Abstract
Background
More and more preclinical studies support the idea that curcumin, a plant-derived natural polyphenol, could be a promising anticancer drug. However, poor bioavailability has limited its efficacy in clinical trials, and plasma curcumin levels remain low despite patients taking gram doses of curcumin.
Methods
This study aimed to evaluate the safety and pharmacokinetics of newly developed nanoparticle curcumin with increased water solubility (named THERACURMIN). Six healthy human volunteers were recruited and received THERACURMIN at a single oral dose of 150 mg. After an interval of 2 weeks, the same subjects then received THERACURMIN at a single dose of 210 mg. Plasma curcumin levels were measured at 0, 1, 2, 4, 6, and 24 h after THERACURMIN intake using high-performance liquid chromatography (HPLC).
Results
One subject reported grade 1 diarrhea after intake of 150 mg THERACURMIN. No other toxicities were observed in this study. C max for THERACURMIN at 150 and 210 mg was 189 ± 48 and 275 ± 67 ng/ml (mean ± SEM), respectively, and the area under the curve for 24 h was estimated to be 2,649 ± 350 and 3,649 ± 430 ng/ml × h (mean ± SEM), respectively. The t 1/2 was estimated to be 9.7 ± 2.1 h for 150 mg and 13.0 ± 3.3 h for 210 mg.
Conclusion
THERACURMIN can safely increase plasma curcumin levels in a dose-dependent manner at least up to 210 mg without saturating the absorption system. To the best of our knowledge, THERACURMIN is the first nanoparticle formulation of curcumin that demonstrates improved bioavailability in human subjects. We believe this compound could be a promising tool when testing the potential anticancer effects of curcumin in clinical trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Curcumin is derived from turmeric (Curcuma longa) and is a natural polyphenol. Curcumin has long been used as a food, coloring agent, and traditional medicine. More and more data support the idea that this chemical could be a promising anticancer drug [1, 8, 31]. Several investigators, including ourselves, have tested plasma curcumin levels in clinical trials and reported that plasma levels remained low despite taking gram doses of curcumin [7, 10, 14, 27]. Furthermore, more than 8 g of curcumin intake did not increase blood curcumin levels in healthy volunteers [34]. Thus, poor bioavailability is the major weak point of curcumin and has been the main hurdle for physicians seeking to verify the therapeutic efficacy of this promising agent in clinical trials. Therefore, many researchers are now focusing on improving its bioavailability through several approaches including innovative drug delivery systems (liposomes, nanoparticles, and phospholipids) [2, 4, 6, 9, 11, 15, 17–19, 22, 24, 26, 29, 30, 32], the use of adjuvants [28], or the development of new curcumin analogs [13, 20, 23]. One of these approaches, a nanoparticle-based drug delivery system, has now been widely used to improve the water solubility of hydrophobic agents [3, 5, 12, 21]. By applying this nanoparticle-based drug delivery system to curcumin, a new form of curcumin (THERACURMIN) has been developed. THERACURMIN has improved water solubility with its mean particle size of 0.19 μm, and oral administration of THERACURMIN demonstrated more than 30-fold higher bioavailability compared with that of conventional curcumin in rat models [25]. Furthermore, C max for THERACURMIN at 30 mg was 30 ng/ml, while it was lower than 2 ng/ml after 30 mg of conventional curcumin intake in healthy human subjects [25]. However, it was not determined whether higher doses of THERACURMIN could safely increase plasma curcumin levels in a dose-dependent manner.
Therefore, in this study, we aimed to determine the safety and improved bioavailability of THERACURMIN at dose levels higher than 30 mg.
