Abstract
Purpose
The objective of this study was to investigate the drug interaction between dasatinib and the gastric acid suppressants (H2-receptor antagonists (H2RA) famotidine and nizatidine and the proton pump inhibitor (PPI) lansoprazole in leukemia Japanese patients.
Methods
Eighteen patients treated with dasatinib and H2RA, PPI or no acid suppressant from whom were obtained a total of 34 pharmacokinetic profiles were enrolled in the study. Dasatinib plasma concentrations from samples obtained just prior to and 1, 2, and 4 h after oral dasatinib administration were analyzed by high-performance liquid chromatography.
Results
There were no significant correlations between the dose-adjusted total area under the observed plasma concentration–time curve (AUC0–4) of dasatinib and gender, age, weight, or body surface area. The only variable factor, the dasatinib dose-adjusted AUC0–4 for patients administered an H2RA or PPI, was significantly lower than for patients not administered an acid suppressant (median (quartile 1–quartile 3) values: 1.47 (0.79–2.29) versus 3.51 (2.50–5.45) ng h/mL/mg, respectively, P = 0.0008). Moreover, the plasma concentration 2 h (C2h) after dasatinib administration gave a high correlation with the AUC0–4 of dasatinib (r = 0.9419, P < 0.0001).
Conclusion
Clinicians should be aware that administration of an acid suppressant such as famotidine, nizatidine, and lansoprazole can decrease the absorption of dasatinib from the gastrointestinal tract, thereby resulting in a significant decrease in the plasma concentration of dasatinib. The combination of dasatinib and an acid suppressant requires careful therapeutic drug monitoring of the dasatinib plasma concentration to ensure effective patient exposure to the drug.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
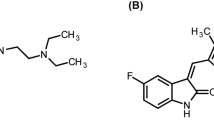
Dasatinib (BMS-354825), a second-generation tyrosine kinase inhibitor, has shown good efficacy in patients with chronic myeloid leukemia (CML) or Philadelphia chromosome positive acute lymphoid leukemia (Ph + ALL) [1, 2]. Dasatinib is a multiple kinase inhibitor that potently inhibits Bcr-Abl, Src family (Src, Lck, Yes, Fyn), c-Kit, and platelet-derived growth factor receptor β kinases [3–5]. Dasatinib exposure is characterized by large inter- and intra-individual variability [6]. Variability in dasatinib exposure has been reported to be due mainly to inter-occasion variability in relative bioavailability [44% coefficient of variation (CV)] and, to a lesser extent, inter-patient variability in relative bioavailability (32% CV) and clearance (25% CV) [7]. As drug pharmacokinetics are generally thought to affect therapeutic outcome and clinical side effects, it is important that the factors responsible for these inter- and intra-patient dasatinib bioavailability differences be elucidated.
One potential cause of variable dasatinib bioavailability is a change in its adsorption profile. After oral administration, drugs typically must be dissolved for them to be absorbed from the gastrointestinal tract. The solubility of dasatinib is pH-dependent, and therefore, an alteration of the pH in the gastrointestinal tract could change dasatinib exposure [8]. The H2-receptor antagonist (H2RA) famotidine and the proton pump inhibitor (PPI) omeprazole are known to decrease the total area under the observed plasma concentration–time curve (AUC) of dasatinib by 61 and 43% and the maximum plasma concentration (C max) of dasatinib by 63 and 42%, respectively [8]. Thus, the change of dasatinib pharmacokinetics by gastric acid suppressants is consistent with reduced absorption. Therefore, it has been recommended that concomitant administration of agents that provide prolonged acid suppression such as H2RA and PPI with dasatinib not be practiced. However, drug interactions between dasatinib and acid suppressants have only been mentioned in pharmaceutical company information, and reports from clinical practice have until now not been reported.
The present study investigated the drug interaction between dasatinib and acid suppressants (H2RA famotidine and nizatidine, and PPI lansoprazole) in Japanese patients with CML or Ph + ALL.
Materials and methods
Patients and protocols
Eighteen Japanese patients with CML or Ph + ALL were selected to participate in this study. The demographic and clinical characteristics of the patients are listed in Table 1. The study protocol was approved by the Ethics Committee of Akita University Hospital, and all recipients gave written informed consent.
