Abstract
Purpose
The purpose of this study was to assess the efficacy and safety of fixed dose rate infusion of gemcitabine and S-1 combination therapy (FGS) in patients with gemcitabine (GEM)-refractory pancreatic cancer (PC) and to explore independent variables associated with survival.
Methods
We retrospectively reviewed consecutive patients with GEM-refractory PC who received FGS at our institution from March 2009 to December 2013. GEM was administered by fixed dose rate intravenous infusion of 1,200 mg/m2 as a 120-min infusion on day 1, and S-1 was administered orally twice a day at a dose of 40 mg/m2 on days 1–7. Cycles were repeated every 14 days.
Results
Sixty-one patients with GEM-refractory PC received FGS. Sixteen patients received FGS as third-line treatment. Twenty-nine patients (48 %) had a history of S-1 administration. The objective response rate was 13 %, and the disease control rate was 49 %. The median progression-free survival time was 2.7 months, and the median overall survival time was 6.0 months. Major Grade 3 or 4 adverse events included neutropenia (15 %), diarrhea (3 %), anorexia (2 %), and fatigue (2 %). A high inflammation-based prognostic score (modified Glasgow prognostic score (mGPS), which incorporates C-reactive protein and albumin), a performance status >0, and serum carbohydrate antigen 19–9 level >2,000 IU/ml were independently associated with a poor outcome.
Conclusions
FGS might be effective and well tolerated as salvage chemotherapy in a practical setting. The inflammation-based prognostic score is a simple and reliable indicator of survival in the setting of salvage chemotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gemcitabine (GEM) monotherapy has been applied for advanced pancreatic cancer (PC) as a standard treatment since a randomized controlled trial demonstrated improved overall survival (OS) compared with that with fluorouracil [1]. Although various GEM-based combination regimens have been evaluated, only nab-paclitaxel or erlotinib added to GEM showed a survival benefit over GEM alone in a phase III study [2–4]. Fluorouracil/leucovorin plus irinotecan plus oxaliplatin (FOLFIRINOX), a GEM-free combination regimen, demonstrated a clear survival benefit compared with GEM for patients with metastatic PC [5]. Therefore, these combination therapies have been considered to be standard first-line therapies.
However, after disease progression during first-line chemotherapy, the options for further anticancer treatment are limited. In Japan, clinical trials of S-1 (TS-1; Taiho Pharmaceutical, Tokyo, Japan) have been conducted since the early 2000s for patients with PC. A phase II study of S-1 first-line monotherapy led to a median progression-free survival (PFS) time of 2.0 months and a median OS time of 4.5 months in GEM-refractory metastatic PC [6]. In GEM-refractory metastatic PC, a recent phase I/II study of fixed dose infusion (FDR) GEM and S-1 combination therapy (FGS) yielded results that demonstrated activity including a response rate of 18 %, a median PFS time of 2.8 months, and a median OS time of 7.0 months, with a favorable toxicity profile [7]. A randomized phase II study comparing GEM administration via 30-min infusion and FDR infusion showed that FDR-GEM was associated with higher intracellular drug concentrations and efficacy [8]. A phase III study E6201 designed to test two promising approaches, FDR-GEM and GEM and oxaliplatin combination therapy (GEMOX), against standard GEM showed that OS time for FDR-GEM was longer than that for standard GEM (p = 0.04), but the difference was not statistically significant with respect to the parameters of the study (p < 0.025) [9]. The results of a phase I/II study of FGS for GEM-refractory PC suggested that even after the failure of standard GEM, the increased intracellular concentration of GEM as a result of FDR infusion and/or the synergistic effect of GEM and S-1 might play an important role in the antitumor effect of FGS for advanced GEM-refractory PC.
No standard salvage chemotherapy has been established for patients with advanced PC after the failure of GEM-based treatment. It is important to clarify the prognostic factors for patients with GEM-refractory advanced PC as well as to evaluate the efficacy and safety of salvage chemotherapy. With respect to measurement of the systemic inflammatory response, the combination of C-reactive protein and albumin (the original Glasgow prognostic score and the modified Glasgow prognostic score (mGPS)) has been shown to have prognostic value in a variety of common solid tumors [10, 11]. To our knowledge, there has been no report on the relationship between the modified Glasgow prognostic score and outcome in salvage chemotherapy for advanced PC.