Materials and methods
Preparation of THERACURMIN
THERACURMIN was provided by the Theravalues Corporation (Tokyo, Japan). THERACURMIN was prepared as follows. Firstly, gum ghatti, which mainly consists of polysaccharides obtained from the exudation of ghatti trees, was dissolved in water to make gum ghatti solution. Curcumin powder was mixed into this solution, and water and glycerin were added to adjust the weight. The mixture was ground using a wet grinding mill (DYNO-MILL®KDL, Willy A Bachofen AG) and then dispersed by a high-pressure homogenizer (Homogenizer 15MR-8TA, APV Gaulin). Stable THERACURMIN was obtained from this procedure. The particle size of THERACURMIN was measured by a laser diffraction scattering method using Microtrac MT-30000II (Microtrac Inc., Montgomeryville, USA). THERACURMIN consisted of 10% curcumin, 2% other curcuminoids such as demethoxycurcumin and bisdemethoxycurcumin, 46% glycerin, 4% gum ghatti, and 38% water. THERACURMIN was provided in capsule form, and each capsule contained 30 mg of THERACURMIN.
Clinical trial design
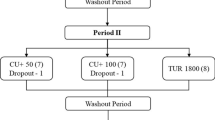
Six healthy human volunteers with normal organ function were recruited. None of the subjects were taking daily medications. They were asked to avoid all foods containing high concentrations of curcumin within 1 day before and 1 day after THERACURMIN intake. Initially, the six subjects received THERACURMIN at a single dose of 150 mg (level 0). Adverse events were graded based on the National Cancer Institute Common Toxicity Criteria version 3.0 [33]. Any grade 3 or higher adverse events were predefined as dose-limiting toxicities (DLT). If the incidence of DLT was two or lower out of six subjects, then we planned to evaluate the safety of THERACURMIN at a single dose of 210 mg (level 1) in the same subjects without DLT at level 0 after an interval of 2 weeks. Blood samples (2 ml) were collected in tubes containing EDTA just before THERACURMIN intake (0 h) and at 1, 2, 4, 6, and 24 h after THERACURMIN intake. The protocol was approved by the institutional review board at Kyoto University Hospital and registered in the University Hospital Medical Information Network (UMIN) Clinical Trial Registry (ID 000003488). All protocol procedures were carried out at Kyoto University Hospital.
Sample preparation and measurement of plasma curcumin levels using an HPLC–MS/MS system
Plasma curcumin levels were measured as previously reported [14]. A 0.1-ml aliquot of each plasma sample was transferred to a 10-ml glass tube, and then 0.11 ml of 0.1 M sodium acetate buffer (pH 5.0) containing 1,000 U β-glucuronidase was added. The resulting solutions were incubated to hydrolyze the curcumin conjugates at 37°C for 1 h. Following the addition of 10 μl of internal standard (IS) working solution (500 ng/ml), 0.5 ml of chloroform was added as an extraction solvent. The sample was vortexed for 1 min followed by ultrasonic vibration for 15 min and then centrifugation at 1610 g for 5 min. The organic layer was transferred to a 1-ml glass tube and evaporated to dryness using a centrifuge concentrator. The dried extract was reconstituted in 100 μl of 50% acetonitrile (MeCN) containing 0.05% formic acid (FA) and then centrifuged at 7,700×g for 10 min. A 10-μl aliquot of the supernatant from the reconstituted sample solution was injected into the chromatographic system.
The high-performance liquid chromatography–tandem mass spectrometry (HPLC–MS/MS) system consisted of Prominence micro-LC system (Shimadzu, Kyoto, Japan) and an API 3200 tandem mass spectrometer (Applied Biosystems, CA, USA) with electrospray ionization (ESI). Samples were subjected to Atlantis T3 (2.1 × 150 mm, 3 μm) (Waters, Milford, USA) as a separation C-18 column using a gradient of binding solvent (0.05% FA/H2O) and elution solvent (0.05% FA/MeCN) at a flow rate of 0.2 ml/min and a column temperature of 40°C. Separation of samples was conducted by a 35-min linear gradient (5–95% elution solvent). The mass spectrometer was operated under multiple reaction monitoring (MRM) mode with a collision energy of 23 eV for curcumin and 33 eV for mepronil. The transitions (precursor to product) monitored were m/z 369 → 285 for curcumin and 270 → 119 for mepronil. Chromatograms were integrated using the ANALYST version 1.5 software.
