Abstract
Purpose
Neuroblastoma (NB) is one of the most common and deadly pediatric solid tumors. NB is characterized by clinical heterogeneity, from spontaneous regression to relentless progression despite intensive multimodality therapy. There is compelling evidence that members of the tropomyosin receptor kinase (Trk) family play important roles in these disparate clinical behaviors. Indeed, TrkB and its ligand, brain-derived neurotrophic factor (BDNF), are expressed in 50–60 % of high-risk NBs. The BDNF/TrkB autocrine pathway enhances survival, invasion, metastasis, angiogenesis and drug resistance.
Methods
We tested a novel pan-Trk inhibitor, GNF-4256 (Genomics Institute of the Novartis Research Foundation), in vitro and in vivo in a nu/nu athymic xenograft mouse model to determine its efficacy in inhibiting the growth of TrkB-expressing human NB cells (SY5Y-TrkB). Additionally, we assessed the ability of GNF-4256 to enhance NB cell growth inhibition in vitro and in vivo, when combined with conventional chemotherapeutic agents, irinotecan and temozolomide (Irino–TMZ).
Results
GNF-4256 inhibits TrkB phosphorylation and the in vitro growth of TrkB-expressing NBs in a dose-dependent manner, with an IC50 around 7 and 50 nM, respectively. Furthermore, GNF-4256 inhibits the growth of NB xenografts as a single agent (p < 0.0001 for mice treated at 40 or 100 mg/kg BID, compared to controls), and it significantly enhances the antitumor efficacy of irinotecan plus temozolomide (Irino–TMZ, p < 0.0071 compared to Irino–TMZ alone).
Conclusions
Our data suggest that GNF-4256 is a potent and specific Trk inhibitor capable of significantly slowing SY5Y-TrkB growth, both in vitro and in vivo. More importantly, the addition of GNF-4256 significantly enhanced the antitumor efficacy of Irino–TMZ, as measured by in vitro and in vivo growth inhibition and increased event-free survival in a mouse xenograft model, without additional toxicity. These data strongly suggest that inhibition of TrkB with GNF-4256 can enhance the efficacy of current chemotherapeutic treatment for recurrent/refractory high-risk NBs with minimal or no additional toxicity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Neuroblastoma (NB) is a common childhood tumor of the peripheral nervous system. Genomic and biological features can predict NB tumor behavior and outcome, but high-risk tumors, especially those in patients over the age of 18 months, are hard to cure. Despite maximally intensive, multimodality therapy, including stem cell transplant, less than 50 % of patients are cured, so more effective and less toxic therapies are greatly needed. There is growing interest in therapies that target particular genes, proteins and pathways that contribute to malignancy [1–3], and increasing evidence suggests that members of the tropomyosin receptor kinase (Trk) family play important roles in NB behavior [4–7].
We and others have shown that TrkA, the receptor for nerve growth factor (NGF), is expressed on most favorable tumors, and the NGF/TrkA pathway may be involved in the spontaneous regression or differentiation seen in favorable NBs, especially in infants [8–12]. Conversely, TrkB and its primary ligand, brain-derived neurotrophic factor (BDNF), are expressed in many unfavorable NBs, and the autocrine activation of this pathway contributes to aggressive behavior, such as enhanced survival, invasion, metastasis, angiogenesis and drug resistance [13–19]. Therefore, targeting this pathway with selective Trk receptor inhibitors, alone or in combination with other agents, should be an effective and relatively nontoxic approach to treat aggressive NBs [2].
Lestaurtinib (CEP-701, Cephalon, Inc.) was the first Trk inhibitor to be developed for the treatment of NBs [14, 20–22]. Indeed, this agent was used in a Phase 1 clinical trial for recurrent/refractory NBs [23]. Although 8/16 (50 %) of patients treated at a biologically effective dose had durable responses lasting more than 10 months on average [23], lestaurtinib is no longer being supported for clinical applications. Newer agents have been developed that are more potent and selective for the Trk family receptors [24–26], but none of these have been carried forward into clinical trials for NB. Thus, there is still a critical need for the exploration of Trk-selective inhibitors in NBs and other cancers with evidence of Trk activation.
We have evaluated the efficacy of a novel, Trk-selective inhibitor, GNF-4256, against TrkB-expressing NB cells in vitro and in vivo in a mouse xenograft model. GNF-4256 inhibits TrkB phosphorylation and the in vitro growth of TrkB-expressing NBs in a dose-dependent manner. Furthermore, GNF-4256 inhibits the growth of NB xenografts as a single agent, and it significantly enhances the antitumor efficacy of irinotecan plus temozolomide (Irino–TMZ). Our data strongly support the development of GNF-4256 or other Trk-selective inhibitors for the treatment of NB and other cancers with Trk activation.
Materials and methods
Compounds
GNF-4256 was designed and synthesized by the Genomics Institute of the Novartis Research Foundation (GNF) as a novel, selective and potent pan-Trk inhibitor. The antiproliferative effects of GNF-4256 were determined in Ba/F3 assays where Ba/F3 cells were rendered TRKA, TRKB and TRKC dependent and IL-3 independent by overexpressing the constitutively active Tel-TRKA, Tel-TRB and Tel-TRKC fusion, respectively. In these assays, GNF-4256 was shown to inhibit Ba/F3-Tel-TRKA, TRKB and TRKC with an IC50 less than 20 nM, while there was no activity in the parental Ba/F3 cells grown in the presence of IL-3 (15 nM for TrkA, 7 nM for TrkB, 2 nM for TrkC). Similar potency was obtained in biochemical assays using the Caliper method with recombinant TRKA, B and C kinase domains [27]. The biochemical kinase selectivity was evaluated by testing GNF-4256 on a panel of 59 kinases, and the cellular selectivity was evaluated on a panel of 36 tyrosine kinases (Supplemental Tables S1 and S2). Overall, GNF-4256 showed very high selectivity for Trks, with only some marginal activity against ROS confirmed in the cellular assay (IC50 = 3.8 μM). GNF-4256 was formulated in 0.5 % Methylcellulose + 0.5 % Tween-80 suspension in distilled water at concentrations of 4 or 10 mg/ml. Fresh batches of suspension were made for each week of in vivo dosing. Normal saline was used as the vehicle control. Irinotecan (Camptostar; Irino) and temozolomide (Temodar; TMZ) were obtained through the pharmacy at the Children’s Hospital of Philadelphia (CHOP).
