments
Prior to the initiation of treatment and at various time points throughout the study, all patients underwent physical examination, assessment of ECOG performance status, electrocardiogram (ECG), echocardiogram or MUGA, and computed tomography (CT) scans to evaluate disease. Patients were restaged at eight-week intervals to evaluate response to treatment according to the Response Evaluation Criteria in Solid Tumors (RECIST version 1.1) [10]. Laboratory evaluations included a complete blood count (with differential and platelets), chemistry panel, cholesterol panel, hemoglobin A1C, fasting plasma glucose, insulin, c-peptide, and fructosamine.
Pharmacokinetics
Samples for PK analysis were collected at the following time points on days 1, 8, and 28 of cycle 1: pre-dose, 1, 2, 4, 8, 10, 12, and 24 h post-dose. Non-compartment methods were used to assess AUC0-∞, AUC0-τ, Cmax, tmax, λZ, and half-life (t1/2). PK parameter estimates were then used to evaluate dose proportionality.
Pharmacodynamics
Fresh tumor biopsy samples for PD analysis were collected prior to treatment, at the end of cycle 1, and after disease progression, for evaluation of phosphorylation status and activation of PI3K downstream signaling targets.
18 F-FDG-positron emission tomography (PET) imaging
PET scans to measure 18 F-FDG uptake were performed at baseline and between days 15 and 22 of cycles 1 and 2.
Statistical considerations
This study tested no formal hypotheses, and analyses were descriptive and exploratory. The study was planned to enroll approximately 20–37 patients, depending on the number of cohorts required to determine the MTD. All patients who received at least one dose of BEZ235 were included in the safety analysis. Planned endpoints for response to treatment included the proportion of patients with complete (CR) and partial (PR) responses, proportion of patients with stable disease, and the time to disease progression.
Results
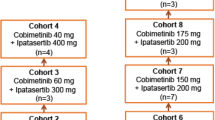
Between April 2011 and April 2013, 33 patients were enrolled (Table 1). The median age was 62 years (range: 20–86 years), and the most common tumor types were colorectal (11 patients, 33 %) and breast (4 patients, 12 %). Twelve patients (36 %) had received four or more prior lines of systemic therapy. The median duration of treatment was 8 weeks (range: 1–41 weeks); treatment duration for all patients by dose level is shown in Fig. 1.
Escalation and maximum tolerated dose
Dose escalation and DLTs are shown in Table 2. Cohort 1 (200 mg BID with lead-in) and Cohort 2 (400 mg BID with lead-in) each enrolled three evaluable patients without occurrence of DLT. Two patients on Cohort 3 (600 mg BID with lead-in) had DLTs of grade 3 mucositis. Following the observation of these toxicities, which occurred early in the cycle, the lead-in was removed from subsequent cohorts by amendment. The next dose level evaluated was 600 mg BID without lead-in, and two of five evaluable patients on that dose level had DLTs (grade 3 mucositis and grade 3 fatigue). The dose was then reduced to 400 mg BID without lead-in, at which both evaluable patients had DLTs (grade 3 hyperglycemia, dehydration, fatigue; grade 3 thrombocytopenia that required delayed start of cycle 2). Cohort 2 (400 mg BID with lead-in) was then re-evaluated, and only one of three evaluable patients at this dose had grade 3 mucositis. However, there was chronic low-grade toxicity at this dose level, including grade 1/2 hyperglycemia, mucositis, fatigue, anorexia, thrombocytopenia, and diarrhea, starting as early as Cycle 1. The dose was reduced again to 300 mg BID without lead-in, at which only one of 10 evaluable patients had DLT (grade 3 mucositis). The MTD and recommended dose for further study was declared as 300 mg BID without lead-in.
Safety
Treatment-related adverse events are shown in Table 3. The most common toxicities included (all grades): diarrhea (19 patients, 58 %), mucositis (19 patients, 58 %), and nausea (14 patients, 42 %). Hyperglycemia (all grades) was seen in 8 patients (24 %) overall and 2 patients dosed at the MTD. Three patients (1 patient at 400 mg BID with no lead-in, 2 patients at 600 mg BID with no lead-in) required dose reductions and 2 patients (both at 600 mg BID with no lead- in) had treatment held. Five patients were treated with metformin, glipizide, and glyburide, and 1 patient required insulin. Mucositis was the most frequent grade 3 toxicity (5 patients, 15 %), and was also the primary DLT. There were no grade 4 treatment-related adverse events reported, and no treatment-related hospitalizations or deaths. There were 13 SAEs on the trial, but none were considered treatment-related. There were also 7 patients (21 %) who had dose reductions including one patient who had 2 dose reductions. Seventeen patients (52 %) had treatments temporarily interrupted. There were no dose reductions for patients treated at the MTD and 4 patients at this dose level had treatment held.