As noted above, FGS was reported to provide promising antitumor activity and tolerable toxicity in patients with GEM-refractory PC. However, the previous study of FGS was limited in patient number, and the efficacy and safety of FGS for patients with GEM-refractory advanced PC are not well known. The aim of the present study was to retrospectively evaluate the efficacy and safety of FGS as salvage chemotherapy for advanced GEM-refractory PC in a clinical setting and to establish a method of selecting patients who will benefit from salvage chemotherapy.
Materials and methods
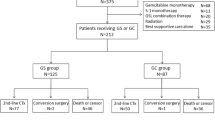
The subjects were consecutive patients with advanced GEM-refractory PC who received FGS between March 2009 and December 2013 as second-line or third-line treatment at Kyorin University Hospital. We retrospectively reviewed their medical records. All patients had a pathological and clinical diagnosis of PC. Informed consent was obtained from each patient, and this retrospective study was approved by the independent ethics committee of Kyorin University School of Medicine.
Eligibility
The patient selection criteria for this study were as follows: both a pathological and clinical diagnosis of PC; disease progression under GEM-based chemotherapy; an Eastern Cooperative Oncology Group performance status (PS) of 0–2; good bone marrow function (white blood cell count ≥3,000/mm3, platelet count ≥75,000/mm3, and hemoglobin ≥8.0 g/dl); renal function (serum creatinine ≤1.5 mg/dl); and liver function (total bilirubin ≤2.0 mg/dl and transaminase levels ≤5 times the upper limit of the respective normal ranges). Patients who had obstructive jaundice were eligible, but only after their serum transaminase levels had decreased to within five times the upper normal limit after biliary drainage. Exclusion criteria were as follows: severe complications, such as active infection, uncontrolled diabetes, massive pleural effusion or ascites, active concomitant malignancy, or severe drug hypersensitivity.
Treatment
GEM was administered every 2 weeks by FDR intravenous infusion of 1,200 mg/m2/120 min on day 1. S-1 was administered orally twice daily on day 1 to day 7, followed by a 1-week rest. The initial dose was determined according to the body surface area (BSA) as follows: BSA < 1.25 m2, 80 mg/day; 1.25 m2 ≤ BSA < 1.50 m2, 100 mg/day; and BSA ≥ 1.50 m2, 120 mg/day. Treatment cycles were repeated every 2 weeks until disease progression or unacceptable toxicity occurred.
Evaluation
Tumor response was assessed approximately every 2 months by contrast-enhanced computed tomography according to the Response Evaluation Criteria in Solid Tumors (RECIST, version 1.1). Toxicity was evaluated according to the Common Terminology Criteria for Adverse Events (CTCAE) version 4.0. Laboratory variables were initially recorded as continuous variables, and later dichotomized according to the median and reference value of each variable. mGPS was constructed, using C-reactive protein and albumin, as follows: Patients with both elevated C-reactive protein (≥1.0 mg/dl) and low albumin (<3.5 g/dl) were allocated a score of 2; patients in whom only C-reactive protein was elevated (≥1.0 mg/dl) were allocated a score of 1, and those with normal C-reactive protein were allocated a score of 0 [11].
Statistical analysis
PFS was counted from the date of treatment initiation to the date of documentation of disease progression or death, and OS was counted from the date of treatment initiation to the date of death or the last follow-up. OS and PFS were calculated using the Kaplan–Meier method. Subgroup analyses were evaluated with the log-rank test, and prognostic factors were identified by univariate analysis. Multivariate analysis was carried out using stepwise Cox proportional hazards regression modeling to identify independent prognostic factors. For the analysis of factors predictive for response to FGS, the univariate relationship between each clinical variable and the achievement of partial response was evaluated using Pearson’s Chi-square test or Fisher’s exact probability test. These variables were also evaluated by a multivariate logistic regression model using backward stepwise selection. The variables with p values <0.1 were selected for multivariate analysis. P values <0.05 were considered statistically significant. The SPSS statistical software program (version 20.0; SPSS, Chicago, IL, USA) was used for all statistical analyses.
