Abstract
Purpose
Effects of genetic polymorphisms/variations of ABCB1, ABCC2, ABCG2 and SLCO1B1 in addition to “UGT1A1*28 or *6” on irinotecan pharmacokinetics/pharmacodynamics in Japanese cancer patients were investigated.
Methods
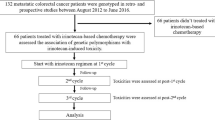
Associations between transporter haplotypes/variations along with UGT1A1*28 or *6 and SN-38 area under the time–concentration curve (AUC) or neutropenia were examined in irinotecan monotherapy (55 patients) and irinotecan–cisplatin-combination therapy (62 patients).
Results
Higher SN-38 AUC values were observed in ABCB1 2677G>T (A893S) (*2 group) for both regimens. Associations of grade 3/4 neutropenia were observed with ABCC2 −1774delG (*1A), ABCG2 421C>A (Q141K) and IVS12 + 49G>T (# IIB) and SLCO1B1 521T>C (V174A) (*15 · 17) in the irinotecan monotherapy, while they were evident only in homozygotes of ABCB1*2, ABCG2 # IIB, SLCO1B1*15 · 17 in the cisplatin-combination therapy. With combinations of haplotypes/variations of two or more genes, neutropenia incidence increased, but their prediction power for grade 3/4 neutropenia is still unsatisfactory.
Conclusions
Certain transporter genotypes additively increased irinotecan-induced neutropenia, but their clinical importance should be further elucidated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Irinotecan, an anticancer prodrug, is widely used for treating a broad range of carcinomas including colorectal and lung cancers. However, unexpected severe diarrhea and neutropenia are important clinical side effects from irinotecan treatment. The active metabolite SN-38 (7-ethyl-10-hydroxycamptothecin), a topoisomerase I inhibitor, is generated by hydrolysis of the parent compound by carboxylesterases [1], and is subsequently glucuronidated by uridine diphosphate glucuronosyltransferases (UGTs), such as UGT1A1, UGT1A7, and UGT1A9, to form an inactive metabolite, SN-38 glucuronide (SN-38G) [2–4]. Irinotecan is also inactivated by CYP3A4 to produce 7-ethyl-10-[4-N-(5-aminopentanoic acid)-1-piperidino]carbonyloxycamptothecin (APC) and 7-ethyl-10-(4-amino-1-piperidino)carbonyloxycamptothecin (NPC) [5]. Irinotecan and its metabolites are excreted into the bile and urine via the action of ATP-binding cassette (ABC) transporters, such as P-glycoprotein (P-gp/ABCB1), multiple resistance-associated protein 2 (MRP2/ABCC2), and breast cancer resistance protein (BCRP/ABCG2) [6]. Transport of SN-38 from the plasma into the liver is mediated by the organic anion transporting polypeptide C (OATP-C/SLCO1B1) [7]. Most of the previous pharmacogenetic studies on irinotecan have focused on UGT1A1 polymorphisms and have shown clinical relevance of UGT1A1*28, a repeat polymorphism in the TATA box [−54_−39A(TA)6TAA>A(TA)7TAA or −40_−39insTA], to severe toxicities [8–10]. Based on these findings, in 2005, the Food and Drug Administration (FDA) of the United States approved an amendment for the label of Camptosar (irinotecan HCl) (NDA 20-571/S-024/S-027/S-028) and the clinical use of a genetic diagnostic kit for the *28 allele. In parallel with this advance in the USA, clinical relevance to severe neutropenia of UGT1A1*6 [211G>A (G71R)], another low-activity allele detected specifically in East-Asians, as well as *28 was demonstrated in several studies on Asian patients [11–14]. Accordingly, in June 2008, the Ministry of Health, Labor and Welfare of Japan approved changes to irinotecan labels (Campto and Topotecin) by adding a caution for the risk of severe toxicities in patients either homozygous or compound heterozygous for UGT1A1*28 and *6 (*28/*28, *6/*6, *28/*6) and the clinical use of a diagnostic kit for UGT1A1*28 and *6. Severe toxicities, however, are found in patients without *6/*6, *28/*28, and *28/*6; therefore, other factors responsible for irinotecan toxicities should be identified.
Several clinical studies have suggested polymorphisms of the drug transporter genes, such as ABCB1, ABCC2, ABCG2, and SLCO1B1, might affect irinotecan pharmacokinetics (PK)/pharmacodynamics (PD) in Caucasian and Asian patients. However, the results obtained from different ethnic populations with various irinotencan regimens are still controversial, and the genetic markers examined also differ [13, 15–26]. We previously identified a number of haplotypes/variations of transporter genes, including ABCB1, ABCC2, ABCG2 and SLCO1B1 in Japanese [12, 26–29], but their clinical significance, either alone or in combination, in irinotecan therapy has not yet been examined.
This study aimed to identify the genetic polymorphisms/variations of ABCB1, ABCC2, ABCG2, and SLCO1B1 which can affect irinotecan PK/PD in Japanese cancer patients. We carefully stratified the patients considering the irinotecan regimen (irinotecan monotherapy or combination therapy with cisplatin) and UGT1A1 genotype (UGT1A1 *6 or *28), and examined additive effects of transporter haplotypes/variations on the area under the time–concentration curves (AUC) of the toxic metabolite SN-38 and on the risk of severe neutropenia.
Patients and methods
Patients
The patients used in this study were the same as those described in a previous paper [12], where details on the eligibility criteria for irinotecan therapy, patient profiles, and irinotecan regimens were described. In this study, 55 patients with irinotecan monotherapy (100 mg/m2 weekly or 150 mg/m2 biweekly) and 62 patients with combination therapy of irinotecan (60 mg/m2 weekly or 70 mg/m2 biweekly) and cisplatin (60 or 80 mg/m2, respectively) were included. This study was approved by the ethics committees of the National Cancer Center and the National Institute of Health Sciences, and written informed consent was obtained from all participants.
