Abstract
Purpose
Low-dose metronomic (LDM) chemotherapy represents a new strategy to treat solid tumors by stronger antiangiogenic activity and less side effects. The aim of the study is to rationally develop a docetaxel metronomic regimen in preclinical settings of gastric cancer.
Methods
In vitro cell proliferation, apoptosis, and thrombospondin-1/vascular endothelial growth factor (TSP-1/VEGF) expression analyses were performed on human umbilical vein endothelial cells (HUVECs) and gastric cancer (BGC-823) cells exposed for 144 h to metronomic concentrations of docetaxel. BGC-823 human gastric cancer xenograft model was used, and tumor growth and side effects were closely monitored. Quantitative real-time PCR was used to determine TSP-1/VEGF mRNA levels in tumor samples. Expression of VEGF and CD31 was observed by immunohistochemistry.
Results
Our results indicated that LDM docetaxel preferentially inhibited HUVEC cell proliferation and induced HUVEC apoptosis. Docetaxel significantly increased TSP-1 expression and secretion in HUVEC cells whereas the expression and secretion of VEGF significantly decreased in BGC-823 cells. LDM docetaxel significantly inhibited BGC-823 tumor growth in the absence of toxicity, which was accompanied by decreases in microvessel density (MVD) and VEGF and increases in TSP-1 gene expression in tumor tissues.
Conclusions
In vitro results show the antiangiogenic properties of LDM docetaxel. In vivo, LDM docetaxel treatment is effective against gastric tumor and microvessel growth without toxic effect on nude mice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite the progress in cancer therapeutics and chemotherapy development with the introduction of new drugs, advanced gastric cancer continues to have an extremely poor prognosis and with limited treatment options [1]. Thus, new therapeutic strategies are urgently needed. Antiangiogenic therapy is one of the most promising novel strategies, and many attempts have been made to prevent or delay tumor growth by anti-angiogenesis.
Recently, there has been considerable interest in the notion of exploiting chemotherapeutic drugs as angiogenesis inhibitors. Maximum tolerated dose (MTD) chemotherapy targeting the tumor cells directly sometimes causes undesirable side effects normally associated with traditional cytotoxic chemotherapy regimens; during the break periods between successive cycles of MTD chemotherapy, the bone marrow recovery sometimes occurs [2]. Any potential damage to the tumor vasculature can be repaired during the long breaks. Continuous, low-dose metronomic (LDM) chemotherapy, administered at close regular intervals with no prolonged breaks, inhibits angiogenesis by targeting the endothelial cells directly and is thought to have fewer side effects as well as a lack of drug resistance [3]. Metronomic chemotherapy is changing the paradigm that more is better. Angiogenesis stimulators such as vascular endothelial growth factor (VEGF) and angiogenesis inhibitors such as thrombospondin-1 (TSP-1) could be key mediators for metronomic chemotherapy activity [4].
Docetaxel is a mitotic spindle poison that induces a mitotic block and exhibits promising activity in gastric cancer [5]. Chemotherapeutic drugs, and docetaxel in particular, chronically administered using a frequent schedule at low dose (metronomic dosing), can cause potent antiangiogenic effects by targeting the endothelial cells of newly growing blood vessels [6].
On the basis of this background, we decided to test, for the first time, the hypothesis that LDM docetaxel can be effective in preclinical settings of gastric cancer treatment; specifically, we investigated the in vitro and in vivo antiangiogenic/antitumor activity and the modulation of TSP-1 and VEGF factor expression/secretion using low-dose schedules. Moreover, we compare the antitumor and antiangiogenic effects of LDM docetaxel with the MTD docetaxel and determine the feasibility of LDM docetaxel therapy for the treatment of gastric cancer.
Materials and methods
Drug, cell lines, and culture
Docetaxel was supplied by Jiangsu Hengrui Medicine Company (China), and it was dissolved in ethanol/water at a stock concentration of 10 mM and stored in aliquots at −20°C. Human umbilical vein endothelial cells (HUVECs) were obtained from the Typical Animal Reserve Center of China. Human gastric cancer cell line BGC-823 was obtained from Cancer Research Institution of China Medical University (China). HUVECs and human BGC-823 gastric cancer cells were cultured in Dulbecco’s modified Eagle’s medium (RPMI 1640) supplemented with 10% fetal bovine serum (FBS) and incubated in 5% CO2 at 37°C.
