Abstract
Purpose
To evaluate the efficacy and safety of S-1 in combination with oxaliplatin in a biweekly schedule as first-line treatment in metastatic colorectal cancer and the association between genetic polymorphisms and treatment outcomes.
Methods
Eligibility included age 18–75 years, at least one measurable lesion, no prior chemotherapy except adjuvant chemotherapy, and Eastern Cooperative Oncology Group Performance Status (PS) 0–2. S-1 40 mg/m2 b.i.d. on days 1–7 with 85 mg/m2 of oxaliplatin on day 1 was repeated every 2 weeks. Genomic DNA from whole blood was analyzed for 15 single-nucleotide polymorphisms (SNPs) among 8 genes.
Results
Fifty-two patients (median age 63 years, range 37–74) were enrolled: 37 men and 15 women; 44 with a PS of 0 and 8 with a PS of 1; and 41 with initially metastatic cancer and 11 with relapsed disease. Among 51 evaluable patients, objective response rate was 47.1% [95% confidence interval (CI) 32.9–61.2]. Median follow-up duration was 17.1 months (range 3.9–28.2 months). Median progression-free survival (PFS) was 6.4 months (95% CI 4.8–8.1), and median overall survival had not been reached yet. Reported grade 3 toxicities were neutropenia (7.7%), thrombocytopenia (5.8%), sensory neuropathy (7.7%) and diarrhea (1.9%). There was no grade 4 toxicity or neutropenic fever. Patients with A/G or G/G genotype in GSTP1 Ile105Val SNP had longer PFS than patients with A/A (median 8.3 vs. 6.1 months, P = 0.04).
Conclusions
Biweekly S-1 with oxaliplatin is effective and has improved tolerability and convenience compared to other fluoropyrimidine with oxaliplatin combinations. GSTP1 Ile105Val SNP is associated with treatment outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is one of the most common malignancies and the fourth leading cause of cancer-related death in Korea [1]. The backbone of chemotherapy in metastatic CRC is fluoropyrimidine. Concentration and duration of exposure are important determinants of the efficacy of 5-fluorouracil (5-FU). The half-life of intravenous (IV) 5-FU in plasma is very short, and potentially cytotoxic concentrations are only maintained for approximately 2 h after bolus administration; continuous infusion (CI) of 5-FU allows sustained plasma exposure [2]. A meta-analysis of 1,219 patients with CRC from six randomized trials revealed a higher response rate (RR) from continuously infused 5-FU compared to bolus administration, and there was a small, but statistically significant, advantage in median survival [3]. Oxaliplatin is a platinum compound with powerful antineoplastic properties, a synergistic effect with 5-FU, a satisfactory safety profile, and convenient administration. The combination of oxaliplatin with 5-FU or capecitabine is now regarded as standard chemotherapy in metastatic CRC [4, 5].
Oral fluoropyrimidine derivatives were invented to, like CI, augment the efficacy of fluoropyrimidine treatment by increasing the duration of exposure, while mitigating the inconveniences and side effects of 5-FU CI. Capecitabine is recognized as an oral alternative of 5-FU in metastatic CRC. In a phase III study comparing capecitabine plus oxaliplatin (XELOX) to the combination of oxaliplatin and leucovorin (LV) plus bolus and CI 5-FU (FOLFOX-4), the median progression-free survival (PFS) and median overall survival (OS) of XELOX were not inferior to those of FOLFOX-4 [6]. A pooled analysis of 6 phase II and III trials also concluded that XELOX was not inferior to FOLFOX-4 [4].
S-1, another oral fluoropyrimidine consists of tegafur, 5-chloro-2,4 dihydroxypyrimidine (CDHP), and potassium oxonate. CDHP induces strong inhibition of dihydropyrimidine dehydrogenase (DPD), and 5-FU converted from tegafur in the liver can maintain a steady-state concentration, allowing prolonged exposure within the human body, while potassium oxonate provides protection from diarrhea [7]. Introduction of S-1 instead of 5-FU in metastatic CRC is thus a rational and feasible treatment approach. In 3 previous phase II studies, the reported RRs of S-1 monotherapy in metastatic or advanced CRC ranged from 24 to 39.5%, with manageable toxicities [8–10].