Results
Between March 2009 and December 2013, 61 patients with GEM-refractory PC received FGS. The patient characteristics of the subjects are shown in Table 1. Of the 61 patients, the median age was 63 years, 40 (66 %) were male, 58 (95 %) had an ECOG PS of 0–1, and 60 (98 %) had metastatic disease. Disease progression had been confirmed before FGS in all patients. All patients had received prior GEM-based therapy. Before FGS, 44 (72 %) received one regimen, and 17 (28 %) received two regimens. As for prior treatment regimens, 29 (48 %) had received S-1 as monotherapy or GEM plus S-1 combination therapy. Median time to treatment failure of prior treatment was 6.3 months (range 0.5–32.4).
A total of 542 courses were administered, with a median of five courses (range 1–62). Dose reduction in GEM and S-1 because of adverse events was conducted in 11 (18.0 %) and 12 (19.7 %) patients, respectively. A rest period of more than 14 days during treatment was required in 22 (36.1 %) patients. The relative dose intensity for GEM and S-1 was 92.6 and 92.3 %, respectively. FGS was discontinued in 56 (91.8 %) patients because of disease progression and in five (8.2 %) patients because of adverse events (Grade 3 cholangitis in two patients, grade 3 interstitial lung disease in one patient, grade 3 stroke in one patient, and grade 3 sick sinus syndrome in one patient). All the patients had died at the time of analysis.
After FGS treatment failure, 17 patients (27.9 %) received chemotherapy: paclitaxel in five patients, clinical trial drugs in four patients, GEM monotherapy in four patients, and others in four patients.
Toxicity
The toxic effects are summarized in Table 2. Hematologic and non-hematologic toxicity were generally mild, with grade 3 neutropenia observed in nine patients (14.8 %), grade 3 diarrhea in two patients (3.3 %), grade 3 anorexia in only one patient (1.6 %), and grade 3 fatigue in only one patient (1.6 %). Grade 3 stroke, which was irreversible, occurred in one patient (1.6 %). Other than this case, all of the adverse events were reversible. There were no treatment-related deaths.
Efficacy
Eight (13.1 %) patients showed a partial response and 22 (36.1 %) showed stable disease, resulting in an overall objective response rate of 13.1 % and a disease control rate of 49.2 %. The median OS time was 6.0 months (95 % CI 3.6–8.4), and the median PFS time was 2.7 months (95 % CI 1.9–3.5) (Fig. 1). The median OS time after the start of first-line therapy was 15.4 months.
Prognostic factors
The median survival time and p values for univariate analysis are shown in Table 3. Among these variables, ECOG performance status (PS) >0, the presence of ascites, serum carcinoembryonic antigen (CEA) level >10 ng/ml, serum carbohydrate antigen 19-9(CA19-9) level >2,000 IU/ml, serum alkaline phosphatase level (ALP) >500 IU/ml, serum albumin level (ALB) <3.5 g/dl, serum C-reactive protein (CRP) level ≥1.0 g/dl, and a high mGPS were significantly associated with poor survival. A previous history of S-1 administration was not a prognostic factor. The results of the Cox proportional hazards model are shown in Table 4. High mGPS, ECOG PS >0, and CA19-9 level >2,000 IU/ml were independently associated with a poor outcome.
Predictive factors
The relationships between clinical factors and the attainment of partial response to FGS were evaluated. ECOG PS >0 (p = 0.103), site of primary lesion(p = 0.588), number of prior chemotherapy regimens (p = 0.607), history of S-1 administration (p = 0.162), time to treatment failure of prior treatment (p = 0.548), the presence of liver metastasis (p = 0.346), the presence of lung metastasis (p = 0.281), the presence of ascites (p = 0.608), CEA level >10 ng/ml (p = 0.452), CA19-9 level >2,000 IU/ml (p = 0.588), ALP > 500 IU/ml (p = 0.128), ALB < 3.5 g/dl (p = 0.136), CRP level ≥1.0 g/dl (p = 0.281), and a high mGPS (p = 0.153) were not significantly associated with response to FGS. There were no variables with p values <0.1 selected for multivariate analysis.
