Abstract
Purpose
Transforming growth factor-beta inhibitors may enhance the antitumor activity of gemcitabine with acceptable safety and tolerability. This open-label, multicenter, non-randomized phase 1b study assessed the safety/tolerability, pharmacokinetics, and tumor response of galunisertib plus gemcitabine in Japanese patients with advanced or metastatic pancreatic cancer.
Methods
During each 28-day cycle, galunisertib 150 mg was administered orally twice daily (300 mg/day) for 14 days, followed by 14 days of rest. Gemcitabine 1000 mg/m2 was intravenously given on Days 8, 15, and 22. Safety was assessed by the incidence of dose-limiting toxicities (DLTs) in the first cycle and treatment-emergent adverse events (TEAEs). Efficacy was assessed by antitumor activity and changes in carbohydrate antigen 19-9 (CA19-9).
Results
No DLTs were reported. All 7 enrolled patients had ≥1 TEAE, of which the most common included anorexia, decreased neutrophil count, and decreased white blood cell count. Grade ≥3 TEAEs were observed in 6 patients; 4 patients had Grade ≥3 TEAEs (decreased neutrophil, white blood cell, and lymphocyte count; hypophosphatemia) considered possibly related to study drug(s). The pharmacokinetic profile of galunisertib in combination with gemcitabine was similar to that previously observed for galunisertib alone. The clinical response [complete response (CR), partial response (PR), or stable disease] rate was 42.9%, and the median progression-free survival was 64 days; no CR/PR were achieved.
Conclusion
Galunisertib plus gemcitabine had an acceptable safety/tolerability profile with evidence of efficacy in Japanese patients with advanced or metastatic pancreatic cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreatic cancer is the fourth leading cause of cancer death in Japan, with approximately 32,000 Japanese people reported to have died from pancreatic cancer in 2014 [1]. The 5-year survival rate in patients with pancreatic cancer in Japan is 7.7% [2]. Regarding treatment, gemcitabine is recommended as a part of the first-line therapy for metastatic pancreatic cancer [3,4,5]. However, despite attempts to improve treatment modalities, advanced or metastatic pancreatic cancer remains difficult to treat and, therefore, an unmet medical need exists for these patients.
Galunisertib (LY2157299 monohydrate), a small molecule inhibitor (SMI) of the type I transforming growth factor-beta receptor (TGF-β RI) serine/threonine kinase, is the first SMI to enter clinical development [6]. The safety and efficacy of galunisertib monotherapy in Caucasian and Japanese patients has been previously assessed. In early-phase clinical trials of primarily Caucasian patients with glioma or hepatocellular carcinoma, galunisertib had an acceptable safety profile and elicited antitumor effects [7, 8]. Further, a non-randomized, open-label, dose escalation study found that galunisertib was well tolerated and adverse events (AEs) were clinically manageable in Japanese patients with advanced solid tumors. Dose escalation was successfully achieved using 80 mg and 150 mg twice-daily (BID) doses of galunisertib in the absence of cardiovascular toxicities or other dose-limiting toxicities (DLTs) [9].
The pathophysiological role of TGF-β in various cancers and its identification as a potential tumor target in pancreatic cancer provides a rationale for investigating galunisertib in combination with gemcitabine [10, 11]. TGF-β cytokines regulate growth and differentiation of various cell types, and abnormal regulation of TGF-β receptors may result in pancreatic tumor progression [10]. In support of this, galunisertib, a TGF-β receptor inhibitor, in combination with gemcitabine, significantly reduced tumor burden, prolonged survival, and reduced spontaneous abdominal metastases in a orthotopic murine model of metastatic pancreatic cancer [11]. Further, an inhibitor of the TGF-β receptor 2, which has shown potent antimetastatic activity in orthotopic human tumor xenografts, syngeneic tumors, and a genetic model of pancreatic cancer, resulted in a survival benefit [12].
Based on this non-clinical background, addition of galunisertib is anticipated to enhance the antitumor activity of gemcitabine. Support for this expectation was found in a phase 1b study of Caucasian patients with advanced cancer, that revealed there were no DLTs, no clinically meaningful cardiotoxicities, and no influence in the pharmacokinetic (PK) profile of galunisertib when galunisertib was administered at a dose of 300 mg/day (150 mg BID) in combination with gemcitabine 1000 mg/m2 [13, 14]. However, there is a lack of data on galunisertib in combination with gemcitabine in Japanese patient populations.
