Abstract
Purpose
Clofarabine increases the activation of 1-β-d-arabinofuranosyl cytosine (araC) in tumor cells, and combination of these two drugs has been shown to result in good clinical activity against various hematologic malignancies. 1-β-d-[4-thio-arabinofuranosyl] cytosine (T-araC) is a new cytosine analog that has exhibited excellent activity against a broad spectrum of human solid tumors and leukemia/lymphoma xenografts in mice and is currently being evaluated in patients as a new drug for the treatment of cancer. Since T-araC has a vastly superior preclinical efficacy profile in comparison to araC, we have initiated studies to determine the potential value of clofarabine/T-araC combination therapy.
Methods
In vitro studies have been conducted to determine the effect of clofarabine on the metabolism of T-araC, and in vivo studies have been conducted to determine the effect of the clofarabine/T-araC combination on five human tumor xenografts in mice.
Results
Initial studies with various tumor cells in culture indicated that a 2-h incubation with clofarabine enhanced the metabolism of T-araC 24 h after its removal by threefold in three tumor cell types (HCT-116 colon, K562 leukemia, and RL lymphoma) and by 1.5-fold in two other tumor cell types (MDA-MB-435 breast (melanoma), and HL-60 leukemia). Pretreatment with clofarabine resulted in a slight decrease in metabolism of T-araC in RPMI-8226 myeloma cells (65% of control) and inhibited metabolism of T-araC in CCRF-CEM leukemia cells by 90%. In vivo combination studies were conducted with various human tumor xenografts to determine whether or not the modulations observed in vitro were reflective of the in vivo situation. Clofarabine and T-araC were administered on alternate days for five treatments each (q2dx5) with the administration of T-araC 24 h after each clofarabine treatment. Combination treatment of HCT-116, K562, HL-60, or RL tumors with clofarabine and T-araC resulted in dramatically superior anti-tumor activity than treatment with either agent alone, whereas this combination resulted in antagonism in CCRF-CEM tumors. The in vivo antitumor activity of clofarabine plus T-araC against HCT-116 tumors was much better than the activity seen with clofarabine plus araC.
Conclusions
These studies provide a rationale for clinical trials using this combination in the treatment of acute leukemias as well as solid tumors and suggest that this combination would exhibit greater antitumor activity than that of clofarabine plus araC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Clofarabine (Fig. 1) is a deoxyadenosine analog that was recently approved by the FDA for use in the treatment of relapsed and refractory pediatric acute lymphoblastic leukemia [1–3]. It has also demonstrated excellent activity against adult acute leukemias. In vitro studies have shown that pretreatment with clofarabine can enhance the accumulation of the 5′ triphosphate of arabinofuranosyl cytosine (araC, Fig. 1) in K562 leukemia cells [4], and clinical trials have indicated that the combination of clofarabine and araC results in good antitumor activity [5, 6]. These investigators concluded that the combination of clofarabine and araC is active in the treatment of relapsed/refractory hematologic malignancies, with an acceptable safety profile. However, the duration of remission and overall survival did not appear to be improved compared to experience with other regimens. In addition the combination of clofarabine plus araC has recently been shown to induce remission in a multiple relapsed pediatric leukemia patient [7].
1-β-d-[4-thio-arabinofuranosyl]-cytosine (T-araC, Fig. 1) is a new agent that has excellent activity against numerous solid tumor xenografts in mice [8, 9]. Although T-araC is structurally similar to araC, the antitumor activity of T-araC against a variety of human tumor xenografts in mice is dramatically better than that of araC, a compound that does not demonstrate solid tumor activity in these animal models or in patients. T-araC has also demonstrated better activity than gemcitabine against various human tumor xenografts in mice [10]. In addition to its activity against solid tumors, T-araC is also very active against numerous human leukemia and lymphoma xenografts in mice [10]. Although the basic mechanism of action of T-araC [11–14] is similar to that of araC [both compounds are phosphorylated to their respective triphosphates (T-araCTP and araCTP), which inhibit DNA synthesis], there are several quantitative differences in the metabolism and biochemical activity of these two compounds that can explain their differences in antitumor activity [15–17]. Most importantly, the half-life of T-araCTP in solid tumor cells is approximately ten times longer than that of araCTP [15]. In addition, T-araCTP is a much more potent inhibitor of DNA synthesis than is araCTP [11]. These preclinical results suggest that T-araC may be superior to araC as an antitumor agent against both solid tumors and hematologic malignancies.
