Abstract
Curcumin is a natural product with many interesting pharmacological properties. However, these are offset by the particularly poor biopharmaceutical properties. The oral bioavailability of curcumin in humans is very low, mainly due to low solubility, poor stability, and extensive metabolism. This has led to multiple approaches to improve bioavailability, including administration of curcumin with metabolism inhibitors, formulation into nanoparticles, modification of the curcumin structure, and development of curcumin prodrugs. In this paper, we focus on the pharmacokinetic outcomes of these approaches. Pharmacokinetic parameters of curcumin after release from prodrugs are dependent on the linker between curcumin and the promoiety, and the release itself may depend on the physiological and enzymatic environment at the site of cleavage. This is an area in which more data are required for rational design of improved linkers. Cytotoxicity of curcumin prodrugs seems to correlate well with cellular uptake in vitro, but the in vivo relevance is uncertain. We conclude that improved experimental and theoretical models of absorption of curcumin prodrugs, development of accurate analytical methods for simultaneous measurement of plasma levels of prodrug and released curcumin, and acquisition of more pharmacokinetic data in animal models for dose prediction in humans are required to facilitate movement of curcumin prodrugs into clinical trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Curcumin has interesting pharmacological effects, but poor biopharmaceutical properties that may be overcome by design of prodrugs of curcumin |
We present a systematic evaluation of pharmacokinetic parameters of curcumin after release from prodrugs to improve understanding of the effects of the molecular design and physiological environment on curcumin release |
New analytical methods for measurement of plasma levels of prodrugs and released curcumin, acquisition of more pharmacokinetic data, and improved theoretical models of absorption of curcumin prodrugs are needed for dose prediction in humans |
1 Introduction
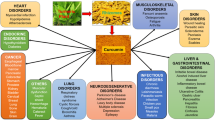
Curcumin is a bioactive phytochemical that is found in turmeric (Curcuma longa L.) and has many interesting pharmacological properties. We have recently published an extensive review of these properties and the reader is directed to this review for further details [1]. Based on these activities, curcumin has been evaluated as a chemotherapeutic agent [2, 3] and has been shown to be beneficial for Alzheimer’s disease [4, 5], cardiovascular health [6], inflammation [7], arthritis [8], metabolic disorders [9] and immunodeficiency conditions [10] in preclinical and clinical trials. Curcumin also has proven safety, with a dose of 8 g per day being well tolerated in a phase II trial for advanced pancreatic cancer [11].
These favorable pharmacological properties are offset by difficulty with the administration of curcumin. This is because curcumin has low water solubility (0.00134 mg/mL) at 25 °C [12] and is unstable at neutral and basic pH due to dissociation of the phenolic proton leading to degradation [13]. Curcumin degradation is blocked by antioxidants at pH 7.4 [14], but the molecule is relatively unstable in the small intestine. Poor absorption coupled with extensive metabolism of curcumin molecules that are absorbed markedly limits the oral bioavailability [15–17]. For example, when curcumin was administered orally to Sprague–Dawley rats at a dose of 1 g/kg, negligible amounts were found in rat plasma and 75 % was excreted in feces [18]. Curcumin given orally at 2 g/kg in rats gives a maximum serum concentration of 1.35 ± 0.23 µg/mL in 0.83 h with an elimination half-life of 1.70 ± 0.58 h, but in humans, an oral dose of 2 g results in very low or undetectable amounts of curcumin in serum, with a maximum concentration of 0.006 ± 0.005 µg/mL after 1 h [19]. Thus, therapeutic levels of curcumin are not attainable following oral administration [20], and the intravenous route is no more effective [1].
Curcumin undergoes extensive metabolism in the liver and intestine. In human hepatocyte suspensions, 35 % of the initial curcumin remains after 2 h of incubation, and the level in rat hepatocyte suspensions was close to the detection limit after the same incubation time [21]. Metabolism in hepatocytes yields major metabolites of hexahydrocurcumin and hexahydrocurcuminol, but curcumin glucuronide and curcumin sulfate are the predominant metabolites found in rat plasma after oral or intravenous administration [21]. An in vitro study of metabolism of curcumin in subcellular fractions of rat and human intestines showed the presence of hexahydrocurcumin and curcumin sulfate in cytosolic fractions of both species and curcumin glucuronide in microsomal fractions [22]. The presence of curcumin glucuronide and curcumin glucuronide/sulfate conjugates in rat plasma after oral administration of curcumin suggests that glucuronidation of curcumin occurs primarily in the intestinal mucosa, with subsequent conjugation with sulfate in the liver [23]. Metzler et al. have published a comprehensive review of metabolism of curcumin [24].
The useful pharmacological properties but poor bioavailability of curcumin have stimulated development of technologies to improve oral delivery of the compound. Here, we will discuss techniques including the prodrug approach, co-administration of curcumin with a metabolism inhibitor, nanotechnology-based curcumin delivery and structural modifications with a focus on the pharmacokinetic outcomes of these methods.