Pharmacokinetics
Pharmacokinetic variables of AUC(0–24), Cmax, and Tmax listed by cohort are shown in Table 4. Pharmacokinetic comparison of AUC with the QD and BID schedules is shown in Figs. 2 and 3 shows mean Cmax by total daily dose for each dosing regimen. Though there is interpatient variability, pharmacokinetics suggest equivalent AUC and lower Cmax with BID dosing compared to QD dosing, and higher Cmax with lead-in doses as compared to regimens without lead-in.
Pharmacodynamics
18 F-FDG-PET imaging
Twenty-seven patients underwent FDG-PET imaging at baseline and after 1–2 cycles of treatment (Fig. 4). Twenty patients (74 %) had a decrease in 18 F-FDG uptake following treatment. One patient (4 %) had no change and the remaining 6 patients (22 %) had an increase in uptake after treatment. The median decrease in SUV was 26 % (Range 5–67 %) for all patients and the median decrease in SUV at the MTD was 42 % (Range 6–67 %).
Response to treatment
Twenty-one patients received at least 8 weeks of treatment and were evaluated for response. No CRs or PRs were reported. 15 patients (45 %) had stable disease as their best response. A total of 10 patients (30 %) received treatment for ≥16 weeks, including colorectal (4 patients), endometrial (3 patients), and one each of melanoma, carcinoid tumor (NOS), and pancreas cancer (Fig. 1). Four of these patients were treated at the MTD.
Discussion
In this phase 1 trial, the recommended dose for further study of sachet formulation of BEZ235 was 300 mg BID. Consistent with reports of other dual PI3K/mTOR inhibitors in development, dose escalation was limited by mucositis, fatigue, and hyperglycemia, and common toxicities included (all grades) diarrhea (58 %), mucositis (58 %), and nausea (42 %). Common AEs in phase 1 studies with the other dual PI3K/mTOR inhibitors in development (XL765, GDC-0980, GSK2126458, and PF-04691502) were similar to those seen in this phase 1 trial of BEZ235, including nausea, vomiting, diarrhea, anorexia, and skin disorders [11–14]. Similarly, the most common toxicities reported in the phase I trial of the pan-PI3K inhibitor SAR245408 were rash 26 %, nausea (22 %) and diarrhea (20 %) [15].
Hyperglycemia was seen in patients treated in the phase 1 trials of PF-04691502 and GSK2126458, and was experienced by 24 % of patients treated in this trial of BEZ235 [13, 14]. In this study, hyperglycemia resulted in 3 dose reductions and 2 patients had treatment held. Most of the hyperglycemic patients on this study achieved glucose control with metformin, glipizide or glyburide and 1 patient was treated with insulin.
Pharmacokinetics suggested lower Cmax and equivalent AUC with BID dosing as compared to QD dosing. This lower Cmax did not result in decreased rates of toxicity. The most common toxicities for patients on QD dosing BEZ235 treatment were fatigue (14 patients, 24 %), diarrhea (15 patients, 25 %), nausea (12 patients, 20 %), and vomiting (10 patients, 17 %) [16]. BID dosing of BEZ235 resulted in fatigue (33 %), diarrhea (58 %), nausea (42 %) and vomiting (33 %). There were no objective responses observed in this study, but prolonged stable disease was observed in 10 patients with colorectal, endometrial, melanoma, carcinoid tumor, and pancreas cancer. This is also consistent with reports of other PI3K/mTOR inhibitors as single agents [11, 17, 18]. Four of the patients with prolonged stable disease were treated at the MTD, suggesting this is a dose within therapeutic range. Decreases in SUV on PET scans at the MTD also suggest potential inhibition of the pathway at this dose. This trial did not select patients based on genetic alterations in this pathway, and it is unknown whether mutations in PIK3CA would increase the likelihood of response.