Discussion
This retrospective study of FGS in patients with GEM-refractory PC demonstrated an ORR of 13 %, DCR of 49 %, and median PFS and OS of 2.7 and 6.0 months, respectively. FGS showed efficacy in both S-1-naïve and non-naïve patients in this study. We explored the independent variables associated with survival in a salvage chemotherapy setting for advanced PC. This study demonstrated that the inflammation-based prognostic score (mGPS) was independently associated with survival in patients with GEM-refractory advanced PC receiving salvage chemotherapy.
In regard to treatment for GEM-refractory PC, the results of a randomized trial comparing best supportive care (BSC) versus oxaliplatin, fluorouracil, and folinic acid (OFF) indicated the benefit of second-line chemotherapy as compared to BSC alone for patients with GEM-refractory advanced pancreatic cancer. Median second-line survival time was 4.8 months for OFF treatment and 2.3 months for BSC alone [12]. However, since the patient number was small (n = 46), OFF has not been recognized as standard salvage chemotherapy in patients with advanced pancreatic cancer. Thus, no standard salvage chemotherapy has been established. Several clinical trials (mainly phase II) of oral fluoropyrimidine monotherapy such as S-1 have been conducted in patients with advanced PC after failure of first-line GEM or a GEM-based combination regimen [6, 13–16]. Median PFS time and median OS time of oral fluoropyrimidine monotherapy were 2.1–4.1 and 4.5–7.6 months (Table 5), which are almost the same as the results of a previous prospective study of FGS [7]. As FOLFIRINOX regimen demonstrated survival benefit over GEM in first-line setting, it could be promising salvage chemotherapy for GEM-refractory patients. Although there is no prospective study using FOLFIRINOX in second-line setting. A retrospective analysis of 27 patients with GEM-refractory PC showed median time to progression of 5.4 months, and median OS was 8.5 months [17]. Another retrospective from Korea assessed 18 patients with GEM-refractory PC noted progression-free survival of 2.8 months and overall survival of 8.4 months [18]. These results suggest the modest clinical activity regarding efficacy with the FOLFIRINOX regimen as a second-line treatment. However, FOLFIRINOX is a potentially highly toxic combination of drugs with serious side effects, and only patients with good performance status are candidates for the regimen even in the first-line setting. Significant toxicity is a concern with FOLFIRINOX in any setting. Prospective studies are needed to better define risks and to determine FOLFIRINOX in the salvage setting.
Whether gemcitabine as FDR infusion is active even after progression during treatment with standard 30-min administration of GEM was the critical clinical question examined in this study. Differentiation between the relative roles of GEM and S-1 in overcoming tumor resistance is difficult. This retrospective study included patients with a history of S-1 administration. Subgroup analysis showed that a history of S-1 administration was not a significant prognostic factor (p = 0.842). This might suggest that FDR infusion of gemcitabine is efficacious ever after failure of standard GEM-based regimens.
Regarding toxicity, grade 3–4 adverse events were not frequent. One death was observed after grade 3 stroke, in a patient with other risk factors, such as age of 82 years and poor performance status. Other than this event, most episodes were reversible, and treatment was generally well tolerated in this study. The median relative dose intensity of GEM and S-1 was 92.6 and 92.3 %, respectively, indicating that treatment was carried out as scheduled in most patients. The safety profile in this study suggests that FGS can be safely administered to patients with PC even in a salvage setting, at least in selected populations. Since the FGS regimen was applied in a practical setting in this study, physical examination and laboratory tests usually were not conducted on day 8. The biweekly schedule allows enough time for recovery from myelosuppression and non-hematologic toxicity before the following cycle, enabling patients to receive treatment as scheduled.