Recent advances in the understanding of the genetic variations that influence drug metabolism, toxicity, and effectiveness are relevant in cancer chemotherapy [11]. Tailored chemotherapy, based on such genetic variations, has the potential to improve cancer treatment.
The objective of this study was to evaluate the efficacy and safety of S-1 in combination with oxaliplatin administered in a biweekly schedule as first-line chemotherapy in metastatic CRC and to examine the association between genetic polymorphisms and treatment outcomes by analyzing single-nucleotide polymorphisms (SNPs).
Patients and methods
Patients
Patients with biopsy-proven metastatic or recurrent CRC were enrolled in this prospective phase II study conducted in two medical centers [Seoul National University Hospital (SNUH) and Seoul Municipal Boramae Hospital (SMBH)]. Eligibility criteria included (1) age between 18 and 75 years; (2) at least one measurable lesion as defined by the Response Evaluation Criteria in Solid Tumors (RECIST) version 1.0 criteria [12]; (3) no previous chemotherapy or radiotherapy except adjuvant chemotherapy or radiotherapy completed more than 1 year previously; (4) an Eastern Cooperative Oncology Group (ECOG) performance status (PS) between 0 and 2; (5) adequate organ and marrow function. Patients with an uncontrolled comorbid illness, an active infection, or a second malignancy other than non-melanoma skin carcinoma or carcinoma in situ of the cervix were ineligible. The study was reviewed and approved by the Institutional Review Boards of SNUH and SMBH. Written informed consent was obtained from all patients prior to study entry.
Treatment and evaluation
Oxaliplatin 85 mg/m2 was administered as a 120-min IV infusion on day 1. Additionally, S-1 40 mg/m2 was orally administered twice daily (80 mg/m2/day) from day 1 through day 7. Treatment was repeated every 2 weeks, and a total of 12 cycles were administered, unless there was documented disease progression, unacceptable toxicity, or patient refusal. After the 12th cycle, additional chemotherapy was allowed based on the investigator’s clinical decision. Oxaliplatin was provided by Sanofi-Aventis Korea Co., Ltd. and S-1 by Jeil Pharmaceutical Co., Ltd. The companies had no influence on the design and conduct of this study.
Dose adjustments at the start of a new cycle were based on the worst toxicity observed during the previous cycle. For grade 3 neutropenia, a patient underwent a 20 mg/m2/day reduction of S-1 (e.g., from 80 to 60 mg/m2/day). For grade 4 neutropenia, 40 mg/m2/day of S-1 was administered with 75 mg/m2 of IV oxaliplatin. For grades 3 and 4 thrombocytopenia, 60 and 40 mg/m2/day of S-1 were administered, respectively, with 75 mg/m2 of IV oxaliplatin. The following toxicities also required a 20 mg/m2/day reduction of S-1, administered with 75 mg/m2 oxaliplatin: grade 4 nausea and or vomiting, grade 3 or 4 diarrhea, grade 4 stomatitis, and grade 3 or 4 skin toxicity. Permanent cessation of oxaliplatin was mandatory if grade 3 or 4 neuropathy occurred on more than 7 days of a cycle, but S-1 was continued as monotherapy.
Subsequent cycles were started only when toxicity measurements satisfied the following criteria: neutrophil count >1,500/μL; platelet count >75,000/μL; and recovery of non-hematologic toxicities to grade 1 or less, except total bilirubin and AST/ALT elevation to grade 2 or less. If the delay period exceeded 3 weeks, patients were withdrawn from the study.
A safety evaluation, including an assessment of laboratory data and any clinical adverse events, was performed after the completion of each cycle. Treatment response was evaluated every 3 cycles by abdominal computed tomography and other appropriate modalities valuable for the assessment of measurable or evaluable lesions. Tumor response was measured unidimensionally according to the RECIST 1.0 criteria, and responses were confirmed at least 4 weeks after initial assessment. To record adverse events, the National Cancer Institute Common Toxicity Criteria (Version 3.0) were used.
We evaluated the association of several clinical characteristics [age (≥65 vs. <65 years old), N stage (regional lymph node positive vs. negative), T stage (T4 vs. non-T4), tumor differentiation (well and moderately differentiated vs. poorly and undifferentiated), ECOG PS (0 vs. 1 and 2), and baseline carcinoembryonic antigen (CEA) level (≤100 vs. >100 ng/mL)] to RR and PFS.