In summary, while BEZ235 monotherapy at its recommended phase 2 dose of 300 mg BID in the sachet formulation was generally well-tolerated, there were no objective responses observed. Pharmacokinetic profile differences observed with the BID sachet compared to QD dosing did not translate into modification of the toxicity profile or response rate. BEZ235 has undergone further study as both a single agent and in combination for a number of solid tumor types, including some trials that were enriched for alterations in the PI3K/Akt/mTOR pathway. While these studies show that BEZ235 is fairly well-tolerated, clinical response has generally been limited [8, 19–22]. BEZ235 is no longer in clinical development.
References
Bachman KE, Argani P, Samuels Y, Silliman N, Ptak J, Szabo S, Konishi H, Karakas B, Blair BG, Lin C, Peters BA, Velculescu VE, Park BH (2004) The PIK3CA gene is mutated with high frequency in human breast cancers. Cancer Biol Ther 3:772–775
Samuels Y, Diaz LA Jr, Schmidt-Kittler O, Cummins JM, Delong L, Cheong I, Rago C, Huso DL, Lengauer C, Kinzler KW, Vogelstein B, Velculescu VE (2005) Mutant PIK3CA promotes cell growth and invasion of human cancer cells. Cancer Cell 7:561–573
Samuels Y, Wang Z, Bardelli A, Silliman N, Ptak J, Szabo S, Yan H, Gazdar A, Powell SM, Riggins GJ, Willson JK, Markowitz S, Kinzler KW, Vogelstein B, Velculescu VE (2004) High frequency of mutations of the PIK3CA gene in human cancers. Science 304:554
Kang S, Bader AG, Vogt PK (2005) Phosphatidylinositol 3-kinase mutations identified in human cancer are oncogenic. Proc Natl Acad Sci U S A 102:802–807
Cantley LC, Neel BG (1999) New insights into tumor suppression: PTEN suppresses tumor formation by restraining the phosphoinositide 3-kinase/AKT pathway. Proc Natl Acad Sci U S A 96:4240–4245
Cully M, You H, Levine AJ, Mak TW (2006) Beyond PTEN mutations: the PI3K pathway as an integrator of multiple inputs during tumorigenesis. Nat Rev Cancer 6:184–192
Burris H, Rodon J, Sharma S, Herbst RS, Tabernero J, Infante JR, Silva A, Demanse D, Hackl W, Baselga J (2010) First-in-human phase I study of the oral PI3K inhibitor BEZ235 in patients (pts) with advanced solid tumors. ASCO Meet Abstr 28:3005
Peyton JD, Rodon Ahnert J, Burris H, Britten C, Chen LC, Tabernero J, Duval V, Rouyrre N, Silva AP, Quadt C, Baselga J (2011) A dose-escalation study with the novel formulation of the oral pan-class I PI3K inhibitor BEZ235, solid dispersion system (SDS) sachet, in patients with advanced solid tumors. ASCO Meet Abstr 29:3066
NCI Common Terminology Criteria for Adverse Events (CTCAE) v.4. http://evs.nci.nih.gov/ftp1/CTCAE/About.html, National Cancer Institute (acessed October, 2014)
Eisenhauer E, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, Rubinstein L, Shankar L, Dodd L, Kaplan R, Lacombe D, Verweij J (2009) New response evaluation criteria in solid tumors: revised RECIST guideline (version 1.1). Eur J Cancer 45:228–247
Brana I, LoRusso P, Baselga J, Heath EI, Patnaik A, Gendreau S, Laird A, Papadopoulos K (2010) A phase I dose-escalation study of the safety, pharmacokinetics (PK), and pharmacodynamics of XL765 (SAR245409), a PI3K/TORC1/TORC2 inhibitor administered orally to patients (pts) with advanced malignancies. ASCO Meet Abstr 28:3030
Hollebecque A, Clamp A, Horsley L, Morgan JA, Bahleda R, George S, Shaw D, Lauchle JO, Ware J, Desai R, Wu J, Fu L, Jayson GC, Soria JC, Wagner AJ 12. Hollebecque A, Clamp A, Horsley L (2011) A phase I study evaluating the pharmokinetics (PK) and pharmodynamics (PD) activity of the dual PI3K/mTOR inhibitor GDC-0980 administered once weekly (QW). AACR/NCI/EORTC Molecular Targets and Cancer Therapeutics Meeting Abstract B153
