Abstract
Purpose
The purpose of the study is to evaluate the effect of gefitinib, an anti-EGFR TKI on circulating tumor cells (CTCs) in patients with metastatic breast cancer (MBC).
Methods
Seventeen patients with MBC with detectable CTCs after the completion of prior treatment received gefitinib 250 mg/day p.o. CTCs were monitored by immunofluorescence microscopy after double staining with anti-cytokeratin (A45-B/B3) and either anti-CD45 or anti-EGFR antibodies.
Results
A median reduction of 96.4 and 94.1 % in CTC count was observed in 11 (64.7 %) and 12 (70.6 %) of patients after the first and the second treatment cycles, respectively. Total CTC numbers declined by 73 and 44 % after the first and second treatment cycles, respectively. In nine patients with EGFR(+)/CK(+) CTCs, gefitinib resulted in a reduction of both EGFR(+) and EGFR(−) CTCs, and after the third course, most detected CTCs were EGFR(−). In two patients, with a sustained decrease in CTC numbers, a PFS of 16.0 and 19.0 months was observed and in one of them, it was associated with clinical objective response.
Conclusion
Treatment-resistant CTCs could be eliminated by gefitinib in MBC, and EGFR expression on CTCs merits further validation as a potential biomarker for specific and effective targeting of CTCs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is considered a systemic disease since early tumor cell dissemination may occur even in patients with small tumors. Several investigators using immunocytochemistry or RT-PCR have shown the presence of cytokeratin-positive epithelial cells in the bone marrow aspirates and the peripheral blood of otherwise metastasis-free patients with stage I and II breast cancers [1–3]. The detection of occult tumor cells in bone marrow (disseminated tumor cells, DTCs) and peripheral blood (circulating tumor cells, CTCs) has been shown to be an independent unfavorable prognostic factor associated with increased distant relapse rate and decreased overall survival [4–7]. In addition, CTCs can be also detected in 40–70 % of patients with metastatic breast cancer (MBC) [8–10]. Using the Cell Search platform, the detection of 5 or more CTCs/7.5 ml of peripheral blood in women with MBC before starting a new line of treatment has been shown to predict progression-free and overall survival, whereas CTC counts in the first follow-up visit were also predictive of treatment outcome [11–16].
Epidermal growth factor receptor (EGFR) is a member of the HER growth factor receptors family. These receptors share a common structure consisting of an extracellular ligand-binding domain, a short transmembrane domain, and an intracellular domain with intrinsic tyrosine kinase activity [17]. Binding of the ligand(s), such as EGF or transforming growth factor-alpha (TGF-alpha) to the extracellular domain of the receptor, initiates a signal transduction cascade that regulates many aspects of tumor cell biology including cell growth, survival, metastasis, and angiogenesis, as well as tumor cell sensitivity to chemotherapy and radiotherapy [17].
Expression of EGFR has been demonstrated in 18–25 % of breast cancers and has been correlated with a higher risk of relapse and death from breast cancer [18, 19]. Substantial increases in EGFR expression have been demonstrated in de novo endocrine-resistant ER-positive disease, whereas a more modest increase in the expression of EGFR or ligands has been detected in acquired endocrine resistance of ER-positive disease [20]. In addition, approximately half of the cases of triple-negative breast cancer and inflammatory breast cancer overexpress EGFR, whereas high EGFR expression is an independent predictor of poor prognosis in inflammatory breast cancer [21].
Gefitinib, a signal transduction inhibitor of the EGFR tyrosine kinase, has demonstrated antitumor activity against chemo- and hormone-resistant breast cancer cell lines [20, 22–24]. Initial phase II studies suggested that gefitinib does not have significant efficacy in pre-treated patients with MBC. In addition, a phase II study, designed to test the efficacy of gefitinib in patients with hormone-resistant breast cancer, was stopped because of low clinical benefit rate [25]. However, in a small randomized study, gefitinib in combination with anastrozole was associated with a marked advantage in PFS compared with anastrozole plus placebo, in postmenopausal women with hormone receptor-positive metastatic disease [26]. Moreover, in a recently reported trial, the combination of anastrozole, fulvestrant, and gefitinib, administered in the neoadjuvant setting in ER-positive breast cancer, resulted in both a significant reduction in cell proliferation, as measured by Ki-67 expression on tumor cells, and in a parallel reduction in the expression of cyclin D1 compared to anastrozole and fulvestrant alone [27].