Cell lines
In vitro studies were performed using SY5Y-TrkB, a subclone of the SH-SY5Y NB cell line that was stably transfected with a TrkB expression vector [14, 22, 24]. The SY5Y parental cell line was used as a Trk-null control. Cells were grown in RPMI-1640 medium (Gibco) containing 10 % fetal bovine serum (Cellgro), 0.4 mg/ml Pen/Strep (Gibco) and 0.3 mg/ml G418 (SY5Y-TrkB cells only, to select for TrkB expression) in 150 cm3 Corning culture flasks. Cells were maintained at 37 °C, 5 % CO2 and harvested using 0.2 % tetrasodium EDTA in phosphate-buffered saline (PBS). For in vivo studies, SY5Y-TrkB cells were grown and harvested as described above.
In vitro studies
To determine the efficacy and specificity of GNF-4256 for TrkB-expressing tumors, SY5Y Trk-null and SY5Y-TrkB cells were grown in 10 cm3 dishes to 70–80 % confluency with standard culture medium. Cells were treated with a concentration of GNF-4256 (1–500 nM) for 1 h and then stimulated with the TrkB ligand, BDNF (100 ng/mL, PeproTech, Rocky Hill, NJ), for 15 min. Cells were then harvested for protein extraction. Trk expression analysis was performed via Western blot using anti-phospho-Trk antibody [Phospho-Trk, Tyr-490 antibody; Cell Signaling Technologies (CST), Danvers, MA] or anti-Pan-Trk antibody (Santa Cruz Biotechnology Inc., Santa Cruz, CA). Downstream signaling inhibition was analyzed using anti-phospho-AKT (CST) and anti-phospho-ERK1/2 antibodies (CST). Blots were reprobed with anti-AKT and anti-ERK1/2 antibodies (CST) to determine uniformity of loading.
Sulphorhodamine B (SRB) assays were performed to determine the effect of GNF-4256 on cell viability and growth. Cells were plated at 5 × 103 cells per well in 96-well Corning plates. Twenty-four hours later, cells were treated with varying concentrations of GNF-4256 for 1 h, followed by cell growth stimulation using 100 ng/ml BDNF. Cells were harvested at 24, 48 and 72 h post-stimulation. Cells were fixed, stained and quantified according to standard SRB protocols. All in vitro experiments were done in triplicate and performed at least three times.
Animals
Six-week-old athymic (nu/nu) mice were obtained from Jackson Laboratories. Mice were housed in a temperature and 12-h light-controlled environment at five animals per cage. We assessed toxicity by daily behavior observation, twice weekly weight measurements, and blood counts before and after treatment. Tissues of treated mice were assessed for gross toxicity post-killing. Abnormal tissues, if found, were examined microscopically. The Institutional Animal Care Committee of the Joseph Stokes, Jr. Research Institute at CHOP, approved the animal studies described.
In vivo studies
Animals were injected subcutaneously in the flank with 1 × 107 SY5Y-TrkB cells in 0.1 ml of Matrigel (BD Bioscience, Palo Alto, CA). Tumors were measured twice per week in three dimensions, and total volume was calculated by: \(\frac{(0.523 \times L \times W \times W)}{1000}\). Oral treatment with GNF-4256 and/or Irino–TMZ began when average tumor size reached 0.2 cm3 (at least 10 mice per arm). Body weights were measured twice weekly, and drug doses were adjusted accordingly. GNF-4256 was administered twice daily (8 h apart), 7 days per week, by oral gavage at final concentrations of either 40 or 100 mg/kg. For combination studies, Irino was administered at 0.63 mg/kg once daily, 5 days a week (Monday to Friday), by oral gavage. TMZ was given at a dose of 7.5 mg/kg once daily, 5 days a week, by oral gavage (Monday to Friday). The same doses of Irino and TMZ were used when administered in combination with GNF-4256. Irino and TMZ were resuspended in normal saline for oral gavage. The doses used for Irino and TMZ were based on previously published studies [28, 29] and our own experience with chemotherapeutic treatment of our xenograft mouse model. Drug administration continued twice daily, 7 days a week (GNF-4256) or once daily 5 days a week (Irino–TMZ) for 4 weeks, or until tumors reached 3 cm3. Retro-orbital and terminal bleeds were used for blood counts and pharmacokinetic studies.
Pharmacokinetic/pharmacodynamic studies
For PK analysis, GNF-4256 was administered at 40 or 100 mg/kg BID for 2 weeks (30 animals per arm). At the end of the 2-week-long experiment, animals were killed at 1, 3, 8, 9 (1 h post-afternoon dose) and 24 h (16 h post-afternoon dose) post-morning dose. Terminal blood and tumor samples were collected from three animals at each time point. Blood samples (~80 μl) were collected in heparinized tubes and centrifuged immediately to separate the plasma. The tumor samples were snap-frozen until analysis. Plasma and tumor samples were also collected from a group of animals that only received 1 day of dosing (both morning and afternoon dose) to establish Day 1 PK. These data were compared with the terminal PK to establish if changes in exposures had occurred during the two-week period. The drug concentrations were determined using a liquid chromatography/mass spectrometry (LC/MS/MS) method with a Zorbax SB-C8 analytical column (2.1 × 30 mm, 3.5 μm, Agilent Technologies Inc., Palo Alto, CA, USA). The lower limits of quantification were 1 ng/ml for plasma and 5 ng/g for tissue. Pharmacokinetic parameters were calculated by noncompartmental regression analysis using Phoenix WinNonlin 6.0 software (Pharsight, USA). The highest concentration (C max) and the area under the concentration–time curve (AUC0–24 h) were reported.