T-araC has been evaluated in two clinical trials to treat solid tumors [18, 19] and is currently being prepared for further clinical evaluation. Because of the demonstrated clinical activity of clofarabine plus araC and the superior preclinical antitumor activity of T-araC, we have conducted in vitro and in vivo experiments to evaluate the effectiveness of combining clofarabine with T-araC. Our results indicate that this combination resulted in excellent tumor cell kill due at least in part to the enhancement of T-araC metabolism in tumor cells. Since T-araC has a superior preclinical efficacy profile in comparison to araC in mouse models of cancer, these studies provide a rationale to evaluate this combination in clinical trials in the treatment of acute leukemias and other cancers.
Materials and methods
Cell culture
CCRF-CEM (human lymphocytic leukemia), K562 (human myelogenous leukemia), HCT-116 (human colon cancer), RPMI-8226 (human myeloma), and RL (human lymphoma) cells were purchased from American Type Culture Collection (Rockville, MD). MDA-MB-435 [human breast (melanoma) cancer] and HL-60 (human leukemia) cells were obtained from the Developmental Therapeutics Program Tumor Repository (Frederick, MD). All of these cell lines were grown in RPMI 1640 medium (Gibco-BRL, Gaithersburg, MD) containing 10% fetal bovine serum (Gibco-BRL), 10 U/ml penicillin, 10 μg/ml streptomycin, and 50 μg/ml gentamycin.
Measurement of the metabolism of T-araC
Cells were incubated with clofarabine and [3H]T-araC as indicated in Fig. 2 and Table 1. After treatment with T-araC 10 ml of the suspension cultures (CCRF-CEM, K562, HL-60, RPMI-8226, and RL cells, approximately 5 × 105 cells/ml) were collected by centrifugation and washed three times with culture medium to remove the compounds. Cell numbers of suspension cultures were determined with a Coulter Counter. HCT-116 and MDA-MB-435 cells were grown to near confluency in T75 flasks. After treatment with T-araC the cells were washed with fresh medium and removed from the flask with trypsin. The total protein was determined as a measure of the number of cells. The cell pellets were treated with ice-cold 0.5 M PCA, the acid-precipitable material was removed by centrifugation, and the supernatant was neutralized with KOH and buffered with KPO4 buffer (pH 7.4). The amount of [3H]T-araCTP in the acid-soluble extract was measured using anion exchange HPLC as previously described [11] and was normalized by cell number (suspension cells) or protein (monolayer cells). All experiments were performed in healthy cell cultures that were in logarithmic growth phase.
Effect of clofarabine (Cl-F-araA) on the metabolism of T-araC in K562 cells. K562 cells were treated with 1 μM of clofarabine for 2 h. The cells were washed free of clofarabine and incubated in drug-free medium. [3H]T-araC (10 μM) was added to the medium at various times after removal of clofarabine. One hour after the addition of T-araC the amount of [3H]T-araCTP in the cells was determined. The results are the mean ± SD of two determinations
In vivo antitumor evaluations
Tumor fragments (30–40 mg from an in vivo passage) or ascites cells (107 cells from an in vivo HL-60 passage) were implanted sc into the flanks of scid mice (RL, CCRF-CEM, K562, and HL-60) or NCr-nu (HCT-116) athymic mice. The resulting tumors were measured twice weekly with electronic calipers and an estimate of the weight was calculated using the equation [(Length × Width2)/2 = mm3], which is converted to mg assuming unit density [20]. Drug treatment began when tumors were approximately 200 mg. Clofarabine and T-araC were administered (ip) once daily every other day for five treatments. AraC was administered (ip) three times daily (4 h between injections) every other day for five days. In mice that were treated with clofarabine plus either T-araC or araC, clofarabine was administered first followed by T-araC (or araC) 24 h later, and the second dose of clofarabine was administered 24 h after the first dose of T-araC (or araC), and so on for a total of five daily treatments for each drug. All treatments listed in the tables and figures were tolerated. Tumor-free survivors are the number of mice without tumors at the end of the experiment divided by the total number of mice in each treatment group. Days to two doublings is the mean time that the tumors took to double twice in size and does not include tumors that completely regressed. T-C (tumor growth delay) is the difference in days to two doublings between drug-treated and saline-treated groups. In the figures the median tumor weight is only shown for time points in which no mice have been removed from the study because of large tumors. All procedures were performed in accordance with a protocol that was approved by the IACUC of Southern Research Institute.