Our group has previously reported the presence of EGFR-expressing CTCs in the peripheral blood of MBC patients using a double immunostaining cytomorphologic assay; all the enrolled patients in this study also had detectable CK-19mRNA-positive CTCs as assessed by a molecular assay [28]. In addition, phosphorylated EGFR was observed in 86 % of patients with EGFR-expressing CTCs, while the downstream PI3K/Akt signalling pathway was also activated on CTCs of 13 out of 16 evaluated patients, suggesting the involvement of this pathway in CTCs’ survival.
Since the persistence of CTCs after the completion of treatment is associated with poor clinical outcome [9, 29, 30], we hypothesized that targeting CTCs surviving after prior chemotherapy and/or endocrine treatment could be beneficial for patients with breast cancer. This pilot study was designed to assess the effect of gefitinib on chemotherapy- or/and hormonotherapy-resistant CTCs in patients with MBC.
Patients and methods
Patients
Women with histologically confirmed MBC were eligible for the study. Patients had to have detectable CTCs detected by both a molecular (CK-19 mRNA-positive cells) and an immunocytochemical (CK-positive cells) assay. After the enrollment of the first eight patients, the trial was amended to include only patients with EGFR-expressing CTCs, since we observed, in a parallel study, activation of both EGFR and downstream signalling pathways in CTCs of patients with MBC [28]. Other eligibility criteria were age >18 years old; performance status 0–2 (WHO); adequate bone marrow, renal, and liver function; and non-progressing disease (stable disease or partial response) as best response to prior treatment. Eight patients with MBC and detectable CK-19mRNA-positive and CK-positive CTCs, fulfilling the inclusion criteria of this study, who had not received gefitinib, were retrospectively selected from a pool of patients followed in our Department. These patients had to have sequential monthly (up to 4 months) assessments of CTC status (using the molecular assay) as well as PBMCs cytospins available for the detection of cytokeratins using immunostaining (historical control group).
Gefitinib was administered at the dose of 250 mg/day orally (1 month equals one cycle) until disease progression, consent withdrawal, or unacceptable toxicity. The primary end point of the study was to evaluate the efficacy of gefitinib in eliminating CK-positive CTCs. Secondary end point was to assess the effect of gefitinib on patients’ clinical outcome.
Disease assessment
Before treatment initiation, all patients had complete physical examination, blood chemistry, and a diagnostic evaluation including computed tomography scans (CT scans) of the chest and abdomen [or magnetic resonance imaging (MRI) if clinically indicated]. Physical examination and blood chemistry were repeated before each treatment cycle. Patients were assessed by CT scans (or MRI if clinically indicated) every 2 months, and response evaluation was performed according to RECIST criteria. The trial was approved by the Institutional Ethics and Scientific Committee as well as by the Hellenic Drug Organization (EOF), and all patients gave written informed consent in order to participate in the study.
Detection of CK-19 mRNA-positive CTCs
Peripheral blood (20 ml in EDTA) was obtained before the initiation of gefitinib and monthly thereafter. Blood samples were obtained at the middle of vein puncture after the first 5 ml of blood was discarded, in order to avoid contamination of blood with epithelial cells from the skin during sample collection. Peripheral blood mononuclear cells (PBMCs) were isolated using density gradient (Ficoll-hypaque; d = 1.077g/mol) centrifugation at 1,800 rpm for 30 min. PBMCs were washed three times with PBS and centrifuged at 1,500 rpm for 10 min. Patients were screened for the presence of CK-19 mRNA-positive cells using the RT-PCR assay, which has been previously described in detail [31, 32]. The presence of CK-positive CTCs was also confirmed by double immunofluorescence staining as described below, and only patients with CTCs detected by both methods were enrolled into the study. The monitoring of CTCs during gefitinib treatment was performed monthly by immunofluorescence microscopy.
Immunofluorescence microscopy
Cytospins were prepared using aliquots of 250.000 PBMCs/slide by cytocentrifugation at 2,000 rpm for 2 min, and slides were dried up and stored at −80 °C until use. Four slides (106 PBMCs) were analyzed per patient. PBMCs’ cytospins were fixed with cold aceton/methanol 9:1 (v/v) for 20 min and stained with mouse A45-B/B3 antibody (detecting CK8, CK18, and CK19; Micromet, Munich, Germany) for 1 h. Subsequently, slides were stained with either CD45 (common leukocyte antigen; Santa Cruz, Santa Cruz, CA, USA) or anti-EGFR (Santa Cruz, CA, USA) antibodies for 1 h. Cells were then incubated with the corresponding secondary antibodies for 45 min [28]. The cytomorphological criteria proposed by Meng et al. [33] (high nuclear/cytoplasmic ratio, larger cells than white blood cells, etc.) were used to characterize a CK-positive cell as a CTC. CTCs were characterized as EGFR-positive if the intensity of EGFR staining was higher than the respective intensity of PBMCs that served as an internal negative control. Furthermore, to verify the specificity of the staining procedure, positive and negative controls prepared by adding or omitting EGFR primary antibodies in SKBR3 breast cancer cells that express EGFR [28] were also included in each experiment. Patients with at least one EGFR(+) CTC were determined as having EGFR(+) CTCs. Slides were analyzed using a confocal laser scanning microscope module (Leica Lasertechnik, Heidelberg, Germany) and a fluorescent microscope (Leica DM 2500). Results are expressed as number of CTCs/106 PBMCs.