Analyses on genetic polymorphisms and PK/PD
Patients’ data on genetic variations and haplotypes of UGT1A1, ABCB1, ABCC2, ABCG2 and SLCO1B1 were previously obtained [12, 26–29]. Regarding ABCG2, combination haplotypes were newly defined using the previously reported haplotypes from three linkage disequilibrium (LD) blocks [28]. Patients’ PK data on the area under the concentration–time curve (AUC) and toxicities were previously obtained [12].
Association analyses
Associations of transporter genotypes with AUC/dose values for irinotecan, SN-38 and SN-38G, absolute neutrophil count (ANC) nadir, and incidence of grade 3 diarrhea or grade 3/4 neutropenia were investigated. For SN-38 AUC/dose and neutropenia, the patients were stratified by the presence of UGT1A1*6 or *28 (UGT+). Statistical significance (two-sided, P < 0.1) was determined by the Mann–Whitney (MW) test or Jonckheere–Terpstra (JT) test for AUC/dose, and by Fisher’s exact test and chi-square test (for trend) for incidence of grade 3 and 4 toxicities, using Prism version 4.0 (GraphPad Prism Software Inc., San Diego, CA, USA) and StatXact version 6.0 (Cytel Inc., Cambridge, MA). Multiplicity adjustment was not applied to bivariate analysis, and contributions of the candidate genetic markers to SN-38 AUC/dose values and ANC nadir were further determined by multiple regression analysis after logarithmic transformation of the AUC/dose values and ANC nadir counts. The variables examined were age, sex, body surface area, history of smoking or drinking, performance status, serum biochemistry (GOT, ALP, creatinine) at baseline, the ANC at baseline (for neutropenia), and genetic markers including UGT1A1*6 or *28 (UGT+) and the transporter haplotypes. The variables in the final models were selected by the forward and backward stepwise procedure at a significance level of 0.20 using JMP version 7.0.0 (SAS Institute Inc., Cary, NC, USA).
Results
Definition of major transporter haplotypes and their selected markers
For screening transporter gene polymorphisms affecting irinotecan PK/PD, major haplotypes and their tagging single nucleotide polymorphisms (SNPs) from ABCB1, ABCC2, ABCG2 and SLCO1B1 were selected (Table 1) according to their frequencies (more than 5%) and/or from preliminary results obtained from all patients treated with irinotecan.
For ABCB1 block 1[26], the haplotype group BJL, which consists of *1B (having −1789G>A), *1J (having −1789G>A and −371A>G) and *1L (having −1789G>A and −145C>G), was selected because an association of the marker SNP −1789G>A with lower expression levels of P-gp has been reported [30]. ABCB1 block 2 *2 was originally defined as haplotypes containing three SNPs, 1236C>T, 2677G>T (A893S) and 3435C>T [31]. Since the *9 haplotype with 1236C>T, 2677G>T (A893S) without 3435C>T [16] showed the same trend for PK/PD as *2 (data not shown), the current study classified the haplotypes with 2677G>T (A893S), *2, *9, *12 and *14 [26], as the *2 group (*2 in this paper). Similarly, the *10 group was classified as haplotypes with 2677G>A (A893T), i.e., *10 and *13, since no differences in PK/PD parameters were observed between these haplotypes. The *4, *6, and *8 haplotypes in block 2 [16, 26] showed no significant effect in the current analysis (data not shown). The ABCB1 block 3 *1b haplotype containing IVS27-182G>T was selected because our previous study showed it was associated with an increased renal clearance of SN-38 [16].
Based on reports showing possible functional alterations of −1774delG [32] and 3972C>T (I1324I) [18, 24], ABCC2 haplotypes containing those variations were classified as *1A and “*1C and *1G (*1C/G)”, respectively, according to our previous definition: *1A, −1774delG; *1C, −24C>T and 3972C>T; *1G, 3972C>T [27]. ABCC2*2 [1246G>A (V417I)] and *1H [2934G>A (S978S)] [27] showed no statistically significant effects (data not shown).
The ABCG2 combinatorial haplotypes were newly defined as combinations of haplotypes across the three blocks [block (−1)–block 1–block 2] previously reported [28]. Major combinations in 177 patients were the wild type # IA (frequency = 0.291), # IIB [containing 421C>A (Q141K) and IVS12 + 49G>T] (0.251) and # IIIC [containing 34G>A (V12M) and IVS9-30A>T] (0.107). Note that # IIB and # IIIC are subgroups of block 1 *2 [421C>A (Q141K)] and block 1*3 [34G>A (V12M)], respectively [28].
The SLCO1B1 haplotypes used were the major haplotypes *1b [containing 388A>G (N130D) without 521T>C (V174A)] [33] and *15 · 17 [containing 521T>C (V174A)], the functional relevance of which has been reported [34].
Association of transporter genotypes with AUC values
Since we previously found that some PK parameters, including AUC/dose, Cmax/dose and t 1/2 for irinotecan and/or its metabolites, as well as incidence of grade 3/4 toxicities were affected by irinotecan regimen [12], the following analyses were conducted using the two groups of patients; i.e., those treated with irinotecan monotherapy (100–150 mg/m2 for initial dosage) or by combination therapy with cisplatin (60–70 mg/m2 for initial dose of irinotecan). Since SN-38 AUC levels were largely dependent on the UGT1A1 genotype “*6 or *28” [12], the associations of transporter genotypes with SN-38 AUC values were analyzed within the groups stratified by the marker UGT1A1 “*6 or *28” (UGT+); i.e., UGT−/−, UGT+/− and UGT+/+. Since the SN-38 AUC/dose level of one patient with haplotypes ABCB1*2 [2677G>T (A893S)] and *14 [2677G>T (A893S) and 1345G>A (E448K)] showed an outlying value (indicated as “a” in Fig. 1), this patient was excluded from the statistical analysis. In this study, we preliminarily found that effect of each transporter genotype on irinotecan PK/PD was generally small. However, it was hypothesized that multiple transporter genotypes might act additively as described below. Accordingly, we adopted a statistical significance level of P = 0.1 (two-sided) to pick up candidate polymorphisms for further evaluation of their combined effects.