Stock solutions of curcumin and mepronil were prepared at a concentration of 1000 ng/ml in methanol (MeOH). The stock solution of mepronil was further diluted with 55% MeOH to prepare a calibration standard at a concentration of 100 ng/ml. The stock solution of curcumin was further diluted with 62% MeOH to prepare a calibration standard at a concentration of 200 ng/ml. Curcumin solution (200 ng/ml) was diluted with 50% MeOH to prepare the following standard solutions: 0.4, 0.8, 1.6, 3.1, 6.3, 12.5, 25.0, 50.0, and 100.0 ng/ml. These solutions were mixed with IS solution (100 ng/ml) at a ratio of 1:1 to prepare IS-containing calibration samples of 0.2–100.0 ng/ml (curcumin) and 50 ng/ml (mepronil). Stock solution (1,000 ng/ml) of mepronil was further diluted with MeOH to prepare the IS working solution at a concentration of 500 ng/ml.
Pharmacokinetic analysis
Area under the curve (AUC) is calculated using the trapezoidal method. Maximum concentrations (C max) and T max are the observed values. The t 1/2 value was calculated by dividing 0.693 by the terminal rate constant, which was derived from the slope of the natural log-transformed concentrations and times on the terminal elimination phase of the decay curve.
Results
Subjects and adverse events
Six healthy Japanese volunteers consisted of five men and one woman (mean age, 44 years; range, 38–51 years; mean body mass index, 24.4; range, 20.2–27.8). Only one subject (case 1, Table 1) reported grade 1 diarrhea lasting from day 1 to day 4 after 150 mg of THERACURMIN intake. However, diarrhea did not recur after the second, 210 mg dose of THERACURMIN in this subject. No other adverse events were observed in this study.
Plasma concentration of total curcumin
Figure 1 shows the size characterization of THERACURMIN using a laser diffraction scattering method, and Fig. 2 shows representative HPLC chromatograms of plasma after enzymatic hydrolysis. Peak plasma curcumin levels after 150 mg THERACURMIN intake ranged from 152 to 285 ng/ml and C max was 189 ± 48 ng/ml (mean ± SEM), while peak plasma curcumin levels after 210 mg of THERACURMIN intake ranged from 221 to 594 ng/ml and C max was 275 ± 67 ng/ml (mean ± SEM) (Fig. 3). The area under the curve for 24 h was estimated to be 2,649 ± 350 and 3,649 ± 430 ng/ml × h (mean ± SEM), respectively. The t 1/2 was estimated to be 9.7 ± 2.1 h for 150 mg and 13.0 ± 3.3 h for 210 mg. Total curcumin was still detectable in plasma at the 24-h time point.
Discussion
A number of preclinical studies have demonstrated that curcumin could be a promising anticancer drug [1, 8, 31]. However, poor bioavailability is the major weak point in its clinical application: plasma curcumin levels remain low despite taking gram doses of curcumin [7, 10, 14, 16, 27, 28] (Table 2). Lao et al. conducted a dose-escalation study of curcumin in twenty-four healthy volunteers and could detect plasma curcumin in only two subjects who took 10 g or 12 g of oral curcumin [16]. In another study by Garcea et al., only trace amounts of curcumin were detected after intake of 3.6 g oral curcumin [10]. Furthermore, intake of more than 8 g curcumin per day was not acceptable to patients [7] and could not increase the blood curcumin levels, probably due to saturation of the absorption system [34]. Therefore, improving bioavailability is essential in order to see the potential benefits of curcumin in clinical studies.