2 Biopharmaceutics and Pharmacokinetics of Curcumin Prodrugs
Prodrugs are pharmacologically inactive derivatives of drugs that are biotransformed chemically or enzymatically to the active drug, and are generally used to improve the biopharmaceutics or pharmacokinetic properties of the drug. For curcumin, attachment of promoieties to the phenolic hydroxyl groups via a biodegradable linkage is the common approach. We have recently published a review of curcumin prodrugs organized by the types of promoieties [25]. Here, we focus on the biopharmaceutics and pharmacokinetics of curcumin prodrugs (Table 1). To our knowledge, compounds 13-15 are the only three curcumin prodrugs for which pharmacokinetic data are available (Table 2).
Dubey et al. and Parvathy et al. prepared curcumin prodrugs as mono- and diesters of amino acids (Table 1, compounds 1–12) [26, 27]. Compound 3 has a significant antibacterial effect, which was attributed to slow metabolism, enhanced water solubility, and better cellular uptake [26]. This conclusion is supported by the aqueous solubility of compounds 2, 4 and 6–12, which ranges from 1–10 mg/mL at pH 6.5 [27].
Singh et al. prepared di-O-decanoyl curcumin (Table 1, compound 13), a lipidic prodrug of curcumin [28]. The pharmacokinetics of compound 13 were investigated by Han et al. in intravenous administration to male Wistar rats at a dose equivalent to 1 mg/kg of curcumin (Table 2) [29]. Following administration, the concentration of compound 13 and curcumin released by compound 13 declined slowly. The released curcumin was detectable for up to 24 h, while curcumin from direct intravenous (i.v.) injection was below the lower limit of quantification (LLOQ) after 20 min. The elimination half-life of curcumin was extended to approximately 7 h, and the AUC of converted curcumin was fourfold higher than that of direct i.v. administered curcumin. These results suggest that compound 13 can provide prolonged plasma levels of curcumin after i.v. administration.
Wei et al. formulated oily microsuspensions and nanosuspensions of compound 13 and examined the pharmacokinetic properties of these formulations given i.m. in male Wistar rats at a dose of 100 mg/kg [30]. After dosing for 1 day, about 70 and 50 % of compound 13 was cleared from the injection sites for the micro- and nanosuspension, respectively. On day 4 after injection, 6.8 and 16.7 % of compound 13 were present at the respective injection sites. The plasma level of compound 13 was below the LLOQ, but the plasma concentrations of curcumin were quantifiable, with plasma levels of 2–6 μg/L from the microsuspension and ≥10 μg/L from the nanosuspension sustained for up to 10 days in rats. The C max of curcumin from the nanosuspension was significantly higher than that derived from the microsuspention (69.0 vs. 18.5 μg/L). The different plasma concentrations between these two formulations might be due to the difference in dissolution behavior between micro- and nanoparticles. In contrast to plasma levels, the curcumin concentration in rat brain was lower than the LLOQ and compound 13 was quantifiable. In addition, compound 13 was detected in spleen, lung, liver, kidney and heart. Amounts of compound 13 and converted curcumin were found significantly in heart and spleen on days 4 and 7 after dosing.
Curcumin diethyl disuccinate (Table 1, compound 14), an ethyl succinate ester of curcumin, has been prepared and investigated for biological activities by Wichitnithad et al. and Wongsrisakul et al. [31, 32]. Compound 14 has a higher cytotoxic effect in Caco-2 cells compared to curcumin (IC50:1.84 ± 0.11 vs. 3.31 ± 0.16 µM). This compound is more stable than curcumin at pH 7.4 and can release curcumin in plasma. Bangphumi et al. investigated the pharmacokinetics of compound 14 in male Wistar rats [33]. The plasma concentration of converted curcumin achieved the highest level of 676 µg/L at 5 min after compound 14 was given intravenously at a dose equivalent to 20 mg/kg curcumin. The plasma level of curcumin decreased markedly within 30 min and then gradually reached a secondary maximum concentration at 2 h. In comparison with direct i.v. injection of curcumin, curcumin derived from compound 14 had a significant increase in volume of distribution and mean resident time. The elimination half-life was increased slightly while other pharmacokinetic parameters did not differ significantly from direct i.v. injection of curcumin. However, when compound 14 was given orally at a dose equivalent to 40 mg/kg of curcumin, the oral bioavailability of curcumin was not improved. Compound 14 was undetectable in plasma, tissue, urine and feces samples after being given to rats intravenously or orally. Curcumin derived from i.v. administration of compound 14 accumulated in brain, heart, intestine, spleen, kidney and liver at higher levels than those after treatment with native curcumin. Rats intravenously administered with compound 14 had higher tissue accumulation of curcumin glucuronide in brain, heart, lung, stomach, intestine, spleen, kidney and liver compared to those that received a direct curcumin injection. About 30–40 % of compound 14 given orally was found as glucuronide metabolite in feces at 24–48 h post-dosing, while negligible amounts of curcumin and its glucuronide conjugate were detected in urine from 0 to 48 h after oral or i.v. administration.