Effects of transporter genotypes on SN-38 AUC/dose in irinotecan monotherapy (N = 54). a Excluded from statistical analysis. The bars represent the medians. UGT+ = UGT1A1*6 or *28. a BJL contains −1789G>A, *2 (block 1) = 325G>A (E109K), *3 (block 1) = 304G>A (G102R); b *2 (block 2) contains 2677G>T (A893S); c *1b (block 3) = IVS27-182G>T, *2 (block 3) = 3751G>A (V1251I); d *1A contains −1774delG; e IIB contains 421C>A (Q141K) and IVS12 + 49G>T; f S = SLCO1B1*15 · 17 containing 521T>C (V174A)
Figure 1 shows the association of transporter genotypes with SN-38 AUC values in the irinotecan monotherapy. In all patients (ALL), higher values of the SN-38 AUC/dose were observed in the ABCB1*2/*2 [1.64-fold of −/−, P = 0.095 (MW test)] (Fig. 1b) and ABCG2 # IIB [1.24-fold of −/−, P = 0.078 (MW test)] genotypes (Fig. 1e) and lower values were observed in the ABCB1*1b (block 3) [0.78-fold of −/−, P = 0.008 (MW test)] (Fig. 1c) genotype. In UGT−/− patients, an increase in SN-38 AUC/dose was observed in the ABCB1 BJL [1.22-fold of −/−, P = 0.073 (MW test)] (Fig. 1a) and ABCG2 # IIB [1.21-fold of −/−, P = 0.082, (MW test)] genotypes (Fig. 1e). In UGT (+/− and +/+) patients, an increase in SN-38 AUC/dose in SLCO1B1*15 · 17 (S) [1.59-fold of −/−, P = 0.036 (MW test)] was also observed (Fig. 1f). Multiple regression analysis for the SN-38 AUC/dose (logarithm-transformed values) in the irinotecan monotherapy revealed significant associations of ABCB1*2/*2 (coefficient = 0.212 ± 0.075, P = 0.007), along with UGT+/− (0.113 ± 0.054, P = 0.040) and UGT+/+ (0.225 ± 0.088, P = 0.014) in the final model [R 2 = 0.226, Intercept = 0.281 (log 10−3h m2/L), N = 53].
Regarding other compounds, ABCB1*2/*2 also showed higher irinotecan AUC/dose (1.27-fold) [66.2 (48.2–82.4) [median (25th–75th percentiles)] for *2/*2 vs. 52.2 (40.6–61.9) for −/− and *2/−; P = 0.063 (MW test)] and SN-38G AUC/dose (1.62-fold) [18.0 (14.6–27.7) for *2/*2 vs. 11.1 (7.7–14.2) for −/− and *2/−; P = 0.002 (MW test)]. Conversely, lower irinotecan AUC/dose for ABCB1*10/*10 (0.79-fold) [54.8 (44.4–65.7) for −/− vs. 43.3 (40.6–54.1) for *10/*10; P = 0.062 (JT test)] was detected.
For the combination therapy with cisplatin, an increase of the SN-38 AUC/dose for ABCB1*2/*2 (1.43-fold) in non-UGT+/+ patients (UGT−/− and UGT+/−) (N = 55) [3.57 (2.72–4.19) for *2/*2 vs. 2.51 (1.99–3.28) for −/− and *2/−; P = 0.032 (MW test)], and a decrease for ABCB1*1b (0.80-fold) in UGT−/− patients (N = 35) [2.03 (1.72–2.33) for *1b/− and *1b/*1b vs. 2.55 (2.02–3.31) for −/−; P = 0.026 (MW test)] were observed. Multivariate analysis, however, showed no significant contributions of these transporter haplotypes to the SN-38 AUC/dose values.
Effects of transporter genotypes on toxicities in irinotecan monotherapy
Since 80 and 100% of UGT+/+ patients showed grade 3/4 neutropenia in the irinotecan monotherapy and combination therapy with cisplatin, respectively, neutropenia incidence was analyzed only in the non-UGT+/+ population. Two patients were excluded from the analysis; one patient who showed an outlier SN-38 value (indicated as “a” in Fig. 1) and a second patient from the cisplatin-combination therapy group who discontinued irinotecan therapy.
In terms of incidence of grade 3/4 neutropenia in irinotecan monotherapy (Table 2), ABCC2*1A-dependent increases [0, 25.8 and 50.0% for −/−, *1A/− and *1A/*1A, respectively; P = 0.014 (chi-square test for trend)] were observed in UGT (−/− and +/−) patients. Higher incidence with ABCG2 # IIB was also found in UGT (−/− and +/−) patients [9.5% for −/− and 35.3% for # IIB/− and # IIB/# IIB, respectively; P = 0.049 (Fisher’s exact test)], and with SLCO1B1*15 · 17(S) in the UGT+/− patients [15.0, 28.6 and 100% for −/−, S/− and S/S, respectively; P = 0.076 (chi-square test for trend)].
Multiple regression analysis for the ANC nadir (logarithm-transformed values) was conducted. The final model [R 2 = 0.466, Intercept = 1.088 (log counts/μL), N = 52] revealed associations of ABCC2*1A/*1A (coefficient = −0.339 ± 0.088, P = 0.0004), ABCG2 # IIB (−0.131 ± 0.067, P = 0.057) and SLCO1B1*15 · 17 (−0.136 ± 0.066, P = 0.046) in addition to UGT+/− (−0.134 ± 0.073, P = 0.074) and UGT+/+ (−0.238 ± 0.117, P = 0.047) and ANC at baseline (0.541 ± 0.226, P = 0.021), but association of ABCB1*2/*2 was not significant (−0.158 ± 0.095, P = 0.104).
