Abstract
Purpose
Ifosfamide (IFS) is often involved in the occurrence of hemorrhagic cystitis due to direct contact of its metabolite acrolein with uroepithelium. It has been shown that COX-2 is involved in this pathogenesis. Thus, we aimed to study the functional changes on the urinary bladder in the putative modifications induced by IFS, as well as the COX-2 role in this process.
Materials and methods
IFS-treated rats were evaluated by cystometrography in absence or presence of COX inhibitors indomethacin or etoricoxib or in the presence of mesna. Experiments with isolated strips of urinary bladder obtained from animals with IFS-induced cystitis, either treated or not treated with COX inhibitors or mesna, were performed. Histological analyses, immunohistochemistry for COX-2, and measurement of plasma PGE2 were also performed.
Results
IFS treatment caused severe inflammation of the bladder tissue. Cystometrography recordings of IFS-treated rats revealed bladder with increased micturition frequency and enhanced filling intravesical pressure. Contractility of the isolated smooth muscle from the rat’s bladder with IFS-induced cystitis showed decreased force development in response to KCl and CCh. Almost all effects induced by IFS were ameliorated by the use of COX inhibitors or mesna. Enzyme expression in the urinary bladder tissue was positive, and plasma concentration of PGE2 was increased in IFS-treated animals and decreased significantly in etoricoxib-treated animals.
Conclusions
IFS causes important changes in the micturition physiology in rats, and the inhibition of the isoenzyme COX-2 could be an important event that could prevent the detrimental effects elicited by IFS-induced hemorrhagic cystitis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ifosfamide (IFS) is an alkylating agent used in a variety of refractory tumors, such as soft tissue sarcomas, refractory germ cell tumors, and malignant lymphomas [1]. IFS is metabolized within the liver into two main compounds: isofosforamide mustard and acrolein, an inactive metabolite excreted by the urinary system [2]. It is well known that renal excretion of acrolein is highly irritating to the urinary bladder, causing toxic effects [3] and responsible for the development of life-threatening complications, such as hemorrhagic cystitis [4].
The involvement of inflammatory mediators, such as nitric oxide (NO), in the urothelium after IL-1β and TNF-α production has been reported [5]. Furthermore, the use of dexamethasone in association with mesna, as well as pretreatment with glutathione or amifostine, prevented inflammatory changes induced by IFS [6, 7]. Recently, it has been shown that prostanoid mediators produced by COX-2 expression may be involved in the pathogenesis of IFS-induced hemorrhagic cystitis and its metabolite acrolein [8, 9].
Despite the well-characterized cytotoxic effects induced by IFS, there are no reports showing the repercussions of IFS treatment on the motor functions of the urinary system. In contrast, cyclophosphamide, another alkylating agent that similarly causes hemorrhagic cystitis, is reported to promote important effects on the motor functions of the urinary bladder smooth muscle, including bladder overactivity in vivo, which can be characterized by decreased bladder capacity and increased micturition frequency [10]. The overactivity of detrusor muscle after experimental cystitis induced by cyclophosphamide has been well studied, and the participation of prostaglandins produced by the COX-2 enzyme on this phenomenon was already described [11]. In the light of these concepts, the present study aimed both to assess the ability of IFS in inducing functional changes on the bladder smooth muscle activity and to evaluate whether COX-2 is involved in the putative modifications induced by IFS on the urinary bladder smooth muscle behavior.
Materials and methods
Animals
Male Wistar rats (150–200 g, 6/group) were obtained from the Department of Physiology and Pharmacology, Fortaleza, Brazil, and kept in appropriate cages under conditions of constant temperature (22–26°C), 12-h light–dark cycle, and free access to food and water. All animal procedures were carried out according to the standards established by the NIH Guide for the Care and Use of Laboratory Animals and the Institutional Animal Care and Use Committee (protocol number 06/06).