Genetic analysis
The polymorphisms investigated included 15 SNPs among 8 genes that were already known for their association with fluoropyrimidine or platinum in terms of efficacy or toxicity [13–20]. The polymorphisms included thymidylate synthase enhancer region(TSER), 3′-utr, and 5′G/C polymorphism for thymidylate synthase (TS); C8092A and Asn118Asn for excision repair cross-complementing-group 1(ERCC1); Lys751Gln, C156A, and Asp312Asn for ERCC2; 5Arg399Gln, Arg194Trp, and Arg280His for X-ray repair cross-complementing-group 1 (XRCC1); Ile105Val for glutathione S-transferase P1 (GSTP1); −48G/T for CYP2A6; I340 M for alanine-glyoxylate aminotransferase (AGXT); A1298C for methylenetetrahydrofolate reductase (MTHFR). We analyzed the relation of each of the 15 SNPs to tumor response, PFS, OS, and major toxicities (neutropenia, stomatitis, diarrhea, and sensory neuropathy). Genomic DNA was extracted from peripheral blood samples using QIAmp DNA blood kits (Qiagen Inc., Hilden, Germany) and stored at 4°C until genotyping.
TSER was assessed by polymerase chain reaction (PCR) technique, and SNPs were analyzed by PCR-restriction fragment length polymorphism (RFLP) method. The PCR volume was 20 μL. In RFLP, amplified reaction products were digested with the restriction enzyme. Digested fragments were visualized on a 3% agarose gel. The genotyping of the CYP2A6 polymorphism CYP2A6*9 (−48G/T, rs28399433) was screened using the TaqMan fluorogenic 5′ nuclease assay (ABI, Foster City, CA, USA).
Statistical analysis
The primary endpoint of the study was to evaluate RR and safety of biweekly S-1 with oxaliplatin chemotherapy. Secondary endpoints were the evaluation of PFS and OS and the association between genetic polymorphisms and treatment outcomes. According to Simon’s optimal two-stage design, at least 46 eligible patients were required on the basis of a null hypothesis of <30% RR versus an alternative of ≥50% (80% power with α = 0.05). The first stage of the study required 15 patients, and if at least 5 objective responses were observed, the second stage required a total of 46 patients. If at least 18 patients responded after the second accrual stage, treatment was considered promising. Estimating a 10% drop-out rate during enrollment, a total of 51 patients were the target sample size. Associations between response rate and polymorphism or between toxicity and polymorphism were assessed by Chi-square test and Fisher’s exact test, where appropriate. PFS and OS were analyzed by the Kaplan–Meier method. Variables showing association with PFS in univariable analysis with P < 0.1 were included for multivariable analysis by a backward Cox regression models. Before we performed the Cox regression analysis, we evaluated the log–log plots for each of independent variables (the clinical factors and SNPs) to confirm that our analyses satisfied the proportional hazard assumption. A correction for multiple testing was not performed. All values were two-sided, and statistical significance was accepted at the P < 0.05 level. Safety was analyzed in all patients who received at least one dose of study medications. SPSS version 15.0 software (SPSS Inc., Chicago, IL, USA) and SAS version 9.1 (SAS Institute, Cary, NC, USA) were used for statistical analyses.
Results
Patient characteristics
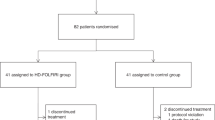
Between May 2007 and May 2009, a total of 52 patients were enrolled. One patient withdrew the consent after the first cycle, and 51 patients were evaluable for response. Baseline patient characteristics and clinical features are summarized in Table 1. During the median follow-up duration of 17.1 months (range 3.9–28.2 months), 46 patients experienced disease progression, and 15 patients died. All of the censored patients in PFS analysis remained progression-free and were receiving study treatment when the analysis was performed. The median number of cycles delivered was 9.0 (range 1–26).