Although total incidence of grade 3 diarrhea was low (11%), an ABCB1*2-dependent increase was observed [0, 15.4 and 28.6% for −/−, *2/− and *2/*2, respectively; P = 0.022 (chi-square test for trend)]. Note that all patients who experienced grade 3 diarrhea had neither the ABCC2*1C/G nor ABCG2 # IIIC genotypes.
Effects on toxicities in combination therapy with cisplatin
Since only four patients (6.0%) experienced grade 3 diarrhea from the cisplatin-combination therapy, association analysis for diarrhea was not done.
Grade 3/4 neutropenia incidence was higher with ABCB1*2 [47.1, 63.3 and 85.7% for −/−, *2/− and *2/*2, respectively; P = 0.073 (chi-square test for trend)] in UGT (−/− and +/−) patients. In UGT−/− patients, a higher incidence was also observed with ABCG2 # IIB [55.6, 83.3 and 100% for −/−, # IIB/− and # IIB/ # IIB, respectively; P = 0.075 (chi-square test for trend)]. Conversely, the incidence was lower with ABCG2 # IIIC [71.4% for −/−, and 25% for # IIIC/− and # IIIC/ # IIIC, respectively; P = 0.006 (Fisher’s exact test)] in UGT (−/− and +/−) patients. Notably, all patients homozygous for ABCG2 # IIB (N = 5) or SLCO1B1*15 · 17 (N = 1) experienced grade 3/4 neutropenia. The effect of ABCC2*1A on neutropenia was not consistent among the UGT genotypes in contrast to the results from the monotherapy. Multiple regression analysis was not applied to the neutropenia parameters in the cisplatin-combination therapy because, as described in the next section, contributions of minor variations could not be ignored.
Minor genetic variations possibly related to grade 4 neutropenia
We have detected a number of rare non-synonymous variations of the transporter genes to which statistical analysis could not be applied. Since grade 4 neutropenia occurred in non-UGT+/+ patients at rates of 8.0% (4/50) in the irinotecan monotherapy and 20% (11/55) in the cisplatin-combination therapy, we investigated possible contributions of these minor transporter variations and another low-activity UGT-haplotype, UGT1A1 # 60- # IB [35], to severe neutropenia.
Among the rare variations detected, eleven heterozygous transporter genetic variations and one UGT1A1 # 60- # IB homozygote were found in non-UGT+/+ patients who experienced grade 4 neutropenia (Table 3). These variations include an amino acid substitution leading to reduced in vitro activity, ABCG2 1465T>C (F489L) [36], and the stop codons, ABCG2 376C>T (Q126X) and 1723C>T (R575X) [28].
Additive effects of transporter gene haplotypes on neutropenia
Since multiple transporters are involved in irinotecan PK/PD, severity of toxicity might depend on the number and combinations of the low-activity variants, each of which does not effectively affect PD. To examine this possibility, we surveyed relationships between ANC nadirs and combinations of haplotypes associated with grade 3/4 neutropenia (P < 0.1) and the minor variations associated with grade 4 neutropenia (listed in the previous section); the data for selected haplotypes/variations are depicted in Fig. 2. For the combination therapy with cisplatin (Fig. 2b), homozygous SLCO1B1*15 · 17 was included, but ABCC2*1A was excluded since its effect in the cisplatin-combination therapy was not consistent among the UGT genotypes.
Additive effects of transporter haplotypes/variations on ANC nadirs in irinotecan monotherapy (a) and combination therapy with cisplatin (b). UGT+ = UGT1A1*6 or *28; B = ABCB1*2; C = ABCC2*1A; G = ABCG2 # IIB (open circle, # IIB/# IIB); S = SLCO1B1*15 · 17 (open square, *15 · 17/*15 · 17); b1–u1 = minor variations listed in Table 3. a None = non-(C, G, S or minors), b None = non-(B, G, S or minors). The bar in each genotype represents the median. The dotted lines in each UGT genotype show the median values of patients without any selected transporter polymorphisms/variations (None). The lines (G3 and G4) represent the border of grade 3 and 4 neutropenia
In the irinotecan monotherapy, ANC nadirs in most patients with either one or more of ABCG2 # IIB, SLCO1B1*15 · 17 and the minor variations were lower than the median ANC nadirs of both UGT−/− and UGT+/− patients without them (None) (Fig. 2a). In particular, the effects were more evident in patients bearing two or more of the selected haplotypes/variations (including the UGT+). Among the patients who experienced grade 3 or 4 neutropenia, 80% of patients had two or more candidate haplotypes/variations in the UGT (−/− and +/−) group (Fig. 2a).
In UGT+/− patients with the cisplatin-combination therapy, ANC nadirs of the patients with ABCB1*2/*2, ABCG2 # IIB/ # IIB, SLCO1B1*15 · 17/*15 · 17 or any minor variations, and their combinations were lower than the median values of patients without these markers (None), except for one patient with ABCB1*2/*2 and SLCO1B1*15 · 17 (B/B + S/−) (Fig. 2b). Also, in UGT−/− and UGT+/− patients, the effects were more evident in the patients with two or more of the selected haplotypes/variations. Among the patients who experienced grade 4 neutropenia, 82% of patients had two or more candidate haplotypes/variations in the UGT (−/− and +/−) group (Fig. 2b).
It was noted that the additive effect of g1 [ABCG2 376C>T (Q126X)] was not observed in the heterozygotes (g1/−), but was evident in the compound heterozygotes with another ABCG2 genetic polymorphism, # IIB, (G/g1) (Fig. 2a, b).
Regarding the combined effects of the above transporter genotypes on SN-38 AUC values, higher levels were observed in patients with the candidate haplotypes/variations of two or more genes in the monotherapy, but this trend was not always evident in the cisplatin-combination therapy patients (data not shown).
Discussion
In this study, we showed possible additive effects of transporter and UGT1A1 genotypes on irinotecan PK and PD. Since multiple transporters are involved in irinotecan PK, it is likely that a functional alteration of one of the responsible transporters can be compensated by other transporters; thus, changes in PK/PD parameters by transporter genotypes may not always be large. However, the overall elimination rate of irinotecan or its metabolites might be altered under the conditions of simultaneously reduced activities of multiple transporters, higher irinotecan doses, or reduced UGT activity.