Solutions and drugs
Ifosfamide (Holoxane™), mesna (Mitexan™) (ASTA Medica-AG. Frankfurt, Germany), and etoricoxib (Arcoxia™; Merck-Sharpe Dome, Brazil) were dissolved in 0.9% sterile saline. Indomethacin (Indocin™; Merck & Sharpe Co., USA) was dissolved in 5% sodium bicarbonate. Urethane and carbachol (CCh) were purchased from Sigma Chemical Co. (St. Louis, MO, USA). The perfusion medium used was fresh modified Tyrode solution (pH 7.4) of the following composition (mM): NaCl 136, KCl 5, MgCl2 0.98, CaCl2 2, NaH2PO4 0.36, NaHCO3 11.9, and glucose 5.5.
IFS-induced hemorrhagic cystitis model
Hemorrhagic cystitis was induced as described in our previous study [6]. In brief, IFS (400 mg/kg) was injected i.p.; 24 h later, the animals were used either for urodynamic studies in vivo or to evaluate bladder smooth muscle activity in vitro. In other experimental groups, animals were treated 1 h before IFS injection with etoricoxib (12 mg/kg, p.o.), a selective COX-2 inhibitor, or indomethacin (2 mg/kg, s.c.), a nonselective COX-2 inhibitor [12]. As positive control, a separate group received mesna (20% of IFS whole dose, 80 mg/kg, i.p.) 0, 4, and 8 h after IFS administration.
Surgical procedures and preparation for urodynamic studies
Intravesical catheter placement
A lower midline abdominal incision was performed under general anesthesia with urethane (50%, 1.2 g/kg, s.c.) [13]. A polyethylene tubing (PE-50) was inserted into the dome of the bladder through the upper bladder wall and secured in place with a 6–0 nylon purse string suture. The distal end of the tubing was filled with saline and then carefully sealed to avoid air into the lumen. The tube was externalized, and then, the abdominal incision was closed with 4–0 nylon sutures. Animals were kept in a warm environment (36°C) for 1 h after the surgery.
Cystometrogram
All groups were evaluated with cystometrogram. Before the start of recording, the bladder was emptied of urine by syringe aspiration, and the catheter was connected via a T tube to a pressure transducer and microinjection pump. The bladder was continuously infused with saline (0.06 ml/min) at room temperature. Intravesical pressure was continuously recorded using data acquisition system for pressure measurements. At least four reproducible micturition cycles were recorded after the initial stabilization period of 30–45 min. The following cystometric parameters were recorded in each animal: filling intravesical pressure, maximum intravesical pressure, and frequency and time of micturition. At the end of each experiment, all the rats were killed by cervical dislocation, and the correct placement of the bladder catheter was verified. Despite the cystometrogram results, we considered for statistical analyses only the animals with a good catheter placement (tip of the catheter within the bladder lumen not touching the bladder wall and no kinked catheters).
In vitro evaluation of urinary bladder contractility
After euthanasia of the rats, the urinary bladder was harvested and cut in longitudinal strips (6.0 × 2.0 mm), then mounted in 5 ml double jacketed of Tyrode solution baths aerated at 37°C with a mixture 95% O2–5% CO2. Strips were stretched with a passive tension of 1 g and recorded using an isometric transducer connected to a PC-based Dataq (PM-1000) acquisition system. After an equilibration period of at least 30 min, control contractions were induced by adding 60 mM potassium chloride to the bath. When two successive control contractions showed similar amplitude, preparations were considered to be equilibrated. Full concentration–response curves were constructed by exposing the preparation to increasing agonist concentrations (KCl [0.01 to 0.12 M] or carbachol–CCh [10−9 to 10−5 M]) added cumulatively to the bath (60 s for each concentration or, when necessary, 90s to observe the plateau response). E max was considered to have been achieved when an increase in the agonist concentration did not induce a significant additional response. The contractile amplitude was measured at the peak deflection. At the end of the experiments, bladder strips were removed from bath chamber and were then stored in an oven for 24 h at 80°C. Afterward, they were weighed for determination of contractile force/mass of dry tissue.