The primary objective of this study was to evaluate the safety and tolerability of galunisertib in combination with gemcitabine as assessed by DLTs in Japanese patients with advanced or metastatic pancreatic cancer. Secondary objectives were to (1) assess the PK profile of galunisertib, gemcitabine, and the deaminated metabolite of gemcitabine, 2′,2′-difluorodeoxyuridine (dFdU), and (2) document any antitumor activity observed after administration of galunisertib and gemcitabine.
Materials and methods
Study design
This was an open-label, multicenter, non-randomized, phase 1b study of galunisertib administered in combination with gemcitabine to patients with advanced or metastatic pancreatic cancer. The study was conducted at 2 study centers in Japan between May 22, 2014 and July 2, 2015.
Written approval was provided by ethics review boards, and the study was conducted in accordance with international ethics guidelines, including the Declaration of Helsinki and the International Conference on Harmonisation Good Clinical Practices Guideline [E6]. Informed consent was obtained from each patient before any protocol procedures or administration of study drug. The trial was registered with ClinicalTrials.gov (NCT02154646).
Study population
Regarding eligibility criteria, the key inclusion criterion was histological or cytological diagnosis of locally advanced or metastatic adenocarcinoma of the pancreas not amenable to resection with curative intent. Prior chemotherapy, radiotherapy, cancer-related hormone therapy, or other investigational therapy was permitted. Patients with previous radical surgery for pancreatic cancer were eligible after documented progression; if these patients received chemoradiotherapy with gemcitabine or other commonly used cytotoxic agents in an adjuvant or neoadjuvant setting, they could be enrolled if the treatment was completed ≥2 weeks before study enrollment. Other inclusion criteria were measurable or non-measurable disease as defined by the Response Evaluation Criteria in Solid Tumors (RECIST version 1.1) [15], males or females at least 20 years of age, and Eastern Cooperative Oncology Group (ECOG) performance status (PS) score ≤1.
The main exclusion criteria were conditions related to moderate or severe cardiac disease (e.g., myocardial infarction within 6 months before study enrollment). Patients with predisposing conditions consistent with developing aneurysm of ascending aorta or aortic stress, as well as a history of cardiac or aortic surgery, were also excluded. Finally, patients were excluded if they had significantly elevated brain natriuretic peptide or troponin I levels at screening.
Treatment plan
Study drug administration
During each 28-day cycle, galunisertib 150 mg was administered orally BID (300 mg/day) morning and evening for 14 days, followed by 14 days of rest. This dose (300 mg/day, 150 mg BID) for the Japanese population was selected based on safety, PK, and pharmacodynamic data from two previous studies [7, 9]. Gemcitabine was given as an intravenous infusion at a dose of 1000 mg/m2 over 30 min (maximum of approximately 60 min) on Days 8, 15, and 22 of each cycle. The plan was to enroll 6 patients continuously without waiting for DLT assessment in each patient. Patients were evaluated for DLTs in the first cycle (Day 1 to Day 28); if DLTs were observed in 2 patients, further enrollment was suspended until the ongoing patient(s) completed DLT evaluation. Further enrollment was continued if no other DLT was observed in the ongoing patient(s). Enrollment was to be stopped either when all 6 evaluable patients were enrolled or when 3 patients with DLTs were observed. Completed treatment cycles were those for which a patient received all of the study drug planned during the cycle.
Dose modifications
In terms of dose modification, it should be noted that no galunisertib dose reduction was allowed during Cycle 1. However, if a patient experienced a DLT-equivalent toxicity in Cycle 2 or beyond, the galunisertib dose was reduced to 160 mg/day (80 mg BID), unless the patient was expected to receive a clinical benefit (in the opinion of the investigator) from continuing to take 300 mg/day; the patient continued to receive the reduced dose even after toxicity recovery. Patients who experienced a second DLT-equivalent toxicity discontinued unless they were expected to receive clinical benefit. Gemcitabine dose adjustments were based on the recommendation of the United States in-label use and dose reductions for gemcitabine when used as monotherapy.