In the irinotecan monotherapy, the increasing effect of ABCB1*2/*2 (block 2) on SN-38 AUC/dose was evident while contributions of ABCB1 BJL (block 1), ABCB1*1b (block 3), ABCG2 # IIB and SLCO1B1*15 · 17 were not significant in the multivariate analysis. For neutropenia, additive effects were suggested for ABCC2*1A/*1A, ABCG2 # IIB, SLCO1B1*15 · 17, and possibly some minor genetic variations in addition to UGT1A1*6 or *28 (Fig. 2a). The association of ABCB1*2 (block 2) with grade 3 diarrhea was also observed.
In the combination therapy with cisplatin, an increase in the SN-38 AUC/dose by ABCB1*2 and for a decrease by ABCB1*1b were observed, but the multivariate analysis did not show their significant contributions. Regarding neutropenia, additive effects of ABCB1*2/*2, ABCG2 # IIB/ # IIB, and possibly, SLCO1B1*15 · 17/*15 · 17 and some minor variations were suggested (Fig. 2b).
Thus, in both regimens, the associations of ABCB1*2 (block 2) with higher SN-38 AUC/dose levels and toxicities (diarrhea or neutropenia), and additive effects of ABCG2 # IIB and SLCO1B1*15 · 17 with UGT1A1*6 or *28 on neutropenia were observed. The current study also suggests that combination genotypes with two or more genes could have a greater effect on neutrophil count reduction than a single gene, indicating a quantitative property of multiple genetic factors affecting phenotype. These findings could partly explain a large interindividual variation in irinotecan toxicities within each UGT genotype.
In this study, influences of the transporter genotypes on SN-38 AUC/dose did not always correlate to an influence on neutropenia as observed in the combination therapy with cisplatin and in the case of ABCB1*2 (block 2) in the monotherapy. Although weak negative correlations were observed between the SN-38 AUC level and ANC nadir, the SN-38 AUC values of patients who exhibited grade 3/4 neutropenia (ANC nadir < 1,000 counts/μL) were fairly diverse, especially in the combination therapy with cisplatin (Fig. 3). It is likely that the extent of toxicities depends not only on systemic exposure levels of the active metabolite for which hepatic UGT activity is a large contributor, but also on the elimination from the target cells (neutrophil progenitor cells or enterocytes) where transporter function might be more critical.
Our previous study showed the association of ABCB1 block 2 *2 [1236C>T, 2677G>T (A893S) and 3435C>T] with lower renal clearance of irinotecan and its metabolites [16]. The current data obtained in the irinotecan monotherapy also suggest higher AUC/dose for irinotecan, SN-38G, and SN-38 with ABCB1*2/*2. Since a high affinity of P-gp for irinotecan is known, lower elimination rate of irinotecan could also result in higher plasma levels of its metabolites. Other studies have also suggested associations of the haplotype 1236T–2677T (corresponding to our *2 group in this study) with a reduced excretion rate of P-gp substrates [37] and SN-38 [25], and associations of the haplotype 2677T–3435T (corresponding to our *2 group in this study) with paclitaxel-induced neutropenia [38].
For ABCC2, ABCC2 −1774delG, a tagging SNP of *1A, was reported to be associated with low promoter activity and cholestatic or mixed-type hepatitis [32]. Patients with ABCC2*1A/*1A together with ABCB1*2/*2 or ABCG2 # IIB showed higher values of SN-38 AUC (Fig. 1) and neutropenia in the monotherapy (Fig. 2a), but these trends were not evident in the UGT−/− patients treated with cisplatin-combination therapy (data not shown). Thus, the effects of ABCC2 might be dependent on combinations with other genetic and non-genetic factors. Conflicting clinical outcomes of ABCC2 3972C>T, a marker of *1C/G, were reported to cause higher AUC of irinotecan and its metabolites in Caucasians treated with irinotecan monotherapy [18] and to lower the incidence of grade 3 diarrhea in Koreans treated with a combination therapy of irinotecan and cisplatin [24]. In the current study, no significant association of ABCC2*1C/G on PK/PD was observed in the monotherapy. Although a high incidence of grand 3/4 neutropenia was observed in patients with ABCC2*1C/G in the combination therapy with cisplatin, most patients also had ABCG2 # IIB (data not shown); thus, the effect of ABCC2*1C/G remains obscure.
For ABCG2, the current study examined the association with the combinatorial haplotypes consisting of the three previously defined block haplotypes [28]. ABCG2 # IIB contains the non-synonymous SNP 421C>A (Q141K), which was detected at higher frequencies in Asians and was reported to cause reduced expression of BCRP in vitro [36, 39–41]. In clinical studies, the association of 421C>A (Q141K) with higher plasma levels of diflomotecan was shown in Caucasians [42]. However, an association of this SNP with irinotecan PK/PD had not been shown [19, 24]. An association of 421C>A (Q141K) alone with irinotecan PK/PD was not significant in our hands (data not shown), but # IIB containing both 421C>A (Q141K) and IVS12 + 49G>T showed a moderate association with neutropenia. It is unclear whether the additional SNP IVS12 + 49G>T itself or another unknown linked SNP is causative for the reduced function. ABCG2 # IIIC contains a non-synonymous SNP 34G>A (V12M) which has no influence on BCRP expression or activity in vitro [36, 39–41]. Our study showed no influence of ABCG2 # IIIC on the SN-38 AUC/dose levels and neutropenia in the irinotecan monotherapy (data not shown), but did show a decreasing trend in grade 3/4 neutropenia in the combination therapy with cisplatin. In contrast, a report on Korean patients suggested the association of ABCG2 34G>A (V12M) with a higher incidence of grade 3 diarrhea in a combination therapy of irinotecan and cisplatin [24].