Bladder smooth muscle immunohistochemistry for COX-2
COX-2 expression in rat urinary bladder was assessed by an immunohistochemical approach previously reported [8]. Briefly, it was carried out according to the streptavidin–biotin–peroxidase complex technique, using a primary antibody raised against COX-2 protein [Rabbit monoclonal antibody (clone SP21), Neomarkers, Freemont, CA, USA] diluted 1:50. Sections (4-μm) were deparaffinised, re-hydrated, immersed in 0.01 M citrate buffer (pH 6.0), and microwaved at 600 w for 15 min; then the slides were sequentially incubated with 3% hydrogen peroxide in methanol for 10 min, with Ultravision Block solution (Neomarkers) for 10 min, and with the primary antibody for 2 h, at room temperature. Sections were washed in PBS 1× with 0.02% Tween 20 and incubated with biotinylated goat anti-polyvalent antibody for 10 min, streptavidin peroxidase for 10 min, and developed with 3,3′-diamino-benzidine for 10 min. Slides were counterstained with Mayer hematoxylin and permanently mounted. Negative controls of reactions were performed with omission of the primary antibody; as positive control, we used colon carcinoma tissue, as indicated by the manufacturer. In the absence of primary antibody, no positive immunostaining was observed.
Plasma quantification of PGE2
In all groups, blood samples (2 ml) were thawed to room temperature before testing, vortexed for 30 s, and centrifuged at room temperature for 5 min at 1000×g; 7 picograms (pg) of tritium-labeled 5, 6, 8, 11, 12, 14, 15-3H (N)-PGE2 was added, followed by absolute ethanol and vortexed for 1 min. The samples were allowed to stand at 4°C for 5 min and then centrifuged (40°C, 10 min, 1500×g), and the supernatant was decanted into 10-ml glass tubes followed by 8 ml of pH 4 adjusted 0.1 M phosphate buffer and vortexed for another 30 s. The samples were percolated and washed with 5 ml water, followed by 5 ml HPLC grade hexane and evaporated under nitrogen at 350°C. The samples were reconstituted with 1 ml EIA buffer, sonicated (30 s), and vortexed (30 s).
Each sample (0.5 ml) was added to 4 ml scintillation fluid and counted in a liquid scintillation counter. The remaining fluid of each sample (500 μl) and the PGE2 standards were incubated overnight with 150 μl of 1 M bicarbonate buffer to convert any PGE2 to bicyclo PGE2. Bicyclo PGE2 concentrations were determined using a commercially available EIA kit. The 96-well EIA plates were read at 412 nm using a plate reader. All PGE2 samples were read at 3 different dilutions, and concentrations were calculated by the mean. PGE2 levels were reported as mean values of ng PGE2/μg total protein.
Statistical analysis
Data were expressed as mean ± standard error of the mean (number of experiments), except for macroscopic and histopathologic evaluations, which were reported as median values. Contractile data were expressed as force (in g)/tissue dry weight (in mg). Statistical significance was assessed by ANOVA. When significant, it was followed by a multiple comparison test as appropriately indicated. For macroscopic and microscopic data, a Kruskal–Wallis nonparametric ANOVA followed by the Dunn test was used for statistical comparisons. Values for pD2, the negative logarithm of half maximum effective concentration–EC50–correspondent to the concentration that can be expected to cause a defined effect on 50%, were shown as geometric mean [95% confidence interval]. The individual concentration–response curves were analyzed by a four parameter logistic equation [y = min + [max − min/[1 + (x/EC50)−Hill slope] for pD2. Statistical significance was accepted when P < 0.05.
Results
Induction of hemorrhagic cystitis
After 24 h, IFS-treated animals developed severe hemorrhagic cystitis, which was characterized macroscopically by the presence of marked edema, intense urothelial damage, leukocyte infiltration, and hemorrhage. Scores were attributed to histological changes induced by the treatment with IFS and analyzed by Gray’s criteria reported previously [8] and were significantly (P < 0.05) different from the saline-treated control group. Bladders from the rats that received etoricoxib, indomethacin, or mesna before treatment with IFS revealed a macroscopically reduced inflammatory pattern that was confirmed by histopathologic parameters (Table 1).
