Abstract
Purpose
This work was initiated to extend data on the effect of pharmacogenetics and chemotherapy pharmacokinetics (PK) on clinical outcome in patients with gastrointestinal malignancies.
Methods
We assessed 44 gene polymorphisms in 16 genes (TYMS, MTHFR, GSTP1, GSTM1, GSTT1, DPYD, XRCC1, XRCC3, XPD, ERCC1, RECQ1, RAD54L, ABCB1, ABCC2, ABCG2 and UGT2B7) in 64 patients with metastatic colorectal cancer (CRC) receiving capecitabine/oxaliplatin and 76 patients with advanced gastroesophageal cancer (GEC) receiving epirubicin/cisplatin/capecitabine, respectively. Plasma concentrations of anticancer drugs were measured for up to 24 h, and results were submitted to population PK analysis. We calculated the association between gene polymorphisms, chemotherapy exposure, tumor response, progression-free survival (PFS), overall survival (OS) and chemotherapy-related toxicity using appropriate statistical tests.
Results
Patients with a low clearance of 5FU were at increased risk of neutropenia (P < 0.05) and hand–foot syndrome (P = 0.002). DPYD T85C, T1896C and A2846T mutant variants were associated with diarrhea (P < 0.05) and HFS (P < 0.02), and IVS14+1G>A additionally with diarrhea (P < 0.001). The TYMS 2R/3G, 3C/3G or 3G/3G promoter variants were associated with worse PFS in the CRC (HR = 2.0, P < 0.01) and GEC group (HR = 5.4, P < 0.001) and worse OS in the GEC group (HR = 4.7, P < 0.001). The GSTP1 A313G mutant variant was associated with a higher PFS (HR = 0.55, P = 0.001) and OS (HR = 0.60, P = 0.002) in the CRC group.
Conclusions
Germline polymorphisms of DPYD, TYMS and GSTP1 have a significant effect on toxicity and clinical outcome in patients receiving capecitabine-based chemotherapy for advanced colorectal or gastroesophageal cancer. These data should further be validated in prospective clinical studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Still today, patients with metastatic colorectal (CRC) and gastroesophageal cancer (GEC) have a bad prognosis [1]. Intravenous 5FU has been partly replaced by its oral prodrug capecitabine, that is similarly effective when given in combination with oxaliplatin [2] or irinotecan [3] in CRC and in combination with epirubicin and either cisplatin (ECC) or oxaliplatin (OCC) in GEC [4]. The replacement of 5FU by capecitabine avoids potential complications such as thromboembolism or disconnection associated with central venous catheter implantation [5]. Drug pathway-associated gene polymorphisms may affect clinical outcome in patients with gastrointestinal malignancies [6, 7]. Polymorphic variants of the promoter region of the gene for thymidylate synthase (TYMS) have been suggested to determine the cancer cell’s sensitivity toward fluoropyrimidines [8, 9]. Functional polymorphisms in the methylenetetrahydrofolate reductase (MTHFR) gene have been associated with response to 5FU monotherapy in patients with advanced CRC [10]. Dihydropyrimidine dehydrogenase (DPYD) is the 5FU rate-limiting catabolic enzyme, and several functional mutations result in increased 5FU exposure and toxicity from fluoropyrimidines [11–15]. Resistance to platinum compounds may be attributed to mutations within the nucleotide excision repair (NER) pathway [16, 17] or to mutations of the detoxifying glutathione-S-transferases (GST) [6, 18, 19]. This prospective clinical trial studied the association between pharmacogenetics, anticancer drug pharmacology and clinical outcome in patients with advanced gastrointestinal malignancies.
Methods
Patient population and study treatment
This prospective study was carried out at the Netherlands Cancer Institute (Amsterdam, The Netherlands) (Table 1). Main eligibility criteria include patients with metastatic CRC or GEC, receiving palliative first-line chemotherapy with 3-weekly capecitabine 1000 mg/m2 b.i.d. for 2 out of 3 weeks and oxaliplatin 130 mg/m2 day 1 or ECC (continuous capecitabine 625 mg/m2 b.i.d., cisplatin 60 mg/m2 day 1, epirubicin 50 mg/m2 day 1), respectively. Treatment was given until disease progression, intolerable toxicity or withdrawal of patient consent, whatever occurred first. Weekly hematology and 6-weekly radiological assessments were performed, and treatment response was assessed according to RECIST version 1.0. Patients had adequate bone marrow and organ function. All patients provided written informed consent. Treatment-related toxicity was graded according to the common toxicity criteria version 3.