Subgroup analysis of this study showed that high mGPS, high CA19-9 level, and poor PS were independently associated with a poor outcome. Previous reports indicated that PS, CRP, ALB, and inflammation-based prognostic score were important prognostic factors in a first-line setting [19–22]. mGPS was reported to be identified as an independent predictor of survival in patients undergoing potentially curative pancreatic resection [23]. It is now widely accepted that inflammation-based prognostic score is a reliable indicator of survival for several malignant tumors [10, 11]. Our results suggested that it is also an important prognostic factor in the setting of salvage chemotherapy for advance pancreatic cancer.
It is important to point out the limitations of this retrospective study. Patients who received FGS may have been more fit, better able to tolerate it and therefore more likely to derive benefit from it. In addition, the gap between the median OS time and the median PFS time in the present study was relatively large. In this study, 27.9 % of patients received chemotherapy after failure of FGS. Post-treatment, including paclitaxel and clinical trial drugs may prolong the survival of selected patients. Although the reason for this gap is unknown, bias arising from the selection of patients with a good general condition may explain these findings. On the other hand, this retrospective study included patients after failure of second-line chemotherapy as well as those after failure of first-line chemotherapy. It thus seems that the patient backgrounds were rather poor when compared to those in recent phase II trials [6, 7, 13, 15].
In conclusion, FGS as salvage chemotherapy in patients with GEM-refractory advanced PC might be effective and well tolerated in a practical setting. Furthermore, the FGS regimen might possibly show some benefit in patients even after both GEM and S-1 failure. These results suggest that it would be of value to further investigate FGS in a clinical trial in patients with GEM-refractory pancreatic cancer. mGPS is simple and useful as a novel predictor of survival for patients with GEM-refractory advanced PC. mGPS is helpful for planning salvage treatment for these patients.
References
Burris HA III, Moore MJ, Andersen J, Green MR, Rothenberg ML, Modiano MR, Cripps MC, Portenoy RK, Storniolo AM, Tarassoff P, Nelson R, Dorr FA, Stephens CD, Von Hoff DD (1997) Improvements in survival and clinical benefit with gemcitabine as first-line therapy for patients with advanced pancreas cancer: a randomized trial. J Clin Oncol 15(6):2403–2413
Moore MJ, Goldstein D, Hamm J, Figer A, Hecht JR, Gallinger S, Au HJ, Murawa P, Walde D, Wolff RA, Campos D, Lim R, Ding K, Clark G, Voskoglou-Nomikos T, Ptasynski M, Parulekar W (2007) Erlotinib plus gemcitabine compared with gemcitabine alone in patients with advanced pancreatic cancer: a phase III trial of the National Cancer Institute of Canada Clinical Trials Group. J Clin Oncol 25(15):1960–1966. doi:10.1200/jco.2006.07.9525
Von Hoff DD, Ervin T, Arena FP, Chiorean EG, Infante J, Moore M, Seay T, Tjulandin SA, Ma WW, Saleh MN, Harris M, Reni M, Dowden S, Laheru D, Bahary N, Ramanathan RK, Tabernero J, Hidalgo M, Goldstein D, Van Cutsem E, Wei X, Iglesias J, Renschler MF (2013) Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med 369(18):1691–1703. doi:10.1056/NEJMoa1304369