Statistical analysis
A linear mixed-effects model was used to test the difference in the rate of tumor volume change over time between groups. The model included group, day and group-by-day interaction as fixed effects and included a random intercept and a random slope for each mouse. Event-free survival (EFS) curves were estimated using Kaplan–Meier method and compared using a log-rank test.
Results
Effect of GNF-4256 on TrkB-expressing SH-SY5Y NB cells in vitro
We first tested the efficacy of GNF-4256 in inhibiting TrkB phosphorylation in our SH-SY5Y-TrkB-transfected NB cell lines. In control SY5Y-TrkB cells, TrkB phosphorylation was seen at maximal intensity 15 min after BDNF addition. In the GNF-4256-treated samples, there was a dose-dependent inhibition of ligand-induced phosphorylation (Fig. 1a). The observed IC50 was between 3 and 10 nM, and the IC90 was between 30 and 100 nM concentrations, with complete inhibition by 200 nM.
a Effect of GNF-4256 on TrkB phosphorylation induced by BDNF (100 ng/ml). SY5Y human NB cells transfected with TrkB (SY5Y-TrkB) were exposed to BDNF for 15 min in the absence or presence of increasing concentrations of GNF-4256. 50 % TrkB phosphorylation inhibition was seen between 10 and 30 nM GNF-4256. Complete TrkB inhibition was observed at 200 nM GNF-4256. Similar signaling inhibition was seen with downstream effector proteins, AKT and Erk1/2. b Effect of GNF-4256 on SY5Y-TrkB cell growth. Cells were grown in 96-well plates in the presence or absence (control) of BDNF (100 ng/ml) and increasing concentrations of GNF-4256. Cells harvested, fixed and stained with sulphorhodamine B at 24, 48 and 72 h post-stimulation revealed increasing growth inhibition with increasing concentrations of GNF-4256. An IC50 was observed at 50 nM GNF-4256
Next, we tested the effect of GNF-4256 on parental (Trk-null) SY5Y and SY5Y-TrkB cells to determine its specificity and sensitivity to TrkB inhibition. Increasing concentrations of GNF-4256 had no effect on the growth of SY5Y Trk-null cells using either an RT-CES or SRB assay (data not shown). However, GNF-4256-treated SY5Y-TrkB cells displayed a dose-dependent decrease in cell growth, with increasing concentrations of GNF-4256 by both RT-CES (data not shown) and SRB assays (Fig. 1b). Growth inhibition of SY5Y-TrkB cells was also seen in the absence of exogenous BDNF, but it was more modest (data not shown). There was a 50 % inhibition of cell growth at 50 nM GNF-4256, and growth levels were comparable to SY5Y-TrkB cells in the absence of ligand at 100 nM. These results established that GNF-4256 is a potent and selective inhibitor of TrkB-expressing NB cells.
Effect of GNF-4256 on SY5Y-TrkB NB xenografts
We next investigated the efficacy of GNF-4256 in inhibiting NB cell growth in vivo using a murine xenograft model. When the tumors grew to 0.2 cm3, we initiated treatment (either GNF-4256 at 40 or 100 mg/kg BID or with saline). We treated mice (10 per group) twice a day, 8 h apart, 7 days per week for 4 weeks (or until tumors exceeded 3 cm3). GNF-4256 administered as a single agent at 40 or 100 mg/kg BID significantly slowed tumor growth compared to control animals (p < 0.0001 for both), but there was no significant difference between the two doses of GNF-4256 (Fig. 2a). Similarly, GNF-4256 dosed at 40 or 100 mg/kg provided significant event-free survival (EFS) compared to control animals (p < 0.0025, p < 0.0001, respectively), but no significant difference was seen between the groups treated with different concentrations of GNF-4256 (Fig. 2b).
a Effect of GNF-4256 as a single agent on SY5Y-TrkB xenograft growth. Animals treated with GNF-4256 at either 40 or 100 mg/kg BID had significantly slower-growing tumors than control animals (p < 0.0001 for both), but exhibited no significant difference between each other. b Effect of GNF-4256 on event-free survival (EFS). Animals dosed twice daily with 40 or 100 mg/kg GNF-4256 for 4 weeks, or until tumors reached 3 cm3, had significantly greater EFS over control animals (p < 0.0025, p < 0.0001, respectively). Again, no significant difference was observed between animals dosed with 40 and 100 mg/kg of GNF-4256. c Western analysis of TrkB phosphorylation in GNF-4256-treated tumors. In vitro control SY5Y-TrkB cells exhibited moderate levels of TrkB phosphorylation, which increases after 15 min of exposure to 100 ng/ml BDNF (lanes 1 and 2). Similar levels of steady-state TrkB phosphorylation are observed in vehicle-treated mouse xenografts, whereas mice treated with GNF-4256 at either 40 or 100 mg/kg exhibit almost complete inhibition of phospho-TrkB at 3 and 8 h post-treatment. No significant difference in inhibition is seen between xenografts from mice treated with 40 or 100 mg/kg GNF-4256
We also examined the phosphorylation of TrkB in the vehicle (saline) and GNF-4256-treated tumors. Saline-treated NB xenografts showed substantial phosphorylation, similar to the same cells treated in vitro with BDNF, but all tumors treated with GNF-4256 at either 40 or 100 mg/kg (three samples shown for each dose) had dramatically reduced TrkB auto-phosphorylation (Fig. 2c).