Cell proliferation assay
In vitro chemosensitivity testing was performed on single-cell suspensions of HUVEC and BGC-823 cells plated in 96-well plastic plates (1% gelatin coated for the endothelial cells) and allowed to attach overnight. Each drug concentration was represented by at least 5 wells. Then, 1 × 103 HUVEC cells/well were treated for 144 h in 200 μl of medium with docetaxel at final concentrations (0.00001–100 nM); 0.5 × 103 BGC-823 cells/well were treated for 144 h in 200 μl of medium with docetaxel at final concentrations (0.01–100 nM) [7]. To maintain a constant concentration of the drug during the protracted 144 h period of the experiments, every 24 h the medium was removed and fresh solutions were added with new medium. After that, the absorption was detected by adding 20 μl tetrazolium (MTT) to each well, incubating for 4 h, sucking out the media, adding 150 μl dimethyl sulfoxide (DMSO) to dissolve the violet-crystal and measuring at a wavelength of 490 nm (A490). The absorbance values were normalized by assigning the value of the control line in the medium without drug to 1.0 and the value of the no cell control to 0. Experiments were performed in triplicate. The half inhibitory concentration (IC50) was defined as the compound or drug concentration required decreasing the A490 to 50% of the control value.
Cell apoptosis assay
To quantify the degree of apoptosis induced by the drug treatments, HUVEC and BGC-823 cells were continuously treated for 144 h with docetaxel at a concentration corresponding to the experimental IC50 of cell proliferation (0.06 and 1.1 nM, respectively) and with vehicle alone. At the end of the incubation, cells quantification of apoptosis cells was performed using an Annexin-V-FITC Apoptosis Detection Kit (Invitrogen, Carlsbad, CA, USA) according to the manufacturer’s instructions. The cells were collected and resuspended in 500 μl of binding buffer, and 5 μl of Annexin-V-fluorescein isothiocyanate (FITC) and 5 μl of propidium iodide (PI) were added. Analyses were performed with a flow cytometer (FACScalibur, Becton–Dickinson, Franklin Lakes, NJ, USA).
Real-time PCR analysis of human VEGF and TSP-1 gene expression on tumor and endothelial cells
To evaluate the expression of the human VEGF and TSP-1 genes, 2 × 104 HUVEC and BGC-823 cells were grown in their respective media and treated with docetaxel at a concentration corresponding to the experimental IC50 of cell proliferation (0.06 and 1.1 nM, respectively), and with vehicle alone for 144 h. At the end of the incubation, the cells were collected and total RNA was extracted by Trizol method (Invitrogen, USA). RNA was reverse transcribed with oligo (dT) primers, and mRNA expression was analyzed by quantitative real-time reverse transcription polymerase chain reaction (PCR) by using the following primers: VEGF sense 5′-GAGCCTTGCCTTGCTGCTCTAC and antisense 5′-CACCAGGGTCTCGATTGGATG; TSP-1 sense 5′-GTTGCATGTGTGTGGAAGCAAC and antisense 5′-ACCACACTGAAGATCTGGCCAG. The relative expression of each gene was assessed in comparison with the housekeeping gene β-actin amplified with the following primers: sense 5′-TGGCACCCAGCACAATGAA and antisense 5′-CTAAGTCATAGTCCGCCTAGAAGCA. cDNAs were amplified for 45 cycles with a PCR Thermal Cycler (Takara, Japan) containing the intercalating agent SYBR Green (Takara Bio, Japan) in a two-step amplification scheme (95°C, 5 s and 60°C, 30 s). Amplifications were normalized to β-actin, and the quantitation of gene expression was performed using the △△Ct calculation, where Ct is the threshold cycle; the amount of target, normalized to the endogenous control and relative to the calibrator (vehicle-treated control tumors), is given as 2−△△Ct.