Clinical outcomes
Of 51 evaluable patients, the best overall response was complete response (CR) in 2 (3.9%), partial response (PR) in 22 (43.1%), stable disease (SD) in 24 (47.1%), and progressive disease (PD) in 3 (5.9%) patients. The overall RR was 46.2% [95% confidence interval (CI) 32.1–60.2] in an intent-to-treat analysis and 47.1% (95% CI 32.9–61.2%) among the evaluable patients (Table 2). Among the evaluable patients, median PFS was 6.4 months (95% CI 4.8–8.1 months) and median OS had not been reached yet (Fig. 1). The 1-year overall survival rate was 75.8%, and the 2-year overall survival rate was 63.9%. Median-delivered dose intensity (DI) of S-1 and oxaliplatin was 250 and 38 mg/m2/week, respectively. Relative DI was 89.3% for S-1 and 89.4% for oxaliplatin.
In univariable analysis, tumor differentiation (well and moderate vs. others) and baseline CEA level (≤100 vs. >100 ng/ml) were related to PFS (Table 3). There was no evidence of an association between clinical characteristics and RR.
Safety
Frequently observed toxicities were sensory neuropathy (73.1%), nausea (48.1%), anorexia (40.3%), diarrhea (23.0%), and stomatitis (15.4%). Neutropenia (7.7%), thrombocytopenia (5.8%), sensory neuropathy (7.7%), and diarrhea (1.9%) were observed as grade 3 toxicities. There were no hematologic or non-hematologic grade 4 toxicities observed. No neutropenic fever was reported. The toxicity profile is summarized in Table 4.
Pharmacogenetic analysis
Fifteen SNPs among 8 genes were analyzed in relation to response, toxicities, and PFS. In the pharmacogenetic analysis of Asn118Asn of ERCC1, grade 3 neutropenia occurred in 4 of 18 patients (22%) with C/T or T/T genotypes compared with none of 33 patients (0%) with the C/C homozygous genotype (P = 0.01). Patients with A/G (n = 12) or G/G (n = 2) genotypes in Ile105Val SNP of GSTP1 had significantly longer PFS compared to patients with the A/A (n = 37) genotype (P = 0.04; median 8.3 vs. 6.1 months, respectively) (Fig. 2). In multivariate analysis, Ile105Val SNP revealed a tendency toward an association with PFS (hazard ratio 0.47, 95% CI 0.21–1.04; P = 0.06) (Table 3). This polymorphism was also associated with neurotoxicity. Patients with A/G or G/G genotypes experienced more frequent G2/3 sensory neuropathy [5 of 14 (35.7%) in A/G or G/G vs. 3 of 37 (8.1%) in A/A, P = 0.03]. There was no evidence of an association between any other SNP and efficacy or toxicity (Table 5).
Discussion
In this study, we assessed the clinical efficacy and safety of biweekly S-1 with oxaliplatin as first-line chemotherapy in metastatic or recurrent CRC. This regimen showed a RR of 47.1%, a median PFS of 6.4 months, satisfactory dose intensities, and an excellent safety profile. Grade 3 neutropenia and grade 3 thrombocytopenia were observed in 4 (7.7%) and 3 patients (5.8%), respectively. No grade 4 hematologic toxicity or neutropenic fever was reported. Non-hematologic toxicities were also outstanding; there was no grade 4 non-hematologic toxicity. Only one patient (1.9%) experienced grade 3 diarrhea. Sensory neuropathy was the most commonly observed non-hematologic toxicity (73.1%).
Considering the objective RR ranged from 41 to 52% for the infusional 5-FU-based combinations and from 27 to 48% for the capecitabine-based regimens with oxaliplatin [4], the overall RR of this study was sufficient to prove efficacy as first-line chemotherapy in metastatic CRC.
With the support of proven activity and safety of S-1 monotherapy [8–10], two studies of S-1 with oxaliplatin as first-line therapy in metastatic CRC were previously reported. A phase I/II study by Yamada et al. [21] determined 130 mg/m2 of oxaliplatin on day 1 with 40–60 mg of S-1 twice daily for 2 weeks followed by 1-week rest in a 3-weekly schedule as a recommended dose. In the phase II part of the study, they reported a RR of 50%, a median PFS of 6.6 months, and a 1-year survival rate of 79% among 28 Japanese patients with metastatic CRC. Zang et al. [22] conducted a phase II study with the same dose and schedule of S-1 in combination with oxaliplatin in 49 Korean patients; the RR was 54%, the median time to progression was 8.5 months, and the OS was 27.2 months.