Outcome measures
Safety
Safety was assessed by the incidence of DLTs, AEs [including treatment-emergent AEs (TEAEs) and serious adverse events (SAEs)], laboratory tests, vital signs, and electrocardiogram (ECG) evaluations (QTc analysis were performed using Bazett’s [QTcB] and Fridericia’s [QTcF] correction methods [16]). AEs were summarized using the Common Terminology Criteria for Adverse Events (CTCAE, version 4.03) and the Medical Dictionary for Regulatory Activities (MedDRA, version 18.1).
DLTs were defined as any of the following events that occurred during the first cycle (Day 1 to Day 28) and were considered by the investigator to be attributable to galunisertib or the combination of galunisertib and gemcitabine: CTCAE Grade 4 thrombocytopenia (or Grade 3 thrombocytopenia with bleeding), febrile neutropenia, Grade 4 neutropenia >7 days, Grade 4 anemia, and Grade ≥3 non-hematological toxicity, except for (1) Grade 3 fatigue, skin rash, nausea, vomiting, constipation, or diarrhea controlled with appropriate supportive care intervention; transient electrolyte abnormality; and transient hepatic enzyme elevation that can recover within 72 h with appropriate management, (2) transient (≤7 days) Grade 3 elevations of bilirubin in the setting of preexisting mechanical obstruction, and (3) transient (≤7 days) Grade 3 elevations of alanine aminotransferase and/or aspartate aminotransferase, without evidence of other hepatic injury, in the setting of preexisting hepatic metastasis or stenting. Other events considered to be DLTs included: any other significant toxicity deemed to be dose-limiting, failure to recover sufficiently from galunisertib toxicities to allow restarting of treatment, suboptimal dosing (<80% of galunisertib 300 mg/day or less than 2 full doses of gemcitabine in Cycle 1) from study drug-related toxicity, and an actual number of gemcitabine administrations <3 due to toxicity.
Pharmacokinetics
The PK analyses were conducted on patients who received at least one dose of study drug and had PK samples collected. The following PK parameters for galunisertib were computed by standard non-compartmental methods of analysis using Phoenix® WinNonlin (Certara, New Jersey, USA): maximum plasma concentration (C max), time to maximum plasma concentration (t max), area under the plasma concentration–time curve from time zero to specified time (AUC(0–t)), area under the plasma concentration–time curve from time zero to the last time point with a measurable plasma concentration (\({\text{AUC}}_{{(0 - t_{\text{last}} )}}\)), area under the plasma concentration–time curve from time zero to infinity (AUC(0–∞)), elimination half-life (t 1/2), apparent volume of distribution at steady state during the terminal phase (V z,ss/F), and apparent total body clearance at steady state (CLss/F). AUC, C max, and t 1/2 for gemcitabine and dFdU were calculated in the same manner. The total body clearance (CL) and volume of distribution at steady state (V ss) were also computed.
Efficacy
Efficacy was assessed by antitumor activity according to RECIST version 1.1 including best overall response, progression-free survival (PFS), duration of response, and bioanalytical assessment of carbohydrate antigen 19-9 (CA19-9). Best overall response (tumor measurement performed every 2 cycles) included complete response (CR), partial response (PR), and stable disease (SD). CR or PR were claimed only if the criteria for these were met at a subsequent time point (at least 4 weeks), whereas SD was claimed if measurements met SD criteria at least once and at least 6 weeks after the first dose of study drug. PFS was defined as the duration from the first dose of study drug to the first objective progression of disease or death from any cause, whichever was earlier. For a patient who was not known to have died or progressed by the data inclusion cutoff date, PFS time was censored at the last objective progression-free disease assessment. Duration of response was assessed for patients who achieved CR or PR and was measured from the start of achieving response (first observation of response before confirmation) to the time of disease progression. CA19-9 was measured in a central laboratory for patients who had a positive result for CA19-9 at baseline (prestudy). CA19-9 value was positive when it exceeded the normal value of the testing laboratory.
Statistical analysis
The sample size was determined by the study design, as previously described, rather than based on a statistical power calculation.
DLT-related safety analyses were conducted, such that a patient was considered non-evaluable for DLTs if they received <80% of the galunisertib dose of 300 mg/day, or less than 2 full doses of gemcitabine in Cycle 1 for reasons other than study drug-related toxicity. Other safety analyses and all efficacy analyses were conducted on all patients who received at least 1 dose of study drug. Patient disposition, demographics, and baseline disease characteristics were summarized for these patients.