Among SLCO1B1 polymorphisms, 521T>C (V174A), a tagging SNP of *15 · 17, was demonstrated to reduce in vitro SN-38 influx [7], and clinical studies in Asians also showed its relevance to a higher SN-38 AUC and severe neutropenia in combination therapy of irinotecan with cisplatin [22–24]. Our results support these previous findings. Note that our *15 · 17 mainly consists of *17 [containing −11187G>A, 521T>C (V174A) and 388A>G (N130D)].
Taken together, the clinical data on transporter genotypes show variability among the studies. The reasons for these conflicting findings might be partly attributed to the ethnic differences in transporter genotypes and the regimens used. In addition, non-genetic factors, such as disease status and inflammation [43, 44], hepatic or renal function [45], and co-administered or pre-administered drugs, may also influence the clinical outcome.
The current study suggests combined effects of multiple haplotypes/variations on neutropenia. From clinical aspects of irinotecan therapy, the benefit of additional genotyping of transporters to predict severe toxicities should be clarified. Regarding grade 3 and 4 neutropenia, positive prediction values for two or more candidate genotypes including UGT (+) (Fig. 2) were 46 and 89% in the monotherapy and the cisplatin-combination therapy, respectively, which are low compared with UGT+/+ (80 and 100%, respectively). Regarding grade 4 neutropenia, positive predictive values for these candidate genotypes were 15 and 41% in the monotherapy and the cisplatin-combination therapy, respectively, while for UGT+/+, they were 0 and 43%, respectively. Further studies using a larger population size are needed to further elucidate the roles of these candidate markers.
In conclusion, the current study suggests there are additive effects for several transporter genotypes on the SN-38 AUC level and the reduction of neutrophil counts in irinotecan therapy. The clinical benefits of additional genotyping of these candidate markers should be further delineated.
References
Slatter JG, Su P, Sams JP, Schaaf LJ, Wienkers LC (1997) Bioactivation of the anticancer agent CPT-11 to SN-38 by human hepatic microsomal carboxylesterases and the in vitro assessment of potential drug interactions. Drug Metab Dispos 25:1157–1164
Iyer L, King CD, Whitington PF, Green MD, Roy SK, Tephly TR, Coffman BL, Ratain MJ (1998) Genetic predisposition to the metabolism of irinotecan (CPT-11). Role of uridine diphosphate glucuronosyltransferase isoform 1A1 in the glucuronidation of its active metabolite (SN-38) in human liver microsomes. J Clin Invest 15:847–854
Ciotti M, Basu N, Brangi M, Owens IS (1999) Glucuronidation of 7-ethyl-10-hydroxycamptothecin (SN-38) by the human UDP-glucuronosyltransferases encoded at the UGT1 locus. Biochem Biophys Res Commun 260:199–202
Gagne JF, Montminy V, Belanger P, Journault K, Gaucher G, Guillemette C (2002) Common human UGT1A polymorphisms and the altered metabolism of irinotecan active metabolite 7-ethyl-10-hydroxycamptothecin (SN-38). Mol Pharmacol 62:608–617
Haaz MC, Rivory L, Riché C, Vernillet L, Robert J (1998) Metabolism of irinotecan (CPT-11) by human hepatic microsomes: participation of cytochrome P-450 3A and drug interactions. Cancer Res 58:468–472
Sparreboom A, Danesi R, Ando Y, Chan J, Figg WD (2003) Pharmacogenomics of ABC transporters and its role in cancer chemotherapy. Drug Resist Updat 6:71–84
Nozawa T, Minami H, Sugiura S, Tsuji A, Tamai I (2005) Role of organic anion transporter OATP1B1 (OATP-C) in hepatic uptake of irinotecan and its active metabolite, 7-ethyl-10-hydroxycamptothecin: in vitro evidence and effect of single nucleotide polymorphisms. Drug Metab Dispos 33:434–439
Ando Y, Saka H, Ando M, Sawa T, Muro K, Ueoka H, Yokoyama A, Saitoh S, Shimokata K, Hasegawa Y (2000) Polymorphisms of UDP-glucuronosyltransferase gene and irinotecan toxicity: a pharmacogenetic analysis. Cancer Res 60:6921–6926
Iyer L, Das S, Janisch L, Wen M, Ramirez J, Karrison T, Fleming GF, Vokes EE, Schilsky RL, Ratain MJ (2002) UGT1A1*28 polymorphism as a determinant of irinotecan disposition and toxicity. Pharmacogenomics J 2:43–47
Innocenti F, Undevia SD, Iyer L, Chen PX, Das S, Kocherginsky M, Karrison T, Janisch L, Ramírez J, Rudin CM, Vokes EE, Ratain MJ (2004) Genetic variants in the UDP-glucuronosyltransferase 1A1 gene predict the risk of severe neutropenia of irinotecan. J Clin Oncol 22:1382–1388
Han JY, Lim HS, Shin ES, Yoo YK, Park YH, Lee JE, Jang IJ, Lee DH, Lee JS (2006) Comprehensive analysis of UGT1A polymorphisms predictive for pharmacokinetics and treatment outcome in patients with non-small-cell lung cancer treated with irinotecan and cisplatin. J Clin Oncol 24:2237–2244