Biweekly S-1 with oxaliplatin achieved similar RRs to 3-weekly studies in spite of a lower planned DI of S-1 (280 mg/m2/week for biweekly vs. 373 mg/m2/week for 3-weekly) with a similar planned DI of oxaliplatin. The median relative DI of the 3-weekly study by Zang et al. [22] was 82% for S-1 and 82% for oxaliplatin, respectively. The satisfactory relative DI of over 89% for both S-1 and oxaliplatin in this study shows that oxaliplatin can be delivered more efficiently by a biweekly schedule without a significantly lower delivered DI of S-1.
Biweekly schedules showed lower frequencies of grade 3 or 4 thrombocytopenia (5.8%) compared to 3-weekly regimens (13% in the study of Zang et al. and 27% in the study of Yamada et al.). Occurrence of grade 3 neutropenia (7.7%) was also lower than 3-weekly studies (10% in the study of Zang et al. and 14% in the study of Yamada et al.). All of the 3 studies of S-1 with oxaliplatin in metastatic CRC showed no grade 4 neutropenia and generally manageable non-hematologic toxicities. Zang et al. supposed that the reduced occurrence of severe non-hematologic toxicity of their study might due in part to the relatively young patient population (median age 56 years, range 24–70) [22] in comparison with other studies, which typically had median ages between 58 and 67 years [5, 6, 9, 23, 24]. In this trial, an excellent toxicity profile was reproduced with similar efficacy in spite of an older population (median age 63, range 37–74) compared to the study of Zang et al. This strongly suggests that the biweekly schedule of S-1 with oxaliplatin combination has better tolerability than the 3-weekly schedule.
These toxicities of biweekly S-1 with oxaliplatin seem to be superior to that of the FOLFOX-4 regimen, for which frequencies of 27–50% for grade 3 or 4 neutropenia, 12–16% for grade 4 neutropenia, and 11–12% for grade 3 or 4 diarrhea were reported in phase III studies [5, 6, 23]. Also, compared to the XELOX regimen, for which frequencies of 7–15% for grade 3 or 4 neutropenia, 14–31% for grade 3 or 4 diarrhea, and 2–19% for hand–foot syndrome (HFS) have been reported [6, 24, 25], biweekly S-1 with oxaliplatin showed less frequent diarrhea and HFS. Sensory neuropathy is one of the most common adverse events in of fluoropyrimidines and oxaliplatin combinations [5, 6, 21, 22, 24], and most patients with sensory neuropathy in our study were grade 1, which is not inferior to other studies.
The efficacy and toxicity data of the present study suggest that biweekly S-1 with oxaliplatin can be considered as a substitute for 5-FU infusion with oxaliplatin, especially for CRC patients with old age, poor PS, or those who are concerned about infections.
Survival correlation of Ile105Val of GSTP1 is in line with previous studies [19, 26–28]. Stoehlmacher et al. conducted an analysis of 107 previously treated advanced CRC patients who received 5-FU with oxaliplatin combination chemotherapy. Patients with the Val/Val (G/G) genotype showed 24.9 months of median OS, while those with the Ile/Ile (A/A) genotype survived 7.9 months, and those with the Ile/Val (A/G) genotype survived 13.3 months (P < 0.001) [19]. A recent study by Chen et al. [27] to analyze the influence of Ile105Val polymorphisms of GSTP1 on clinical outcomes in 166 Chinese patients with metastatic CRC who had been treated with first-line FOLFOX-4 chemotherapy also exhibited similar results; patients with A/G or G/G genotypes had a higher response to FOLFOX-4 (56.1 vs. 37.6%, P = 0.04) and a longer PFS (P < 0.01) as well as OS (P < 0.01) than patients with A/A genotypes. This polymorphism was identified as an independent prognostic factor by adjusted analysis (P = 0.01).
Association of neuropathy and Ile105Val of GSTP1 was also revealed in previous studies [27–29]. The Arbeitsgemeinschaft Internische Onkologie group, for example, conducted a phase III study in metastatic gastroesophageal adenocarcinoma with 5-FU and LV plus either oxaliplatin or cisplatin [28]. On pharmacogenetic analysis, patients with grade 3 or 4 neuropathy associated with the GSTP1-105 Ile/Ile genotype were at higher risk of experiencing grade 3 neurotoxicity, with an odds ratio of 5.8 (95% CI 1.21–27.86), compared with patients with Ile/Val or Val/Val genotypes (P = 0.03).