Results
Effect of clofarabine on the metabolism of T-araC in tumor cells in culture
Incubation of K562 cells with 1 μM clofarabine for 1, 2, 4, or 6 h inhibited the metabolism of 10 μM 3H-T-araC by about 50% (data not shown). The dose of clofarabine used in the in vitro studies was the plasma concentration that is achieved in patients treated with clofarabine at the maximally tolerated dose in adult patients [4, 21]. In this experiment clofarabine was not removed from the medium prior to analysis of T-araC metabolism. Under similar conditions clofarabine stimulated the metabolism of 10 μM araC by about 70%, which was similar to results obtained by Cooper et al. [4]. When clofarabine was removed from the cell culture prior to the addition of T-araC, treatment with clofarabine stimulated the phosphorylation of T-araC. The results in Fig. 2 indicated that a 2-h incubation with clofarabine at 1 μM resulted in a three- to five-fold increase in the metabolism of 10 μM T-araC 24 h after the removal of clofarabine. A 2-h incubation with clofarabine also stimulated the metabolism of 0.1 and 1 μM T-araC 24 h after the removal of clofarabine (data not shown). Treatment of K562 cells with 1 μM clofarabine for 2 h had a significant effect on subsequent cell growth shown in Fig. 2, which indicated that this dose and schedule of clofarabine was cytotoxic to these cells. Clofarabine had a similar effect on the metabolism of araC in K562 cells. The deoxycytidine (dCyd) kinase activity in K562 cell-free extracts prepared 24 h after a 2-h incubation with clofarabine was increased from 103 ± 11 (in nontreated cells) to 289 ± 60 pmoles/mg-min (N = 3).
The effect of clofarabine on the metabolism of T-araC was also evaluated in other cell types to determine how many tumor types might be sensitive to this combination (Table 1). Clofarabine stimulated the metabolism of T-araC by about three-fold in HCT-116, K562, and RL tumor cells; it had a small positive effect on the metabolism of T-araC in HL-60 and MDA-MB-435 tumor cells; and it inhibited the metabolism of T-araC in RPMI-8226 and CCRF-CEM tumor cells. These results indicated that the effect of clofarabine on the metabolism of T-araC was not uniform, but that clofarabine had a positive effect on the metabolism of T-araC in five of seven cell types.
Effect of clofarabine on the antitumor activity of T-araC against human tumor xenografts in mice
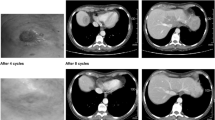
We first evaluated the clofarabine/T-araC combination on HCT-116 colon tumors (Fig. 3, Table 2). Previous work demonstrated that optimal biochemical modulation occurs with the sequential addition of clofarabine followed 4 h later with araC [4]. Our results indicated that optimal enhancement of T-araC metabolism occurred 24 h after treatment with clofarabine. Therefore, we chose to treat mice with clofarabine followed 24 h later by T-araC for five rounds of treatment. The maximally tolerated dosages (MTD) of clofarabine and T-araC when administered as single agents were 100 and 160 mg/kg/dose (q2dx5), respectively. The effect of clofarabine on araC antitumor activity was also evaluated in this experiment, but the optimal schedule of araC in mice is to administer it three times daily instead of once daily. The MTD of araC administered three times a day every other day for 5 days was 30 mg/kg/dose. Treatment with either clofarabine or araC alone did not result in any antitumor activity against HCT-116 xenografts, whereas treatment with T-araC alone (160 mg/kg/dose) demonstrated a good delay in tumor growth (T-C value of 35 days), but did not result in any tumor-free survivors.