Compound 15 (Table 1) is a curcumin-oligo(ethylene glycol) conjugate with a β-thioester linker that readily forms a nanomicelle structure with an average diameter of 37 ± 3.4 nm and shows greater cytotoxicity than free curcumin [34]. Intravenous injection of compound 15 at a dose equivalent to 6.25 mg/kg of curcumin in athymic nude mice gave a peak curcumin plasma level of 6.8 µg/mL and this level was maintained at 0.1–0.2 µg/mL for 2 h post-injection. Pharmacokinetic parameters of compound 15 were not calculated. Curcumin was highly distributed to liver, spleen and tumor tissues after i.v. administration of compound 15. Interestingly, the concentration of curcumin in spleen decreased after injection for 1 h while that in tumor tissues increased to more than 8 µg/g of tissue. This accumulation behavior could be due to enhanced permeability and retention in tumor tissue.
3 Cellular Uptake of Curcumin Prodrugs
Curcumin prodrugs may enter cells through passive diffusion, endocytosis or transport mechanisms, and cellular uptake data are generally consistent with cytotoxicity. A summary of studies of cellular uptake of curcumin conjugates is given in Table 3. Internalization of compound 14 (described above) as a chitosan-alginate nanoparticle formulation was assessed in Caco-2 cells using confocal laser scanning microscopy (CLSM) [35]. After incubation for 72 h, compound 14 was internalized by the cells, and the nanoparticle formulation enhanced uptake of compound 14. Compound 15 (also described above) can form nanomicelles, and was used to encapsulate doxorubicin for cellular uptake [34]. Fluorescence microscopy showed no doxorubicin in MCF-7/ADR cells after incubation with 2 µg/mL free doxorubicin for 4 h. In contrast, doxorubicin-loaded nanoparticles of compound 15 delivered doxorubicin at the same dose into MCF-7/ADR cells efficiently in 4 h. This may be due to nanoparticles being internalized by endocytosis. The released curcumin may also downregulate MDR proteins, which promotes intracellular retention of doxorubicin.
Sarika et al. used succinic acid as a linker to prepare galactosylated pullulan-curcumin (Table 1, compound 16) and pullulan-curcumin (Table 1, compound 17) conjugates [36]. These conjugates form self-assembling spherical micelles in an aqueous medium with CMCs of 0.027 and 0.031 mg/mL, respectively, and enhance the aqueous solubility of curcumin by up to 200-fold and 314-fold, respectively. The stability of curcumin also increased significantly. Compound 17 showed greater cytotoxicity against HepG2 cells than compound 16 and free curcumin. Compounds 16 and 17 were evaluated for involvement of ASGPR in uptake in HepG2 cells. ASGPR, which is present on the surface of hepatocytes, recognizes and transports galactose-terminal molecules to lysosomes in the liver cells [37]. A higher fluorescence intensity of curcumin was found in HepG2 cells treated with compounds 16 and 17 compared to treatment with curcumin alone. Compound 16 exhibited stronger intensity than compound 17, due to higher internalization or slower metabolism of compound 16 in HepG2 cells.
Hyaluronic acid (HA) is a linear negatively charged polysaccharide with alternating units of D-glucuronic acid and N-acetylglucosamine. A HA-curcumin conjugate (Table 1, compound 18) is able to form a nanomicelle spontaneously and curcumin can be encapsulated in the hydrophobic core, with a resultant increase in aqueous solubility of curcumin [38]. Alginic acid is an anion polysaccharide containing subunits of β-D-mannuronic acid and its C-5 epimer α-L-guluronic acid. Dey et al. conjugated curcumin to alginic acid (Table 1, compound 19) and found significant improvement in the aqueous solubility and stability of curcumin at physiological pH [39]. Compound 19 also exhibited better cytotoxicity against L-929 mouse fibroblasts. Gum arabic is a branched, complex polysaccharide of arabinose, rhamnose, galactose and glucoronic acid residues that is derived from the acacia tree. A curcumin conjugate of this polysaccharide (Table 1, compound 20) showed more accumulation of curcumin in HepG2 cells due to the presence of galactose groups in gum arabic facilitating internalization, compared to free curcumin [37, 40]. CLSM of uptake in HepG2 and MCF-7 cells indicated that compound 20 and curcumin were located in cytoplasmic and nuclear compartments [40].
Polyethylene glycol (PEG) is a hydrophilic homopolymer of ethylene oxide with biocompatible properties. Safavy et al. used PEGs of 750 and 3500 Da to enhance the aqueous solubility of curcumin (Table 1, compounds 21 and 22) [20]. These compounds have half-lives for curcumin release of 60 and 200 min, respectively, and both have superior cytotoxic effects to unconjugated curcumin. Fluorescence microscopy showed internalization of compound 22 in PC-3 cells. Compound 22 exhibited higher fluorescence intensity of curcumin in these cells in comparison with free curcumin, and was retained in the nuclear compartment longer than curcumin. Conjugation of curcumin with PEG can prevent cellular efflux, which contributes to higher cytotoxic effects.