Members of the glutathione S-transferase superfamily are important in cellular defense mechanisms. The substitution of isoleucine with valine at codon 105 lowers the catalytic activity of GSTP1 protein [30] and defense mechanisms against chemotherapeutic agents like platinum decline [31]. This process may explain the association between Ile105Val polymorphism and PFS. Chen et al. suggested that Asian populations may have a lower prevalence of Ile105Val polymorphism in GSTP1 based on patient distribution in their study (75.3% for A/A, 22.9% for A/G, and 1.8% for G/G) compared to that in a study by Stoehlmacher et al. [19] (49% for A/A, 42% for A/G, and 9% for G/G) and another Western study [29]. Patient distribution of Ile105Val polymorphism in this study was 72.5% for A/A, 23.5% for A/G, and 3.9% for G/G; similar distribution in the study of Chen et al. supports the existence of ethnic difference. The association between GSTP1 Ile105Val and treatment outcome merits further investigation into a large study. The relationship between frequency of neutropenia and Asn118Asn of ERCC1 has yet to be established, and some results indicating no association [28, 32, 33]; interpretation should be reserved until other supportive data emerge.
In conclusion, S-1 with oxaliplatin administered in a biweekly schedule is effective and has better tolerability and convenience compared to other fluoropyrimidine with oxaliplatin combinations in metastatic CRC. GSTP1 Ile105Val SNP is associated with clinical outcomes.
References
Won YJ, Sung J, Jung KW, Kong HJ, Park S, Shin HR, Park EC, Ahn YO, Hwang IK, Lee DH, Choi JS, Kim WC, Lee TY, Yoo CI, Bae JM, Kim ON, Chung W, Kong IS, Lee JS (2009) Nationwide cancer incidence in Korea, 2003–2005. Cancer Res Treat 41:122–131
Grem JL (2002) 5-Fluorouracil and its biomodulation in the management of colorectal cancer. In: Saltz L (ed) Colorectal cancer: multimodality management. Humana Press Inc, Totowa, pp 469–470
Meta-analysis Group in Cancer (1998) Efficacy of intravenous continuous infusion of fluorouracil compared with bolus administration in advanced colorectal cancer. J Clin Oncol 16:301–308
Arkenau HT, Arnold D, Cassidy J, Diaz-Rubio E, Douillard JY, Hochster H, Martoni A, Grothey A, Hinke A, Schmiegel W, Schmoll HJ, Porschen R (2008) Efficacy of oxaliplatin plus capecitabine or infusional fluorouracil/leucovorin in patients with metastatic colorectal cancer: a pooled analysis of randomized trials. J Clin Oncol 26:5910–5917
de Gramont A, Figer A, Seymour M, Homerin M, Hmissi A, Cassidy J, Boni C, Cortes-Funes H, Cervantes A, Freyer G, Papamichael D, Le Bail N, Louvet C, Hendler D, de Braud F, Wilson C, Morvan F, Bonetti A (2000) Leucovorin and fluorouracil with or without oxaliplatin as first-line treatment in advanced colorectal cancer. J Clin Oncol 18:2938–2947
Cassidy J, Clarke S, Diaz-Rubio E, Scheithauer W, Figer A, Wong R, Koski S, Lichinitser M, Yang TS, Rivera F, Couture F, Sirzen F, Saltz L (2008) Randomized phase III study of capecitabine plus oxaliplatin compared with fluorouracil/folinic acid plus oxaliplatin as first-line therapy for metastatic colorectal cancer. J Clin Oncol 26:2006–2012
Shirasaka T, Shimamato Y, Ohshimo H, Yamaguchi M, Kato T, Yonekura K, Fukushima M (1996) Development of a novel form of an oral 5-fluorouracil derivative (S-1) directed to the potentiation of the tumor selective cytotoxicity of 5-fluorouracil by two biochemical modulators. Anticancer Drugs 7:548–557
Ohtsu A, Baba H, Sakata Y, Mitachi Y, Horikoshi N, Sugimachi K, Taguchi T (2000) Phase II study of S-1, a novel oral fluorophyrimidine derivative, in patients with metastatic colorectal carcinoma. S-1 Cooperative Colorectal Carcinoma Study Group. Br J Cancer 83:141–145