Genotyping of candidate germline mutations
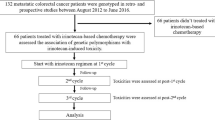
Germline mutations were analyzed from peripheral blood: DPYD c.85T>C (rs1801265), c.496A>G (rs2297595), c.1601G>A (rs1801158), c.1627A>G (rs1801159), c.1679T>G (rs55886062), c.T1896C (rs17376848), c.1905+1G>A (rs3918290), c.2846A>T (rs67376798), ABCC2 c.–24C>T (rs717620), c.1249C>A (rs2273697), c.2366C>T (rs1059762), c.4488C>T (rs8187707), GSTT1*0 (deletion), GSTM1*0 (deletion), GSTP1 c.313A>G (rs1695), TYMS 28 bp VNTR (2R/3R), 3R C>G, TYMS 3′-UTR 6 bp-deletion, MTHFR c.677C>T (rs1801133), ERCC1 c.118C>T (rs11615), ERCC2 c.312G>A (rs1799793), c.751A>C (rs13181), XRCC1 c.399A>G (rs25487), ABCG2 c.34G>A(rs2231137), c.421C>A (rs2231142), c.1465T>C, c.1768A>T, ABCB1 c.1236C>T (rs1128503), c.2650C>T (rs9282563), c.2677G>T/A (rs2032582), c.3320A>C (rs55852620), c.3435C>T (rs1045642), UGT2B7 c.–161T>C (rs7668258), c.–138G>A (rs73823859), c.–125T>C (rs7668282), c.211G>T (rs12233719), c.801T>A (rs7438284), c.802C>T (rs7439366), c.1059C>G (rs4292394), c.1062C>T (rs4348159), XRCC3 c.241C>T (rs861539), RECQ1 c.159A>C, RAD54L c.157C>T (rs1048771). Location of each specific polymorphism as well as the primers used for gene amplification is outlined in the supplementary article files. TYMS high-expression genotype was defined as the presence of at least one 3G allele (2R/3G, 3C/3G or 3G/3G). DNA amplification was performed in a PTC-200 Thermocycler (MJ Research, Waltham, Mass). DNA sequencing was performed using the BigDye Terminator Cycle Sequencing Ready Reaction Kit on an ABI Prism 3100 DNA analyzer (Applied Biosystems). For sequence alignment, the SEQSCAPE bioinformatics software package (version 2.1; Applied Biosystems) was used. SNPs with a missing call rate ≥5 % were excluded. Negative controls were included in each analysis. The investigators performing genetic analyses (V.D.D. and P.H.M.S.) were blinded to patient characteristics and clinical outcome. Specific mutations and respective primers used are outlined in the supplementary article files (Figs. 1, 2).
Kaplan–Meier estimates of progression-free survival (PFS) (left panels) and overall survival (OS) (right panels) for patients with advanced-stage colorectal cancer (top panels) and advanced gastroesophageal cancer (bottom panels) according to the thymidylate synthase (TYMS) high and low genotype, as defined in the “Methods” section
Chemotherapy pharmacokinetic analysis
Blood sampling for all chemotherapy drugs was performed on day 1 of the first treatment cycle and up to 24 h after the start of treatment. Chemotherapy drugs were measured using validated flameless atomic absorption spectrometry [20] and high-performance liquid chromatography (HPLC) [21, 22], respectively. Population pharmacokinetics (PK) analysis of the concentration–time data of chemotherapy drugs and metabolites was performed using the nonlinear mixed-effect modeling program (NONMEM) version 7.2 (ICON Development Solutions, Hanover, USA). Log-transformed plasma concentrations were used together with NONMEM’s first-order conditional estimation method with interaction. Concentration–time data of oxaliplatin and cisplatin were described using a linear two-compartment model, while a linear five-compartment model was used for epirubicin/epirubicinol and for capecitabine and metabolites [23]. Proportional error models were used for interindividual and residual unexplained drug variability. Model selection was based on data fit, precision of parameter estimates and goodness-of-fit plots.