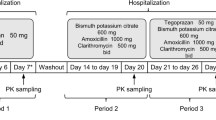
Retrospectively, the 18 patients (34 therapeutic courses) were divided into two groups: dasatinib therapy together with either 30 mg of lansoprazole (Takepron®, Takeda Pharmaceutical Co. Ltd, Osaka, Japan, 5 patients, 12 courses), 20–40 mg/day of famotidine (Gaster®, Astellas Co. Ltd., Tokyo, Japan, 4 patients, 5 courses) and 300 mg/day of nizatidine (Acinon®, Zeria Pharmaceutical Co., Ltd., Tokyo, Japan, 3 patients, 4 courses) or no acid suppressant (6 patients, 14 courses) (Table 1). Dasatinib (Sprycel®; Bristol-Myers, Tokyo, Japan) was given orally at 20–100 mg once daily at a designated time (08:00), or 70 mg twice daily at designated times (08:00 and 20:00). In the steady-state drug concentration period on days 7, 14, 28, and 42 after beginning dasatinib therapy, whole blood samples were collected just prior to and at 1, 2, and 4 h after oral dasatinib administration.
HPLC system
Plasma concentrations of dasatinib were measured by high-performance liquid chromatography (HPLC) [9]. Following the addition of imatinib (20 ng/methanol 10 μL) as an internal standard to a 200 μL plasma sample, the plasma sample was diluted with 800 μL of water and vortexed for 30 s. This mixture was applied to an Oasis HLB extraction cartridge that had been activated previously with methanol and water (1.0 mL each). The cartridge was then washed with 1.0 mL of water and 1.0 mL of 60% methanol in water and eluted with 1.0 mL of 100% methanol. Eluates were evaporated to dryness in a vacuum at 40°C using a rotary evaporator (Iwaki, Tokyo, Japan). The resulting residue was then dissolved in 20 μL of methanol and vortexed for 30 s; 20 μL of mobile phase was added to the sample, and the sample was vortexed for another 30 s. A 20 μL aliquot of the sample was then processed by HPLC. The HPLC system was comprised of a PU-2080 plus chromatography pump (JASCO, Tokyo, Japan) equipped with a CAPCELL PAK C18 MG П (250 × 4.6 mm I.D., Shiseido, Tokyo, Japan) HPLC column, a UV-2075 light source, and an ultraviolet detector (JASCO). The mobile phase was 0.5% KH2PO4 (pH 3.5)-acetonitrile-methanol (55:25:20, v/v/v), which was degassed in an ultrasonic bath prior to use. The flow rate was 0.5 mL/min at ambient temperature, and sample detection was carried out at 250 nm. The lower limit of quantification of this assay was 0.5 ng/mL. The between day and between run coefficients of variation for dasatinib were less than 18.3 and 15.8%, respectively. The mean extraction recovery for dasatinib was 94.0% in the concentration range of 0.5–1,000 ng/mL.
Phamacokinetic analysis
Pharmacokinetic analysis of dasatinib was carried out with a standard non-compartmental method using WinNonlin (Pharsight Co., CA, version 4.0.1). The total area under the observed plasma concentration–time curve (AUC) was calculated using the linear trapezoidal rule. The dosage adjustment was calculated by dividing each computational parameter by the dosage of dasatinib, since its dose-dependent pharmacokinetics increased linearly over the dose range of 15–240 mg/day [10].
Statistical analysis
The clinical characteristics of patients taking dasatinib were expressed as a number or mean value ± standard deviation (range). The normal distribution of each data type was assessed based on a histogram. The AUC0–4 of dasatinib for each group was expressed as a median value (quartile 1–quartile 3). The dasatinib AUC0–4 for two groups was compared using the Mann–Whitney test. The Spearman’s rank correlation coefficient test or simple linear regression analysis was applied to assess a correlation between two groups. A P value less than 0.05 was considered statistically significant. Statistical analyses were performed using statistics software, IBM SPSS Statistics 19.0 for Windows (SPSS IBM Japan Inc., Tokyo, Japan).
Results
A total of 34 pharmacokinetic profiles were obtained from 18 patients under conditions of different dosages, different dasatinib ingestion periods, and the presence of acid suppressant. The plasma concentration–time profiles from 0 to 4 h after administration of dasatinib in the 34 therapeutic courses are shown in Fig. 1. A histogram of the dose-adjusted AUC0–4 of dasatinib is shown in Fig. 2. Distribution of the dose-adjusted AUC0–4 of dasatinib in the 34 profiles is remarkably large with up to a 12-fold difference observed between highest and lowest AUCs. However, the plasma concentration at 2 h (C 2h) after dasatinib administration showed a high correlation with the measured AUC0–4 of dasatinib (r = 0.9419, P < 0.0001). The correlation coefficients (r) between the measured AUC0–4 of dasatinib and the predose, 1 and 4 h plasma concentrations were −0.0686 (P = 0.7935), 0.8694 (P < 0.0001) and 0.6972 (P < 0.0001), respectively. The correlation between the measured and predicted AUC0–4 of dasatinib using only the C 2h sampling point in the equation (predicted AUC0–4 = 2.508 · C 2h + 45.558) is shown in Fig. 3. The coefficient of determination (r 2) between the predicted AUC0–4 with the C 2h point and the measured AUC0–4 was 0.9114 (P < 0.0001).