Shirao K, Ohtsu A, Takada H, Mitachi Y, Hirakawa K, Horikoshi N, Okamura T, Hirata K, Saitoh S, Isomoto H, Satoh A (2004) Phase II study of oral S-1 for treatment of metastatic colorectal carcinoma. Cancer 100:2355–2361
Van den Brande J, Schoffski P, Schellens JH, Roth AD, Duffaud F, Weigang-Kohler K, Reinke F, Wanders J, de Boer RF, Vermorken JB, Fumoleau P (2003) EORTC Early Clinical Studies Group early phase II trial of S-1 in patients with advanced or metastatic colorectal cancer. Br J Cancer 88:648–653
Yong WP, Innocenti F, Ratain MJ (2006) The role of pharmacogenetics in cancer therapeutics. Br J Clin Pharmacol 62:35–46
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92:205–216
Gamelin L, Capitain O, Morel A, Dumont A, Traore S, Anne le B, Gilles S, Boisdron-Celle M, Gamelin E (2007) Predictive factors of oxaliplatin neurotoxicity: the involvement of the oxalate outcome pathway. Clin Cancer Res 13:6359–6368
Gurubhagavatula S, Liu G, Park S, Zhou W, Su L, Wain JC, Lynch TJ, Neuberg DS, Christiani DC (2004) XPD and XRCC1 genetic polymorphisms are prognostic factors in advanced non-small-cell lung cancer patients treated with platinum chemotherapy. J Clin Oncol 22:2594–2601
Ishida Y, Kawakami K, Tanaka Y, Kanehira E, Omura K, Watanabe G (2002) Association of thymidylate synthase gene polymorphism with its mRNA and protein expression and with prognosis in gastric cancer. Anticancer Res 22:2805–2809
Kawakami K, Watanabe G (2003) Identification and functional analysis of single nucleotide polymorphism in the tandem repeat sequence of thymidylate synthase gene. Cancer Res 63:6004–6007
Osian G, Procopciuc L, Vlad L, Iancu C, Mocan T, Mocan L (2009) C677T and A1298C mutations in the MTHFR gene and survival in colorectal cancer. J Gastrointestin Liver Dis 18:455–460
Ryu JS, Hong YC, Han HS, Lee JE, Kim S, Park YM, Kim YC, Hwang TS (2004) Association between polymorphisms of ERCC1 and XPD and survival in non-small-cell lung cancer patients treated with cisplatin combination chemotherapy. Lung Cancer 44:311–316
Stoehlmacher J, Park DJ, Zhang W, Groshen S, Tsao-Wei DD, Yu MC, Lenz HJ (2002) Association between glutathione S-transferase P1, T1, and M1 genetic polymorphism and survival of patients with metastatic colorectal cancer. J Natl Cancer Inst 94:936–942
Zhou W, Gurubhagavatula S, Liu G, Park S, Neuberg DS, Wain JC, Lynch TJ, Su L, Christiani DC (2004) Excision repair cross-complementation group 1 polymorphism predicts overall survival in advanced non-small cell lung cancer patients treated with platinum-based chemotherapy. Clin Cancer Res 10:4939–4943
Yamada Y, Tahara M, Miya T, Satoh T, Shirao K, Shimada Y, Ohtsu A, Sasaki Y, Tanigawara Y (2008) Phase I/II study of oxaliplatin with oral S-1 as first-line therapy for patients with metastatic colorectal cancer. Br J Cancer 98:1034–1038
Zang DY, Lee BH, Park HC, Song HH, Kim HJ, Jung JY, Kim JH, Kim HY, Kwon JH, Hwang SW, Park SR, Park CH, Kim KO, Kim MJ, Jang KM (2009) Phase II study with oxaliplatin and S-1 for patients with metastatic colorectal cancer. Ann Oncol 20:892–896
Goldberg RM, Sargent DJ, Morton RF, Fuchs CS, Ramanathan RK, Williamson SK, Findlay BP, Pitot HC, Alberts SR (2004) A randomized controlled trial of fluorouracil plus leucovorin, irinotecan, and oxaliplatin combinations in patients with previously untreated metastatic colorectal cancer. J Clin Oncol 22:23–30