Amphiphilic block copolymers contain segments with large differences in solubility and are able to form self-assembling micelles in an aqueous environment while entrapping a hydrophobic drug in the micelle core. This increases the overall water solubility of the drug and prevents hydrolysis. As an illustration of this approach, Wang et al. prepared polymeric conjugates of curcumin (Table 1, compounds 23 and 24) using a PEG-PLA copolymer linked to curcumin via a pH-labile hydrazone [41]. Compound 23 self-assembles into a micelles with a CMC value of 2.6 ± 0.3 µM and releases small amounts of curcumin into buffer at pH 7.4 over 24 h. Since hydrazone is hydrolyzed at acidic pH, a higher release rate is obtained at pH 5.0 and 6.0. Compounds 23 and 24 are effectively internalized and localized in the cytoplasm of HeLa and HepG2 cells. However, compound 23 exhibits higher internalization, which may be due to different architecture of micelle formation. These results agree well with the superior cytotoxicity and curcumin release rate of compound 23.
Incorporation of an acetal group into the linker between the drug molecule and the polymer yields a pH-responsive drug delivery system. Li et al. synthesized an acetal-linked mPEG-PLA curcumin conjugate (Table 1, compound 25) and compared the pH-dependent curcumin release with that from compound 26 (Table 1), which acted as a control [42]. Cellular internalization of compound 25 was investigated in HepG2 cells in comparison with compound 26 and free curcumin. CLSM showed localization in cytosol and increased curcumin in cells with time, but the forms of curcumin could not be differentiated based on images from CLSM.
Yang et al. used Tris as a linker between mPEG-PLA and curcumin for multiple conjugation [43]. In comparison to a simple mPEG-PLA curcumin conjugate (Table 1, compound 27), a mPEG-PLA-Tris curcumin conjugate (Table 1, compound 28) had a higher particle size but a lower CMC value (7.8 ± 1.3 vs. 2.3 ± 0.4 μg/mL). The lower CMC indicates higher stability of the micelle. Compounds 27, 28 and their curcumin-loaded micelles were investigated for their cellular uptake in HepG2 cells compared with free curcumin. CLSM images showed that the micelles with and without loaded curcumin were located in the cytoplasm, while free curcumin was distributed in cytoplasmic and nuclear compartments, suggesting different cellular uptake mechanisms for free and micelle-bound curcumin.
Waghela et al. conjugated curcumin to PLGA directly (Table 1, compound 29) using the free carboxylic acid in PLGA [44]. Compound 29 effectively killed HCT 116 cells (human colorectal carcinoma) after incubation for 6–24 h. This conjugate had a slow curcumin release profile at physiological pH, which improved retention and cellular uptake of curcumin. HCT 116 cells treated with compound 29 showed intense fluorescence within the cells, while those treated with unconjugated curcumin did not show fluorescence at any time points.
Pluronic F68 (poloxamer 188) is a block copolymer used in pharmaceutical formulations. Cai et al. attached curcumin to F68 via a succinic acid linker to give compound 30 (Table 1) [45] and Fang et al. used cis-aconitic acid as a linker to connect curcumin to F68 to obtain compound 31 (Table 1) [46]. Compound 31 breaks down in acidic media and releases curcumin rapidly. It also exerts more anticancer activity than curcumin on human ovarian carcinoma and hepatocellular carcinoma cells. The enhanced cytotoxicity of compound 31 is consistent with its efficient cellular internalization. The fluorescence intensity of curcumin in cells treated with compound 31 increased significantly in a time-dependent manner. At 6 h, the fluorescence intensity of curcumin from compound 31 was higher than that in cells incubated with curcumin alone. Internalization of compound 31 decreased to 40 % after incubation for 6 h at 4 °C, compared to 37 °C, implying energy-dependent endocytosis. This was confirmed by pretreatment of the cells with 10 µM genistein, an endocytic inhibitor.
4 Other Approaches for Improvement of the Bioavailability of Curcumin
Examples of methods used for improvement of the solubility and bioavailability of curcumin are summarized in Table 4. One approach is use of a molecule that blocks metabolism of curcumin. Thus, Shoba et al. found that dosing of 20 mg/kg piperine, a UDP-glucuronosyltransferase (UGT) inhibitor, with 2 g/kg curcumin in rats improved the bioavailability of curcumin by 154 %, and that 2 g of curcumin coadministered with piperine in healthy human volunteers increased bioavailability by 2000 % [19]. In a cross-over design trial of the effect of piperine on pharmacokinetics of curcumin in six healthy male volunteers, co-administration of curcumin and piperine produced a two-fold enhancement of AUC of curcumin, compared to that with administration of curcumin alone [15]. Grill et al. recently compared the effects of four UGT inhibitors, piperine, quercetin, tangeretin and silibinin, on the oral bioavailability of mice, using a self-microemulsifying drug delivery system (SMEDDS) [47]. In mouse liver microsomes, silibinin and quercetin inhibited curcumin glucuronidation, but in vivo there was no difference in plasma concentrations of curcumin using SMEDDS with curcumin alone and curcumin plus tangeretin. However, SMEDDS with curcumin plus silibinin significantly increased the plasma level and improved the oral bioavailability of curcumin by 3.5-fold, compared to SMEDDS with curcumin alone.