Ueno H, Ioka T, Ikeda M, Ohkawa S, Yanagimoto H, Boku N, Fukutomi A, Sugimori K, Baba H, Yamao K, Shimamura T, Sho M, Kitano M, Cheng AL, Mizumoto K, Chen JS, Furuse J, Funakoshi A, Hatori T, Yamaguchi T, Egawa S, Sato A, Ohashi Y, Okusaka T, Tanaka M (2013) Randomized phase III study of gemcitabine plus S-1, S-1 alone, or gemcitabine alone in patients with locally advanced and metastatic pancreatic cancer in Japan and Taiwan: GEST Study. J Clin Oncol 31(13):1640–1648. doi:10.1200/jco.2012.43.3680
Conroy T, Desseigne F, Ychou M, Bouche O, Guimbaud R, Becouarn Y, Adenis A, Raoul JL, Gourgou-Bourgade S, de la Fouchardiere C, Bennouna J, Bachet JB, Khemissa-Akouz F, Pere-Verge D, Delbaldo C, Assenat E, Chauffert B, Michel P, Montoto-Grillot C, Ducreux M (2011) FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med 364(19):1817–1825. doi:10.1056/NEJMoa1011923
Morizane C, Okusaka T, Furuse J, Ishii H, Ueno H, Ikeda M, Nakachi K, Najima M, Ogura T, Suzuki E (2009) A phase II study of S-1 in gemcitabine-refractory metastatic pancreatic cancer. Cancer Chemother Pharmacol 63(2):313–319. doi:10.1007/s00280-008-0741-7
Morizane C, Okusaka T, Ueno H, Kondo S, Ikeda M, Furuse J, Shinichi O, Nakachi K, Mitsunaga S, Kojima Y, Suzuki E, Ueno M, Yamaguchi T (2012) Phase I/II study of gemcitabine as a fixed dose rate infusion and S-1 combination therapy (FGS) in gemcitabine-refractory pancreatic cancer patients. Cancer Chemother Pharmacol 69(4):957–964. doi:10.1007/s00280-011-1786-6
Tempero M, Plunkett W, Ruiz Van Haperen V, Hainsworth J, Hochster H, Lenzi R, Abbruzzese J (2003) Randomized phase II comparison of dose-intense gemcitabine: 30-min infusion and fixed dose rate infusion in patients with pancreatic adenocarcinoma. J Clin Oncol 21(18):3402–3408. doi:10.1200/jco.2003.09.140
Poplin E, Feng Y, Berlin J, Rothenberg ML, Hochster H, Mitchell E, Alberts S, O’Dwyer P, Haller D, Catalano P, Cella D, Benson AB 3rd (2009) Phase III, randomized study of gemcitabine and oxaliplatin versus gemcitabine (fixed-dose rate infusion) compared with gemcitabine (30-min infusion) in patients with pancreatic carcinoma E6201: a trial of the Eastern Cooperative Oncology Group. J Clin Oncol 27(23):3778–3785. doi:10.1200/jco.2008.20.9007
Forrest LM, McMillan DC, McArdle CS, Angerson WJ, Dunlop DJ (2003) Evaluation of cumulative prognostic scores based on the systemic inflammatory response in patients with inoperable non-small-cell lung cancer. Br J Cancer 89(6):1028–1030. doi:10.1038/sj.bjc.6601242
Proctor MJ, Morrison DS, Talwar D, Balmer SM, O’Reilly DS, Foulis AK, Horgan PG, McMillan DC (2011) An inflammation-based prognostic score (mGPS) predicts cancer survival independent of tumour site: a Glasgow Inflammation Outcome Study. Br J Cancer 104(4):726–734. doi:10.1038/sj.bjc.6606087
Pelzer U, Schwaner I, Stieler J, Adler M, Seraphin J, Dorken B, Riess H, Oettle H (2011) Best supportive care (BSC) versus oxaliplatin, folinic acid and 5-fluorouracil (OFF) plus BSC in patients for second-line advanced pancreatic cancer: a phase III-study from the German CONKO-study group. Eur J Cancer 47(11):1676–1681. doi:10.1016/j.ejca.2011.04.011
Sudo K, Yamaguchi T, Nakamura K, Denda T, Hara T, Ishihara T, Yokosuka O (2011) Phase II study of S-1 in patients with gemcitabine-resistant advanced pancreatic cancer. Cancer Chemother Pharmacol 67(2):249–254. doi:10.1007/s00280-010-1311-3