Results
Patient characteristics
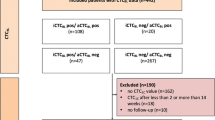
Forty-seven patients with MBC were screened for the presence of CTCs using both a real-time PCR assay (CK-19 mRNA-positive cells) and an immunofluorescence assay. Seventeen patients with CTCs detectable by both methods were enrolled into the study. Nine patients, after the amendment was implemented, were enrolled on the basis of the detection of EGFR-expressing CTCs. Patients’ characteristics are listed in Table 1. Eleven (64.7 %) patients were postmenopausal and 13 (76.4 %) had received prior adjuvant treatment. Nine (52.9 %) and four (23.5 %) patients had hormone receptor- and HER2-positive tumors, respectively. Nine (52.9 %) patients had visceral disease and 10 (58.8 %) had received two or more prior lines of treatment.
Effect of gefitinib on CTCs
Ninety-one treatment courses were administered in the whole group of patients (median: four courses/patient; range 2–19); all patients completed at least two and 14 (82 %) at least three treatment courses. After the completion of the first treatment course, the total CTC numbers, as detected by double immunostaining, decreased in 11 out of 17 (64.7 %) patients by a median of 96.4 % (range 66.7–100.0 %), whereas in the remaining six (35.3 %) patients, their number was increased (Fig. 1). After the second treatment course, CTC numbers were decreased, by a median of 94.1 % (range 50.0–100.0 %), in 12 (70.6 %) patients and increased in five (29.4 %). Conversely, a progressive increase in CTCs’ numbers was observed in seven out of the eight patients of the historical control group (Table 2).
A total of 393 CTCs were detected at baseline in the whole group of patients with a median of five CTCs/patient (range 1–33). CTC counts decreased to 106 (median: three CTCs/patient; range 0–21) and 220 (median: three CTCs/patient; range 0–53), corresponding to a 73 and 44 % decrease compared to the baseline, after the first, and second treatment courses, respectively.
Effect of gefitinib on CTCs according to EGFR expression
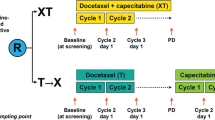
Nine patients had been enrolled on the basis of EGFR expression on CTCs. As shown in Fig. 2a and b, EGFR expression on CTCs was mainly membranous and to a lesser extent intracellular, whereas CK staining was mainly cytoplasmic. Among a total of 336 CTCs (median: six CTCs/patient; range 2–133) detected at baseline in this cohort of patients, 74 (22 %) expressed EGFR (median: two EGFR(+)/CK(+) CTCs/patient; range 1–28). As a negative control, PBMCs from 10 healthy female blood donors were also evaluated for CK/EGFR co-expression by double staining immunofluorescence; there were no cells that stained positive for EGFR and CK in these healthy blood donors.
EGFR expression in CTCs from breast cancer patients. a Confocal laser scanning microscopic sections of a patient’s CTC stained with antibodies against pan-cytokeratins (A45-B/B3; green) and EGFR (red); magnification (×60). b Double immunofluorescence staining of patient’s CTCs with anti-pancytokeratin (green) and anti-EGFR (red) antibodies and Dapi (for nucleus staining); magnification (×20) (ARIOL system)
Sixty-three treatment courses were administered in this group of patients; 8 out of 9 patients completed at least three courses. CTC numbers were decreased by a median of 100 % (range 87.3–100 %) and 98.3 % (range 66.7–100 %) in five (55.5 %) and six (66.7 %) patients, after the completion of the first and second treatment courses, respectively. Total CTC numbers detected in all patients declined from 336 to 83 (a decrease by 75.3 %) and 114 (a decrease by 66.1 %) after the first and second treatment course, respectively (Table 3). The number of EGFR(+) CTCs was reduced from 74 at baseline to 25 (a 66.2 % decrease) at the end of the first course and to 23 (a 68.9 % decrease) at the end of the second treatment course (Table 3). Similarly, EGFR(−) CTCs were also reduced from 262 to 58 (a 77.8 % decrease) and 91 (a 65.2 % decrease) at the end of the first and second treatment courses, respectively (Table 3). However, among a total of 89 CTCs identified at the end of the third course in 7 out of the 8 patients who completed 3 treatment courses (no available sample in one patient), only 8 CTCs (8.9 %) expressed EGFR, whereas 81 (91.0 %) were EGFR(−) (Table 3).