Nanoparticle-based drug delivery systems are suitable for improving water solubility of hydrophobic agents like curcumin, and various forms of nanoparticle curcumin have recently been synthesized [2, 6, 9, 11, 15, 22, 24, 26, 29, 30]. Bisht et al. have synthesized polymeric nanoparticle-encapsulated curcumin composed of N-isopropylacrylamide, N-vinyl-2-pyrrolidone, and poly-ethyleneglycol-monoacrylate and reported that the efficacy of this nanoparticle-encapsulated curcumin was similar to that of conventional curcumin in vitro and in vivo [6]. Shaikh et al. have also reported the improved bioavailability of curcumin with nanoparticle encapsulation in rat models [26]. Similarly, THERACURMIN has improved water solubility with its mean particle size of 0.19 μm (Fig. 1), and oral administration of THERACURMIN demonstrated more than 30-fold higher bioavailability compared with that of conventional curcumin in rat models. C max for THERACURMIN at 30 mg was 30 ng/ml, while it was lower than 2 ng/ml after 30 mg of conventional curcumin intake in healthy human subjects [25]. However, it was not determined whether higher doses of THERACURMIN could safely increase plasma curcumin levels in a dose-dependent manner. Therefore, we proceeded to determine the safety and improved bioavailability of THERACURMIN at dose levels higher than 30 mg.
With a dose of 150 mg of THERACURMIN, we observed the plasma curcumin level (189 ± 48 ng/ml, mean ± SEM), which compared well with the level observed after intake of 8 g of conventional curcumin in our previous study in pancreatic cancer patients (134 ± 70 ng/ml) [14], or in other previous studies using gram doses of curcumin (Table 2). Only one subject reported grade 1 diarrhea lasting for 4 days after 150 mg of THERACURMIN intake and no DLT was observed. Therefore, we proceeded to evaluate a dose of 210 mg of THERACURMIN in the same subjects after an interval of 2 weeks. As expected, plasma curcumin levels increased in a dose-dependent manner (275 ± 67 ng/ml, mean ± SEM) without saturating the absorption system. No adverse events including diarrhea, which was observed at a dose of 150 mg, were reported.
Our current results demonstrate that THERACURMIN can safely increase the plasma curcumin level in a dose-dependent manner at least up to 210 mg. In rat models, THERACURMIN was able to increase plasma curcumin levels in a dose-dependent manner up to at least 80 mg/kg without increasing toxicity (unpublished data). This suggests that an intake of more than 210 mg of THERACURMIN may be able to increase plasma curcumin levels higher without saturating the absorption system in human subjects, and further studies are now underway to test this hypothesis.
To the best of our knowledge, THERACURMIN is the first nanoparticle formulation that demonstrates improved bioavailability in human subjects. We believe this compound could be a promising tool when testing the potential anticancer effects of curcumin in clinical trials. Several clinical trials are now underway to evaluate the therapeutic efficacy of THERACURMIN in cancer patients.
References
Anand P, Kunnumakkara AB, Newman RA, Aggarwal BB (2007) Bioavailability of curcumin: problems and promises. Mol Pharm 4:807–818
Anand P, Nair HB, Sung B, Kunnumakkara AB, Yadav VR, Tekmal RR, Aggarwal BB (2010) Design of curcumin-loaded PLGA nanoparticles formulation with enhanced cellular uptake, and increased bioactivity in vitro and superior bioavailability in vivo. Biochem Pharmacol 79:330–338
Ankola DD, Viswanad B, Bhardwaj V, Ramarao P, Kumar MN (2007) Development of potent oral nanoparticulate formulation of coenzyme Q10 for treatment of hypertension: can the simple nutritional supplements be used as first line therapeutic agents for prophylaxis/therapy? Eur J Pharm Biopharm 67:361–369