To assess the exposure of GNF-4256 in the plasma and tumor tissues, we next performed a pharmacokinetic analysis. Animals were dosed for either 1 day (Day 1), or for 2 weeks (Day 14) to determine whether changes in exposure occurred over time. Plasma and tumor samples were collected at 1, 3, 8, 9 and 24 h post-dosing on Day 1 and Day 14 of treatment. 9 and 24-h levels were obtained after the second daily dosing. GNF-4256 was absorbed and distributed rapidly into tumor tissue with a T max of 1 h (Fig. 3). GNF-4256 exposure increased under-dose proportionally from 40 mg/kg BID to 100 mg/kg BID: A 2.5-fold increase of dose resulted in 1.6-fold (plasma) to 1.9-fold (tumor) increase in AUC0–24 h (Table 1). Although the AUC0–24 h at 100 mg/kg BID dose was higher than that at 40 mg/kg BID dose, the time of free plasma concentrations above the in vitro IC50 of TrkB (approximately 18 h) on Day 14 was similar (Fig. 3a, b), which could explain the similar in vivo tumor growth inhibition observed with both dose groups (Fig. 2). Consequently, 40 mg/kg BID was established as a sufficient dosing regimen for our NB xenograft model.
a, b Plasma concentration–time plots of GNF-4256 dosed at 40 and 100 mg/kg BID, respectively. Animals were dosed for either 1 day (Day 1), or for 2 weeks (Day 14), and blood and tumor samples were taken at 1, 3, 8, 9 and 24 h post-treatment. 9 and 24-h levels were obtained after the second daily dosing. Plasma concentrations peaked 1 h after dosing (1 and 9 h on graphs) and declined linearly over time. c, d Tumor concentration–time plots of GNF-4256 dosed at 40 and 100 mg/kg BID, respectively. GNF-4256 was absorbed and distributed rapidly into tumor tissue with a T max of 1 h (similar to blood plasma results). Similar drug levels are seen between Day 1 and Day 14 samples, as well as between samples treated with 40 and 100 mg/kg GNF-4256. Both blood serum and tumor samples were harvested and snap-frozen until analysis
Compared to the single-day treatment groups, the plasma and tumor exposures in the animals receiving 2 weeks of treatment were similar, suggesting GNF-4256 was not accumulated after multiple days of dosing (Fig. 3). The tumor and plasma exposure were also similar, suggesting that GNF-4256 has low-to-moderate tumor distribution (Fig. 3). These observations of no accumulation and low-to-moderate tumor distribution were consistent with the PK properties (i.e., short half-life and low volume of the distribution) of GNF-4256 determined in an IV single-dose mouse PK study (data not shown). Importantly, no substantial toxicity was observed in either group.
Effect of combining GNF-4256 with Irino–TMZ in SY5Y-TrkB NB xenografts
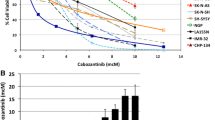
NB patients with recurrent or refractory disease are often treated using a combination of the chemotherapeutic agents, Irino and TMZ. To determine whether co-treatment with GNF-4256 would enhance the therapeutic efficacy of this combination, we first performed an SRB assay in vitro. We treated SY5Y-TrkB cells with either single-agent GNF-4256 (30, 50, 75 nM), Irino–TMZ (3, 100 µM, respectively), or a combination of all three drugs (at different GNF-4256 concentrations) and analyzed cell growth at 24, 48 and 72 h after stimulation with BDNF (Fig. 4). Growth inhibition reached baseline levels (comparable to no BDNF treatment) at 75 nM GNF-4256 alone, and this was similar to treatment with Irino–TMZ. Adding GNF-4256 to Irino–TMZ treatment decreased cell growth significantly below the control cell index, suggesting enhanced cell death with the combination.
Effect of GNF-4256 in combination with chemotherapeutic agents on SY5Y-TrkB cell growth. Cells were grown in 96-well plates in the absence (control) or presence of BDNF (100 ng/ml), along with either single-agent GNF-4256 (30, 50, 75 nM), Irino (3 μM), TMZ (100 μM), Irino–TMZ (3, 100 μM) or a combination of all three drugs (using one of the three GNF-4256 concentrations above). Cells harvested, fixed and stained with sulphorhodamine B at 24, 48 and 72 h post-stimulation revealed that GNF-4256 treatment at 75 nM inhibited cell growth to baseline control levels. GNF-4256 treatment in combination with Irino–TMZ decreased cell growth significantly below the control cell index, suggesting cell death
Based on these results, we wanted to determine whether we could achieve greater in vivo treatment efficacy using co-treatment of GNF-4256 with Irino–TMZ. We treated mice bearing NB xenografts with vehicle, GNF-4256, Irino–TMZ or GNF-4256 plus Irino–TMZ for either 4 weeks, or until tumor sizes exceeded 3 cm3. GNF-4256 was administered orally at 40 mg/kg twice daily, 7 days a week, and Irino–TMZ was administered orally once daily, 5 days a week.
Co-treatment of GNF-4256 with Irino–TMZ resulted in significant slowing of tumor growth (Fig. 5a). The effects of either single-agent GNF-4256 or Irino–TMZ alone were significant compared to vehicle-treated tumors (p < 0.0003, p < 0.0001, respectively), but not significantly different from each other. The combination of GNF-4256 and Irino–TMZ was significantly better than either treatment alone (compared to GNF-4256, p < 0.0001, and to Irino–TMZ, p < 0.0071). Similarly, both single-agent GNF-4256 and Irino–TMZ-treated animals had a significantly better EFS compared to controls (p < 0.0375, p < 0.0095), although they were not significantly different from each other (Fig. 5b). Also, the combination of GNF-4256 with Irino–TMZ was significantly better than either therapy alone (p < 0.0226 and p < 0.0331, respectively).
a Effect of GNF-4256 alone or in combination with Irino–TMZ on SY5Y-TrkB xenografts. Treatment of xenografts with GNF-4256 (40 mg/kg BID) or Irino–TMZ (Irino 0.63 mg/kg QD 5 days/week, TMZ 7.5 mg/kg QD 5 days/week) alone significantly slowed tumor growth compared to vehicle-treated animals (p < 0.0003, p < 0.0001, respectively). Singly treated GNF-4256 tumors did not display significantly different growth patterns than Irino–TMZ-treated tumors. However, the combination of GNF-4256 and Irino–TMZ produced an enhanced tumor growth inhibition response compared to either single-treatment group (p < 0.0001, p < 0.0071, respectively). b Event-free survival (EFS) analysis of combination therapy. Mice were killed when their tumor size exceeded 3 cm3. Both single-therapy groups had a survival advantage over the control group, GNF-4256 40 mg/kg BID (p < 0.0375) and Irino–TMZ (p < 0.0095), but they were not significantly different from each other. The combination therapy, however, provided significantly greater EFS over either single therapy (p < 0.023 and p < 0.033, respectively)
In the combination therapy with Irino–TMZ, we also monitored the plasma and tumor exposure of GNF-4256. The terminal plasma and tumor samples were collected at 1 and 4 h post-dose on the last day of treatment (steady state). Both plasma and tumor concentrations obtained from the single-agent treatment groups were similar to that from the combination treatment group, suggesting that exposure of GNF-4256 was not altered by co-administration of Irino–TMZ (Supplemental Table S3). The effect of GNF-4256 on the exposure of Irino–TMZ was not determined in this combination study.