Clinical outcome according to the effect on CTCs
The median duration of gefitinib treatment was 3.9 months (range 1.9–18.8) and 4.2 months (range 1.9–18.8) in the whole group of patients and in patients with known EGFR status of CTCs, respectively. Disease control rate (DCR) was 41.2 and 44.4 %, and the median PFS was 16 (range 5–76) and 18 weeks (range 8–76) in the whole group and in patients with known EGFR status, respectively.
As shown in Table 3, gefitinib was associated with a significant decrease in the absolute number of EGFR(+)/CK(+) and EGFR(−)/CK(+) CTCs after the first month of treatment in 4 (44.4 %) patients; this effect was sustained for at least 3 months. Among them, one patient had a partial response, two had disease stabilization, and one progressed. Moreover, in 2 (22.2 %) of these patients (#5, #6; Table 3), the elimination of CTCs was maintained for the whole period that sequential monthly blood samples were evaluated (up to 6 months); in these particular patients, a prolonged PFS of 16.0 and 19.0 months, associated with disease stabilization in one and objective partial response in the other, was recorded. Both patients had visceral disease and had been previously treated with one and two chemotherapy regimens for advanced disease, respectively.
In 3 (33.3 %) patients (#7, #8, #9; Table 3), a significant increase in both EGFR(+)/CK(+) and EGFR(−)/CK(+) subpopulations was documented after the first treatment course and this was further confirmed after the second course. Interestingly, in two of them, the subsequent increase in CTC numbers mainly concerned the EGFR(−)/CK(+) subpopulation. Two out of these three patients with increasing CTC numbers experienced progressive disease as best response to treatment.
Discussion
Increasing evidence supports the role of CTCs as a potent prognostic and predictive tool in MBC patients. Indeed, using the FDA-approved Cell Search system, it has been shown that increased numbers of CTCs before and after one cycle of a systemic treatment for metastatic disease or at any time during therapy were associated with shorter median PFS and OS representing an earlier and more reliable indicator of response to treatment compared to imaging studies. In addition, serial enumeration of CTCs was strongly correlated with radiologic assessment and accurately predicted disease progression [16]. CTCs surviving after the administration of chemotherapy and/or hormone therapy are expected to present resistance to these therapeutic modalities, and this is associated with a poor clinical outcome [9, 29, 30]. Therefore, it is an unmet need to identify new therapeutic targets for the treatment for patients with “resistant” CTCs.
The molecular characterization of CTCs is extremely important since it might guide the implementation of targeted therapies. In the current pilot and exploratory study, we sought to investigate whether gefitinib could eradicate cytokeratin-positive CTCs, detectable by using both a molecular and an immunocytochemical assay, after the completion of prior therapy in patients with MBC, since phosphorylated EGFR and downstream signalling kinases have been shown to be expressed on CTCs and could be involved in the metastatic potential of CTCs [28].
The presented results indicate that the administration of gefitinib was associated with an early and significant decrease in CTC numbers in more than 50 % of treated patients. In addition, the sustained elimination of CTCs seems to be associated with a better clinical outcome. A similar decrease in CK-positive CTCs could not be observed in an historical control group of eight patients who did not received gefitinib; however, this comparison has serious and obvious limitations and should be considered with caution. Despite the important individual variability of the frequency of EGFR-expressing CTCs, similar results could also be observed when the group of patients with known CTCs’ EGFR status was analyzed separately. It is interesting to note that EGFR(+) and EGFR(−) subpopulations of CTCs presented comparable elimination rates during gefitinib treatment, although the effect on EGFR(+) CTCs was more important and sustainable. The elimination of EGFR(−)/CK(+) CTCs during gefitinib administration seems unexpected; however, we cannot exclude a low, but undetectable by immunofluorescence, expression of EGFR which could be sufficient enough to transactivate other HER receptors through heterodimerization. Indeed, breast cancer cell lines with low EGFR expression levels are sensitive to the antitumor effect of gefitinib, if they co-express high levels of HER2 and this effect is mediated, at least partly, by gefitinib-induced reduction of HER1/HER2 heterodimer phosphorylation [34–36]. Although in the present study the co-expression of HER2 and EGFR on individual CTCs has not been evaluated, we have previously shown that 44 and 63 % of patients with MBC have detectable EGFR(+)/CK(+) and HER2(+)/CK(+) CTCs, respectively; in addition, triple-staining experiments demonstrated the co-expression of both EGFR and HER2 on the same CTCs [28]. Therefore, it could be hypothesized that gefitinib might be effective even against CTCs with low, but undetectable by immunofluorescence, EGFR levels that express HER2.