Safety data were summarized by frequency (DLTs and AEs), or using summary statistics (laboratory tests and vital signs). Efficacy data were summarized by frequency or using summary statistics, depending on the characteristics of the data. The clinical response rate was the percentage of patients who experienced a best overall response of CR, PR, or SD. A waterfall plot of the best percentage change in tumor size and a line plot of percentage change from baseline in tumor size was created. Percent change from baseline in tumor size was calculated, where a decrease from baseline reflects better outcome.
Results
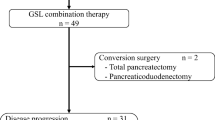
Patient disposition and extent to exposure
Of the 9 patients who entered the study, 2 patients failed to meet the entry criteria. All 7 enrolled patients received at least 1 dose of study drug. Of the 7 enrolled patients, 6 patients were eligible for DLT-related safety analysis and all 7 patients were eligible for other safety assessments.
All 7 enrolled patients discontinued study treatment due to progressive disease. For galunisertib, the median number of maximum cycles per patient was 2 cycles (range 1–10 cycles), and the median number of completed treatment cycles per patient was 2 cycles (range 0–6 cycles). For gemcitabine, the median number of maximum cycles per patient was 2 cycles (range 1–10 cycles), and the median number of completed treatment cycles per patient was 0 cycles (range 0–3 cycles). The median (range) dose intensity of galunisertib and gemcitabine was 85.7% (67.9–100.0%) and 70.6% (49.2–80.7%), respectively.
Demographic and baseline clinical characteristics
All 7 enrolled patients were Japanese and had adenocarcinoma of the pancreas (Union for International Cancer Control Stage II: 3 patients, 42.9%; Stage IV: 4 patients, 57.1% at initial diagnosis). The median age was 65 years (range 51–73 years), and 5 of 7 patients (71.4%) were male. ECOG PS was 0 for 3 patients (42.9%) and 1 for 4 patients (57.1%). A total of 6 patients (85.7%) had undergone at least 1 prior therapy, including surgery (pancreaticoduodenectomy) of curative intent (n = 4) and prior systemic therapies (n = 5) (Table 1).
Safety evaluations
No patients reported DLTs during the study. All 7 enrolled patients reported ≥1 TEAE during the study, and all patients reported TEAEs that were considered possibly related to study drug(s). The most commonly reported AEs (all grades), regardless of relatedness to treatment, were anorexia (n = 6), fatigue (n = 5), nausea (n = 5), neutrophil count decreased (n = 5), anemia (n = 4), and platelet count decreased (n = 4). A total of 6 patients (85.7%) had TEAEs with a severity of Grade ≥3 (Table 2), of whom 4 patients (57.1%) had Grade ≥ 3 TEAEs considered possibly related to study drug(s) [neutrophil count decreased (n = 4), white blood cell decreased (n = 2), hypophosphatemia (n = 1), lymphocyte count decreased (n = 1)]. A total of 2 SAEs (Grade 3 cholecystitis and Grade 3 duodenal stenosis) were reported in 1 patient during the study; neither SAE was considered related to either study drug. No deaths or discontinuations due to AEs were reported during the study. Laboratory results reported as abnormal were mostly Grade 1 or 2; the Grade 3 or 4 abnormal laboratory values mostly related to decreased blood cell counts. Postbaseline vital signs showed no clear pattern, and no patients met ICH criteria for abnormal ECGs (QTc interval >450 ms, QTc interval increases from baseline >30 ms) [16]. Several patients had overall abnormal echocardiography findings, but most were also present at baseline and were not considered AEs.
Pharmacokinetic evaluations
All 7 patients who provided blood samples for PK evaluation were included in the PK analysis. The PK profile of galunisertib was characterized by rapid absorption, with median t max of approximately 2 h postdose (Fig. 1). At steady state, on Day 14 in Cycle 1, the mean t 1/2 was 7.38 h. The mean CLss/F and V z,ss/F at steady state were 31.5 L/h and 335 L, respectively (Table 3). The PK profiles of gemcitabine and dFdU were similar to those reported in literature; the mean CL, and V ss of gemcitabine were 87.2 L/h/m2 and 34.2 L/m2, respectively (Table 4).