As shown in Fig. 2, dasatinib had extremely variable pharmacokinetics; however, there were no significant correlations between the dose-adjusted AUC0–4 of dasatinib and gender, age, weight, or body surface area (Table 2). As the only variable factor, there was a significant difference in the dose-adjusted AUC0–4 of dasatinib between the groups administered acid suppressants (H2RA and PPI) and not given acid suppressants (P = 0.0008) (Fig. 4, Table 2). The median (quartile 1–quartile 3) dose-adjusted C 2h of dasatinib with an acid suppressant (H2RA and PPI) and without an acid suppressant was 0.34 (0.10–0.72) ng/mL/mg and 1.23 (0.63–2.23) ng/mL/mg, respectively, (P = 0.0009).
Comparison of dose-adjusted a area under the plasma concentration–time curve from 0 to 4 h (AUC0–4) and b plasma concentration 2 h after dasatinib administration according to the presence or absence of a co-administered acid suppressant. H2RA H2-receptor antagonist, PPI proton pump inhibitor. Graphical analysis was done using an SPSS box and whiskers plot. The box spans data between two quartiles (IQR), with the median represented as a bold horizontal line. The ends of the whiskers (vertical lines) represent the smallest and largest values that are not outliers. Outliers (circles) are values between 1.5 and 3 IQRs from the end of the box
Discussion
The present retrospective study shows that the usual therapeutic dose of acid suppressants (H2RA and PPI) has a clinically significant influence on the dose-adjusted AUC0–4 of dasatinib. The absolute quantity of dasatinib absorbed from the gastrointestinal tract appears to be reduced by H2RA or PPI. Clinicians frequently use acid suppressants to prevent gastrointestinal dysfunction by a medicine. However, clinicians should be aware that administration of acid suppressants can diminish the absorption of dasatinib, thereby resulting in a significant decrease in its plasma concentration. Currently, most hospital laboratories do not monitor the plasma concentration of dasatinib. The pharmacokinetics of dasatinib are characterized by large intra- and inter-individual variability, and this drug is susceptible to drug interactions with many co-administered drugs such as H2RA or PPI. These features of dasatinib and the clinical background of patients taking dasatinib suggest the necessity of performing therapeutic drug monitoring (TDM) to ensure effective patient exposure to the drug and to avoid the risk of toxicity.
Although AUC is the most commonly used pharmacokinetic parameter to characterize exposure to a drug, many blood collection time-points are required to accurately calculate AUC values. Taking into account the time required for blood collection, inconvenience to the patient, and the cost of measuring plasma concentrations, AUC measurement is not appropriate for determining drug interactions or patient compliance. Therefore, it is clinically important that prediction of AUC is calculated from limited patient blood samples. The C 2h point for dasatinib in the present study accurately predicted the AUC0–4 of dasatinib in a shorter time frame and the diminished plasma concentration from drug interactions with H2RA and PPI. The 25% quartile dose-adjusted C 2h of dasatinib without acid suppressants was 0.63 ng/mL/mg, whereas the 75% quartile dose-adjusted C 2h of dasatinib with H2RA or PPI was 0.72 ng/mL/mg. Therefore, C 2h monitoring of dasatinib would be a useful time point to estimate dasatinib exposure and could help in deciding to withdraw an acid suppressant.
Our results must be interpreted within the context of the study limitations. This study was performed with a small number of patients. Although our results agree with those of a previous report [8], further examination with a larger sample size is necessary. In addition, several investigators have suggested that the threshold plasma trough concentration of imatinib, a therapeutic agent for CML and gastrointestinal stromal tumors [11, 12], should be set above 1,000 ng/mL for CML patients to achieve a complete cytogenetic response (CCyR) or major molecular response (MMR) [13–17]. However, a consensus target plasma concentration for dasatinib has not been communicated, although the trough plasma concentration of dasatinib has been reported to correlate with toxicity [18]. While we did not consider how a decrease in plasma concentration of dasatinib by H2RA or PPI influenced the clinical effect, at least a determination of the absorbed dasatinib from the gastrointestinal tract would be needed to estimate drug efficacy. A low absorbed dose of dasatinib due to an H2RA or PPI interaction might not have been sufficient to reach the plasma concentration necessary to observe a clinical response. Further examination of the correlation between clinical evaluation and the pharmacokinetics of dasatinib is necessary.