Encapsulation of curcumin into nanotechnology-based drug delivery systems is another approach to improve the solubility, stability, and absorption of curcumin [15–17, 48, 49]. For example, Khalil et al. administered curcumin-loaded PLGA and PLGA-PEG nanoparticles to rats at a single dose of 50 mg/kg [50]. The PLGA and PLGA-PEG formulations increased the half-life of curcumin from 1 to 4 and 6 h, increased C max by 2.9- and 7.4-fold, and enhanced the bioavailability by 15.6- and 55.4-fold, respectively, compared to an aqueous curcumin suspension. The greater effect of the PLGA-PEG nanoparticles was due to a particular reduction in clearance of curcumin with this formulation.
Chemical modifications to the curcumin structure to improve solubility may come at the expense of a reduced therapeutic effect, since the phenolic hydroxyl and β-diketone moieties of curcumin are important for several pharmacological activities and the hydrophobicity of curcumin increases its affinity for biological targets [1]. A monocarbonyl curcumin analog, EF-24, has oral and intraperitoneal bioavailability of 60.1 and 34.7 %, respectively, after administration at 10 mg/kg to mice. However, the clearance of EF-24 exceeded the liver blood flow rate and the compound had a large volume of distribution. These results suggest that EF-24 is rapidly metabolized and extensively distributed to tissues after intravenous administration [51]. The development of curcumin analogs and their biological activities has recently been reviewed by Vyas et al. [52].
5 Challenges and Prospects for Pharmacokinetic and Metabolism Studies of Curcumin Prodrugs
The solubility, stability and lipophilicity are important physicochemical properties of curcumin prodrugs [53]. Several amino acid-curcumin conjugates show significantly improved aqueous solubility [27], and solubility and stability against hydrolysis can be improved using curcumin conjugates of hydrophilic polymers [20, 34, 36, 38–43, 45, 46, 54, 55]. However, there is currently no experimental lipophilicity data (logP or logD) for any curcumin prodrugs in the literatures. This gap in information can potentially be filled by computational prediction models. Our observation for curcumin and several prodrugs is that there is a general tendency for overestimation of solubility and rate of solution using current models. However, these models are improving and it is very likely that further improvements in parameterization will increase the accuracy of predictions for low-solubility compounds.
There are multiple transport mechanisms in the gastrointestinal, and human intestinal absorption cannot be fully predicted based on physicochemical properties and non-biological permeation models [56]. Therefore, biological intestinal absorption models including in vivo animal models, in situ intestinal segments, everted gut sacs, intestinal mucosa/Ussing chamber, isolated membrane vesicle and Caco-2 cell models have been widely used [57]. An intestinal permeation study is required to demonstrate enhanced intestinal absorption by a prodrug approach, but such studies have yet to be reported. As described above, there are only four reported animal pharmacokinetic studies of three curcumin prodrugs [29, 30, 33, 34]. ADME behaviors of curcumin prodrugs in animals are required so that preclinical pharmacokinetic data could be subjected to allometric scaling of drug doses for human studies. To date, animal pharmacokinetic data and in vivo toxicity of curcumin prodrugs are still limited and do not allow dose prediction for a clinical study in humans.
Curcumin prodrugs can be categorized by the nature of the curcumin-promoiety linkage, which is based on ester, ether, hydrazone and disulfide bonds. Some linkers liberate curcumin in specific conditions such as an acidic environment while others require specific enzymes or endogenous compounds such as glutathione to cleave the linker. Carboxylesterase such as acetylcholinesterase, butyrylcholinesterase, paraoxonase, and arylesterase play crucial roles in bioconversion of ester prodrugs to pharmacologically active forms [58–60], and the tissue distribution and substrate specificity of esterases is important in understanding the pharmacokinetic and biopharmaceutics properties of ester-based curcumin prodrugs. This issue is particularly important in quantification of ester- or amide-based curcumin prodrugs especially in cellular permeation or absorption studies. Due to interspecies differences in the type and substrate specificity of esterases present in biological matrices or tissues, the level of expression and substrate specificity of esterases should be determined in species used in preclinical studies of curcumin prodrugs [61]. To date, the specific enzymes that activate curcumin prodrugs and the sites of bioactivation have not been investigated. This and the lack of information on in vitro plasma stability and hepatic metabolism of curcumin prodrugs may hinder development of the compounds in preclinical and clinical studies.
In a pharmacokinetic study, collection of biological specimens (e.g. blood or plasma) from animals or humans is required. At this step, the stability of the curcumin prodrug needs to be taken into account. Stability of drug molecules and/or their metabolites in biological matrices is an important factor in quantitative analysis, and the instability of analytes during processes such as sample collection, handling, storage and extraction causes under- or overestimation of the analyte concentration, which leads to improper calculation of pharmacokinetic parameters. Ester-based curcumin prodrugs can undergo ex vivo ester bond cleavage by the same plasma esterases that mediate in vivo hydrolysis. Determination of these curcumin prodrugs in biological samples cannot be achieved if this is not blocked. Strategies to prevent ex vivo cleavage of curcumin prodrugs during bioanalysis include controlling the sample temperature, modifying pH of matrices, and adding esterase inhibitors [62, 63], with prior screening for appropriate inhibitors [64, 65]. Success in developing a curcumin prodrug as a drug depends on obtaining good pharmacokinetic profiles, for which an accurate and precise analytical method is essential. For example, compounds 13 and 14 could not be detected after administrations in rat. The undetected level of these prodrugs in biological samples could be due to complete hydrolysis in the samples or low sensitivity of the analytical method. Therefore, rapid hydrolysis resulting in very low amount of curcumin prodrugs is a concern during analytical method development. Recently, we have developed a new LC–MS/MS method that allows the determination of compound 14 in rat plasma using bis(4-nitrophenyl) phosphate (or BNPP), an esterase inhibitor, and a temperature control approach to prevent ex vivo hydrolysis of compound 14 [66]. The method was found to be successful in supporting a pharmacokinetic study of compound 14 in Wistar rats [66].