Effect of clofarabine plus T-araC on HCT-116 colon tumors. Mice bearing HCT-116 colon tumor xenografts were treated ip with clofarabine, T-araC, araC, clofarabine plus T-araC, or clofarabine plus araC as described in the legend to Table 2. Tumor size was measured twice weekly with calipers for 10 weeks after initiation of therapy. There were six mice per treatment group, except for the vehicle-treated control group (12 mice). The T-araC component of this experiment has been repeated once with similar results. The time for the size of each tumor to double twice was calculated and the mean ± SD are shown in the figure for each treatment group, except for mice treated with 50 mg/kg clofarabine plus 80 mg/kg T-araC, where there were four tumor-free survivors. In this treatment group the sizes of the two tumors at the end of the experiment (90 days post implant) were 198 and 2,925 mg
Treatment of mice bearing HCT-116 tumors with alternating dosages of 50 mg/kg/dose clofarabine and 80 mg/kg/dose T-araC (separated by 24 h) for five rounds of treatment (the maximally tolerated doses when combined) resulted in a dramatic enhancement of antitumor activity with four of six tumor-free survivors. Even when the doses were reduced to 12.5 mg/kg/dose of clofarabine followed by 20 mg/kg/dose of T-araC, there were still two of six tumor-free survivors with a T-C value of 37 days in the four remaining mice, which was comparable to that seen after treatment with 160 mg/kg/dose of T-araC, which is the highest tolerated dosages when administered alone. Even though combination of clofarabine plus araC resulted in better antitumor activity than treatment with either agent alone, only modest antitumor activity was observed with this combination (no tumor-free survivors, T-C value of 18 days).
Excellent antitumor activity was also observed with the clofarabine/T-araC combination against human K562 leukemia, HL-60 leukemia, and RL lymphoma xenografts (Figs. 4, 5, Table 3). Treatment of mice bearing K562 leukemia with clofarabine (25 mg/kg/dose) plus T-araC (40 mg/kg/dose) resulted in five of six tumor-free survivors (Fig. 4), which was much better than that seen with either agent alone at the same dosages. Treatment with clofarabine (25 mg/kg/dose) resulted in a T-C value of 15 days, and for T-araC (40 mg/kg/dose), the T-C value was 38 days, but there were no tumor-free survivors with either compound. The antitumor activity of the clofarabine/T-araC combination was also better than treatment with either clofarabine at 100 mg/kg/dose (T-C value of 28 days, 1/6 tumor-free survivors) and was similar to treatment with T-araC at 160 mg/kg/dose (T-C value of 57 days, 3/6 tumor-free survivors). Treatment of mice bearing HL-60 leukemia with clofarabine (25 mg/kg/dose) plus T-araC (40 mg/kg/dose) also resulted in five of six tumor-free survivors (Fig. 5), whereas there were no tumor-free survivors in mice treated with either clofarabine at 25 mg/kg/dose (T-C value of 5 days) or T-araC at 40 mg/kg/dose (T-C value of 12 days). Higher dosages of clofarabine and T-araC were not evaluated in this experiment, because it is known that HL-60 tumors are very sensitive to these two agents. Both clofarabine and T-araC are curative against this tumor xenograft [10]. A similar enhancement of antitumor activity was seen by the combination in mice bearing the RL lymphoma (Table 3). As observed with the HCT-116 tumor, combination of even low dosages of clofarabine and T-araC resulted in better antitumor activity than could be achieved with either agent alone (at higher dosages).