Statistical analysis
The primary objective was to assess the quantitative effect of these 44 gene polymorphisms in 16 drug pathway-associated genes on progression-free survival (PFS), and secondary objectives were to assess the quantitative effect of the same gene polymorphisms on chemotherapy toxicity, objective response rate (ORR) and overall survival (OS) and to assess the relationship between chemotherapy clearance, toxicity and clinical outcome (ORR, PFS, OS). The association between demographics, chemotherapy exposure, pharmacogenetics and clinical outcome was explored using the method of Kaplan–Meier (PFS, OS) and logistic regression (radiological response). Multivariate cox proportional hazards models were used to determine the predictive value of chemotherapy exposure and pharmacogenetics, correcting for prognostic factors (performance score, age, gender). Association between demographics (age, gender, performance score), organ function (creatinine clearance, bilirubin), pharmacogenetics, chemotherapy exposure and toxicity was explored using Fisher’s exact tests (for binary variables) and Wilcoxon-type tests for trend (for ordinal variables with three levels). All tests of significance were two-sided; P < 0.05 was considered significant. No correction for multiple testing was applied, and the results of the present study should be considered hypothesis generating. Statistical analyses were performed using STATA 11.0 (STATA Corp, College Station, Texas, USA).
Results
Patient characteristics are outlined in Table 1. Patients in both groups received a median of six chemotherapy cycles. Cisplatin was changed to carboplatin in three patients for renal dysfunction and in one patient for sensory polyneuropathy. In the CRC group, median follow-up was 5 years and 4 months, median PFS 7.9 months and median OS 15.1 months. In the GEC group, median follow-up was 4 years and 8 months, median PFS 6.1 months and median OS 9.3 months.
Chemotherapy pharmacokinetics
Men had a 11 % higher CLOX compared with women (P = 0.008), and CCL was correlated with platinum clearance (P = 0.01). GSTP1 c.313G homozygous mutants had a 44 % higher clearance for epirubicin (CLEPI) (P = 0.008) and ABCB1 c.3435T mutants a 21 % higher CLEPI (P < 10−4). There was a positive association between body surface area and corrected clearance for capecitabine (CLCAP/F) (P = 0.03), and XRCC1 c.399G mutants had a 21 % lower CLCAP/F (P = 0.006). The single DPYD c.1905+1G>A mutant patient with advanced distal esophageal carcinoma had a 66 % lower CL5FU/F, and XRCC1 c.399G mutants had a 42 % higher CL5FU/F. Population PK models were supported by goodness-of-fit plots, relative standard errors and visual predictive checks.
Genetic, pharmacological and clinical predictors of toxicity
Polymorphic genotypes did not deviate significantly from Hardy–Weinberg equilibrium, although the power to detect potential deviations is low in this dataset. Major genotypes versus fluoropyrimidine-associated toxicity are outlined in Table 2. The full table of functional, non-silent genotypes with a minor allele frequency of ≥5 % and fluoropyrimidine-associated toxicity can be found in the supplementary article files. The single carrier of a mutant DPYD c.1905+1G>A allele experienced diarrhea CTC grade 3, resulting in hospitalization 10 days after starting ECC chemotherapy. After a 50 % dose reduction of capecitabine, the patient received six cycles of ECC without further complications. Patients experiencing chemotherapy-associated neutropenia had a lower CL5FU/F compared with patients with no neutropenia in patients with CRC (32.0 vs. 45.2 L/h, P = 0.005) and GEC (34.2 vs. 41.5 L/h, P = 0.04). Patients experiencing diarrhea had a nonsignificantly lower CL5FU/F in the CTC group (40.4 vs. 45.3 L/h), and patients experiencing HFS had a significantly lower CL5FU/F in the GEC group (30.9 vs. 42.4 L/h, P = 0.002). Two patients in the GEC group experienced heart failure with decreased left ventricular ejection fraction. None of the patients had an impaired elimination of epirubicin (81.6 and 79.1 L/h as compared with the population average of 77.4 L/h). Both patients discontinued epirubicin and fully recovered from heart dysfunction.
Genetic, pharmacological and clinical predictors of clinical outcome
The association between gene polymorphisms and clinical outcome is outlined in Table 3. The full table of functional, non-silent genotypes with a minor allele frequency of ≥5 % and clinical outcome can be found in the supplementary article files.