Immunohistochemical analysis of the COX-2 expression within the bladder smooth muscle
COX-2 expression was seen mainly within the bladder smooth muscle cells in those animals treated with IFS when compared with the saline-treated animals (P < 0.05, Fig. 1; Table 1). Treatment with etoricoxib, indomethacin, or mesna reduced the intensity of COX-2 expression (P < 0.05) in bladder smooth muscle cells.
Immunohistochemistry for COX-2 expression. COX-2 is seen within smooth muscle cells of bladder obtained from animals treated with IFS. In a, it is observed a bladder from animal treated with saline + IFS 400 mg/kg showing high expression of COX-2. Treatment of the animal with indomethacin 2 mg/kg before IFS (b) or mesna (d) abolished cells marked for COX-2 marked cells. In + etoricoxib-treated animals, (c) light COX-2 expression can be seen. Arrows indicate COX-2 positive cells. ×400. Bar 100 μm
Effects of IFS-induced hemorrhagic cystitis upon rat urodynamics
Distension of the bladder above a given volume threshold for the micturition reflex-induced typical micturition contractions in the control animals and treatment with IFS markedly changed the micturition pattern (Fig. 2). Filling intravesical pressure was significantly (P < 0.05, Holm-Sidak test) higher in IFS-treated rats (30.26 ± 2.22 cmH2O; n = 5) than in saline-treated rats (6.36 ± 3.32 cmH2O; n = 5; Table 2). It is noteworthy that rats with hemorrhagic cystitis showed a cystometrographic profile undeniably different from those trace recordings obtained from saline-treated animals (Fig. 2, panels b and a, respectively). The main feature in most of the IFS-treated animals was the lack of an observable bladder contraction that could be associated with micturition, which occurred through an intermittent dripping of urine. Thus, in IFS-treated animals, maximum intravesical pressure, micturition frequency, and time of micturition were not determined.
Cystometrogram recordings in saline-treated rats (a) and rats treated with vehicle + IFS 400 mg/kg, ip (b), indomethacin 2 mg/kg + IFS (c), etoricoxib 12 mg/kg + IFS (d), or mesna 80 mg/kg + IFS (e). Dots under trace recordings indicate micturition. Calibrations for all traces are provided by the vertical scale in cmH2O, while horizontal is 2 min. Note the more pronounced stiffness of the filling phase in recordings of indomethacin- or etoricoxib-treated rats
Urodynamic effects of COX inhibitors and mesna in rats with IFS-induced cystitis
The rats that received etoricoxib or indomethacin 1 h before IFS, as well as animals that received mesna after treatment with IFS reversed all the changes seen in cystometrography traces from animals treated only with IFS. Cystometrogram parameters, such as filling intravesical pressure, maximum intravesical pressure, and urinary frequency, showed values that did not reach statistical difference in relation to values recorded to saline-treated rats (P > 0.05, ANOVA; Table 2). However, the time of micturition in animals treated with either etoricoxib (15.8 ± 4.61 s; n = 5) or indomethacin (13.07 ± 2.20 s; n = 5) but not with mesna was significantly higher (P < 0.05, Holm-Sidak test) than control values (6.40 ± 0.57 s; n = 5). Of note, in etoricoxib- or indomethacin-treated animals, filling pressures rose more rapidly than in saline- or even in mesna-treated rats (Fig. 2).