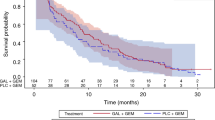
Efficacy evaluations
A total of 6 patients had evaluable tumor responses: 3 patients had SD as best overall response; 3 patients had progressive disease; and 1 patient was not evaluable. The clinical response (CR + PR + SD) rate was 42.9%. A waterfall plot of the best percentage change in tumor size is presented in Fig. 2. One patient, who had progressive disease as the best overall response to treatment in a non-target lesion, was omitted from the analysis and figure because this patient did not have a target lesion for measurement; therefore, no change from baseline in a target lesion could be represented. The median PFS was 64 days (range 22–316 days). Duration of response could not be assessed as no CR or PR was achieved as a best overall response to treatment.
All patients had high CA19-9 levels throughout the study, except for one patient who had normal levels at all testing time points. Postbaseline changes in serum CA19-9 levels were variable and showed no clear pattern. Four of 7 patients had nominal changes (i.e., stable levels) observed postbaseline, whereas the remaining 3 patients had variable levels throughout the study, of which only 1 patient appeared to have a substantial increase from baseline.
Discussion
The results of this open-label, multicenter, non-randomized, phase 1b study suggest that galunisertib in combination with gemcitabine has a favorable safety and tolerability profile in Japanese patients with advanced or metastatic pancreatic cancer. Further, the PK profile of galunisertib in combination with gemcitabine was broadly similar to that of galunisertib administered alone in Japanese patients [9]. Approximately 40% of patients had a best overall response of SD, including 2 patients with a reduction in tumor size (Fig. 2); no patients reported a CR or PR. Clinically, these results suggest that the response of Japanese patients to galunisertib–gemcitabine combination chemotherapy is generally consistent with that previously noted in Japanese patients who received galunisertib monotherapy [9].
In the present study, TEAEs possibly related to galunisertib were mostly mild or moderate in severity, and no DLTs were observed. These results are generally consistent with those observed in Japanese patients who received galunisertib 300 mg/day (150 mg BID, n = 9) monotherapy [9]. With regard to the observed lack of DLTs, this is also consistent with results seen in non-Japanese patients who received galunisertib 300 mg/day (150 mg BID, n = 5) in combination with gemcitabine 1000 mg/m2 [13]. In Japanese patients, the incidence of TEAEs in this study, especially those classified as Grade ≥3, appeared to be higher with combination therapy than with galunisertib monotherapy, but TEAEs were considered manageable in both studies [9]. Further, from a review of a phase 1 study of gemcitabine monotherapy in Japanese patients, it is possible that the most common Grade ≥3 TEAEs seen with galunisertib–gemcitabine combination therapy in the current study were related primarily to gemcitabine therapy. Whether the higher incidence of toxicity was a result of patient demographics (such as previous chemotherapy treatment) cannot be determined, given the small number of patients in this study. In addition, no new toxicities were observed in this study compared with previous studies [9, 13]. Laboratory tests, vital signs, ECGs, and echocardiography findings were variable and showed no clear patterns. Cardiac toxicity did not appear to be clinically significant in this study, with only 2 patients (28.6%) experiencing Grade 1 cardiac disorder AEs, neither of which were considered related to study drugs.
The PK profile of galunisertib in combination with gemcitabine, characterized by rapid absorption, was broadly similar to that of galunisertib administered alone in Japanese patients although the t max after oral dosing with combination therapy was slightly longer (median of approximately 2 h) and the C max was slightly lower [9]. The PK of gemcitabine, when co-administered with galunisertib, was also similar to that of gemcitabine administered alone in a previous phase 1 study of patients with pancreatic cancer (Study B9E-JE-P11D).
The sample size of the present study was small, and antitumor activity was not a primary objective of the study. Therefore, it is difficult to make clear conclusions about the efficacy of galunisertib in combination with gemcitabine in Japanese patients from these results. Further, it should be noted that the best overall response achieved by any patient was SD. A larger study (n = 156) in non-Japanese patients with Stage II–IV unresectable pancreatic cancer concluded that combination therapy resulted in an improved OS and PFS [14]. Further investigation is required to clarify the efficacy of this combination chemotherapy in Japanese patients with metastatic pancreatic cancer.
The main strength of this study is the enrollment of patients within a single racial population and that the study objectives were met in this population of Japanese patients. The main limitation of this study is the small number of enrolled patients (inherent to phase 1 study designs), which limits the confidence in the conclusions that can be drawn from these results, especially those related to efficacy.