Human VEGF and TSP-1 detection in conditioned media by ELISA and EIA
Human HUVEC and BGC-823 cells were grown in their respective media and treated with docetaxel at a concentration corresponding to the experimental IC50 of cell proliferation (0.06 and 1.1 nM, respectively), and with vehicle alone for 144 h. To measure the secreted VEGF and TSP-1, at the end of the experiment the medium of each well was collected and assessed for human VEGF and TSP-1 levels by the ELISA Kit VEGF Quantikine (R&D Systems, USA) and by the ChemiKine Human TSP-1 EIA Kit (Chemicon, USA), respectively, and normalized by total protein concentration. The optical density was determined using the microplate reader Multiskan Spectrum (Thermo Labsystems, Italy) set to 450 nm (with a wavelength correction set to 540 nm) for the VEGF kit and to 490 nm for the TSP-1 kit. All experiments were repeated, independently, three times with at least five samples for each concentration.
Animals and schedule
A group of female BALB/c nude mice (5–6 week age) were purchased from the Animal Experiment Center of Beijing (China). Mice were housed under pathogen-free conditions and fed with animal chow and water ad libitum. All the animal experiments were approved by the Institutional Animal Care and Use Committee of China Medical University. After a 2-week quarantine, BGC-823 Cells (2 × 106) were suspended in 0.2 ml of culture medium without FBS and injected into the right flank of each BALB/c nude mice. Approximately 2 weeks later (average tumor size, 100 mm3), the mice were randomized into three groups (each group had 10 mice) as follows: control [intraperitoneal (i.p.) injection of 0.2 ml physiological saline daily]; MTD (i.p. injection of 15 mg/kg docetaxel once every 2 weeks); LDM (i.p. injection of 0.5 mg/kg docetaxel 3 times a week). The experimental period ended 65 days after the inoculation of tumor cells whereas control mice were killed by an anaesthetic overdose when the tumor volume reached a mean value of 2,000 mm3.
Tumor growth, side effects, and quality of life of mice
The mice were closely monitored, and body weight and tumor size recorded twice a week. Tumor volume (TV) was estimated using the formula: TV (mm3) = (width2 × length)/2. Blood samples were collected through orbital sinus once a week to count white blood cells (WBC). During the experiment period, side effects such as weight loss, change in behavior and feeding, reaction to stimulation, ruffling of fur, and psychosis (distress) were observed.
Real-time PCR analysis and immunohistochemical detection of VEGF and CD31 on BGC-823 tumor tissue samples
After surgical resection, tumor tissue samples from all the different treatment groups were split into two aliquots: one immediately frozen in liquid nitrogen for the analysis of human VEGF and TSP-1 gene expression by real-time PCR as described above; the other fixed immediately in 10% buffered formalin phosphate for 12–24 h and embedded in paraffin for immunohistochemistry.
Five-micrometre sections were cut for immunohistochemistry using the PV-9000 kit (Beijing Zhongshan Goldenbridge Biotechnology Company, Beijing, China). Rabbit anti-human monoclonal antibody for VEGF (dilution, 1:50) was purchased from Fuzhou Maixin Company (China). Rat anti-mouse monoclonal antibody for CD31 (dilution, 1:100) was purchased from Dako (Japan). Antigens were retrieved after they were placed in a pressure cooker at a full pressure for 160 s in citrate buffer (pH 6.0). All procedures were implemented according to their manufacturer’s instructions, respectively. For negative controls, sections were processed as above but treated with 0.01 mol/l phosphate-buffered saline (PBS) instead of primary antibodies.
Cytoplasmic staining was scored positive for VEGF. The degree of positivity was evaluated by calculating the percentage of immunoreactive cells on a minimum of 500 cells [7].
Microvessel density (MVD) was assessed by immunohistochemical analysis with antibodies to the endothelial marker CD31 and determined according to the method of Liu TG and colleagues [8]. Briefly, the immunostained sections were initially screened at low magnifications (40× and 100×) to identify hot spots, which are the areas of highest neovascularization. Any yellow brown-stained endothelial cell or endothelial cell cluster that was clearly separate from adjacent microvessels, tumor cells, and other connective tissue elements was considered a single, countable microvessel. Within the hot spot area, the stained microvessels were counted in a single high-power (200×) field, and the average vessel count in 3 hot spots was considered the value of MVD. All counts were performed by three investigators in a blinded manner. Microvessel counts were compared between the observers, and discrepant results were reassessed. The consensus was used as the final score for analysis.