Effects of the treatment with IFS on the contractile responses of the rat urinary bladder smooth muscle to KCl or CCh in vitro
Isolated strips of rat urinary bladder stimulated with increasing concentrations of KCl (0.01 to 0.12 M; Fig. 3) or CCh (10−9 to 10−5 M; Fig. 4) produced full concentration–response curves in a concentration-dependent manner (P < 0.001, ANOVA). Strips obtained from saline-treated animals maximally contracted to values of 0.489 ± 0.068 g/mg of tissue (n = 7) and 1.048 ± 0.133 g/mg of tissue (n = 5) in response to KCl (0.12 M) or CCh (10−5 M), respectively (Table 3). Twenty-four hours after treatment with IFS, urinary smooth muscle showed KCl- or CCh-induced maximal contractions that corresponded to 0.240 ± 0.030 g/mg of tissue (n = 7) and 0.406 ± 0.076 g/mg of tissue (n = 7), values significantly smaller than those obtained from saline-treated tissues (P < 0.05, Holm-Sidak test). Moreover, the pharmacological potency for these contractile agents changed significantly in tissues obtained from animals treated with IFS compared with those of saline-treated group. Treatment with IFS significantly (P < 0.05, Holm-Sidak) decreased pD2 value for KCl (1.33 ± 0.07 in IFS vs. 1.54 ± 0.06 in control tissues), but increased it for contraction induced by CCh (6.78 ± 0.04 in IFS vs. 6.48 ± 0.06 in control). Similarly, these values also reached statistical significance (P < 0.05, Holm-Sidak).
Concentration–response curves to KCl in rat isolated urinary bladder smooth muscle. Contractile responsiveness was determined to cumulative additions of KCl (0.005 to 0.12 M) in isolated tissues obtained from animals treated 24 h earlier with either saline (Control; full circles) or IFS alone (empty circles). The concentration–effect curves were also performed in isolated tissues of animals that received etoricoxib (a), indomethacin (b), or mesna (c) 1 h before administration of IFS. Data are the mean ± SEM. n values are showed in Table 3
Concentration–response curves to CCh in rat isolated urinary bladder smooth muscle. Contractile responsiveness was determined to cumulative additions of CCh (10−9 to 10−5 M) in isolated tissues obtained from animals treated 24 h earlier with either saline (Control; full circles) or IFS alone (empty circles). The concentration–effect curves were also performed in isolated tissues of animals that received etoricoxib (a), indomethacin (b) or mesna (c) 1 h before administration of IFS. Data are the mean ± SEM. n values are showed in Table 3
Effects of etoricoxib, indomethacin, or mesna treatment on the IFS-inhibited contractile responses of the rat-isolated urinary bladder smooth muscle to KCl or CCh
Treatment with either etoricoxib or indomethacin 1 h before treatment with IFS showed values for maximal responses significantly (P < 0.05, Holm-Sidak test) greater than those obtained from strips of IFS-treated group (Figs. 3 and 4). Neither E max nor pD2 values of etoricoxib- or indomethacin-treated groups achieved significance compared with the control group, but pD2 values significantly differed from values of IFS-treated group. Treatment with mesna at 0, 4 and 8 h after IFS made the smooth muscle of the urinary bladder more responsive to KCl (pD2 of 1.72 ± 0.04; n = 6) when compared to urinary bladder treated with saline (pD2 of 1.54 ± 0.06; n = 7), but their E max values did not achieve significance (P > 0.05, ANOVA) neither to KCl (0.632 ± 0.014 g/mg of tissue in mesna-treated tissue vs. 0.489 ± 0.068 g/mg of tissue in control) nor to CCh (1.281 ± 0.058 g/mg of tissue in mesna-treated tissue vs. 1.048 ± 0.133 in control).
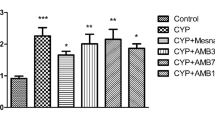
Determination of plasmatic levels of PGE2
After 24 h of IFS treatment, the animals with cystitis had PGE2 plasma concentrations of 1196.7 ± 197.1 ng/μg of total protein (n = 5; P < 0.05; Student-Newman-Keuls test), a 43% increase when compared with saline-treated animals (833.1 ± 49.8 ng/μg of total protein; n = 5). On the other hand, the animals treated with either indomethacin or etoricoxib 1 h before IFS administration and rats treated with mesna (80 mg/kg, 0, 4, and 8 h after IFS) exhibited lower plasma PGE2 levels (P < 0.05, Student-Newman-Keuls test, compared with animals treated with IFS only) with a 116, 62, and 67% decrease, respectively (P < 0.05). It is noteworthy that values seen in indomethacin-treated animals (560.2 ± 9.0 ng/μg of total protein; n = 5), but not values from etori- or mesna-treated rats, were significantly (P < 0.05, Student-Newman-Keuls test) different from results seen in samples of saline group.