Conclusion
The overall safety findings of this phase 1b study of Japanese patients with advanced or metastatic pancreatic cancer were consistent with the known safety profiles for galunisertib and gemcitabine, and can, therefore, be considered acceptable for this patient population. The PK profile of galunisertib in combination with gemcitabine was similar to the PK profile of galunisertib administered alone. Galunisertib in combination with gemcitabine may be associated with some clinical response to treatment in this patient population. However, further investigation is required to fully assess the efficacy of this combination in Japanese patients with advanced or metastatic pancreatic cancer.
References
Cancer Information Service NCC, Japan (2016) Cancer registry and statistics. http://ganjoho.jp/data/reg_stat/statistics/dl/cancer_mortality(1958-2014).xls. Accessed 30 September 2016
Center for Cancer Control and Information Services NCC (2016) Monitoring of cancer incidence in Japan—Survival 2006–2008 Report. http://ganjoho.jp/data/reg_stat/statistics/dl/cancer_survival(1993-2008).xls. Accessed 30 September 2016
Khorana AA, Mangu PB, Berlin J, Engebretson A, Hong TS, Maitra A, Mohile SG, Mumber M, Schulick R, Shapiro M, Urba S, Zeh HJ, Katz MHG (2016) Potentially curable pancreatic cancer: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol 34:2541–2556. doi:10.1200/jco.2016.67.5553
Sohal DPS, Mangu PB, Khorana AA, Shah MA, Philip PA, O’Reilly EM, Uronis HE, Ramanathan RK, Crane CH, Engebretson A, Ruggiero JT, Copur MS, Lau M, Urba S, Laheru D (2016) Metastatic pancreatic cancer: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol 34:2784–2796. doi:10.1200/jco.2016.67.1412
Balaban EP, Mangu PB, Khorana AA, Shah MA, Mukherjee S, Crane CH, Javle MM, Eads JR, Allen P, Ko AH, Engebretson A, Herman JM, Strickler JH, Benson AB, Urba S, Yee NS (2016) Locally advanced, unresectable pancreatic cancer: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol 34:2654–2668. doi:10.1200/jco.2016.67.5561
Herbertz S, Sawyer JS, Stauber AJ, Gueorguieva I, Driscoll KE, Estrem ST, Cleverly AL, Desaiah D, Guba SC, Benhadji KA, Slapak CA, Lahn MM (2015) Clinical development of galunisertib (LY2157299 monohydrate), a small molecule inhibitor of transforming growth factor-beta signaling pathway. Drug Des Devel Ther 9:4479–4499. doi:10.2147/DDDT.S86621
Rodon J, Carducci MA, Sepulveda-Sánchez JM, Azaro A, Calvo E, Seoane J, Braña I, Sicart E, Gueorguieva I, Cleverly AL, Pillay NS, Desaiah D, Estrem ST, Paz-Ares L, Holdhoff M, Blakeley J, Lahn MM, Baselga J (2015) First-in-human dose study of the novel transforming growth factor-β receptor I kinase inhibitor LY2157299 monohydrate in patients with advanced cancer and glioma. Clin Cancer Res 21:553–560. doi:10.1158/1078-0432.ccr-14-1380
Faivre SJSA, Kelley RK, Merle P, Gane E, Douillard JY, Waldschmidt D, Mulcahy MF, Costentin C, Minguez B, Papappicco P, Gueorguieva I, Cleverly A, Desaiah D, Lahn MM, Ameryckx S, Benhadji KA, Raymond E, Giannelli G (2014) A phase 2 study of a novel transforming growth factor-beta (TGF-β1) receptor I kinase inhibitor, LY2157299 monohydrate (LY), in patients with advanced hepatocellular carcinoma (HCC). J Clin Oncol 32(suppl 3):Abstract LBA173
Fujiwara Y, Nokihara H, Yamada Y, Yamamoto N, Sunami K, Utsumi H, Asou H, TakahashI O, Ogasawara K, Gueorguieva I, Tamura T (2015) Phase 1 study of galunisertib, a TGF-beta receptor I kinase inhibitor, in Japanese patients with advanced solid tumors. Cancer Chemother Pharmacol 76:1143–1152. doi:10.1007/s00280-015-2895-4
Miyazono K (2000) TGF-β/SMAD signaling and its involvement in tumor progression. Biol Pharm Bull 23:1125–1130. doi:10.1248/bpb.23.1125
Melisi D, Ishiyama S, Sclabas GM, Fleming JB, Xia Q, Tortora G, Abbruzzese JL, Chiao PJ (2008) LY2109761, a novel transforming growth factor β receptor type I and type II dual inhibitor, as a therapeutic approach to suppressing pancreatic cancer metastasis. Mol Cancer Ther 7:829–840. doi:10.1158/1535-7163.mct-07-0337