Patients with metastatic colorectal cancer
Carriers of the TYMS high-expression genotype had a significantly worse PFS (HR = 2.03, P = 0.006) and a nonsignificantly worse OS (HR = 1.48, P = 0.14). GSTP1 c.313G mutant carriers had a significantly improved tumor response (47.2 vs. 10.5 %, P = 0.006), improved PFS (HR = 0.61 for GSTP1 c.313G mutants, HR = 0.24 for GSTP1 c.313G homozygous mutants, P < 0.001) and OS (HR = 0.70 for GSTP1 c.313G mutants, HR = 0.23 for GSTP1 c.313G homozygous mutants, P < 0.001). When correcting for known prognostic factors, the TYMS high-expression genotype predicted for worse OS (HR = 1.70, P = 0.08), and the GSTP1 c.313G homozygous mutant genotype predicted for improved OS (HR 0.56, P = 0.001).
Patients with metastatic gastroesophageal cancer
Carriers of the TYMS high-expression genotype had a significantly worse PFS (HR = 5.43, P < 0.001) and OS (HR = 4.74, P < 0.001). Carriers of the GSTP1 c.313G mutant allele had a nonsignificantly improved tumor response (P = 0.07), and this was mainly driven by GSTP1 c.313G homozygous mutant carriers who had a high tumor response of 77.8 %. Carriers of the ERCC2 c.751C mutant allele had a nonsignificantly improved tumor response, with ERCC2 c.751A>C wild type, heterozygous and homozygous mutant carriers having response rates of 36.3, 51.0 and 75.0 %, respectively (P = 0.10). When correcting for known prognostic factors, the TYMS high-expression genotype predicted for worse OS (HR = 5.44, P < 0.001).
Discussion
This is one of very few studies [24, 25] to combine the analysis of drug pathway-associated germline polymorphisms and anticancer drug PK in patients with advanced gastrointestinal malignancies. Drug pathway-associated candidate genes harboring established and mostly functional polymorphic variants were included in the present study, so that any association between mutant variants and study endpoints (toxicity, clinical outcome) should be plausible from a biological viewpoint. Carriers of the TYMS high-expression genotype had a worse clinical outcome, and this was independent of chemotherapy exposure, in particular capecitabine. These findings may suggest that capecitabine dose escalation or adaptation is unlikely to improve clinical outcome, as chemotherapy response is primarily driven by tumor chemosensitivity rather than chemotherapy exposure. The functional relevance of the TYMS promoter genetics has first been shown by Kawakami et al. [26], who later found a higher survival in carriers of the low-expression compared with the high-expression TYMS genotype in early-stage CRC [27]. A higher treatment response to capecitabine has been found in patients with advanced CRC carrying the TYMS double-repeat variant [28, 29]. In the study by Pullarkat et al. [29], carriers of the TYMS double-repeat variant had a median survival of 16.2 months compared with 8.3 months in patients with one triple-variant allele and 8.5 months in patients with two triple-variant alleles. Goekkurt et al. [30] found carriers of the low-expression TYMS genotype to have a nonsignificantly higher survival compared with carriers of the high-expression genotype (10.2 vs. 6.0 months) when receiving 5FU/cisplatin for advanced gastric cancer. The favorable effect of the TYMS low-expression genotype was confirmed in patients with early-stage gastric cancer receiving adjuvant 5FU [31] and in patients with advanced gastric cancer receiving 5FU/cisplatin [7]. For GSTP1, previous studies in patients with advanced colorectal cancer receiving 5-fluorouracil and oxaliplatin showed carriers of the mutant GSTP1-105 G/G genotype to have a higher risk of grade 3 neurotoxicity compared with carriers of GSTP1-105 A/G and GSTP1-105 A/A genotypes [6, 18]. The GSTP1 c.313A>G mutant variant is suggested to result in a reduced enzymatic activity of GSTP1 and consequential reduced detoxification of the platinum salts, resulting in an increased risk of neurotoxicity, but also improved clinical outcome. Similar to Chen and colleagues, we found an improved outcome in patients with advanced colorectal cancer who were carriers of the mutant GSTP1 c.313A>G allele, with respect to both PFS and OS. We did not find such a correlation between the mutant GSTP1 c.A105G allele and neurotoxicity, although there was a statistical trend for more neurotoxicity in the group of gastroesophageal cancer patients when carrying the mutant GSTP1-105 G/G genotype (44 vs. 19 %, P = 0.09). Finally, a meta-analysis by Ye et al. [32] studied the effect of GSTP1 c.313A>G on clinical outcome in a total of 275 patients with advanced CRC. While homozygous carriers of the mutant GSTP1 c.313A>G allele had a 37 % improvement of the risk of tumor progression (HR = 0.63, 95 % CI 0.35–1.14), this difference was not statistically significant [32].