Discussion
This present study shows that hemorrhagic cystitis induced experimentally by IFS promotes detrimental changes on motor functions of the rat lower urinary tract, which interferes with the urinary bladder emptying process in anesthetized rats, as well as alters its contractile behavior assessed by in vitro methods. We hypothesize that this phenomenon might involve inflammatory events mediated by COX-2 expression within urinary bladder with consequent rise in the plasmatic levels of PGE2. Selective inhibition of COX-2 activity may ameliorate, at least partially, these functional changes. Despite the relatively well-known functional consequences of the cyclophosphamide-induced effects on lower urinary tract, to the best of our knowledge, there is no study showing such changes associated with the use of IFS, especially in terms of micturition or smooth muscle physiology.
As we have shown, IFS causes inflammation in the urinary bladder, which was confirmed by the presence of edema, epithelial damage, and hemorrhage in the bladder tissue. Intense COX-2 expression within smooth muscle cells and increased levels of PGE2 were seen after treatment with IFS. In animals with cystitis, cystometrographic analysis revealed marked changes in bladder activity, with an increase in the filling bladder pressure and urinary incontinence. Cyclophosphamide, another alkylating agent also produces urinary changes as increased micturition frequency in awakened rats [14]. A key event observed in most of the IFS-treated animals was the lack of a typical bladder contraction that could be associated with micturition, which may be due to reduced muscle responsiveness to physiological stimuli involved in micturition reflex. Prostanoids, such as PGE2, may activate or sensitize bladder afferents, thereby changing the micturition reflex threshold through activation of capsaicin-sensitive bladder afferent nerves [15]. Also, if prostanoids are applied on the mucosal or serosal surface of the urinary bladder, they can stimulate the micturition reflex [16, 17]. This may be translated as uncontrolled activity of the detrusor smooth muscle stretched by a given filling volume beyond the threshold level to trigger micturition reflex, which causes increased intravesical pressure. Urine release occurred as intermittent dripping that showed observable and cyclic variations on its rate but without alterations that could be detectable in the trace recordings.
The present study corroborates early reports showing that the excitability of the urinary smooth muscle is changed, whether inflammation is present [18–20]. As seen herein, bladder strips from animals with inflamed bladder responded to either KCl or CCh with maximum force values that were lower than those observed in control tissues, indicating that cystitis-induced effects were mediated by a general decrement of the smooth muscle ability to produce contractile responses. Pharmacological potency of the contractile agents was differentially changed after inducing cystitis. While potency for KCl was diminished as seen through a decreased pD2 value compared to control group, a half maximum contractile response was reached with a concentration of CCh lesser than that obtained in tissues from saline-treated rats, which indicates increased potency for that muscarinic agonist. These results suggest that acute inflammation may modify urinary synaptic mechanisms, but such underlying mechanisms involved in the detrimental effects of ifosfamide deserve further investigations. As a matter of fact, it is well known that under experimental cyclophosphamide-induced cystitis, the cholinergic response of the urinary bladder was substantially affected, resulting in a decreased contractile response to KCl and CCh [21, 22].
Cyclooxygenase inhibition with indomethacin, a nonselective cyclooxygenase inhibitor [23], or etoricoxib, a selective COX-2 inhibitor [24], attenuated the effects induced by IFS in filling intravesical pressure values and recovered the maximum contractile responses of the isolated bladder smooth muscle, which were abolished in tissues of IFS-treated rats. Because changes observed on both urodynamic and contractility parameters were similarly altered in animals treated with either indomethacin or etoricoxib, we may conclude that functional alterations seen in IFS-treated animals require the induction of the enzyme COX-2.
Cystometrogram recordings from indomethacin- or etoricoxib-treated rats show that during the storage phase, increases of the bladder pressure were more notorious than in control animals, revealing that inflammatory process induced by IFS alters bladder compliance, and at least part of this phenomenon is physiologically regulated by the release of prostanoids. Indeed, augmented micturition frequency and pressure threshold was accompanied by an increase in the minimal intravesical pressure, which was also considered to be due to a reduction in bladder compliance [25]. Similarly, COX-2 inhibitors prevent or reverse the urodynamic changes associated with bladder inflammation induced by cyclophosphamide [19].