Diaz-Rubio E, Tabernero J, Gomez-Espana A, Massuti B, Sastre J, Chaves M, Abad A, Carrato A, Queralt B, Reina JJ, Maurel J, Gonzalez-Flores E, Aparicio J, Rivera F, Losa F, Aranda E (2007) Phase III study of capecitabine plus oxaliplatin compared with continuous-infusion fluorouracil plus oxaliplatin as first-line therapy in metastatic colorectal cancer: final report of the Spanish Cooperative Group for the Treatment of Digestive Tumors Trial. J Clin Oncol 25:4224–4230
Hochster HS, Hart LL, Ramanathan RK, Childs BH, Hainsworth JD, Cohn AL, Wong L, Fehrenbacher L, Abubakr Y, Saif MW, Schwartzberg L, Hedrick E (2008) Safety and efficacy of oxaliplatin and fluoropyrimidine regimens with or without bevacizumab as first-line treatment of metastatic colorectal cancer: results of the TREE Study. J Clin Oncol 26:3523–3529
Sweeney C, McClure GY, Fares MY, Stone A, Coles BF, Thompson PA, Korourian S, Hutchins LF, Kadlubar FF, Ambrosone CB (2000) Association between survival after treatment for breast cancer and glutathione S-transferase P1 Ile105Val polymorphism. Cancer Res 60:5621–5624
Chen YC, Tzeng CH, Chen PM, Lin JK, Lin TC, Chen WS, Jiang JK, Wang HS, Wang WS (2010) Influence of GSTP1 I105V polymorphism on cumulative neuropathy and outcome of FOLFOX-4 treatment in Asian patients with colorectal carcinoma. Cancer Sci 101:530–535
Goekkurt E, Al-Batran SE, Hartmann JT, Mogck U, Schuch G, Kramer M, Jaeger E, Bokemeyer C, Ehninger G, Stoehlmacher J (2009) Pharmacogenetic analyses of a phase III trial in metastatic gastroesophageal adenocarcinoma with fluorouracil and leucovorin plus either oxaliplatin or cisplatin: a study of the arbeitsgemeinschaft internistische onkologie. J Clin Oncol 27:2863–2873
Lecomte T, Landi B, Beaune P, Laurent-Puig P, Loriot MA (2006) Glutathione S-transferase P1 polymorphism (Ile105Val) predicts cumulative neuropathy in patients receiving oxaliplatin-based chemotherapy. Clin Cancer Res 12:3050–3056
Watson MA, Stewart RK, Smith GB, Massey TE, Bell DA (1998) Human glutathione S-transferase P1 polymorphisms: relationship to lung tissue enzyme activity and population frequency distribution. Carcinogenesis 19:275–280
Goto S, Iida T, Cho S, Oka M, Kohno S, Kondo T (1999) Overexpression of glutathione S-transferase pi enhances the adduct formation of cisplatin with glutathione in human cancer cells. Free Radic Res 31:549–558
Kalikaki A, Kanaki M, Vassalou H, Souglakos J, Voutsina A, Georgoulias V, Mavroudis D (2009) DNA repair gene polymorphisms predict favorable clinical outcome in advanced non-small-cell lung cancer. Clin Lung Cancer 10:118–123
Seo BG, Kwon HC, Oh SY, Lee S, Kim SG, Kim SH, Han H, Kim HJ (2009) Comprehensive analysis of excision repair complementation group 1, glutathione S-transferase, thymidylate synthase and uridine diphosphate glucuronosyl transferase 1A1 polymorphisms predictive for treatment outcome in patients with advanced gastric cancer treated with FOLFOX or FOLFIRI. Oncol Rep 22:127–136
Acknowledgments
This study was supported by a grant of the Korea Health 21 R&D project, Ministry for Health, Welfare and Family Affairs, Republic of Korea (A030001) and a grant of the Korea Healthcare technology R&D Project, Ministry for Health, Welfare & Family affairs, Republic of Korea. (A091081). We thank Medical Research Collaborating Center, Seoul National University Hospital, Seoul, Korea for statistical consultation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hong, J., Han, SW., Ham, H.S. et al. Phase II study of biweekly S-1 and oxaliplatin combination chemotherapy in metastatic colorectal cancer and pharmacogenetic analysis. Cancer Chemother Pharmacol 67, 1323–1331 (2011). https://doi.org/10.1007/s00280-010-1425-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-010-1425-7