These data suggest that singly administered GNF-4256 has antitumor efficacy similar to Irino–TMZ in treating TrkB-expressing NB xenografts, and it significantly enhances the efficacy of Irino–TMZ in a murine NB xenograft model without increasing toxicity. Furthermore, we saw no effect on animal weight or behavior, no obvious organ toxicity and no effect on blood counts, suggesting that GNF-4256 is not only effective, but also safe to administer as a Trk inhibitor.
Discussion
NBs are well known for having heterogeneous clinical behavior, from spontaneous regression or differentiation, to relentless progression despite intensive, multimodality therapy. Previously, we and others have demonstrated that the Trk family of neurotrophin receptors plays an important role in this behavior (reviewed in [4–7]). Expression of TrkA is prevalent on biologically favorable neuroblastomas, especially those from infants, and the NGF/TrkA pathway may be responsible for the spontaneous regression or differentiation seen in these tumors [8–12]. Conversely, TrkB and its ligand BDNF are expressed in biologically unfavorable tumors, especially those with MYCN amplification, and this autocrine survival pathway may contribute to enhanced survival, invasion, metastasis, angiogenesis and drug resistance [13–19]. As a result, there has been increasing interest in agents that selectively inhibit the TrkB pathway, either alone or in combination with other agents, to treat recurrent or refractory NBs.
We have shown previously that the Trk inhibitor, lestaurtinib (CEP-701 or related compounds), was effective at inhibiting TrkB autophosphorylation and NB growth in a mouse xenograft model [14, 20–22]. Furthermore, we showed that lestaurtinib, when delivered at biologically relevant doses, produced protracted responses and significantly inhibited NB growth with limited toxicity in a Phase I clinical trial [23]. Unfortunately, lestaurtinib is no longer being supported for clinical applications, so we are exploring novel, second-generation Trk inhibitors as targeted therapy for NBs.
GNF-4256 is a novel, selective pan-Trk inhibitor discovered by the Genomic Institute of the Novartis Research Foundation. GNF-4256 selectively inhibits all Trk receptors (TrkA, TrkB, TrkC) with similar potency at nanomolar concentrations, but no other receptor tyrosine kinases are inhibited at these levels. Furthermore, it is formulated as an oral agent, making it suitable for clinical administration. Thus, GNF-4256 is an ideal candidate for further investigation as a treatment for NBs and other tumors in which Trk family genes are oncogenic drivers.
We have demonstrated that GNF-4256 is a potent and selective inhibitor of Trk autophosphorylation and NB tumor growth both in vitro and in vivo, using our TrkB model. Furthermore, GNF-4256 had no effect on the Trk-null parental SY5Y cells, demonstrating that the Trk pathway mediated its antitumor affect. Remarkably, GNF-4256 had similar antitumor potency to the combination of Irino and TMZ, a chemotherapy combination frequently used to treat patients with recurrent or refractory NB. Given that essentially no toxicity was seen in animals treated with 40 mg/kg of GNF-4256, this makes it an attractive agent for treating relapse patients. Moreover, combination therapy of GNF-4256 and Irino–TMZ significantly enhanced the antitumor efficacy over Irino–TMZ alone, presumably by blocking an important survival pathway and inhibiting the consequences of BDNF/TrkB overexpression, such as invasion, metastasis, angiogenesis and drug resistance [13–19].
Although many high-risk NBs have overexpression of BDNF and TrkB, there are a variety of other tumors in children and adults with Trk gene activation. TrkA is activated by translocation with several partner genes in papillary thyroid cancer [30–33], as well as a subset of lung cancers [34]. It can also be activated by autocrine overexpression in breast, prostate and pancreatic cancers [35–51]. TrkC is activated by translocation in infantile fibrosarcomas, congenital mesoblastic nephromas and secretory breast cancers [52–57], and it can also be activated by autocrine overexpression in medulloblastoma, nasopharyngeal cancer and medullary thyroid cancer [58–63]. To date, TrkB is only activated by autocrine overexpression, in such diseases as anaplastic Wilms tumor, as well as colorectal, gastric, lung, ovarian and hepatocellular cancer [64–73]. Indeed, because of its frequency of activation, TrkB has been proposed as a promising target for cancer therapy [74]. Interestingly, to date, Trk receptors are rarely activated by mutation, although Trk activation occurs in many of the tumors tested.
Thus, given the variety of different tumors showing activation of different Trk genes, targeting Trk receptors with a pan-Trk inhibitor would be of benefit for a variety of cancers in both children and adults. There have been limited trials with Trk inhibitors, at least in children, and so the side effects of inhibiting all Trk receptors is unknown, but the side effects of lestaurtinib in a Phase 1 clinical trial in NB patients were limited to mild, including reversible liver transaminase elevations [23]. Given that GNF-4256 and possibly other second-generation Trk inhibitors are more potent and specific for Trk genes relative to other tyrosine kinases, the further development of this agent and its use in Phase 1 clinical trials is certainly warranted.