6 Conclusion
The interesting pharmacological properties but poor biopharmaceutics properties of curcumin have led to prodrug development for the delivery of curcumin. Most such prodrugs are in the very early stage of drug discovery and development, but several curcumin prodrugs have moved to preclinical studies. Biological evaluation of curcumin prodrugs has mainly been limited to in vitro toxicity and a possible lack of bioactivation in an in vitro model should be considered. In addition, only a few physicochemical properties have been determined and in vitro ADME assays for metabolic stability in plasma and liver tissues, metabolite identification, plasma protein binding, enzyme induction/inhibition and transporter assays have not been performed. Animal pharmacokinetic studies of curcumin prodrugs are also limited in number. Therefore, there is a need for increased preclinical development of curcumin prodrugs for prediction of human pharmacokinetics, pharmacodynamics, dose and drug–drug interaction.
References
El-Magboub A, et al. Biological targets and pharmacology of curcumin. In: Pouliquen DL, editor. Curcumin: synthesis, emerging role in pain management and health implications. Nova Science Publishers Inc: New York; 2014. p. 103–34.
Dona S, et al. Chemopreventive and chemotherapeutic potential of curcumin in breast cancer. Curr Drug Targets. 2012;13(14):1799–819.
Nautiyal J, et al. Combination of dasatinib and curcumin eliminates chemo-resistant colon cancer cells. J Mol Signal. 2011;6(1):1–11.
Begum AN, et al. Curcumin structure-function, bioavailability, and efficacy in models of neuroinflammation and alzheimer’s disease. J Pharmacol Exp Ther. 2008;326(1):196–208.
Ishrat T, et al. Amelioration of cognitive deficits and neurodegeneration by curcumin in rat model of sporadic dementia of Alzheimer’s type (SDAT). Eur Neuropsychopharm. 2009;19(9):636–47.
Nemmar A, Subramaniyan D, Ali BH. Protective effect of curcumin on pulmonary and cardiovascular effects induced by repeated exposure to diesel exhaust particles in mice. PLoS One. 2012;7(6):e39554.
Buadonpri W, et al. Synthetic curcumin inhibits carrageenan-induced paw edema in rats. J Health Res. 2009;23(1):11–6.
Chandran B, Goel A. A randomized, pilot study to assess the efficacy and safety of curcumin in patients with active rheumatoid arthritis. Phytother Res. 2012;26(11):1719–25.
Chuengsamarn S, et al. Curcumin extract for prevention of type 2 diabetes. Diabetes Care. 2012;35(11):2121–7.
Gandapu U, et al. Curcumin-loaded apotransferrin nanoparticles provide efficient cellular uptake and effectively inhibit HIV-1 replication in vitro. PLoS One. 2011;6(8):e23388.
Dhillon N, et al. Phase II trial of curcumin in patients with advanced pancreatic cancer. Clin Cancer Res. 2008;14(14):4491–9.
Carvalho DDM, et al. Production, solubility and antioxidant activity of curcumin nanosuspension. Food Sci Technol (Campinas). 2015;35(1):115–9.
Wang YJ, et al. Stability of curcumin in buffer solutions and characterization of its degradation products. J Pharm Biomed Anal. 1997;15(12):1867–76.
Oetari S, et al. Effects of curcumin on cytochrome P450 and glutathione S-transferase activities in rat liver. Biochem Pharmacol. 1996;51(1):39–45.
Anand P, et al. Bioavailability of curcumin: problems and promises. Mol Pharmaceut. 2007;4(6):807–18.
Prasad S, Tyagi AK, Aggarwal BB. Recent developments in delivery, bioavailability, absorption and metabolism of curcumin: the golden pigment from golden spice. Cancer Res Treat. 2014;46(1):2–18.
Liu W, et al. Oral bioavailability of curcumin: problems and advancements. J Drug Target. 2016;24(8):694–702.
Wahlström B, Blennow G. A study on the fate of curcumin in the rat. Acta Pharmacol Toxicol. 1978;43(2):86–92.
Shoba G, et al. Influence of piperine on the pharmacokinetics of curcumin in animals and human volunteers. Planta Med. 1998;64(4):353–6.
Safavy A, et al. Design and development of water-soluble curcumin conjugates as potential anticancer agents. J Med Chem. 2007;50(24):6284–8.