Statistical analysis
Results are reported as mean values ± standard error. The analysis by ANOVA, followed by the Student–Newman–Keuls test, was used to assess the statistical differences of data in vitro and in vivo. All statistical analyses were performed by using SPSS 17.0 software package. P values lower than 0.05 were considered significant.
Results
LDM treatment with docetaxel preferentially inhibits endothelial cell proliferation
The 144-h docetaxel exposure inhibited the cell growth of HUVEC in a concentration-dependent manner, and the calculated IC50 value was 0.06 ± 0.005 nM (Fig. 1a); in contrast, docetaxel did not significantly affect the proliferation of BGC-823 cell line at low concentrations, showing much higher IC50 value (1.1 ± 0.024 nM; Fig. 1b).
Effect of continuous docetaxel on HUVEC (a) and BGC-823 (b) cells growth. The inhibitory effects of the drug were studied using prolonged continuous exposures (144 h) on the HUVEC and BGC-823 cell lines. The cell proliferation was assayed using MTT colorimetric assay (n = 5 wells for each concentration at least and experiments were performed in triplicate). An IC50 value was calculated using the dose–response curve to assessment of efficiency of growth inhibition
LDM treatment with docetaxel preferentially induces endothelial cell apoptosis
As shown in Fig. 2, after 144 h of treatment at their docetaxel IC50s, a significant percentage of apoptotic HUVEC cells (early apoptosis plus late apoptosis) in the treated sample was found (17.12 + 11.14)% when compared to the control (2.56 + 4.42)%. This apoptotic percentage was similar to that obtained and expected, when treating cancer cells at higher doses such as their IC50s (Fig. 2).
Docetaxel treatment increase chemotherapeutic agent-induced apoptosis in HUVEC (a, b) and BGC-823 (c, d) cells. a, c cells were treated without drug. b docetaxel on proliferating HUVEC cells treated at their experimental IC50s (lower concentrations) for 144 h. d docetaxel on proliferating BGC-823 cancer cells treated at their experimental IC50s (higher concentrations) for 144 h. Early apoptotic cells were defined as Annexin-V-positive, PI-negative cells, and late apoptotic cells were defined as Annexin-V-positive, PI-positive cells. Experiments were repeated three times (n = 5 samples for each concentration at least)
LDM treatment with docetaxel modulates expression and secretion of TSP-1 and VEGF in endothelial and cancer cells
Docetaxel significantly increased TSP-1 expression in HUVEC cells tested at their IC50s (1.72 ± 0.11 vs. 1.0 of control expression; P < 0.05; Fig. 3a). In contrast, TSP-1 expression in BGC-823 cancer cells was decreased at IC50 docetaxel concentration when compared to controls (Fig. 3b). Moreover, docetaxel exposure positively modulated TSP-1 protein secretion (normalized for total protein) in HUVEC cells tested (Fig. 3a), confirming the data obtained at the mRNA level. In particular, TSP-1 secretion was significantly increased up to 810 ± 76% in HUVEC cells versus 100% of controls, at the IC50 docetaxel concentrations (Fig. 3a). Interestingly, results obtained with cancer cell cultures revealed that at docetaxel concentrations corresponding to their IC50s exposure, secreted TSP-1 was unchanged in BGC-823 cells (Fig. 3b).