Abbreviations
- BDNF:
-
Brain-derived neurotrophic factor
- Irino:
-
Irinotecan
- NGF:
-
Nerve growth factor
- NB:
-
Neuroblastoma
- RT-CES:
-
Real-time cell electrical sensing
- SRB:
-
Sulphorhodamine B
- TMZ:
-
Temozolomide
- Trk:
-
Tropomyosin receptor kinase
References
Brodeur GM (2003) Neuroblastoma: biological insights into a clinical enigma. Nat Rev Cancer 3(3):203–216
Brodeur GM, Iyer R, Croucher JL, Zhuang T, Higashi M, Kolla V (2014) Therapeutic targets for neuroblastomas. Expert Opin Ther Targets 18(3):277–292
Maris JM, Hogarty MD, Bagatell R, Cohn SL (2007) Neuroblastoma. Lancet 369(9579):2106–2120
Brodeur GM, Minturn JE, Ho R, Simpson AM, Iyer R, Varela CR et al (2009) Trk receptor expression and inhibition in neuroblastomas. Clin Cancer Res 15(10):3244–3250
Thiele CJ, Li Z, McKee AE (2009) On Trk—the TrkB signal transduction pathway is an increasingly important target in cancer biology. Clin Cancer Res 15(19):5962–5967
Nakagawara A (2001) Trk receptor tyrosine kinases: a bridge between cancer and neural development. Cancer Lett 169(2):107–114
Brodeur GM, Nakagawara A, Yamashiro DJ, Ikegaki N, Liu XG, Azar CG et al (1997) Expression of TrkA, TrkB and TrkC in human neuroblastomas. J Neurooncol 31(1–2):49–55
Kogner P, Barbany G, Dominici C, Castello MA, Raschella G, Persson H (1993) Coexpression of messenger RNA for TRK protooncogene and low affinity nerve growth factor receptor in neuroblastoma with favorable prognosis. Cancer Res 53(9):2044–2050
Nakagawara A, Arima M, Azar CG, Scavarda NJ, Brodeur GM (1992) Inverse relationship between trk expression and N-myc amplification in human neuroblastomas. Cancer Res 52(5):1364–1368
Nakagawara A, Arima-Nakagawara M, Scavarda NJ, Azar CG, Cantor AB, Brodeur GM (1993) Association between high levels of expression of the TRK gene and favorable outcome in human neuroblastoma. N Engl J Med 328(12):847–854
Nakagawara A, Brodeur GM (1997) Role of neurotrophins and their receptors in human neuroblastomas: a primary culture study. Eur J Cancer 33(12):2050–2053
Suzuki T, Bogenmann E, Shimada H, Stram D, Seeger RC (1993) Lack of high-affinity nerve growth factor receptors in aggressive neuroblastomas. J Natl Cancer Inst 85(5):377–384
Acheson A, Conover JC, Fandl JP, DeChiara TM, Russell M, Thadani A et al (1995) A BDNF autocrine loop in adult sensory neurons prevents cell death. Nature 374(6521):450–453 see comments
Ho R, Eggert A, Hishiki T, Minturn JE, Ikegaki N, Foster P et al (2002) Resistance to chemotherapy mediated by TrkB in neuroblastomas. Cancer Res 62(22):6462–6466
Jaboin J, Hong A, Kim CJ, Thiele CJ (2003) Cisplatin-induced cytotoxicity is blocked by brain-derived neurotrophic factor activation of TrkB signal transduction path in neuroblastoma. Cancer Lett 193(1):109–114
Jaboin J, Kim CJ, Kaplan DR, Thiele CJ (2002) Brain-derived neurotrophic factor activation of TrkB protects neuroblastoma cells from chemotherapy-induced apoptosis via phosphatidylinositol 3′-kinase pathway. Cancer Res 62(22):6756–6763
Matsumoto K, Wada RK, Yamashiro JM, Kaplan DR, Thiele CJ (1995) Expression of brain-derived neurotrophic factor and p145TrkB affects survival, differentiation, and invasiveness of human neuroblastoma cells. Cancer Res 55(8):1798–1806
Nakagawara A, Azar CG, Scavarda NJ, Brodeur GM (1994) Expression and function of TRK-B and BDNF in human neuroblastomas. Mol Cell Biol 14(1):759–767
Nakamura K, Martin KC, Jackson JK, Beppu K, Woo CW, Thiele CJ (2006) Brain-derived neurotrophic factor activation of TrkB induces vascular endothelial growth factor expression via hypoxia-inducible factor-1alpha in neuroblastoma cells. Cancer Res 66(8):4249–4255
Evans AE, Kisselbach KD, Liu X, Eggert A, Ikegaki N, Camoratto AM et al (2001) Effect of CEP-751 (KT-6587) on neuroblastoma xenografts expressing TrkB. Med Pediatr Oncol 36(1):181–184
Evans AE, Kisselbach KD, Yamashiro DJ, Ikegaki N, Camoratto AM, Dionne CA et al (1999) Antitumor activity of CEP-751 (KT-6587) on human neuroblastoma and medulloblastoma xenografts. Clin Cancer Res 5(11):3594–3602
Iyer R, Evans AE, Qi X, Ho R, Minturn JE, Zhao H et al (2010) Lestaurtinib enhances the antitumor efficacy of chemotherapy in murine xenograft models of neuroblastoma. Clin Cancer Res 16(5):1478–1485
Minturn JE, Evans AE, Villablanca JG, Yanik GA, Park JR, Shusterman S et al (2011) Phase I trial of lestaurtinib for children with refractory neuroblastoma: a new approaches to neuroblastoma therapy consortium study. Cancer Chemother Pharmacol 68(4):1057–1065
Iyer R, Varela CR, Minturn JE, Ho R, Simpson AM, Light JE et al (2012) AZ64 Inhibits TrkB and enhances the efficacy of chemotherapy and local radiation in neuroblastoma xenografts. Cancer Chemother Pharmacol (in press)
Thress K, Macintyre T, Wang H, Whitston D, Liu ZY, Hoffmann E et al (2009) Identification and preclinical characterization of AZ-23, a novel, selective, and orally bioavailable inhibitor of the Trk kinase pathway. Mol Cancer Ther 8(7):1818–1827