Minami H, Sai K, Saeki M, Saito Y, Ozawa S, Suzuki K, Kaniwa N, Sawada J, Hamaguchi T, Yamamoto N, Shirao K, Yamada Y, Ohmatsu H, Kubota K, Yoshida T, Ohtsu A, Saijo N (2007) Irinotecan pharmacokinetics/pharmacodynamics and UGT1A genetic polymorphisms in Japanese: Roles of UGT1A1*6 and *28. Pharmacogenet Genomics 17:497–504
Jada SR, Lim R, Wong CI, Shu X, Lee SC, Zhou Q, Goh BC, Chowbay B (2007) Role of UGT1A1*6, UGT1A1*28 and ABCG2 c.421C>A polymorphisms in irinotecan-induced neutropenia in Asian cancer patients. Cancer Sci 98:1461–1467
Sai K, Saito Y, Sakamoto H, Shirao K, Kurose K, Saeki M, Ozawa S, Kaniwa N, Hirohashi S, Saijo N, Sawada J, Yoshida T (2008) Importance of UDP-glucuronosyltransferase 1A1*6 for irinotecan toxicities in Japanese cancer patients. Cancer Lett 261:165–171
Mathijssen RH, Marsh S, Karlsson MO, Xie R, Baker SD, Verweij J, Sparreboom A, McLeod HL (2003) Irinotecan pathway genotype analysis to predict pharmacokinetics. Clin Cancer Res 9:3246–3253
Sai K, Kaniwa N, Itoda M, Saito Y, Hasegawa R, Komamura K, Ueno K, Kamakura S, Kitakaze M, Shirao K, Minami H, Ohtsu A, Yoshida T, Saijo N, Kitamura Y, Kamatani N, Ozawa S, Sawada J (2003) Haplotype analysis of ABCB1/MDR1 blocks in a Japanese population reveals genotype-dependent renal clearance of irinotecan. Pharmacogenetics 13:741–757
Zhou Q, Sparreboom A, Tan EH, Cheung YB, Lee A, Poon D, Lee EJ, Chowbay B (2005) Pharmacogenetic profiling across the irinotecan pathway in Asian patients with cancer. Br J Clin Pharmacol 59:415–424
Innocenti F, Undevia SD, Chen PX, Das S, Ramirez J, Dolan ME, Relling MV, Kroetz DL, Ratain MJ (2004) Pharmacogenetic analysis of interindividual irinotecan (CPT-11) pharmacokinetic (PK) variability: evidence for a functional variant of ABCC2. In: 2004 ASCO annual meeting proceedings (post-meeting edition), vol 22, No 14S, abstract no: 2010
de Jong FA, Marsh S, Mathijssen RH, King C, Verweij J, Sparreboom A, McLeod HL (2004) ABCG2 pharmacogenetics: ethnic differences in allele frequency and assessment of influence on irinotecan disposition. Clin Cancer Res 10:5889–5894
de Jong FA, Scott-Horton TJ, Kroetz DL, McLeod H, Friberg LE, Mathijssen RH, Verweij J, Marsh S, Sparreboom A (2007) Irinotecan-induced diarrhea: functional significance of the polymorphic ABCC2 transporter protein. Clin Pharmacol Ther 81:42–49
Xiang X, Jada SR, Li HH, Fan L, Tham LS, Wong CI, Lee SC, Lim R, Zhou QY, Goh BC, Tan EH, Chowbay B (2006) Pharmacogenetics of SLCO1B1 gene and the impact of *1b and *15 haplotypes on irinotecan disposition in Asian cancer patients. Pharmacogenet Genomics 16:683–691
Takane H, Miyata M, Burioka N, Kurai J, Fukuoka Y, Suyama H, Shigeoka Y, Otsubo K, Ieiri I, Shimizu E (2007) Severe toxicities after irinotecan-based chemotherapy in a patient with lung cancer: a homozygote for the SLCO1B1*15 allele. Ther Drug Monit 29:666–668
Han JY, Lim HS, Shin ES, Yoo YK, Park YH, Lee JE, Kim HT, Lee JS (2008) Influence of the organic anion-transporting polypeptide 1B1 (OATP1B1) polymorphisms on irinotecan-pharmacokinetics and clinical outcome of patients with advanced non-small cell lung cancer. Lung Cancer 59:69–75
Han JY, Lim HS, Park YH, Lee SY, Lee JS (2009) Integrated pharmacogenetic prediction of irinotecan pharmacokinetics and toxicity in patients with advanced non-small cell lung cancer. Lung Cancer 63:115–120
Michael M, Thompson M, Hicks RJ, Mitchell PL, Ellis A, Milner AD, Di Iulio J, Scott AM, Gurtler V, Hoskins JM, Clarke SJ, Tebbut NC, Foo K, Jefford M, Zalcberg JR (2006) Relationship of hepatic functional imaging to irinotecan pharmacokinetics and genetic parameters of drug elimination. J Clin Oncol 24:4228–4235
Sai K, Itoda M, Saito Y, Kurose K, Katori N, Kaniwa N, Komamura K, Kotake T, Morishita H, Tomoike H, Kamakura S, Kitakaze M, Tamura T, Yamamoto N, Kunitoh H, Yamada Y, Ohe Y, Shimada Y, Shirao K, Minami H, Ohtsu A, Yoshida T, Saijo N, Kamatani N, Ozawa S, Sawada J (2006) Genetic variations and haplotype structures of the ABCB1 gene in a Japanese population: an expanded haplotype block covering the distal promoter region, and associated ethnic differences. Ann Hum Genet 70:605–622
Sai K, Saito Y, Itoda M, Fukushima-Uesaka H, Nishimaki-Mogami T, Ozawa S, Maekawa K, Kurose K, Kaniwa N, Kawamoto M, Kamatani N, Shirao K, Hamaguchi T, Yamamoto N, Kunitoh H, Ohe Y, Yamada Y, Tamura T, Yoshida T, Minami H, Matsumura Y, Ohtsu A, Saijo N, Sawada J (2008) Genetic variations and haplotypes of ABCC2 encoding MRP2 in a Japanese population. Drug Metab Pharmacokinet 23:139–147
Maekawa K, Itoda M, Sai K, Saito Y, Kaniwa N, Shirao K, Hamaguchi T, Kunitoh H, Yamamoto N, Tamura T, Minami H, Kubota K, Ohtsu A, Yoshida T, Saijo N, Kamatani N, Ozawa S, Sawada J (2006) Genetic variation and haplotype structure of the ABC transporter gene ABCG2 in a Japanese population. Drug Metab Pharmacokinet 21:109–121