TSP-1 gene expression and secretion in HUVEC (a) and BGC-823 (b) cells exposed to docetaxel at a concentration corresponding to the experimental IC50 of cell proliferation and with vehicle alone for 144 h. VEGF expression and secretion in HUVEC (c) and BGC-823 (d) cells exposed to the above mentioned docetaxel concentrations. All experiments were repeated three times (n = 5 samples for each concentration at least). *P < 0.05 versus vehicle-treated controls
The results of VEGF gene expression and protein secretion analysis showed a differential response among HUVEC cells and BGC-823 cells after 144 h docetaxel treatments. Docetaxel, at its IC50 levels, significantly increased VEGF expression in HUVECs (1.42 ± 0.08 vs. 1.0 of control expression; Fig. 3c) whereas there was a significant decrease in VEGF mRNA in BGC-823 cells (0.61 ± 0.04 vs. 1.0 of control expression; Fig. 3d). Although very low secreted level of VEGF was measured (normalized for total protein), significant increment was observed at a docetaxel concentration corresponding to IC50 level in HUVEC cells (362 ± 17.8 vs. 100% of control; Fig. 3c). On the contrary, VEGF secretion significantly decreased in BGC-823 cells (Fig. 3d) at their IC50 concentrations.
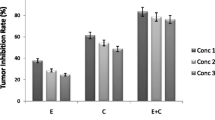
Tumor growth assessment
As shown in Fig. 4, the tumors in the control group grew rapidly, reaching 2,000 mm3 in volume 42 days after implantation; thus, all the mice in this group were killed according to the preestablished criteria. In contrast, in the MTD and LDM groups, the tumors had reached only 1,284 ± 172 mm3 and 928 ± 111 mm3 42 days after implantation, respectively, being significantly smaller than the control tumors (both P < 0.05). Interestingly, when LDM docetaxel was administered continuously, tumor growth was delayed, compared to the MTD group, when assessed after 3 weeks of treatment (P < 0.05; Fig. 4).
Tumor growth curve of each group (n = 10 mice per group). Tumor growth was inhibited in mice receiving conventional MTD docetaxel at the prophase, after which tumors grew fast while on therapy. For mice receiving continuous LDM docetaxel, tumor growth was delayed for a long period of time. *P < 0.05 versus vehicle-treated controls; **P < 0.05 versus MTD group
Toxicity evaluation
Mice treated with the conventional MTD regimen appeared to be reluctant to move, and their skin was flabby and lackluster; over 85% of them lost 10% of their body weight, and a marked reduction of WBC counts was observed in mice of the MTD group. The continuous LDM docetaxel regimen was not associated with weight loss, leucopenia, or other signs of toxicity.
Real-time PCR analysis on BGC-823 tumor tissue samples
Figure 5 showed the modulation of human TSP-1 and VEGF gene expression in treated tumors compared with vehicle-treated control tumors. A significant increase in TSP-1 expression was found in the metronomic docetaxel treated tumors (1.68 ± 0.05 vs. 1.0 of control expression; P < 0.05) whereas no significant changes were demonstrated at the MTD dose (Fig. 5). The VEGF expression in the LDM docetaxel treated group was lower than that in the control group (P < 0.05), whereas the VEGF expression in the MTD group also was lower than that in the control group, however, without significant difference (P > 0.05).
Histopathologic analysis on BGC-823 tumor tissue samples
Measurement of angiogenic indices showed some differences among the various groups (Fig. 6g). Tumors derived from mice in the control group (Fig. 6a) showed the highest microvessel counts. Those from mice subjected to MTD group (Fig. 6b) had intermediate values, whereas the lowest counts were measured in tumors from mice that received LDM chemotherapy (Fig. 6c). There was positive expression of VEGF in the cytoplasm of some tumor cells. Compared with the MTD group (Fig. 6e), VEGF expression was lower in the continuous LDM docetaxel group (Fig. 6f) (P < 0.05; Fig. 6g). The results indicated that metronomic docetaxel chemotherapy inhibited tumor angiogenesis.
Immunohistochemistry of mouse CD31 and human VEGF in BGC-823 xenografts (n = 5 slides per group at least). (a–c) Illustrated are immunohistochemical staining of CD31 (×200). a control group; b MTD group; c LDM group. (d–f) Illustrated are immunohistochemical staining of VEGF (×200). d control group; e MTD group; f LDM group. g quantification of MVD and VEGF positivity in BGC-823 tumor xenografts. *P < 0.05 versus vehicle-treated controls; **P < 0.05 versus MTD group
Discussion
Our translational study, for the first time, rationally demonstrated that LDM docetaxel is effective in preclinical settings of gastric cancer (in vitro and in vivo), as an antiangiogenic and antitumor schedule, modulating both TSP-1 and VEGF gene expression and secretion.