The kinetics of the EGFR(+) and EGFR(−) subpopulations of CTCs revealed that at the end of the third treatment course, CTC counts showed an increasing trend that mainly concerned the EGFR(−)/CK(+) subpopulation, whereas the number of EGFR(+)/CK(+) CTCs was further decreased. However, the small number of the enrolled patients limits the importance of this observation, which needs to be confirmed in a subsequent and larger study. However, these observations seem to indicate that the EGFR(−)/CK(+) subpopulation of CTCs, which increases during treatment, could represent gefitinib-resistant cells.
The evaluation of the kinetics of EGFR(+) and EGFR(−) CTCs in individual patients is noteworthy since it appears to be correlated with clinical outcome. Indeed, two main groups of patients could be distinguished; the first one is characterized by a clear decrease in both subpopulations of CTCs after the first treatment cycle, which was sustained for the subsequent two cycles; conversely, the second group is characterized by an early increase in EGFR(+) and EGFR(−) subpopulations of CTCs (Table 3), which further supports the hypothesis that EGFR(−)/CK(+) CTCs have to be gefitinib-resistant. Clinically, in 2 out of 5 patients of the first group, a prolonged PFS of 16.0 and 19.0 months was observed in association with a long-lasting objective response in one of them. On the contrary, in 2 out of 3 patients with increasing CTC numbers, progressive disease as best response to treatment was recorded. Therefore, the prolonged elimination of both EGFR(+) and EGFR(−) CTCs upon treatment with gefitinib might be a signal indicating treatment efficacy and disease control, supporting the relevance of CTCs as a clinical biomarker for treatment monitoring.
Although these results are interesting, they should be considered as hypothesis generating due to the pilot and exploratory design of the trial, which enrolled only a small number of patients. Therefore, our observations should be interpreted with caution since there is not a parallel non-treated control group studied prospectively. The used historical control group was consisted of patients selected on the basis of the sequential monthly enumeration of CTCs and the availability of cytospins for further immunostaining for the detection of CK-positive CTCs. In addition, the detection of CTCs was not confirmed with the Cell Search assay, which represents the gold standard assay for the enumeration of CTCs in the metastatic setting, since at the time that the study was initiated, the Cell Search platform was not available in our laboratory. Finally, the correlation of CTC changes during treatment with the clinical outcome was retrospective and exploratory. However, the presented results are in favor of the hypothesis that the molecular characterization of CTCs could used as a potential tool for the selection of targeted treatments in breast cancer. Indeed, it has been demonstrated that the administration of trastuzumab is associated with the elimination of HER2(+) CTCs in pre-treated patients with MBC [37]. Furthermore, a randomized phase II study reported that in patients with HER2-negative early breast cancer with CK-19mRNA-positive CTCs detectable both before and after the completion of adjuvant chemotherapy, the administration of trastuzumab was associated with a significantly lower incidence of clinical relapses and a longer disease-free survival compared to patients who received the standard of care [38]. In two small phase II trials, lapatinib was administered in MBC patients with HER2-negative disease and HER2-positive [39] or EGFR-positive [40] CTCs. In the second study, lapatinib was reported to result in a decrease in CTC counts in 43 % of patients, with most of these having a greater decrease in their EGFR-positive CTC pool [40].
In summary, the current study implies that the assessment of molecular targets on CTCs is a reasonable, feasible, and clinically relevant approach in order to select patients for targeted treatments. Large, well-designed and controlled studies are needed to further evaluate the molecular characterization of CTCs in the individualization of treatment for breast cancer patients.