Todaka A, Fukutomi A, Boku N, Onozawa Y, Hironaka S, Yasui H, Yamazaki K, Taku K, Machida N, Sakamoto T, Tomita H (2010) S-1 monotherapy as second-line treatment for advanced pancreatic cancer after gemcitabine failure. Jpn J Clin Oncol 40(6):567–572. doi:10.1093/jjco/hyq005
Boeck S, Wilkowski R, Bruns CJ, Issels RD, Schulz C, Moosmann N, Laessig D, Haas M, Golf A, Heinemann V (2007) Oral capecitabine in gemcitabine-pretreated patients with advanced pancreatic cancer. Oncology 73(3–4):221–227. doi:10.1159/000127413
Takahara N, Isayama H, Nakai Y, Sasaki T, Hamada T, Uchino R, Mizuno S, Miyabayashi K, Kogure H, Yamamoto N, Sasahira N, Hirano K, Ijichi H, Tateishi K, Tada M, Koike K (2013) A retrospective study of S-1 and oxaliplatin combination chemotherapy in patients with refractory pancreatic cancer. Cancer Chemother Pharmacol 72(5):985–990. doi:10.1007/s00280-013-2278-7
Assaf E, Verlinde-Carvalho M, Delbaldo C, Grenier J, Sellam Z, Pouessel D, Bouaita L, Baumgaertner I, Sobhani I, Tayar C, Paul M, Culine S (2011) 5-fluorouracil/leucovorin combined with irinotecan and oxaliplatin (FOLFIRINOX) as second-line chemotherapy in patients with metastatic pancreatic adenocarcinoma. Oncology 80(5–6):301–306. doi:10.1159/000329803
Lee MG, Lee SH, Lee SJ, Lee YS, Hwang JH, Ryu JK, Kim YT, Kim DU, Woo SM (2013) 5-Fluorouracil/leucovorin combined with irinotecan and oxaliplatin (FOLFIRINOX) as second-line chemotherapy in patients with advanced pancreatic cancer who have progressed on gemcitabine-based therapy. Chemotherapy 59(4):273–279. doi:10.1159/000356158
Tanaka T, Ikeda M, Okusaka T, Ueno H, Morizane C, Hagihara A, Iwasa S, Kojima Y (2008) Prognostic factors in Japanese patients with advanced pancreatic cancer treated with single-agent gemcitabine as first-line therapy. Jpn J Clin Oncol 38(11):755–761. doi:10.1093/jjco/hyn098
Yi JH, Lee J, Park SH, Lee KT, Lee JK, Lee KH, Choi DW, Choi SH, Heo JS, Lim do H, Park YS, Lim HY, Kang WK, Park K, Park JO (2011) A prognostic model to predict clinical outcomes with first-line gemcitabine-based chemotherapy in advanced pancreatic cancer. Oncology 80(3–4):175–180. doi:10.1159/000328449
Shimoda M, Katoh M, Kita J, Sawada T, Kubota K (2010) The Glasgow prognostic score is a good predictor of treatment outcome in patients with unresectable pancreatic cancer. Chemotherapy 56(6):501–506. doi:10.1159/000321014
Glen P, Jamieson NB, McMillan DC, Carter R, Imrie CW, McKay CJ (2006) Evaluation of an inflammation-based prognostic score in patients with inoperable pancreatic cancer. Pancreatology 6(5):450–453. doi:10.1159/000094562
La Torre M, Nigri G, Cavallini M, Mercantini P, Ziparo V, Ramacciato G (2012) The Glasgow prognostic score as a predictor of survival in patients with potentially resectable pancreatic adenocarcinoma. Ann Surg Oncol 19(9):2917–2923. doi:10.1245/s10434-012-2348-9
Conflict of interest
Junji Furuse receives research funding and honoraria from Taiho Pharmaceutical Co. and Eli Lilly.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kasuga, A., Okano, N., Naruge, D. et al. Retrospective analysis of fixed dose rate infusion of gemcitabine and S-1 combination therapy (FGS) as salvage chemotherapy in patients with gemcitabine-refractory advanced pancreatic cancer: inflammation-based prognostic score predicts survival. Cancer Chemother Pharmacol 75, 457–464 (2015). https://doi.org/10.1007/s00280-014-2665-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-014-2665-8