Antony B, Merina B, Iyer VS, Judy N, Lennertz K, Joyal S (2008) A pilot cross-over study to evaluate human oral bioavailability of BCM-95CG (Biocurcumax), a novel Bioenhanced preparation of curcumin. Indian J Pharm Sci 70:445–449
Bala I, Bhardwaj V, Hariharan S, Kharade SV, Roy N, Ravi Kumar MN (2006) Sustained release nanoparticulate formulation containing antioxidant-ellagic acid as potential prophylaxis system for oral administration. J Drug Target 14:27–34
Bisht S, Feldmann G, Soni S, Ravi R, Karikar C, Maitra A (2007) Polymeric nanoparticle-encapsulated curcumin (“nanocurcumin”): a novel strategy for human cancer therapy. J Nanobiotechnol 5:3
Cheng AL, Hsu CH, Lin JK, Hsu MM, Ho YF, Shen TS, Ko JY, Lin JT, Lin BR, Ming-Shiang W, Yu HS, Jee SH, Chen GS, Chen TM, Chen CA, Lai MK, Pu YS, Pan MH, Wang YJ, Tsai CC, Hsieh CY (2001) Phase I clinical trial of curcumin, a chemopreventive agent, in patients with high-risk or pre-malignant lesions. Anticancer Res 21:2895–2900
Corson TW, Crews CM (2007) Molecular understanding and modern application of traditional medicines: triumphs and trials. Cell 130:769–774
Das RK, Kasoju N, Bora U (2010) Encapsulation of curcumin in alginate-chitosan-pluronic composite nanoparticles for delivery to cancer cells. Nanomedicine 6:153–160
Garcea G, Berry DP, Jones DJ, Singh R, Dennison AR, Farmer PB, Sharma RA, Steward WP, Gescher AJ (2005) Consumption of the putative chemopreventive agent curcumin by cancer patients: assessment of curcumin levels in the colorectum and their pharmacodynamic consequences. Cancer Epidemiol Biomarkers Prev 14:120–125
Gupta V, Aseh A, Rios CN, Aggarwal BB, Mathur AB (2009) Fabrication and characterization of silk fibroin-derived curcumin nanoparticles for cancer therapy. Int J Nanomedicine 4:115–122
Hariharan S, Bhardwaj V, Bala I, Sitterberg J, Bakowsky U, Ravi Kumar MN (2006) Design of estradiol loaded PLGA nanoparticulate formulations: a potential oral delivery system for hormone therapy. Pharm Res 23:184–195
John VD, Kuttan G, Krishnankutty K (2002) Anti-tumour studies of metal chelates of synthetic curcuminoids. J Exp Clin Cancer Res 21:219–224
Kanai M, Yoshimura K, Asada M, Imaizumi A, Suzuki C, Matsumoto S, Nishimura T, Mori Y, Masui T, Kawaguchi Y, Yanagihara K, Yazumi S, Chiba T, Guha S, Aggarwal BB (2010) A phase I/II study of gemcitabine-based chemotherapy plus curcumin for patients with gemcitabine-resistant pancreatic cancer. Cancer Chemother Pharmacol [Epub ahead of print]
Koppolu B, Rahimi M, Nattama S, Wadajkar A, Nguyen KT (2010) Development of multiple-layer polymeric particles for targeted and controlled drug delivery. Nanomedicine 6:355–361
Lao CD, MTt Ruffin, Normolle D, Heath DD, Murray SI, Bailey JM, Boggs ME, Crowell J, Rock CL, Brenner DE (2006) Dose escalation of a curcuminoid formulation. BMC Complement Altern Med 6:10
Li L, Braiteh FS, Kurzrock R (2005) Liposome-encapsulated curcumin: in vitro and in vivo effects on proliferation, apoptosis, signaling, and angiogenesis. Cancer 104:1322–1331
Liu A, Lou H, Zhao L, Fan P (2006) Validated LC/MS/MS assay for curcumin and tetrahydrocurcumin in rat plasma and application to pharmacokinetic study of phospholipid complex of curcumin. J Pharm Biomed Anal 40:720–727
Marczylo TH, Verschoyle RD, Cooke DN, Morazzoni P, Steward WP, Gescher AJ (2007) Comparison of systemic availability of curcumin with that of curcumin formulated with phosphatidylcholine. Cancer Chemother Pharmacol 60:171–177
Mosley CA, Liotta DC, Snyder JP (2007) Highly active anticancer curcumin analogues. Adv Exp Med Biol 595:77–103