References
Lambrechts AC, van ‘t Veer LJ, Rodenhuis S (1998) The detection of minimal numbers of contaminating epithelial tumor cells in blood or bone marrow: use, limitations and future of RNA-based methods. Ann Oncol 9(12):1269–1276
Pantel K, Cote RJ, Fodstad O (1999) Detection and clinical importance of micrometastatic disease. J Natl Cancer Inst 91(13):1113–1124
Daskalaki A, Agelaki S, Perraki M, Apostolaki S, Xenidis N, Stathopoulos E, Kontopodis E, Hatzidaki D, Mavroudis D, Georgoulias V (2009) Detection of cytokeratin-19 mRNA-positive cells in the peripheral blood and bone marrow of patients with operable breast cancer. Br J Cancer 101(4):589–597
Cote RJ, Rosen PP, Lesser ML, Old LJ, Osborne MP (1991) Prediction of early relapse in patients with operable breast cancer by detection of occult bone marrow micrometastases. J Clin Oncol 9(10):1749–1756
Braun S, Pantel K, Muller P, Janni W, Hepp F, Kentenich CR, Gastroph S, Wischnik A, Dimpfl T, Kindermann G, Riethmuller G, Schlimok G (2000) Cytokeratin-positive cells in the bone marrow and survival of patients with stage I, II, or III breast cancer. New Engl J Med 342(8):525–533
Diel IJ, Kaufmann M, Costa SD, Holle R, von Minckwitz G, Solomayer EF, Kaul S, Bastert G (1996) Micrometastatic breast cancer cells in bone marrow at primary surgery: prognostic value in comparison with nodal status. J Natl Cancer Inst 88(22):1652–1658
Mansi JL, Easton D, Berger U, Gazet JC, Ford HT, Dearnaley D, Coombes RC (1991) Bone marrow micrometastases in primary breast cancer: prognostic significance after 6 years’ follow-up. Eur J Cancer 27(12):1552–1555
Bidard FC, Vincent-Salomon A, Sigal-Zafrani B, Dieras V, Mathiot C, Mignot L, Thiery JP, Sastre-Garau X, Pierga JY (2008) Prognosis of women with stage IV breast cancer depends on detection of circulating tumor cells rather than disseminated tumor cells. Ann Oncol 19(3):496–500
Cristofanilli M, Hayes DF, Budd GT, Ellis MJ, Stopeck A, Reuben JM, Doyle GV, Matera J, Allard WJ, Miller MC, Fritsche HA, Hortobagyi GN, Terstappen LW (2005) Circulating tumor cells: a novel prognostic factor for newly diagnosed metastatic breast cancer. J Clin Oncol 23(7):1420–1430
Riethdorf S, Fritsche H, Muller V, Rau T, Schindlbeck C, Rack B, Janni W, Coith C, Beck K, Janicke F, Jackson S, Gornet T, Cristofanilli M, Pantel K (2007) Detection of circulating tumor cells in peripheral blood of patients with metastatic breast cancer: a validation study of the cell search system. Clin Cancer Res 13(3):920–928
Cristofanilli M, Budd GT, Ellis MJ, Stopeck A, Matera J, Miller MC, Reuben JM, Doyle GV, Allard WJ, Terstappen LW, Hayes DF (2004) Circulating tumor cells, disease progression, and survival in metastatic breast cancer. New Engl J Med 351(8):781–791
Hayes DF, Cristofanilli M, Budd GT, Ellis MJ, Stopeck A, Miller MC, Matera J, Allard WJ, Doyle GV, Terstappen LW (2006) Circulating tumor cells at each follow-up time point during therapy of metastatic breast cancer patients predict progression-free and overall survival. Clin Cancer Res 12(14 Pt 1):4218–4224
Dawood S, Broglio K, Valero V, Reuben J, Handy B, Islam R, Jackson S, Hortobagyi GN, Fritsche H, Cristofanilli M (2008) Circulating tumor cells in metastatic breast cancer: from prognostic stratification to modification of the staging system? Cancer 113(9):2422–2430
Nole F, Munzone E, Zorzino L, Minchella I, Salvatici M, Botteri E, Medici M, Verri E, Adamoli L, Rotmensz N, Goldhirsch A, Sandri MT (2008) Variation of circulating tumor cell levels during treatment of metastatic breast cancer: prognostic and therapeutic implications. Ann Oncol 19(5):891–897
Botteri E, Sandri MT, Bagnardi V, Munzone E, Zorzino L, Rotmensz N, Casadio C, Cassatella MC, Esposito A, Curigliano G, Salvatici M, Verri E, Adamoli L, Goldhirsch A, Nole F (2010) Modelling the relationship between circulating tumour cells number and prognosis of metastatic breast cancer. Breast Cancer Res Treat 122(1):211–217