Ireson C, et al. Characterization of metabolites of the chemopreventive agent curcumin in human and rat hepatocytes and in the rat in vivo, and evaluation of their ability to inhibit phorbol ester-induced prostaglandin E2 production. Cancer Res. 2001;61(3):1058–64.
Ireson CR, et al. Metabolism of the cancer chemopreventive agent curcumin in human and rat intestine. Cancer Epidem Biomar. 2002;11(1):105–11.
Asai A, Miyazawa T. Occurrence of orally administered curcuminoid as glucuronide and glucuronide/sulfate conjugates in rat plasma. Life Sci. 2000;67(23):2785–93.
Metzler M, et al. Curcumin uptake and metabolism. BioFactors. 2013;39(1):14–20.
Rojsitthisak P, et al. Design, synthesis and biological activities of curcumin prodrugs. In: Pouliquen DL, editor. Curcumin: synthesis, emerging role in pain management and health implications. Nova Science Publishers Inc: New York; 2014. p. 135–76.
Dubey SK, et al. Design, synthesis and characterization of some bioactive conjugates of curcumin with glycine, glutamic acid, valine and demethylenated piperic acid and study of their antimicrobial and antiproliferative properties. Eur J Med Chem. 2008;43(9):1837–46.
Parvathy KS, Negi PS, Srinivas P. Curcumin–amino acid conjugates: synthesis, antioxidant and antimutagenic attributes. Food Chem. 2010;120(2):523–30.
Singh RK, et al. Synthesis, antibacterial and antiviral properties of curcumin bioconjugates bearing dipeptide, fatty acids and folic acid. Eur J Med Chem. 2010;45(3):1078–86.
Han YR, et al. A simple RP-HPLC method for the simultaneous determination of curcumin and its prodrug, curcumin didecanoate, in rat plasma and the application to pharmacokinetic study. Biomed Chromatogr. 2011;25(10):1144–9.
Wei XL, et al. Oily nanosuspension for long-acting intramuscular delivery of curcumin didecanoate prodrug: preparation, characterization and in vivo evaluation. Eur J Pharm Sci. 2013;49(2):286–93.
Wichitnithad W, et al. Synthesis, characterization and biological evaluation of succinate prodrugs of curcuminoids for colon cancer treatment. Molecules. 2011;16(2):1888–900.
Wongsrisakul J, et al. Antinociceptive effects of curcumin diethyl disuccinate in animal models. J Health Res. 2010;24(4):175–80.
Bangphumi K, et al. Pharmacokinetics of curcumin diethyl disuccinate, a prodrug of curcumin, in Wistar rats. Eur J Drug Metab Pharmacokinet. 2015;1–9.
Tang H, et al. Amphiphilic curcumin conjugate-forming nanoparticles as anticancer prodrug and drug carriers: in vitro and in vivo effects. Nanomedicine. 2010;5(6):855–65.
Bhunchu S, Rojsitthisak P, Rojsitthisak P. Effects of preparation parameters on the characteristics of chitosan–alginate nanoparticles containing curcumin diethyl disuccinate. J Drug Deliv Sci Technol. 2015;28:64–72.
Sarika PR, et al. Galactosylated pullulan–curcumin conjugate micelles for site specific anticancer activity to hepatocarcinoma cells. Colloids Surf B Biointerfaces. 2015;133:347–55.
Yan L, et al. Targeted delivery of macromolecular drugs: asialoglycoprotein receptor (ASGPR) expression by selected hepatoma cell lines used in antiviral drug development. Curr Drug Deliv. 2008;5(4):299–302.
Li J, et al. Modified curcumin with hyaluronic acid: combination of pro-drug and nano-micelle strategy to address the curcumin challenge. Food Res Int. 2015;69:202–8.
Dey S, Sreenivasan K. Conjugation of curcumin onto alginate enhances aqueous solubility and stability of curcumin. Carbohydr Polym. 2014;99:499–507.
Sarika PR, et al. Gum arabic-curcumin conjugate micelles with enhanced loading for curcumin delivery to hepatocarcinoma cells. Carbohydr Polym. 2015;134:167–74.
Wang Z, et al. Tuning the architecture of polymeric conjugate to mediate intracellular delivery of pleiotropic curcumin. Eur J Pharm Biopharm. 2015;90:53–62.
Li M, et al. Acetal-linked polymeric prodrug micelles for enhanced curcumin delivery. Colloids Surf B Biointerfaces. 2016;140:11–8.
Yang R, et al. Biodegradable polymer-curcumin conjugate micelles enhance the loading and delivery of low-potency curcumin. Pharm Res. 2012;29(12):3512–25.
Waghela BN, et al. Curcumin conjugated with PLGA potentiates sustainability, anti-proliferative activity and apoptosis in human colon carcinoma cells. PLoS One. 2015;10(2):e0117526.
Cai Y, et al. Synthesis, characterization and anti-cancer activity of Pluronic F68–curcumin conjugate micelles. Drug Deliv 2015;1–9.
Fang XB, et al. pH-sensitive micelles based on acid-labile pluronic F68–curcumin conjugates for improved tumor intracellular drug delivery. Int J Pharm. 2016;502(1–2):28–37.