Millham R, Houk B, Borzillo G (2011) First-in-patient study of PF-04691502, a small molecule intravenous dual inhibitor of PI3K and mTOR in patients with advanced cancer: update on safety, efficacy, and pharmacology. AACR/NCI/EORTC Molecular Targets and Cancer Therapeutics Meeting Abstract B163
Munster PN, van der Noll R, Voest EE, Dees EC, Tan AR, Specht JM, Falchook GS, Daud A, Lolkema MP, Grilley-Olson JE, Yu EY, Fu S, Bergsland EK, Kleha J, Peng S, Smith DA, Lampkin TA, Schellens JHM, Morris SR, R. Kurzrock R (2011) Phase I first-in-human study of the PI3 kinase inhibitor GSK2126458 (GSK458) in patients with advanced solid tumors (study P3K112826). ASCO Meeting Abstracts 29:3018
Shapiro GI, Rodon J, Bedell C, Kwak EL, Baselga J, Braña I, Pandya SS, Scheffold C, Laird AD, Nguyen LT, Xu Y, Egile C, Edelman G (2014) Phase I safety, pharmacokinetic, and pharmacodynamic study of SAR245408 (XL147), an oral pan-class I PI3K inhibitor, in patients with advanced solid tumors. Clin Cancer Res 20:233–245
Burris H, Rodon J, Sharma S, Herbst RS, Tabernero J, Infante JR, Silva A, Demanse D, Hackl W, Baselga J (2010) First-in-human phase I study of the oral dual PI3K and mTORC1/2 inhibitor BEZ235 in patients with advanced solid tumors. ASCO Meeting Oral Presentation 3005
Hollebecque A, Clamp A, Horsley L (2011) A phase 1 study evaluating the pharmacokinetics (PK) and pharmacodynamic (PD) activity of the dual PI3K/mTOR inhibitor GDC-0980 administered once weekly (QW). American Association for Cancer Research, Orlando
Millham R, Houk B, Borzillo G (2011) First-in-patient study of PF-049691502, a small molecule intravenous dual inhibitor of PI3K and mTOR in patients with advanced cancer: update on safety, efficacy, and pharmacology. AACR-NCI-EORTC International Conference on Molecular Target and Cancer Therapeutics San Franciso, CA, Abstract B163
Campone M, Fumoleau P, Gil-Martin M, Isambert N, Beck JT, Becerra C, Shtivelband M, Duval V, di Tomaso E, Roussou P, Urban P, Urruticoechea A (2012) A multicenter, open-label Ph IB/II study of BEZ235, an oral dual PI3K/mTOR inhibitor, in combination with paclitaxel in patients with HER2-negative, locally advanced or metastatic breast cancer. San Antonio Breast Cancer Symposium Abstract:P6-11-08
Mayer IA, Abramson VG, Balko JM, Isakoff SJ, Forero A, Kuba MG, Sanders ME, Li Y, Winer E, Arteaga CL (2012) SU2C phase 1b trial of dual PI3K/ mTOR inhibitor BEZ235 with letrozole in ER+/HER2- METASTATIC BREAST CANCER (MBC). San Antonio Breast Cancer Symposium Abstract: P6-10-05
Ahnert JR, Schuler MH, Machiels J-P H, Hess D, Paz-Ares L, Awada A, von Moos R, Steeghs N, Zambrano CC, Peggy De Mesmaeker P, Richly H, Herremans C, Joerger M, Jaime JC, Alsina M, Baffert F, Demanse D, Duval V, Morozov A, Dirix L (2014) Phase lb study of BEZ235 plus either paclitaxel (PTX) in advanced solid tumors (aST) or PTX plus trastuzumab (TZ) in HER2+ breast cancer (BC). ASCO Meet Abstr 32:621
Siegel AP, Bryce AH, Lin AM, Friedlander TW, Hsieh AC, Hang E, Weinberg VK, Ryan CJ (2014) Results of a multicenter phase I/II trial of abiraterone acetate plus BEZ235 in metastatic, castration-resistant prostate cancer (mCRPC). ASCO Meet Abstr 32:e16042
Acknowledgments
The investigators are grateful to the patients who participated in this trial as well as the very important contributions of the site personnel.
Compliance with Ethical Standards
ᅟ
Disclosures of potential conflicts of interest
The study was funded in part by a grant from Novartis. The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bendell, J.C., Kurkjian, C., Infante, J.R. et al. A phase 1 study of the sachet formulation of the oral dual PI3K/mTOR inhibitor BEZ235 given twice daily (BID) in patients with advanced solid tumors. Invest New Drugs 33, 463–471 (2015). https://doi.org/10.1007/s10637-015-0218-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-015-0218-6