Liu MC, Shields PG, Warren RD, Cohen P, Wilkinson M, Ottaviano YL, Rao SB, Eng-Wong J, Seillier-Moiseiwitsch F, Noone AM, Isaacs C (2009) Circulating tumor cells: a useful predictor of treatment efficacy in metastatic breast cancer. J Clin Oncol 27(31):5153–5159
Olayioye MA, Neve RM, Lane HA, Hynes NE (2000) The ErbB signalling network: receptor heterodimerization in development and cancer. EMBO J 19(13):3159–3167
Arpino G, Weiss H, Lee AV, Schiff R, De Placido S, Osborne CK, Elledge RM (2005) Estrogen receptor-positive, progesterone receptor-negative breast cancer: association with growth factor receptor expression and tamoxifen resistance. J Natl Cancer Inst 97(17):1254–1261
Rimawi MF, Shetty PB, Weiss HL, Schiff R, Osborne CK, Chamness GC, Elledge RM (2010) Epidermal growth factor receptor expression in breast cancer association with biologic phenotype and clinical outcomes. Cancer 116(5):1234–1242
Gutteridge E, Agrawal A, Nicholson R, Leung Cheung K, Robertson J, Gee J (2010) The effects of gefitinib in tamoxifen-resistant and hormone-insensitive breast cancer: a phase II study. Int J Cancer 126(8):1806–1816
Masuda H, Zhang D, Bartholomeusz C, Doihara H, Hortobagyi GN, Ueno NT (2012) Role of epidermal growth factor receptor in breast cancer. Breast Cancer Res Treat 136(2):331–345
Ciardiello F, Caputo R, Bianco R, Damiano V, Fontanini G, Cuccato S, De Placido S, Bianco AR, Tortora G (2001) Inhibition of growth factor production and angiogenesis in human cancer cells by ZD1839 (Iressa), a selective epidermal growth factor receptor tyrosine kinase inhibitor. Clin Cancer Res 7(5):1459–1465
Ciardiello F, Caputo R, Bianco R, Damiano V, Pomatico G, De Placido S, Bianco AR, Tortora G (2000) Antitumor effect and potentiation of cytotoxic drugs activity in human cancer cells by ZD-1839 (Iressa), an epidermal growth factor receptor-selective tyrosine kinase inhibitor. Clin Cancer Res 6(5):2053–2063
Ciardiello F, Caputo R, Borriello G, Del Bufalo D, Biroccio A, Zupi G, Bianco AR, Tortora G (2002) ZD1839 (IRESSA), an EGFR-selective tyrosine kinase inhibitor, enhances taxane activity in bcl-2 overexpressing, multidrug-resistant MCF-7 ADR human breast cancer cells. Int J Cancer 98(3):463–469
Green MD, Francis PA, Gebski V, Harvey V, Karapetis C, Chan A, Snyder R, Fong A, Basser R, Forbes JF (2009) Gefitinib treatment in hormone-resistant and hormone receptor-negative advanced breast cancer. Ann Oncol 20(11):1813–1817
Cristofanilli M, Valero V, Mangalik A, Royce M, Rabinowitz I, Arena FP, Kroener JF, Curcio E, Watkins C, Bacus S, Cora EM, Anderson E, Magill PJ (2010) Phase II, randomized trial to compare anastrozole combined with gefitinib or placebo in postmenopausal women with hormone receptor-positive metastatic breast cancer. Clin Cancer Res 16(6):1904–1914
Massarweh S, Tham YL, Huang J, Sexton K, Weiss H, Tsimelzon A, Beyer A, Rimawi M, Cai WY, Hilsenbeck S, Fuqua S, Elledge R (2011) A phase II neoadjuvant trial of anastrozole, fulvestrant, and gefitinib in patients with newly diagnosed estrogen receptor positive breast cancer. Breast Cancer Res Treat 129(3):819–827
Kallergi G, Agelaki S, Kalykaki A, Stournaras C, Mavroudis D, Georgoulias V (2008) Phosphorylated EGFR and PI3 K/Akt signaling kinases are expressed in circulating tumor cells of breast cancer patients. Breast Cancer Res 10(5):R80
Xenidis N, Vlachonikolis I, Mavroudis D, Perraki M, Stathopoulou A, Malamos N, Kouroussis C, Kakolyris S, Apostolaki S, Vardakis N, Lianidou E, Georgoulias V (2003) Peripheral blood circulating cytokeratin-19 mRNA-positive cells after the completion of adjuvant chemotherapy in patients with operable breast cancer. Ann Oncol 14(6):849–855
Xenidis N, Markos V, Apostolaki S, Perraki M, Pallis A, Sfakiotaki G, Papadatos-Pastos D, Kalmanti L, Kafousi M, Stathopoulos E, Kakolyris S, Mavroudis D, Georgoulias V (2007) Clinical relevance of circulating CK-19 mRNA-positive cells detected during the adjuvant tamoxifen treatment in patients with early breast cancer. Ann Oncol 18(10):1623–1631