Kim SR, Saito Y, Sai K, Kurose K, Maekawa K, Kaniwa N, Ozawa S, Kamatani N, Shirao K, Yamamoto N, Hamaguchi T, Kunitoh H, Ohe Y, Yamada Y, Tamura T, Yoshida T, Minami H, Ohtsu A, Saijo N, Sawada J (2007) Genetic variations and frequencies of major haplotypes in SLCO1B1 encoding the transporter OATP1B1 in Japanese subjects: SLCO1B1*17 is more prevalent than *15. Drug Metab Pharmacokinet 22:456–461
Takane H, Kobayashi D, Hirota T, Kigawa J, Terakawa N, Otsubo K, Ieiri I (2004) Haplotype-oriented genetic analysis and functional assessment of promoter variants in the MDR1 (ABCB1) gene. J Pharmacol Exp Ther 311:1179–1187
Kim RB, Leake BF, Choo EF, Dresser GK, Kubba SV, Schwarz UI, Taylor A, Xie HG, McKinsey J, Zhou S, Lan LB, Schuetz JD, Schuetz EG, Wilkinson GR (2001) Identification of functionally variant MDR1 alleles among European Americans and African Americans. Clin Pharmacol Ther 70:189–199
Choi JH, Ahn BM, Yi J, Lee JH, Lee JH, Nam SW, Chon CY, Han KH, Ahn SH, Jang IJ, Cho JY, Suh Y, Cho MO, Lee JE, Kim KH, Lee MG (2007) MRP2 haplotypes confer differential susceptibility to toxic liver injury. Pharmacogenet Genomics 17:403–415
Tirona RG, Leake BF, Merino G, Kim RB (2001) Polymorphisms in OATP-C: identification of multiple allelic variants associated with altered transport activity among European- and African-Americans. J Biol Chem 276:35669–35675
Niemi M, Schaeffeler E, Lang T, Fromm MF, Neuvonen M, Kyrklund C, Backman JT, Kerb R, Schwab M, Neuvonen PJ, Eichelbaum M, Kivistö KT (2004) High plasma pravastatin concentrations are associated with single nucleotide polymorphisms and haplotypes of organic anion transporting polypeptide-C (OATP-C, SLCO1B1). Pharmacogenetics 14:429–440
Saeki M, Saito Y, Sai K, Maekawa K, Kaniwa N, Sawada J, Kawamoto M, Saito A, Kamatani N (2007) A combinatorial haplotype of the UDP-glucuronosyltransferase 1A1 gene (#60-#IB) increases total bilirubin concentrations in Japanese volunteers. Clin Chem 53:356–358
Tamura A, Wakabayashi K, Onishi Y, Takeda M, Ikegami Y, Sawada S, Tsuji M, Matsuda Y, Ishikawa T (2007) Re-evaluation and functional classification of non-synonymous single nucleotide polymorphisms of the human ATP-binding cassette transporter ABCG2. Cancer Sci 98:231–239
Wong M, Evans S, Rivory LP, Hoskins JM, Mann GJ, Farlow D, Clarke CL, Balleine RL, Gurney H (2005) Hepatic technetium Tc 99m-labeled sestamibi elimination rate and ABCB1 (MDR1) genotype as indicators of ABCB1 (P-glycoprotein) activity in patients with cancer. Clin Pharmacol Ther 77:33–42
Sissung TM, Mross K, Steinberg SM, Behringer D, Figg WD, Sparreboom A, Mielke S (2006) Association of ABCB1 genotypes with paclitaxel-mediated peripheral neuropathy and neutropenia. Eur J Cancer 42:2893–2896
Imai Y, Nakane M, Kage K, Tsukahara S, Ishikawa E, Tsuruo T, Miki Y, Sugimoto Y (2002) C421A polymorphism in the human breast cancer resistance protein gene is associated with low expression of Q141K protein and low-level drug resistance. Mol Cancer Ther 1:611–616
Kondo C, Suzuki H, Itoda M, Ozawa S, Sawada J, Kobayashi D, Ieiri I, Mine K, Ohtsubo K, Sugiyama Y (2004) Functional analysis of SNPs variants of BCRP/ABCG2. Pharm Res 21:1895–1903
Mizuarai S, Aozasa N, Kotani H (2004) Single nucleotide polymorphisms result in impaired membrane localization and reduced ATPase activity in multidrug transporter ABCG2. Int J Cancer 109:238–246
Sparreboom A, Gelderblom H, Marsh S, Ahluwalia R, Obach R, Principe P, Twelves C, Verweij J, McLeod HL (2004) Diflomotecan pharmacokinetics in relation to ABCG2 421C>A genotype. Clin Pharmacol Ther 76:38–44
Teng S, Piquette-Miller M (2008) Regulation of transporters by nuclear hormone receptors: implications during inflammation. Mol Pharm 5:67–76
Englund G, Jacobson A, Rorsman F, Artursson P, Kindmark A, Rönnblom A (2007) Efflux transporters in ulcerative colitis: decreased expression of BCRP (ABCG2) and Pgp (ABCB1). Inflamm Bowel Dis 13:291–297
de Jong F, van der Bol J, Mathijssen R, van Gelder T, Wiemer E, Sparreboom A, Verweij J (2008) Renal function as a predictor of irinotecan-induced neutropenia. Clin Pharmacol Ther 84:254–262
Acknowledgments
This study was supported in part by the Program for the Promotion of Fundamental Studies in Health Sciences of the National Institute of Biomedical Innovation, and by the Program for the Promotion of Studies in Health Sciences of the Ministry of Health, Labor and Welfare of Japan. We thank Yakult Honsha Co., Ltd (Tokyo, Japan) for providing analytical standards of irinotecan and its metabolites. We also thank Ms. Chie Sudo for her administrative assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sai, K., Saito, Y., Maekawa, K. et al. Additive effects of drug transporter genetic polymorphisms on irinotecan pharmacokinetics/pharmacodynamics in Japanese cancer patients. Cancer Chemother Pharmacol 66, 95–105 (2010). https://doi.org/10.1007/s00280-009-1138-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-009-1138-y