Effect of clofarabine plus T-araC on K562 leukemia. K562 leukemia fragments were implanted sc into the flanks of scid mice. When tumors were approximately 200 mg, mice were treated ip with saline, clofarabine (25 mg/kg/dose, Q2Dx5 starting on day 10), T-araC (40 mg/kg/dose, Q2Dx5 starting on day 11), or clofarabine (25 mg/kg/dose, Q2Dx5 starting on day 10) plus T-araC (40 mg/kg/dose, Q2Dx5 starting on day 11). The tumors were measured twice weekly with calipers after initiation of treatment and the weight was calculated as described. There were six mice per treatment group, except for the vehicle-treated control group (12 mice). The time for the size of each tumor to double twice was calculated and the mean ± standard deviations are shown in the figure for each treatment group, except for mice treated with 25 mg/kg clofarabine plus 40 mg/kg T-araC, where there were five tumor-free survivors. In this treatment group the size of the one tumor at the end of the experiment (118 days post implant) was 2,176 mg
Effect of clofarabine plus T-araC on HL-60 leukemia. HL-60 leukemia ascites cells (1 × 107 cells) were injected sc into the flanks of scid mice. When tumors were approximately 200 mg, mice were treated ip with saline, clofarabine (25 mg/kg/dose, Q2Dx5 starting on day 10), T-araC (40 mg/kg/dose, Q2Dx5 starting on day 11), or clofarabine (25 mg/kg/dose, Q2D5 starting on day 10) plus T-araC (40 mg/kg/dose, Q2Dx5 starting on day 11). The tumors were measured twice weekly with calipers after initiation of treatment and the weight was calculated as described. There were six mice per treatment group, except for the vehicle-treated control group (ten mice). The time for the size of each tumor to double twice was calculated and the mean ± SD are shown in the figure for each treatment group, except for mice treated with 25 mg/kg clofarabine plus 40 mg/kg T-araC, where there were five tumor-free survivors. In this treatment group the size of the one tumor at the end of the experiment was 2,890 mg (51 days post implant). Note that the HL-60 tumor is a very aggressive tumor in scid mice, and that seven of ten mice died in the vehicle-treated group between days 16 and 19 post implant. Mice treated with any of the drugs survived until they were euthanized due to tumor size
Consistent with the in vitro results, the clofarabine/T-araC combination was only as effective as treatment with T-araC alone against CCRF-CEM leukemia, which indicated that there was antagonism with these two agents in this tumor model (Fig. 6).
Effect of clofarabine plus T-araC on CCRF-CEM leukemia. CCRF-CEM leukemia fragments were implanted sc into the flanks of scid mice. When tumors were approximately 200 mg, mice were treated ip with saline, clofarabine (50 mg/kg/dose, Q2Dx5 starting on day 16), T-araC (80 mg/kg/dose, Q2Dx5 starting on day 17), or clofarabine (50 mg/kg/dose, Q2Dx5 starting on day 16) plus T-araC (80 mg/kg/dose, Q2Dx5 starting on day 17). The tumors were measured twice weekly with calipers after initiation of treatment and the weight was calculated as described. There were six mice per treatment group, except for the vehicle-treated control group (12 mice). The time for the size of each tumor to double twice was calculated and the mean ± SD are shown in the figure for each treatment group
Discussion
In this work we have shown that the combination of clofarabine plus T-araC resulted in dramatically better antitumor activity in four of the five human tumor xenografts that were tested. The antitumor activity of this combination was much better than that which could be achieved with either agent alone. In addition, the antitumor activity of the combination was achieved at dosages that were well below the maximally tolerated dosages of the individual compounds. With the HCT-116 tumors the clofarabine/T-araC combination was superior to that obtained with the single agents even at dosages of drug in the combination therapy that were only 12% of those used in single agent therapy. Since the antitumor efficacy of nucleoside analogs is limited by their toxicity to normal tissues, efficacy at lower dosages could dramatically influence the usefulness of these agents in patients. As expected for cytotoxic agents, mice could not tolerate the clofarabine/T-araC combination when both compounds were dosed at their individual MTDs. However, the mice could tolerate the combination when the dosage of each drug was reduced by 50%, which indicated that the combination treatment of these two drugs only resulted in additive toxicity.