Three DPYD variants have consistently been associated with toxicity from fluoropyrimidines, i.e., DYPD c.1679T>G (DPYD*13, rs55886062) [13, 14, 33], c.1905+1G>A (IVS14+1G>A, DPYD*2A, rs3918290) [13–15] and c.2846A>T (rs67376798) [13, 14]. Despite the low population frequencies of these polymorphic variants, associations with capecitabine-related toxicity were found for DPYD c.85T>C, c.1896T>C, c.1905+1G>A and c.2846A>T in the present study. A single patient with advanced distal esophageal carcinoma was heterozygous mutant for DPYD c.1905+1G>A, and this patient suffered from grade 3 diarrhea in the first cycle of capecitabine. The effect of DPYD polymorphic variants on the catabolism of fluoropyrimidines and treatment-related toxicity has resulted in clinical practice guidelines for DPYD genotype-guided dosing of fluoropyrimidines, recommending substantial dose reductions in heterozygous carriers of one of these 3 DPYD risk mutations [34]. A 50 % dose reduction in carriers of the IVS14+1G>A allele and a 25 % reduction in carriers of the c.2846A>T variant allele are suggested to be adequate according to a Dutch study including 546 patients with advanced CRC receiving capecitabine-based chemotherapy [11]. This is in close consensus with what was found in the present study, with a 66 % reduction of CL5FU/F in the single DPYD c.1905+1G>A mutant patient. A creatinine clearance <88 ml/min (lowest tertile) was associated with an increased risk of experiencing capecitabine-related HFS in the present study, suggesting that these patients may already be at risk to experience capecitabine-related toxicity. This is further supported by previous work of Hénin and colleagues who found a quasi-linear relationship between creatinine clearance and the risk of HFS, with the risk of HFS increasing by 7 % (95 % CI 2–11 %) for each 10 ml/min decrease in creatinine clearance [35].
The present study is mainly limited by its low power, why results of this study should be considered hypothesis generating. To encounter this inherent weakness, we selected only drug pathway-associated candidate genes harboring established and mostly functional polymorphic variants with a higher a priori likelihood for being associated with clinical endpoints as defined in this study.
In conclusion, germline polymorphisms of DPYD, TYMS and GSTP1 have a significant effect on toxicity and clinical outcome in patients receiving capecitabine-based chemotherapy for advanced colorectal or gastroesophageal cancer. Pharmacogenetic profiling is attractive, as it provides clinically relevant information from a single blood sample, is invariant over time, overcomes tumor heterogeneity and informs individual anticancer treatment in patients with advanced gastrointestinal malignancies. These findings may ultimately lead to an improved understanding of host–tumor interactions underlying cancer progression and treatment response and should further be validated in prospective clinical studies.