Grill AE, Koniar B, Panyam J. Co-delivery of natural metabolic inhibitors in a self-microemulsifying drug delivery system for improved oral bioavailability of curcumin. Drug Deliv Transl Res. 2014;4(4):344–52.
Ahmad MZ, et al. Progress in nanotechnology-based drug carrier in designing of curcumin nanomedicines for cancer therapy: current state-of-the-art. J Drug Target. 2016;24(4):273–93.
Rungphanichkul N, et al. Preparation of curcuminoid niosomes for enhancement of skin permeation. Pharmazie. 2011;66(8):570–5.
Khalil NM, et al. Pharmacokinetics of curcumin-loaded PLGA and PLGA–PEG blend nanoparticles after oral administration in rats. Colloids Surf B Biointerfaces. 2013;101:353–60.
Reid JM, et al. Mouse pharmacokinetics and metabolism of the curcumin analog, 4-piperidinone, 3,5-bis[(2-fluorophenyl)methylene]-acetate(3E,5E) (EF-24; NSC 716993). Cancer Chemother Pharmacol. 2014;73(6):1137–46.
Alok V, et al. Perspectives on new synthetic curcumin analogs and their potential anticancer properties. Curr Pharm Des. 2013;19(11):2047–69.
Zhou L and Wang J. Physico-chemical characterization in drug discovery. Trends in bio/pharmaceutical industry. Preclinical formulation. 2009;12–18
Wichitnithad W, et al. Effects of different carboxylic ester spacers on chemical stability, release characteristics, and anticancer activity of mono-PEGylated curcumin conjugates. J Pharm Sci. 2011;100(12):5206–18.
Manju S, Sreenivasan K. Synthesis and characterization of a cytotoxic cationic polyvinylpyrrolidone–curcumin conjugate. J Pharm Sci. 2011;100(2):504–11.
Li AP. Screening for human ADME/Tox drug properties in drug discovery. Drug Discov Today. 2001;6(7):357–66.
van Breemen RB, Li Y. Caco-2 cell permeability assays to measure drug absorption. Expert Opin Drug Metab Toxicol. 2005;1(2):175–85.
Liederer BM, Borchardt RT. Enzymes involved in the bioconversion of ester-based prodrugs. J Pharm Sci. 2006;95(6):1177–95.
Yang YH, et al. Enzyme-mediated hydrolytic activation of prodrugs. Acta Pharm Sin B. 2011;1(3):143–59.
Fukami T, Yokoi T. The emerging role of human esterases. Drug Metab Pharmacokinet. 2012;27(5):466–77.
Bahar FG, et al. Species difference of esterase expression and hydrolase activity in plasma. J Pharm Sci. 2012;101(10):3979–88.
Li W, Zhang J, Tse FLS. Strategies in quantitative LC-MS/MS analysis of unstable small molecules in biological matrices. Biomed Chromatogr. 2011;25(1–2):258–77.
Li W, et al. LC-MS bioanalysis of ester prodrugs and other esterase labile molecules. In: Li W, Zhang J and Tse FLS (eds.) Handbook of LC-MS Bioanalysis. Wiley; 2013. pp. 429–445.
Zeng J, et al. Simultaneous determination of a selective adenosine 2A agonist, BMS-068645, and its acid metabolite in human plasma by liquid chromatography-tandem mass spectrometry—evaluation of the esterase inhibitor, diisopropyl fluorophosphate, in the stabilization of a labile ester-containing drug. J Chromatogr B Analyt Technol Biomed Life Sci. 2007;852(1–2):77–84.
Fung EN, et al. Effective screening approach to select esterase inhibitors used for stabilizing ester-containing prodrugs analyzed by LC–MS/MS. Bioanalysis. 2010;2(4):733–43.
Ratnatilaka Na Bhuket P, et al. Simultaneous determination of curcumin diethyl disuccinate and its active metabolite curcumin in rat plasma by LC–MS/MS: application of esterase inhibitors in the stabilization of an ester-containing prodrug. J Chromatogr B Analyt Technol Biomed Life Sci. 2016;1033–1034:301–10.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this manuscript was supported by the Annual Research Fund of the Faculty of Pharmaceutical Sciences, Chulalongkorn University (P. Rojsitthisak), the Ratchadapiseksompoch Endowment Fund of Chulalongkorn University (CU-58-003-HR and CU-59-031-AM) (P. Rojsitthisak), the National Research University Project, Office of Higher Education Commission (NRU59-047-AM) (P. Rojsitthisak) and the scholarship from the Graduate School, Chulalongkorn University to commemorate the 72nd anniversary of his Majesty King Bhumibala Aduladeja (P. Ratnatilaka Na Bhuket).
Conflicts of interest
Pahweenvaj Ratnatilaka Na Bhuket, Asma El-Magboub, Ian S. Haworth and Pornchai Rojsitthisak declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ratnatilaka Na Bhuket, P., El-Magboub, A., Haworth, I.S. et al. Enhancement of Curcumin Bioavailability Via the Prodrug Approach: Challenges and Prospects. Eur J Drug Metab Pharmacokinet 42, 341–353 (2017). https://doi.org/10.1007/s13318-016-0377-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13318-016-0377-7