Additionally, our data are in accordance that the beneficial action of mesna was not restricted to prevention of the inflammatory process and its inhibition upon PGE2 levels in the plasma, but it also ameliorated contractile parameters of the rat urinary bladder strips in response to contractile agents, such as K+ and CCh. Pretreatment with mesna turns the bladder smooth muscle more responsive to KCl, but not to CCh, by a mechanism not determined in the present study. However, it is noteworthy that the increasing effect induced in vitro by mesna herein do not seem to influence motor behavior of the lower urinary tract in vivo, because animals treated with both mesna and IFS showed a functional profile similar to the animals treated with saline alone.
In conclusion, our data show that IFS induces hemorrhagic cystitis with pathophysiological implications on the motor behavior of the urinary bladder. Such changes in the responsiveness of the urinary smooth muscle seem to be mediated by multiple factors but clearly involve an increased expression of the enzyme COX-2. Finally, prevention of the inflammatory process ameliorates the consequences of the IFS-induced cystitis.
References
Higgs D, Nagy C, Einhorn LH (1989) Ifosfamide: a clinical review. Semin Oncol Nurs 5:70–77
Kaijser GP, Korst A, Beijnen JH, Bult A, Underberg WJ (1993) The analysis of ifosfamide and its metabolites. Anticancer Res 13:1311–1324
Kehrer JP, Biswal SS (2000) The molecular effects of acrolein. Toxicol Sci 57:6–15
Stillwell TJ, Benson RC (1988) Cyclophosphamide-induced hemorrhagic cystitis: a review of 100 patients. Cancer 61:451–457
Ribeiro RA, Freitas HC, Campos MC, Santos CC, Figueiredo FC, Brito GA, Cunha FQ (2002) Tumor necrosis factor-alpha and interleukin-1beta mediate the production of nitric oxide involved in the pathogenesis of ifosfamide induced hemorrhagic cystitis in mice. J Urol 167:2229–2234
Vieira MM, Brito GA, Belarmino-Filho JN, Macedo FY, Nery EA, Cunha FQ, Ribeiro RA (2003) Use of dexamethasone with mesna for the prevention of ifosfamide-induced hemorrhagic cystitis. Int J Urol 10:595–602
Batista CK, Mota JM, Souza ML, Leitão BT, Souza MH, Brito GA, Cunha FQ, Ribeiro RA (2007) Amifostine and glutathione prevent ifosfamide- and acrolein-induced hemorrhagic cystitis. Cancer Chemother Pharmacol 59:71–77
Macedo FY, Baltazar F, Almeida PR, Távora F, Ferreira FV, Schmitt FC, Brito GA, Ribeiro RA (2008) Cyclooxygenase-2 expression on ifosfamide-induced hemorrhagic cystitis in rats. J Cancer Res Clin Oncol 134:19–27
Macedo FY, Baltazar F, Mourao LC (2008) Induction of COX-2 expression by acrolein in the rat model of hemorrhagic cystitis. Exp Toxicol Pathol 59:425–430
Büyüknacar HS, Kumcu EK, Göçmen C, Onder S (2008) Effect of phosphodiesterase type 4 inhibitor rolipram on cyclophosphamide-induced cystitis in rats. Eur J Pharmacol 31:293–299
Chuang YC, Yoshimura N, Huang CC, Wu M, Chiang PH, Chancellor MB (2009) Intravesical botulinum toxin A administration inhibits COX-2 and EP4 expression and suppresses bladder hyperactivity in cyclophosphamide-induced cystitis in rats. Eur Urol 56:159–166
Bressan E, Tonussi CR (2008) Antiinflammatory effects of etoricoxib alone and combined with NSAIDs in LPS-induced reactive arthritis. Inflamm Res 57:586–592
Matsuura S, Downie JW (2000) Effect of anesthetics on reflex micturition in the chronic cannula-implanted rat. Neurourol Urodyn 19:87–99