References
Siegel R, Ma J, Zou Z, Jemal A (2014) Cancer statistics, 2014. CA Cancer J Clinic 64(1):9–29. doi:10.3322/caac.21208
Diaz-Rubio E, Tabernero J, Gomez-Espana A, Massuti B, Sastre J, Chaves M, Abad A, Carrato A, Queralt B, Reina JJ, Maurel J, Gonzalez-Flores E, Aparicio J, Rivera F, Losa F, Aranda E, Spanish Cooperative Group for the Treatment of Digestive Tumors T (2007) Phase III study of capecitabine plus oxaliplatin compared with continuous-infusion fluorouracil plus oxaliplatin as first-line therapy in metastatic colorectal cancer: final report of the Spanish Cooperative Group for the Treatment of Digestive Tumors Trial. J Clin Oncol Off J Am Soc Clin Oncol 25 (27):4224–4230. doi:10.1200/JCO.2006.09.8467
Skof E, Rebersek M, Hlebanja Z, Ocvirk J (2009) Capecitabine plus Irinotecan (XELIRI regimen) compared to 5-FU/LV plus Irinotecan (FOLFIRI regimen) as neoadjuvant treatment for patients with unresectable liver-only metastases of metastatic colorectal cancer: a randomised prospective phase II trial. BMC Cancer 9:120. doi:10.1186/1471-2407-9-120
Cunningham D, Starling N, Rao S, Iveson T, Nicolson M, Coxon F, Middleton G, Daniel F, Oates J, Norman AR, Upper Gastrointestinal Clinical Studies Group of the National Cancer Research Institute of the United K (2008) Capecitabine and oxaliplatin for advanced esophagogastric cancer. N Engl J Med 358(1):36–46. doi:10.1056/NEJMoa073149
Hitz F, Klingbiel D, Omlin A, Riniker S, Zerz A, Cerny T (2012) Athrombogenic coating of long-term venous catheter for cancer patients: a prospective, randomised, double-blind trial. Ann Hematol 91(4):613–620. doi:10.1007/s00277-011-1343-8
Ruzzo A, Graziano F, Loupakis F, Rulli E, Canestrari E, Santini D, Catalano V, Ficarelli R, Maltese P, Bisonni R, Masi G, Schiavon G, Giordani P, Giustini L, Falcone A, Tonini G, Silva R, Mattioli R, Floriani I, Magnani M (2007) Pharmacogenetic profiling in patients with advanced colorectal cancer treated with first-line FOLFOX-4 chemotherapy. J Clin Oncol Off J Am Soc Clin Oncol 25(10):1247–1254. doi:10.1200/JCO.2006.08.1844
Ruzzo A, Graziano F, Kawakami K, Watanabe G, Santini D, Catalano V, Bisonni R, Canestrari E, Ficarelli R, Menichetti ET, Mari D, Testa E, Silva R, Vincenzi B, Giordani P, Cascinu S, Giustini L, Tonini G, Magnani M (2006) Pharmacogenetic profiling and clinical outcome of patients with advanced gastric cancer treated with palliative chemotherapy. J Clin Oncol Off J Am Soc Clin Oncol 24(12):1883–1891. doi:10.1200/JCO.2005.04.8322
Cui YH, Liu TS, Zhuang RY, Gao HJ, Li H (2009) Polymorphism of thymidylate synthase gene and chemosensitivity of 5-fluorouracil regimen in metastatic gastrointestinal cancer. J Dig Dis 10(2):118–123. doi:10.1111/j.1751-2980.2009.00373.x
Arrazubi V, Suarez J, Guerrero D, Gomez M, Viudez A, Arias F, Balen E, Vera R (2013) Prognostic significance of thymidylate synthase polymorphisms in rectal cancer patients treated with neoadjuvant chemoradiotherapy. Colorect Dis Off J Assoc Coloproctol GB Irel 15(4):428–435. doi:10.1111/codi.12009
Castillo-Fernandez O, Santibanez M, Bauza A, Calderillo G, Castro C, Herrera R, Serrano A, Arrieta O, Herrera LA (2010) Methylenetetrahydrofolate reductase polymorphism (677 C>T) predicts long time to progression in metastatic colon cancer treated with 5-fluorouracil and folinic acid. Arch Med Res 41(6):430–435. doi:10.1016/j.arcmed.2010.08.011
Deenen MJ, Tol J, Burylo AM, Doodeman VD, de Boer A, Vincent A, Guchelaar HJ, Smits PH, Beijnen JH, Punt CJ, Schellens JH, Cats A (2011) Relationship between single nucleotide polymorphisms and haplotypes in DPYD and toxicity and efficacy of capecitabine in advanced colorectal cancer. Clin Cancer Res Off J Am Assoc Cancer Res 17(10):3455–3468. doi:10.1158/1078-0432.CCR-10-2209