In conclusion, co-administration of acid suppressants (famotidine, nizatidine, and lansoprazole) significantly decreased the plasma dasatinib concentration. An interaction between dasatinib and acid suppressants was observed for most patients to diminish the absorption of dasatinib. The combination of dasatinib and acid suppressants requires careful TDM of the dasatinib plasma concentration to ensure effective patient exposure to the drug.
References
Kantarjian H, Shah NP, Hochhaus A, Cortes J, Shah S, Ayala M, Moiraghi B, Shen Z, Mayer J, Pasquini R, Nakamae H, Huguet F, Boque C, Chuah C, Bleickardt E, Bradley-Garelik MB, Zhu C, Szatrowski T, Shapiro D, Baccarani M (2010) Dasatinib versus imatinib in newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med 362(24):2260–2270. doi:10.1056/NEJMoa1002315
Foa R, Vitale A, Vignetti M, Meloni G, Guarini A, De Propris MS, Elia L, Paoloni F, Fazi P, Cimino G, Nobile F, Ferrara F, Castagnola C, Sica S, Leoni P, Zuffa E, Fozza C, Luppi M, Candoni A, Iacobucci I, Soverini S, Mandelli F, Martinelli G, Baccarani M (2011) Dasatinib as first-line treatment for adult patients with Philadelphia chromosome-positive acute lymphoblastic leukemia. Blood. doi:10.1182/blood-2011-05-351403
Lombardo LJ, Lee FY, Chen P, Norris D, Barrish JC, Behnia K, Castaneda S, Cornelius LA, Das J, Doweyko AM, Fairchild C, Hunt JT, Inigo I, Johnston K, Kamath A, Kan D, Klei H, Marathe P, Pang S, Peterson R, Pitt S, Schieven GL, Schmidt RJ, Tokarski J, Wen ML, Wityak J, Borzilleri RM (2004) Discovery of N-(2-chloro-6-methyl- phenyl)-2-(6-(4-(2-hydroxyethyl)-piperazin-1-yl)-2-methylpyrimidin-4- ylamino)thiazole-5-carboxamide (BMS-354825), a dual Src/Abl kinase inhibitor with potent antitumor activity in preclinical assays. J Med Chem 47(27):6658–6661. doi:10.1021/jm049486a
Shah NP, Tran C, Lee FY, Chen P, Norris D, Sawyers CL (2004) Overriding imatinib resistance with a novel ABL kinase inhibitor. Science 305(5682):399–401. doi:10.1126/science.1099480
Das J, Chen P, Norris D, Padmanabha R, Lin J, Moquin RV, Shen Z, Cook LS, Doweyko AM, Pitt S, Pang S, Shen DR, Fang Q, de Fex HF, McIntyre KW, Shuster DJ, Gillooly KM, Behnia K, Schieven GL, Wityak J, Barrish JC (2006) 2-aminothiazole as a novel kinase inhibitor template. Structure-activity relationship studies toward the discovery of N-(2-chloro-6-methylphenyl)-2-[[6-[4-(2-hydroxyethyl)-1-piperazinyl)]-2-methyl-4-pyrimidinyl]amino)]-1,3-thiazole-5-carboxamide (dasatinib, BMS-354825) as a potent pan-Src kinase inhibitor. J Med Chem 49 (23):6819–6832. doi:10.1021/jm060727j
van Erp NP, Gelderblom H, Guchelaar HJ (2009) Clinical pharmacokinetics of tyrosine kinase inhibitors. Cancer Treat Rev 35(8):692–706. doi:10.1016/j.ctrv.2009.08.004
Dai G, Pfister M, Blackwood-Chirchir A, Roy A (2008) Importance of characterizing determinants of variability in exposure: application to dasatinib in subjects with chronic myeloid leukemia. J Clin Pharmacol 48(11):1254–1269. doi:10.1177/0091270008320604
Brave M, Goodman V, Kaminskas E, Farrell A, Timmer W, Pope S, Harapanhalli R, Saber H, Morse D, Bullock J, Men A, Noory C, Ramchandani R, Kenna L, Booth B, Gobburu J, Jiang X, Sridhara R, Justice R, Pazdur R (2008) Sprycel for chronic myeloid leukemia and Philadelphia chromosome-positive acute lymphoblastic leukemia resistant to or intolerant of imatinib mesylate. Clin Cancer Res Off J Am Assoc Cancer Res 14(2):352–359. doi:10.1158/1078-0432.CCR-07-4175