Stathopoulou A, Gizi A, Perraki M, Apostolaki S, Malamos N, Mavroudis D, Georgoulias V, Lianidou ES (2003) Real-time quantification of CK-19 mRNA-positive cells in peripheral blood of breast cancer patients using the lightcycler system. Clin Cancer Res 9(14):5145–5151
Xenidis N, Perraki M, Kafousi M, Apostolaki S, Bolonaki I, Stathopoulou A, Kalbakis K, Androulakis N, Kouroussis C, Pallis T, Christophylakis C, Argyraki K, Lianidou ES, Stathopoulos S, Georgoulias V, Mavroudis D (2006) Predictive and prognostic value of peripheral blood cytokeratin-19 mRNA-positive cells detected by real-time polymerase chain reaction in node-negative breast cancer patients. J Clin Oncol 24(23):3756–3762
Meng S, Tripathy D, Frenkel EP, Shete S, Naftalis EZ, Huth JF, Beitsch PD, Leitch M, Hoover S, Euhus D, Haley B, Morrison L, Fleming TP, Herlyn D, Terstappen LW, Fehm T, Tucker TF, Lane N, Wang J, Uhr JW (2004) Circulating tumor cells in patients with breast cancer dormancy. Clin Cancer Res 10(24):8152–8162
Moasser MM, Basso A, Averbuch SD, Rosen N (2001) The tyrosine kinase inhibitor ZD1839 (“Iressa”) inhibits HER2-driven signalling and suppresses the growth of HER2-overexpressing tumor cells. Cancer Res 61(19):7184–7188
Campiglio M, Locatelli A, Olgiati C, Normanno N, Somenzi G, Vigano L, Fumagalli M, Menard S, Gianni L (2004) Inhibition of proliferation and induction of apoptosis in breast cancer cells by the epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor ZD1839 (‘Iressa’) is independent of EGFR expression level. J Cell Physiol 198(2):259–268
Moulder SL, Yakes FM, Muthuswamy SK, Bianco R, Simpson JF, Arteaga CL (2001) Epidermal growth factor receptor (HER1) tyrosine kinase inhibitor ZD1839 (Iressa) inhibits HER2/neu (erbB2)-overexpressing breast cancer cells in vitro and in vivo. Cancer Res 61(24):8887–8895
Bozionellou V, Mavroudis D, Perraki M, Papadopoulos S, Apostolaki S, Stathopoulos E, Stathopoulou A, Lianidou E, Georgoulias V (2004) Trastuzumab administration can effectively target chemotherapy-resistant cytokeratin-19 messenger RNA-positive tumor cells in the peripheral blood and bone marrow of patients with breast cancer. Clin Cancer Res 10(24):8185–8194
Georgoulias V, Bozionelou V, Agelaki S, Perraki M, Apostolaki S, Kallergi G, Kalbakis K, Xyrafas A, Mavroudis D (2012) Trastuzumab decreases the incidence of clinical relapses in patients with early breast cancer presenting chemotherapy-resistant CK-19mRNA-positive circulating tumor cells: results of a randomized phase II study. Ann Oncol 23(7):1744–1750
Pestrin M, Bessi S, Puglisi F, Minisini AM, Masci G, Battelli N, Ravaioli A, Gianni L, Di Marsico R, Tondini C, Gori S, Coombes CR, Stebbing J, Biganzoli L, Buyse M, Di Leo A (2012) Final results of a multicenter phase II clinical trial evaluating the activity of single-agent lapatinib in patients with HER2-negative metastatic breast cancer and HER2-positive circulating tumor cells. A proof-of-concept study. Breast Cancer Res Treat 134(1):283–289
Stebbing J, Payne R, Reise J, Frampton AE, Avery M, Woodley L, Di Leo A, Pestrin M, Krell J, Coombes RC (2013) The efficacy of lapatinib in metastatic breast cancer with HER2 non-amplified primary tumors and EGFR positive circulating tumor cells: a proof-of-concept study. PLoS One 8(5):e62543
Acknowledgments
This work was supported by a grant from Astra Zeneca (UK) and from the Cretan Association for Biomedical Research (CABR).
Disclosure
There is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Antonia Kalykaki and Sofia Agelaki contributed equally to this work.
Clinicaltrials.gov: NCT00428896
Rights and permissions
About this article
Cite this article
Kalykaki, A., Agelaki, S., Kallergi, G. et al. Elimination of EGFR-expressing circulating tumor cells in patients with metastatic breast cancer treated with gefitinib. Cancer Chemother Pharmacol 73, 685–693 (2014). https://doi.org/10.1007/s00280-014-2387-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-014-2387-y