Saif MW (2013) Dihydropyrimidine dehydrogenase gene (DPYD) polymorphism among Caucasian and non-Caucasian patients with 5-FU- and capecitabine-related toxicity using full sequencing of DPYD. Cancer Genom Proteomics 10(2):89–92
Loganayagam A, Arenas Hernandez M, Corrigan A, Fairbanks L, Lewis CM, Harper P, Maisey N, Ross P, Sanderson JD, Marinaki AM (2013) Pharmacogenetic variants in the DPYD, TYMS, CDA and MTHFR genes are clinically significant predictors of fluoropyrimidine toxicity. Br J Cancer 108(12):2505–2515. doi:10.1038/bjc.2013.262
Froehlich TK, Amstutz U, Aebi S, Joerger M, Largiader CR (2015) Clinical importance of risk variants in the dihydropyrimidine dehydrogenase gene for the prediction of early-onset fluoropyrimidine toxicity. Int J Cancer J Int du Cancer 136(3):730–739. doi:10.1002/ijc.29025
Li Q, Liu Y, Zhang HM, Huang YP, Wang TY, Li DS, Sun HZ (2014) Influence of DPYD genetic polymorphisms on 5-fluorouracil toxicities in patients with colorectal cancer: a meta-analysis. Gastroenterol Res Pract 2014:827989. doi:10.1155/2014/827989
Huang D, Zhou Y (2014) Nucleotide excision repair gene polymorphisms and prognosis of non-small cell lung cancer patients receiving platinum-based chemotherapy: a meta-analysis based on 44 studies. Biomed Rep 2(4):452–462. doi:10.3892/br.2014.282
Qin Q, Zhang C, Yang X, Zhu H, Yang B, Cai J, Cheng H, Ma J, Lu J, Zhan L, Liu J, Liu Z, Xu L, Sun X (2013) Polymorphisms in XPD gene could predict clinical outcome of platinum-based chemotherapy for non-small cell lung cancer patients: a meta-analysis of 24 studies. PLoS ONE 8(11):e79864. doi:10.1371/journal.pone.0079864
Chen YC, Tzeng CH, Chen PM, Lin JK, Lin TC, Chen WS, Jiang JK, Wang HS, Wang WS (2010) Influence of GSTP1 I105 V polymorphism on cumulative neuropathy and outcome of FOLFOX-4 treatment in Asian patients with colorectal carcinoma. Cancer Sci 101(2):530–535. doi:10.1111/j.1349-7006.2009.01418.x
Lv H, Han T, Shi X, Yao Y, Yao Y, Qiu W, Yue L, Liang J (2014) Genetic polymorphism of GSTP1 and ERCC1 correlated with response to platinum-based chemotherapy in non-small cell lung cancer. Med Oncol 31(8):86. doi:10.1007/s12032-014-0086-5
Brouwers EE, Tibben MM, Joerger M, van Tellingen O, Rosing H, Schellens JH, Beijnen JH (2005) Determination of oxaliplatin in human plasma and plasma ultrafiltrate by graphite-furnace atomic-absorption spectrometry. Anal Bioanal Chem 382(7):1484–1490. doi:10.1007/s00216-005-3302-5
van Asperen J, van Tellingen O, Beijnen JH (1998) Determination of doxorubicin and metabolites in murine specimens by high-performance liquid chromatography. J Chromatogr B Biomed Sci Appl 712(1–2):129–143
Vainchtein LD, Rosing H, Schellens JH, Beijnen JH (2010) A new, validated HPLC-MS/MS method for the simultaneous determination of the anti-cancer agent capecitabine and its metabolites: 5′-deoxy-5-fluorocytidine, 5′-deoxy-5-fluorouridine, 5-fluorouracil and 5-fluorodihydrouracil, in human plasma. Biomed Chromatogr BMC 24(4):374–386. doi:10.1002/bmc.1302
Joerger M, Huitema AD, Koeberle D, Rosing H, Beijnen JH, Hitz F, Cerny T, Schellens JH, Gillessen S (2014) Safety and pharmacology of gemcitabine and capecitabine in patients with advanced pancreatico-biliary cancer and hepatic dysfunction. Cancer Chemother Pharmacol 73(1):113–124. doi:10.1007/s00280-013-2327-2
Guichard SM, Macpherson JS, Mayer I, Reid E, Muir M, Dodds M, Alexander S, Jodrell DI (2008) Gene expression predicts differential capecitabine metabolism, impacting on both pharmacokinetics and antitumour activity. Eur J Cancer 44(2):310–317. doi:10.1016/j.ejca.2007.10.023