Miura M, Takahashi N, Sawada K (2011) Quantitative determination of imatinib in human plasma with high-performance liquid chromatography and ultraviolet detection. J Chromatogr Sci 49(5):412–415
Christopher LJ, Cui D, Wu C, Luo R, Manning JA, Bonacorsi SJ, Lago M, Allentoff A, Lee FY, McCann B, Galbraith S, Reitberg DP, He K, Barros A Jr, Blackwood-Chirchir A, Humphreys WG, Iyer RA (2008) Metabolism and disposition of dasatinib after oral administration to humans. Drug Metab Dispos Biol Fate Chem 36(7):1357–1364. doi:10.1124/dmd.107.018267
Goldman JM (2007) How I treat chronic myeloid leukemia in the imatinib era. Blood 110(8):2828–2837. doi:10.1182/blood-2007-04-038943
O’Brien SG, Guilhot F, Larson RA, Gathmann I, Baccarani M, Cervantes F, Cornelissen JJ, Fischer T, Hochhaus A, Hughes T, Lechner K, Nielsen JL, Rousselot P, Reiffers J, Saglio G, Shepherd J, Simonsson B, Gratwohl A, Goldman JM, Kantarjian H, Taylor K, Verhoef G, Bolton AE, Capdeville R, Druker BJ (2003) Imatinib compared with interferon and low-dose cytarabine for newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med 348(11):994–1004. doi:10.1056/NEJMoa022457
Picard S, Titier K, Etienne G, Teilhet E, Ducint D, Bernard MA, Lassalle R, Marit G, Reiffers J, Begaud B, Moore N, Molimard M, Mahon FX (2007) Trough imatinib plasma levels are associated with both cytogenetic and molecular responses to standard-dose imatinib in chronic myeloid leukemia. Blood 109(8):3496–3499. doi:10.1182/blood-2006-07-036012
Larson RA, Druker BJ, Guilhot F, O’Brien SG, Riviere GJ, Krahnke T, Gathmann I, Wang Y (2008) Imatinib pharmacokinetics and its correlation with response and safety in chronic-phase chronic myeloid leukemia: a subanalysis of the IRIS study. Blood 111(8):4022–4028. doi:10.1182/blood-2007-10-116475
Widmer N, Decosterd LA, Leyvraz S, Duchosal MA, Rosselet A, Debiec-Rychter M, Csajka C, Biollaz J, Buclin T (2008) Relationship of imatinib-free plasma levels and target genotype with efficacy and tolerability. Br J Cancer 98(10):1633–1640. doi:10.1038/sj.bjc.6604355
Singh N, Kumar L, Meena R, Velpandian T (2009) Drug monitoring of imatinib levels in patients undergoing therapy for chronic myeloid leukaemia: comparing plasma levels of responders and non-responders. Eur J Pharmacol 65(6):545–549. doi:10.1007/s00228-009-0621-z
Takahashi N, Wakita H, Miura M, Scott SA, Nishii K, Masuko M, Sakai M, Maeda Y, Ishige K, Kashimura M, Fujikawa K, Fukazawa M, Katayama T, Monma F, Narita M, Urase F, Furukawa T, Miyazaki Y, Katayama N, Sawada K (2010) Correlation between imatinib pharmacokinetics and clinical response in Japanese patients with chronic-phase chronic myeloid leukemia. Clin Pharmacol Ther 88(6):809–813. doi:10.1038/clpt.2010.186
Shayani S (2010) Dasatinib, a multikinase inhibitor: therapy, safety, and appropriate management of adverse events. Ther Drug Monit 32(6):680–687. doi:10.1097/FTD.0b013e3181f4d9c5
Acknowledgments
This work was supported by a grant (no. 23590168) from the Japan Society for the Promotion of Science, Tokyo, Japan.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Takahashi, N., Miura, M., Niioka, T. et al. Influence of H2-receptor antagonists and proton pump inhibitors on dasatinib pharmacokinetics in Japanese leukemia patients. Cancer Chemother Pharmacol 69, 999–1004 (2012). https://doi.org/10.1007/s00280-011-1797-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-011-1797-3