The evolution toward metronomic administration of chemotherapeutic drugs is based on several factors: (1) high-dose chemotherapy is not very effective and is associated with high toxicity; (2) metronomic chemotherapy may significantly delay the onset of mutation-dependent mechanisms of acquired drug resistance; (3) metronomic chemotherapy, in which the cumulative dose is significantly less than MTD-based chemotherapy, has several potential advantages, including lower toxicity and adverse side effects; (4) more importantly, it seems that despite the lower cumulative doses administered, metronomic chemotherapy is superior to MTD-based regimens for inhibiting tumor growth in preclinical models and clinical trials [6, 9, 10].
Our results are highly suggestive of the presence of the so-called ‘antiangiogenic window’ [11] when protracted exposure to low concentrations of docetaxel was used. Indeed, there was a clear trend showing the effectiveness of docetaxel picomolar concentrations against endothelial cells, but not against tumor cells. This was the case not only for the inhibition of proliferation but also for the induction of apoptosis. These findings may be explained by the changes of TSP-1 and VEGF expression and secretion. TSP-1, a component of the extracellular matrix that can also be secreted and found in the circulation, is a well known endogenous inhibitor of angiogenesis [12]. It seems to act primarily by binding to CD36 receptors, which are expressed by endothelial cells [13]. This interaction blocks proliferation and induces apoptosis in endothelial cells [14, 15], but would not be expected to occur in CD36-negative cells, such as most bone-marrow-derived haematopoietic stem cells or hair-follicle cells. In vitro docetaxel protracted treatment induced a significant increase in TSP-1 expression and secretion in HUVEC cells at effective concentrations (IC50). Up-regulating the endogenous angiogenesis inhibitor TSP-1 has been previously described as a mediator of the specific antiangiogenic effects of this kind of therapy [16–18], and our results implicate this endogenous angiogenesis inhibitor as a major mediator of the low-concentration docetaxel anti-endothelial in vitro effects we studied. In the present research, docetaxel, at its IC50 levels, did not induce TSP-1 expression and secretion in BGC-823 cancer cells and the cellular mechanism for this still awaits elucidation.
Angiogenesis is tightly regulated by pro-angiogenic and anti-endothelial growth factors. VEGF is one of the most essential pro-angiogenic growth factors [19], and it also appears to be critical in the angiogenic process [20]. TSP-1 can also bind and sequester VEGF and therefore block its pro-angiogenic activity [10]. In our work, however, we could not show decrease in VEGF mRNA and VEGF secretion at a docetaxel concentration corresponding to IC50 level in HUVEC cells. In this regard, Bocci G et al. [7] have reported that VEGF levels increased in HUVEC cells responded to metronomic therapy. However, the exact mechanisms need further study. In the present study, docetaxel protracted treatment significantly caused a strong inhibition of VEGF expression and secretion in cancer cells. In this regard, Benelli et al. [6] have showed that 1-week exposure to 10 and 100 pM docetaxel significantly inhibited VEGF production. Moreover, Colleoni et al. [21–23] have reported that serum VEGF levels declined in patients who responded to metronomic therapy.
To proceed with the development of LDM docetaxel, the second step was to establish the antitumor and antiangiogenic activity of this schedule in vivo. On the basis of our in vitro IC50 data and on data from previously published studies [9], we decided to treat animals with above MTD and LDM regimens. Our findings show that LDM docetaxel had significant effects on therapeutic response. One of the major factors that account for the limited advances made in cancer treatment is acquired drug resistance. Metronomic chemotherapy is less likely to acquire resistance compared with conventional chemotherapy, since the target of the therapy is presumed to be the genetically stable and activated endothelial cell rather than the genetically unstable cancer cell [24]. In the present study, tumor growth was delayed at the prophase in mice receiving MTD docetaxel, after which the tumors began to grow progressively while on therapy, which could be easily explained by drug resistance. But when LDM docetaxel was administered, the regimen produced a long period of growth delay in tumor mass. Moreover, we did not observe toxic effects at the doses administered in the LDM group, as evidenced by body weight and WBC counts, which remained similar to those of control mice during the treatment period.