Schlingensiepen K-H, Stauder G, Bischof A, Egger T, Hafner M, Herrmuth H, Kielmanowicz M, Jachimczak P (2004) TGF-beta2 suppression in pancreatic cancer by the antisense oligonucleotide AP 12009: preclinical efficacy data. Proc Am Assoc Cancer Res 45(suppl):Abstract 2955
Kozloff MCR, Nadal T, Gueorguieva I, Cleverly A, Desaiah D, Lahn MMF, Pillay S, Blunt A, Tabernero J, Macarulla T (2013) Phase Ib study evaluating safety and pharmacokinetics (PK) of the oral transforming growth factor-beta (TGF-β) receptor I kinase inhibitor LY2157299 monohydrate (LY) when combined with gemcitabine in patients with advanced cancer. J Clin Oncol 31(suppl):Abstract 2563
Melisi D, Garcia-Carbonero R, Macarulla T, Pezet D, Deplanque G, Fuchs M, Trojan J, Oettle H, Kozloff M, Cleverly A, Gueorguieva I, Desaiah D, Lahn MM, Blunt A, Benhadji KA, Tabernero J (2016) A randomized phase II, double-blind study to evaluate the efficacy and safety of galunisertib + gemcitabine (GG) or gemcitabine + placebo (GP) in patients with unresectable pancreatic cancer (PC). Cancer Res 76(suppl 14):Abstract CT068. doi:10.1158/1538-7445.am2016-ct068
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, Rubinstein L, Shankar L, Dodd L, Kaplan R, Lacombe D, Verweij J (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45:228–247. doi:10.1016/j.ejca.2008.10.026
International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use (2005) The clinical evaluation of QT/QTc interval prolongation and proarrhythmic potential for nonantiarrhythmic drugs. http://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E14/E14_Guideline.pdf. Accessed 20 Jan 2017
Acknowledgements
The authors would like to thank all study participants and their families. We also wish to thank the study team members at the study centers, Eli Lilly and Company, and the CROs.
Author information
Authors and Affiliations
Contributions
All authors participated in the interpretation of study results, and in the drafting, critical revision, and approval of the final version of the manuscript. MI, ML, KO, and HU were involved in the study design and data analyses. MI and HU were involved in data collection. MI, HT, SK, and HU were investigators in the study, and KO conducted the pharmacokinetic analysis. KB was involved in the analysis and interpretation of data.
Corresponding author
Ethics declarations
Funding
This study was sponsored by Eli Lilly Japan, manufacturer/licensee of galunisertib (LY2157299 monohydrate, Grant Number H9H-JE-JBAO). Medical writing assistance was provided by Mark Snape, MB BS, CMPP and Hiroko Ebina, BPharm, Ph, MBA of ProScribe—Envision Pharma Group, and was funded by Eli Lilly and Company. ProScribe’s services complied with international guidelines for Good Publication Practice (GPP3). Eli Lilly Japan was involved in the study design, data collection, data analysis, and preparation of the manuscript.
Conflict of interest
KB/HF and ML/KO are current and former employees of Eli Lilly and Company, respectively. ML, KB, and HF own shares in Eli Lilly and Company. MI has received research funding from Taiho and Eli Lilly and Company, SK has received research funding from Eli Lilly and Company, Pfizer, Aslan Pharmaceuticals, AstraZeneca and Bayer, and HU has received research funding from Taiho and Eli Lilly and Company, and has been involved in a speakers’ bureau with Taiho. HT has no conflicts of interest to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Ikeda, M., Takahashi, H., Kondo, S. et al. Phase 1b study of galunisertib in combination with gemcitabine in Japanese patients with metastatic or locally advanced pancreatic cancer. Cancer Chemother Pharmacol 79, 1169–1177 (2017). https://doi.org/10.1007/s00280-017-3313-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-017-3313-x