Hu VY, Malley S, Dattilio A, Folsom JB, Zvara P, Vizzard MA (2003) COX-2 and prostanoid expression in micturition pathways after cyclophosphamide-induced cystitis in the rat. Am J Physiol Regul Integr Comp Physiol 284:R574–R585
Maggi CA (1992) Prostanoids as local modulators of reflex micturition. Pharmacol Res 25:13–20
Ishizuka O, Mattiasson A, Andersson KE (1995) Prostaglandin E2-induced bladder hyperactivity in normal, conscious rats: involvement of tachykinins? J Urol 153:2034–2038
Bultitude MI, Hills NH, Shuttleworth KED (1976) Clinical and experimental studies on the action of prostaglandins and their synthesis inhibitors on detrusor muscle in vitro and in vivo. Br J Urol 48:631–637
Yoshimura N, De Groat WC (1999) Increased excitability of afferent neurons innervating rat urinary bladder after chronic bladder inflammation. J Neurosci 19:4644–4653
Lecci A, Birder LA, Meini S, Catalioto RM, Tramontana M, Giuliani S, Criscuoli M, Maggi CA (2000) Pharmacological evaluation of the role of cyclooxygenase isoenzymes on the micturition reflex following experimental cystitis in rats. Br J Pharmacol 130:331–338
Lagos P, Ballejo G (2004) Role of spinal nitric oxide synthase-dependent processes in the initiation of the micturition hyperreflexia associated with cyclophosphamide-induced cystitis. Neuroscience 125:663–670
Mok MH, Knight GE, Andrews PL, Hoyle CH, Burnstock G (2000) The effects of cyclophosphamide on neurotransmission in the urinary bladder of Suncus murinus, the house musk shrew. J Auton Nerv Syst 80:130–136
Giglio D, Aronsson P, Eriksson L, Tobin G (2007) In vitro characterization of parasympathetic and sympathetic responses in cyclophosphamide-induced cystitis in the rat. Basic Clin Pharmacol Toxicol 100:96–108
Mitchell JA, Akarasereenont P, Thiemermann C, Flower RJ, Vane JR (1993) Selectivity of nonsteroidal antiinflammatory drugs as inhibitors of constitutive and inducible cyclooxygenase. Proc Natl Acad Sci USA 90:11693–11697
Riendeau D, Percival MD, Brideau C, Charleson S, Dubé D, Ethier D, Falgueyret JP, Friesen RW, Gordon R, Greig G, Guay J, Mancini J, Ouellet M, Wong E, Xu L, Boyce S, Visco D, Girard Y, Prasit P, Zamboni R, Rodger IW, Gresser M, Ford-Hutchinson AW, Young RN, Chan CC (2001) Etoricoxib (MK-0663): preclinical profile and comparison with other agents that selectively inhibit cyclooxygenase-2. J Pharmacol Exp Ther 296:558–566
Lecci A, Meini S, Patacchini R, Tramontana M, Giuliani S, Criscuoli M, Maggi CA (1999) Effect of dexamethasone on cyclophosphamide-induced cystitis in rats: lack of relation with bradykinin B1 receptor-mediated motor responses. Eur J Pharmacol 369:99–106
Acknowledgments
The authors gratefully acknowledge the technical assistance of Maria Silvandira Freire França and Antônio Haroldo Pinheiro Ferreira (Universidade Federal do Ceará, Fortaleza, CE, Brazil) and Giuliana B Francisco (FMRP–USP, Ribeirao Preto, SP, Brazil). This work was supported by CAPES and PRONEX/FUNCAP/CNPq.
Conflict of interest statement
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Macedo, F.Y.B., Mourão, L.T.C., Palheta, R.C. et al. Cyclooxygenase-2 contributes to functional changes seen on experimental hemorrhagic cystitis induced by ifosfamide in rat urinary bladder. Cancer Chemother Pharmacol 67, 935–943 (2011). https://doi.org/10.1007/s00280-010-1392-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-010-1392-z