In the in vivo studies, MTD docetaxel did not significantly change the expression levels of TSP-1/VEGF mRNA. Instead, LDM docetaxel caused a marked increase in TSP-1 mRNA in tumor xenografts whereas the VEGF mRNA expression in the LDM group decreased significantly. These results exhibited strong antiangiogenic activity of LDM schedule.
MVD is accepted as a standard indicator of angiogenesis [25], and VEGF expression is strictly correlated with MVD [26]. In the present study, MVD in tumor xenografts was markedly decreased in metronomic schedules when compared to control group and also to the MTD regimen, which were in agreement with the findings of Ji et al. [27–29]. VEGF protein expression in tumors was similar to that of MVD. Our data indicated that LDM chemotherapy exhibited the inhibitory effects of angiogenesis by decreasing MVD value and VEGF expression.
In summary, the results presented here have shown an effective and safer strategy by using LDM docetaxel chemotherapy compared with MTD docetaxel therapy in respect of tumor growth and side effects, in a nude mouse model of BGC-823 gastric cancers. These effects seem to be mediated in part by antivascular, antiproliferative, and apoptotic of the LDM regimen. Both assessment of expression levels of TSP-1 and VEGF hold promise as biomarkers of the antiangiogenic activity and therapeutic response. Our data suggest that LDM docetaxel is highly efficacious and should be considered for clinical trials and further preclinical studies.
References
Albert A (2008) New drugs in the treatment of gastric tumors. Clin Transl Oncol 10:256–261
Ooyama A, Oka T, Zhao HY, Yamamoto M, Akiyama S, Fukushima M (2008) Anti-angiogenic effect of 5-Fluorouracil-based drugs against human colon cancer xenografts. Cancer Lett 267:26–36
Orlando L, Cardillo A, Rocca A et al (2006) Prolonged clinical benefit with metronomic chemotherapy in patients with metastatic breast cancer. Anticancer Drugs 17:961–967
Scharovsky OG, Mainetti LE, Rozados VR (2009) Metronomic chemotherapy is changing the paradigm that more is better. Curr Oncol 16:7–15
Tetzlaff ED, Cheng JD, Ajani JA (2008) Review of docetaxel in the treatment of gastric cancer. Ther Clin Risk Manag 4:999–1007
Benelli R, Monteghirfo S, Balbi C et al (2009) Novel antivascular efficacy of metronomic docetaxel therapy in prostate cancer: hnRNP K as a player. Int J Cancer 124:2989–2996
Bocci G, Falcone A, Fioravanti A et al (2008) Antiangiogenic and anticolorectal cancer effects of metronomic irinotecan chemotherapy alone and in combination with semaxinib. Br J Cancer 98:1619–1629
Liu TG, Huang Y, Cui D et al (2009) Inhibitory effect of ginsenoside Rg3 combined with gemcitabine on angiogenesis and growth of lung cancer in mice statistical analysis. BMC Cancer 9:250
Kamat AA, Kim TJ, Landen CN et al (2007) Metronomic chemotherapy enhances the efficacy of antivascular therapy in ovarian cancer. Cancer Res 67:281–288
Kerbel RS, Kamen BA (2004) The anti-angiogenic basis of metronomic chemotherapy. Nat Rev Cancer 4:423–436
Bocci G, Nicolaou KC, Kerbel RS (2002) Protracted low-dose effects on human endothelial cell proliferation and survival in vitro reveal a selective antiangiogenic window for various chemotherapeutic drugs. Cancer Res 62:6938–6943
Lawler J (2002) Thrombospondin-1 as an endogenous inhibitor of angiogenesis and tumor growth. J Cell Mol Med 6:1–12
Dawson DW, Pearce SF, Zhong R, Silverstein RL, Frazier WA, Bouck NP (1997) CD36 mediates the In vitro inhibitory effects of thrombospondin-1 on endothelial cells. J Cell Biol 138:707–717