Mu L, Feng SS (2003) A novel controlled release formulation for the anticancer drug paclitaxel (Taxol): PLGA nanoparticles containing vitamin E TPGS. J Control Release 86:33–48
Mukerjee A, Vishwanatha JK (2009) Formulation, characterization and evaluation of curcumin-loaded PLGA nanospheres for cancer therapy. Anticancer Res 29:3867–3875
Ohori H, Yamakoshi H, Tomizawa M, Shibuya M, Kakudo Y, Takahashi A, Takahashi S, Kato S, Suzuki T, Ishioka C, Iwabuchi Y, Shibata H (2006) Synthesis and biological analysis of new curcumin analogues bearing an enhanced potential for the medicinal treatment of cancer. Mol Cancer Ther 5:2563–2571
Sahu A, Bora U, Kasoju N, Goswami P (2008) Synthesis of novel biodegradable and self-assembling methoxy poly(ethylene glycol)-palmitate nanocarrier for curcumin delivery to cancer cells. Acta Biomater 4:1752–1761
Sasaki H, Sunagawa Y, Takahashi K, Imaizumi A, Fukuda H, Hashimoto T, Wada H, Katanasaka Y, Kakeya H, Fujita M, Hasegawa K, Morimoto T (2011) Innovative preparation of curcumin for improved oral bioavailability. Biol Pharm Bull (in press)
Shaikh J, Ankola DD, Beniwal V, Singh D, Kumar MN (2009) Nanoparticle encapsulation improves oral bioavailability of curcumin by at least 9-fold when compared to curcumin administered with piperine as absorption enhancer. Eur J Pharm Sci 37:223–230
Sharma RA, Euden SA, Platton SL, Cooke DN, Shafayat A, Hewitt HR, Marczylo TH, Morgan B, Hemingway D, Plummer SM, Pirmohamed M, Gescher AJ, Steward WP (2004) Phase I clinical trial of oral curcumin: biomarkers of systemic activity and compliance. Clin Cancer Res 10:6847–6854
Shoba G, Joy D, Joseph T, Majeed M, Rajendran R, Srinivas PS (1998) Influence of piperine on the pharmacokinetics of curcumin in animals and human volunteers. Planta Med 64:353–356
Shutava TG, Balkundi SS, Vangala P, Steffan JJ, Bigelow RL, Cardelli JA, O’Neal DP, Lvov YM (2009) Layer-by-layer-coated gelatin nanoparticles as a vehicle for delivery of natural polyphenols. ACS Nano 3:1877–1885
Sou K, Inenaga S, Takeoka S, Tsuchida E (2008) Loading of curcumin into macrophages using lipid-based nanoparticles. Int J Pharm 352:287–293
Strimpakos AS, Sharma RA (2008) Curcumin: preventive and therapeutic properties in laboratory studies and clinical trials. Antioxid Redox Signal 10:511–545
Takahashi M, Uechi S, Takara K, Asikin Y, Wada K (2009) Evaluation of an oral carrier system in rats: bioavailability and antioxidant properties of liposome-encapsulated curcumin. J Agric Food Chem 57:9141–9146
Trotti A, Colevas AD, Setser A, Rusch V, Jaques D, Budach V, Langer C, Murphy B, Cumberlin R, Coleman CN, Rubin P (2003) CTCAE v3.0: development of a comprehensive grading system for the adverse effects of cancer treatment. Semin Radiat Oncol 13:176–181
Vareed SK, Kakarala M, Ruffin MT, Crowell JA, Normolle DP, Djuric Z, Brenner DE (2008) Pharmacokinetics of curcumin conjugate metabolites in healthy human subjects. Cancer Epidemiol Biomarkers Prev 17:1411–1417
Acknowledgments
This work was supported by the Grant-in-Aid for Young Scientists (21790661) from the Japan Society for the Promotion of Science and Japanese Research Foundation for Clinical Pharmacology.
Conflict of interest
A. Imaizumi is a consultant to Theravalues Corporation. Y. Otsuka and H. Sasaki are employees of Theravalues Corporation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kanai, M., Imaizumi, A., Otsuka, Y. et al. Dose-escalation and pharmacokinetic study of nanoparticle curcumin, a potential anticancer agent with improved bioavailability, in healthy human volunteers. Cancer Chemother Pharmacol 69, 65–70 (2012). https://doi.org/10.1007/s00280-011-1673-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-011-1673-1