Zage PE, Graham TC, Zeng L, Fang W, Pien C, Thress K et al (2011) The selective Trk inhibitor AZ623 inhibits brain-derived neurotrophic factor-mediated neuroblastoma cell proliferation and signaling and is synergistic with topotecan. Cancer 117(6):1321–1391
Blackwell LJ, Birkos S, Hallam R, Van De Carr G, Arroway J, Suto CM et al (2009) High-throughput screening of the cyclic AMP-dependent protein kinase (PKA) using the caliper microfluidic platform. Methods Mol Biol 565:225–237
Thompson J, Zamboni WC, Cheshire PJ, Richmond L, Luo X, Houghton JA et al (1997) Efficacy of oral irinotecan against neuroblastoma xenografts. Anticancer Drugs 8(4):313–322
Stewart CF, Zamboni WC, Crom WR, Houghton PJ (1997) Disposition of irinotecan and SN-38 following oral and intravenous irinotecan dosing in mice. Cancer Chemother Pharmacol 40(3):259–265
Greco A, Mariani C, Miranda C, Pagliardini S, Pierotti MA (1993) Characterization of the NTRK1 genomic region involved in chromosomal rearrangements generating TRK oncogenes. Genomics 18(2):397–400
Greco A, Miranda C, Pagliardini S, Fusetti L, Bongarzone I, Pierotti MA (1997) Chromosome 1 rearrangements involving the genes TPR and NTRK1 produce structurally different thyroid-specific TRK oncogenes. Genes Chromosomes Cancer 19(2):112–123
Greco A, Roccato E, Pierotti MA (2004) TRK oncogenes in papillary thyroid carcinoma. Cancer Treat Res 122:207–219
Pierotti MA, Bongarzone I, Borrello MG, Mariani C, Miranda C, Sozzi G et al (1995) Rearrangements of TRK proto-oncogene in papillary thyroid carcinomas. J Endocrinol Invest 18(2):130–133
Vaishnavi A, Capelletti M, Le AT, Kako S, Butaney M, Ercan D et al (2013) Oncogenic and drug-sensitive NTRK1 rearrangements in lung cancer. Nat Med 19(11):1469–1472
Davidson B, Reich R, Lazarovici P, Ann Florenes V, Nielsen S, Nesland JM (2004) Altered expression and activation of the nerve growth factor receptors TrkA and p75 provide the first evidence of tumor progression to effusion in breast carcinoma. Breast Cancer Res Treat 83(2):119–128
Descamps S, Lebourhis X, Delehedde M, Boilly B, Hondermarck H (1998) Nerve growth factor is mitogenic for cancerous but not normal human breast epithelial cells. J Biol Chem 273(27):16659–16662
Descamps S, Pawlowski V, Revillion F, Hornez L, Hebbar M, Boilly B et al (2001) Expression of nerve growth factor receptors and their prognostic value in human breast cancer. Cancer Res 61(11):4337–4340
Dolle L, Adriaenssens E, El Yazidi-Belkoura I, Le Bourhis X, Nurcombe V, Hondermarck H (2004) Nerve growth factor receptors and signaling in breast cancer. Curr Cancer Drug Targets 4(6):463–470
Dolle L, El Yazidi-Belkoura I, Adriaenssens E, Nurcombe V, Hondermarck H (2003) Nerve growth factor overexpression and autocrine loop in breast cancer cells. Oncogene 22(36):5592–5601
Jin W, Kim GM, Kim MS, Lim MH, Yun C, Jeong J et al (2010) TrkC plays an essential role in breast tumor growth and metastasis. Carcinogenesis 31(11):1939–1947
Lagadec C, Meignan S, Adriaenssens E, Foveau B, Vanhecke E, Romon R et al (2009) TrkA overexpression enhances growth and metastasis of breast cancer cells. Oncogene 28(18):1960–1970
George DJ, Suzuki H, Bova GS, Isaacs JT (1998) Mutational analysis of the TrkA gene in prostate cancer. Prostate 36(3):172–180
MacGrogan D, Saint-Andre JP, Dicou E (1992) Expression of nerve growth factor and nerve growth factor receptor genes in human tissues and in prostatic adenocarcinoma cell lines. J Neurochem 59(4):1381–1391
Pflug BR, Dionne C, Kaplan DR, Lynch J, Djakiew D (1995) Expression of a Trk high affinity nerve growth factor receptor in the human prostate. Endocrinology 136(1):262–268
Walch ET, Marchetti D (1999) Role of neurotrophins and neurotrophins receptors in the in vitro invasion and heparanase production of human prostate cancer cells. Clin Exp Metastasis 17(4):307–314
Weeraratna AT, Arnold JT, George DJ, DeMarzo A, Isaacs JT (2000) Rational basis for Trk inhibition therapy for prostate cancer. Prostate 45(2):140–148
Miknyoczki SJ, Wan W, Chang H, Dobrzanski P, Ruggeri BA, Dionne CA et al (2002) The neurotrophin-trk receptor axes are critical for the growth and progression of human prostatic carcinoma and pancreatic ductal adenocarcinoma xenografts in nude mice. Clin Cancer Res 8(6):1924–1931
Miknyoczki SJ, Chang H, Klein-Szanto A, Dionne CA, Ruggeri BA (1999) The Trk tyrosine kinase inhibitor CEP-701 (KT-5555) exhibits significant antitumor efficacy in preclinical xenograft models of human pancreatic ductal adenocarcinoma. Clin Cancer Res 5(8):2205–2212
Miknyoczki SJ, Dionne CA, Klein-Szanto AJ, Ruggeri BA (1999) The novel Trk receptor tyrosine kinase inhibitor CEP-701 (KT-5555) exhibits antitumor efficacy against human pancreatic carcinoma (Panc1) xenograft growth and in vivo invasiveness. Ann N Y Acad Sci 880:252–262
Miknyoczki SJ, Lang D, Huang L, Klein-Szanto AJ, Dionne CA, Ruggeri BA (1999) Neurotrophins and Trk receptors in human pancreatic ductal adenocarcinoma: expression patterns and effects on in vitro invasive behavior. Int J Cancer 81(3):417–427
Sakamoto Y, Kitajima Y, Edakuni G, Sasatomi E, Mori M, Kitahara K et al (2001) Expression of Trk tyrosine kinase receptor is a biologic marker for cell proliferation and perineural invasion of human pancreatic ductal adenocarcinoma. Oncol Rep 8(3):477–484