Guo N, Krutzsch HC, Inman JK, Roberts DD (1997) Thrombospondin 1 and type I repeat peptides of thrombospondin 1 specifically induce apoptosis of endothelial cells. Cancer Res 57:1735–1742
Jiménez B, Volpert OV, Crawford SE, Febbraio M, Silverstein RL, Bouck N (2000) Signals leading to apoptosis-dependent inhibition of neovascularization by thrombospondin-1. Nat Med 6:41–48
Damber JE, Vallbo C, Albertsson P, Lennernas B, Norrby K (2006) The antitumour effect of low-dose continuous chemotherapy may partly be mediated by thrombospondin. Cancer Chemother Pharmacol 58:354–360
Laquente B, Lacasa C, Ginestà MM, Casanovas O, Figueras A, Galán M, Ribas IG, Germà JR, Capellà G, Viñals F (2008) Antiangiogenic effect of gemcitabine following metronomic administration in a pancreas cancer model. Mol Cancer Ther 7:638–647
Bocci G, Francia G, Man S, Lawler J, Kerbel RS (2003) Thrombospondin 1, a mediator of the antiangiogenic effects of low-dose metronomic chemotherapy. Proc Natl Acad Sci USA 100:12917–12922
Bando H (2007) Vascular endothelial growth factor and bevacitumab in breast cancer. Breast Cancer 14:163–173
Hayes DF, Miller K, Sledge G (2007) Angiogenesis as targeted breast cancer therapy. Breast 16(Suppl 2):S17–S19
Colleoni M, Rocca A, Sandri MT et al (2002) Low-dose oral methotrexate and cyclophosphamide in metastatic breast cancer: antitumor activity and correlation with vascular endothelial growth factor levels. Ann Oncol 13:73–80
Colleoni M, Orlando L, Sanna G et al (2006) Metronomic low-dose oral cyclophosphamide and methotrexate plus or minus thalidomide in metastatic breast cancer: antitumor activity and biological effects. Ann Oncol 17:232–238
Correale P, Cerretani D, Remondo C et al (2006) A novel metronomic chemotherapy regimen of weekly platinum and daily oral etoposide in high-risk non-small cell lung cancer patients. Oncol Rep 16:133–140
Bocci G, Nicolaou KC, Kerbel R (2002) Protracted low-dose effects on human endothelial cell proliferation and survival in vitro reveal a selective antiangiogenic window for various chemotherapeutic drugs. Cancer Res 62:6938–6943
Magnon C, Galaup A, Rouffiac V et al (2007) Dynamic assessment of antiangiogenic therapy by monitoring both tumoral vascularization and tissue degeneration. Gene Ther 14:108–117
Maria RR, Francesca C, Francesca G (2005) Microdensity vessels and with vascular endothelial growth factor expression in ovarian carcinoma. Int J Surg Pathol 13:135–142
Ji Y, Hayashi K, Amoh Y et al (2007) The camptothecin derivative CPT-11 inhibits angiogenesis in a dual-color imageable orthotopic metastatic nude mouse model of human colon cancer. Anticancer Res 27:713–718
Zhang Q, Kang X, Zhao W (2006) Antiangiogenic effect of low-dose cyclophosphamide combined with ginsenoside Rg3 on Lewis lung carcinoma. Biochem Biophys Res Commun 342:824–828
Zhang M, Tao W, Pan S et al (2009) Low-dose metronomic chemotherapy of paclitaxel synergizes with cetuximab to suppress human colon cancer xenografts. Anticancer Drugs 20:355–363
Acknowledgments
The study was supported by the National Natural Science Foundation of China (No. 30973503 and No. 81071650), Special foundation for Climbing Scholars of Universities in Liaoning Province (2009–2011) and Research Fund for the Doctoral Program of Higher Education (20092104110008).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wu, H., Xin, Y., Zhao, J. et al. Metronomic docetaxel chemotherapy inhibits angiogenesis and tumor growth in a gastric cancer model. Cancer Chemother Pharmacol 68, 879–887 (2011). https://doi.org/10.1007/s00280-011-1563-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-011-1563-6