Suenaga M, Fuse N, Yamaguchi T, Yamanaka Y, Motomura S, Matsumoto H, Hamamoto Y, Mizunuma N, Doi T, Hatake K, Iwasaki J, Ohtsu A (2014) Pharmacokinetics, safety, and efficacy of FOLFIRI plus bevacizumab in Japanese colorectal cancer patients with UGT1A1 gene polymorphisms. J Clin Pharmacol. doi:10.1002/jcph.246
Kawakami K, Omura K, Kanehira E, Watanabe Y (1999) Polymorphic tandem repeats in the thymidylate synthase gene is associated with its protein expression in human gastrointestinal cancers. Anticancer Res 19(4B):3249–3252
Kawakami K, Watanabe G (2003) Identification and functional analysis of single nucleotide polymorphism in the tandem repeat sequence of thymidylate synthase gene. Cancer Res 63(18):6004–6007
Park DJ, Stoehlmacher J, Zhang W, Tsao-Wei D, Groshen S, Lenz HJ (2002) Thymidylate synthase gene polymorphism predicts response to capecitabine in advanced colorectal cancer. Int J Colorectal Dis 17(1):46–49
Pullarkat ST, Stoehlmacher J, Ghaderi V, Xiong YP, Ingles SA, Sherrod A, Warren R, Tsao-Wei D, Groshen S, Lenz HJ (2001) Thymidylate synthase gene polymorphism determines response and toxicity of 5-FU chemotherapy. Pharmacogenomics J 1(1):65–70
Goekkurt E, Hoehn S, Wolschke C, Wittmer C, Stueber C, Hossfeld DK, Stoehlmacher J (2006) Polymorphisms of glutathione S-transferases (GST) and thymidylate synthase (TS)—novel predictors for response and survival in gastric cancer patients. Br J Cancer 94(2):281–286. doi:10.1038/sj.bjc.6602891
Kawakami K, Graziano F, Watanabe G, Ruzzo A, Santini D, Catalano V, Bisonni R, Arduini F, Bearzi I, Cascinu S, Muretto P, Perrone G, Rabitti C, Giustini L, Tonini G, Pizzagalli F, Magnani M (2005) Prognostic role of thymidylate synthase polymorphisms in gastric cancer patients treated with surgery and adjuvant chemotherapy. Clin Cancer Re Off J Am Assoc Cancer Res 11(10):3778–3783. doi:10.1158/1078-0432.CCR-04-2428
Ye F, Liu Z, Tan A, Liao M, Mo Z, Yang X (2013) XRCC1 and GSTP1 polymorphisms and prognosis of oxaliplatin-based chemotherapy in colorectal cancer: a meta-analysis. Cancer Chemother Pharmacol 71(3):733–740. doi:10.1007/s00280-012-2067-8
van Kuilenburg AB, Dobritzsch D, Meinsma R, Haasjes J, Waterham HR, Nowaczyk MJ, Maropoulos GD, Hein G, Kalhoff H, Kirk JM, Baaske H, Aukett A, Duley JA, Ward KP, Lindqvist Y, van Gennip AH (2002) Novel disease-causing mutations in the dihydropyrimidine dehydrogenase gene interpreted by analysis of the three-dimensional protein structure. Biochem J 364(Pt 1):157–163
Caudle KE, Thorn CF, Klein TE, Swen JJ, McLeod HL, Diasio RB, Schwab M (2013) Clinical Pharmacogenetics Implementation Consortium guidelines for dihydropyrimidine dehydrogenase genotype and fluoropyrimidine dosing. Clin Pharmacol Ther 94(6):640–645. doi:10.1038/clpt.2013.172
Henin E, You B, VanCutsem E, Hoff PM, Cassidy J, Twelves C, Zuideveld KP, Sirzen F, Dartois C, Freyer G, Tod M, Girard P (2009) A dynamic model of hand-and-foot syndrome in patients receiving capecitabine. Clin Pharmacol Ther 85(4):418–425. doi:10.1038/clpt.2008.220
Acknowledgments
This work was supported by a fellowship grant of the European Society of Medical Oncology Grant (ESMO), a research grant of the Union International Contre le Cancer Grant (UICC) and a Research Grant from the Swiss National Science Foundation (SNF) (PBBSB-102331).
Conflict of interest
No potential conflicts of interest were disclosed by the authors.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Joerger, M., Huitema, A.D.R., Boot, H. et al. Germline TYMS genotype is highly predictive in patients with metastatic gastrointestinal malignancies receiving capecitabine-based chemotherapy. Cancer Chemother Pharmacol 75, 763–772 (2015). https://doi.org/10.1007/s00280-015-2698-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-015-2698-7