Euhus DM, Timmons CF, Tomlinson GE (2002) ETV6-NTRK3—Trk-ing the primary event in human secretory breast cancer. Cancer Cell 2(5):347–348
Makretsov N, He M, Hayes M, Chia S, Horsman DE, Sorensen PH et al (2004) A fluorescence in situ hybridization study of ETV6-NTRK3 fusion gene in secretory breast carcinoma. Genes Chromosom Cancer 40(2):152–157
Tognon C, Knezevich SR, Huntsman D, Roskelley CD, Melnyk N, Mathers JA et al (2002) Expression of the ETV6-NTRK3 gene fusion as a primary event in human secretory breast carcinoma. Cancer Cell 2(5):367–376
Knezevich SR, McFadden DE, Tao W, Lim JF, Sorensen PH (1998) A novel ETV6-NTRK3 gene fusion in congenital fibrosarcoma. Nat Genet 18(2):184–187
Liu Q, Schwaller J, Kutok J, Cain D, Aster JC, Williams IR et al (2000) Signal transduction and transforming properties of the TEL–TRKC fusions associated with t(12, 15)(p13;q25) in congenital fibrosarcoma and acute myelogenous leukemia. EMBO J 19(8):1827–1838
Rubin BP, Chen CJ, Morgan TW, Xiao S, Grier HE, Kozakewich HP et al (1998) Congenital mesoblastic nephroma t(12, 15) is associated with ETV6-NTRK3 gene fusion: cytogenetic and molecular relationship to congenital (infantile) fibrosarcoma. Am J Pathol 153(5):1451–1458
Chou TT, Trojanowski JQ, Lee VM (2000) A novel apoptotic pathway induced by nerve growth factor-mediated TrkA activation in medulloblastoma. J Biol Chem 275(1):565–570
Grotzer MA, Janss AJ, Fung K, Biegel JA, Sutton LN, Rorke LB et al (2000) TrkC expression predicts good clinical outcome in primitive neuroectodermal brain tumors. J Clin Oncol 18(5):1027–1035
Kim JY, Sutton ME, Lu DJ, Cho TA, Goumnerova LC, Goritchenko L et al (1999) Activation of neurotrophin-3 receptor TrkC induces apoptosis in medulloblastomas. Cancer Res 59(3):711–719
Segal RA, Goumnerova LC, Kwon YK, Stiles CD, Pomeroy SL (1994) Expression of the neurotrophin receptor TrkC is linked to a favorable outcome in medulloblastoma. Proc Natl Acad Sci USA 91(26):12867–12871
Ng YK, Wong EY, Lau CP, Chan JP, Wong SC, Chan AS et al (2012) K252a induces anoikis-sensitization with suppression of cellular migration in Epstein-Barr virus (EBV)—associated nasopharyngeal carcinoma cells. Invest New Drugs 30(1):48–58
McGregor LM, McCune BK, Graff JR, McDowell PR, Romans KE, Yancopoulos GD et al (1999) Roles of trk family neurotrophin receptors in medullary thyroid carcinoma development and progression. Proc Natl Acad Sci USA 96(8):4540–4545
Eggert A, Grotzer MA, Ikegaki N, Zhao H, Cnaan A, Brodeur GM et al (2001) Expression of the neurotrophin receptor TrkB is associated with unfavorable outcome in Wilms’ tumor. J Clin Oncol 19(3):689–696
Martin-Zanca D, Oskam R, Mitra G, Copeland T, Barbacid M (1989) Molecular and biochemical characterization of the human trk proto-oncogene. Mol Cell Biol 9(1):24–33
Mitra G, Martin-Zanca D, Barbacid M (1987) Identification and biochemical characterization of p70TRK, product of the human TRK oncogene. Proc Natl Acad Sci U S A 84(19):6707–6711
Yu Y, Zhang S, Wang X, Yang Z, Ou G (2010) Overexpression of TrkB promotes the progression of colon cancer. Apmis 118(3):188–195
Okugawa Y, Tanaka K, Inoue Y, Kawamura M, Kawamoto A, Hiro J et al (2013) Brain-derived neurotrophic factor/tropomyosin-related kinase B pathway in gastric cancer. Br J Cancer 108(1):121–130
Guo D, Hou X, Zhang H, Sun W, Zhu L, Liang J et al (2011) More expressions of BDNF and TrkB in multiple hepatocellular carcinoma and anti-BDNF or K252a induced apoptosis, suppressed invasion of HepG2 and HCCLM3 cells. J Exp Clin Cancer Res 30:97
Jin W, Lee JJ, Kim MS, Son BH, Cho YK, Kim HP (2011) DNA methylation-dependent regulation of TrkA, TrkB, and TrkC genes in human hepatocellular carcinoma. Biochem Biophys Res Commun 406(1):89–95
Harada T, Yatabe Y, Takeshita M, Koga T, Yano T, Wang Y et al (2011) Role and relevance of TrkB mutations and expression in non-small cell lung cancer. Clin Cancer Res 17(9):2638–2645
Doebele R, Vaishnavi A, Capelletti M, Le A, Kako S, Butaney M et al (2013) NTRK1 gene fusions as a novel oncogene target in lung cancer. American Society of Clinical Oncology Annual Meeting 2013. ASCO University, Chicago, IL, p. suppl: abstr 8023
Yu X, Liu L, Cai B, He Y, Wan X (2008) Suppression of anoikis by the neurotrophic receptor TrkB in human ovarian cancer. Cancer Sci 99(3):543–552
Desmet CJ, Peeper DS (2006) The neurotrophic receptor TrkB: a drug target in anti-cancer therapy? Cell Mol Life Sci 63(7–8):755–759
Acknowledgments
This work was supported in part by grants from the NIH (CA-094194; GMB), Alex’s Lemonade Stand Foundation and the Audrey E. Evans Endowed Chair in Molecular Oncology (GMB).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Croucher, J.L., Iyer, R., Li, N. et al. TrkB inhibition by GNF-4256 slows growth and enhances chemotherapeutic efficacy in neuroblastoma xenografts. Cancer Chemother Pharmacol 75, 131–141 (2015). https://doi.org/10.1007/s00280-014-2627-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-014-2627-1