The clofarabine/araC combination has been evaluated in patients with hematologic malignancies [5–7], because of their individual effectiveness and the in vitro results indicating enhance metabolism [4]. One of the primary differences between araC and T-araC is the excellent solid tumor activity of T-araC that has been observed in various human tumor xenografts in mice. T-araC is one of the best single agents in this regard that we have evaluated. It is active in most human tumor xenografts tested and is better than either clofarabine or gemcitabine when compared in these models in terms of numbers of sensitive tumors and induction of regressions. The excellent solid tumor activity seen with the clofarabine/T-araC combination at low dosages of the two compounds seen in our in vivo studies suggests that this combination may also be effective in the treatment of solid tumors in people, whereas a combination of clofarabine plus araC would not be advised in this setting due to the lack of demonstrated solid tumor activity of araC. Phase I trials on T-araC in heavily pretreated patients with relapsed solid tumors resulted in partial responses in some patients. This is in direct contrast to araC which does not show any response in patients with solid tumors. While clofarabine has demonstrated good solid tumor activity in human solid tumor xenografts in mice [22], its effect in humans with solid tumors is not well established. The primary dose limiting toxicity of T-araC in these first two trials was fatigue. The mechanism of this fatigue is not understood, but the side effect profile of both T-araC and clofarabine does not indicate that there would be dose-limiting overlapping toxicities.
The effect of clofarabine on the metabolism of T-araC in the tumor types studied was not uniform, which suggests that the combination would not be effective in all cases. It is encouraging that in a tumor type (HL-60) in which the metabolism of T-araC was increased by only 50%, the clofarabine/T-araC combination still resulted in enhanced antitumor activity. This result suggests that the enhanced antitumor activity observed with this combination could be a consequence of more than just the enhancement of T-araC metabolism. It is also possible that the metabolites of clofarabine and T-araC complement one another in their inhibition of DNA synthesis in tumor cells and that this interaction at the molecular level contributes to the excellent antitumor activity of this combination. Clofarabine triphosphate is a potent inhibitor of ribonucleotide reductase [23], causing a decrease in intracellular dCTP levels. Reduction of dCTP levels would potentiate the activity of any dCyd analog, such as T-araC, by decreasing the intracellular concentration of the natural nucleotide (dCTP) that would compete with T-araCTP for incorporation into DNA by DNA polymerases. It is not certain how much the inhibition of ribonucleotide reductase contributes to the antitumor activity of this combination, because of the considerable amount of time between the administration of clofarabine and T-araC. However, since the retention time of clofarabine triphosphate in tumor cells is quite long [2, 24] and the potency of clofarabine triphosphate is quite high [23, 25], significant amounts of clofarabine triphosphate could still be present in tumor cells at the time of T-araC treatment 24 h after administration of clofarabine.
At this time it is not clear why treatment with clofarabine resulted in an inhibition of T-araC metabolism in CCRF-CEM cells. Others have shown [26] that treatment with cladribine (a compound that is structurally similar to clofarabine) resulted in a decline in dCyd kinase activity, which suggested that clofarabine may also decrease dCyd kinase activity in this cell line. Regardless, the fact that all tumor types did not respond to clofarabine in the same manner suggests that it may be necessary to perform some preliminary analysis in patients to determine which tumors would be sensitive to the combination treatment.
We showed that dCyd kinase activity in K562 cells was increased after treatment with clofarabine; however, the mechanism of enhancement of T-araC metabolism has not been thoroughly evaluated. In our experiments it is not known whether the increase in activity was due to the production of more protein or to the post-translational modification of dCyd kinase that results in enhanced activity of the enzyme. Others have shown that treatment of cells with nucleoside analogs and other agents that inhibit DNA synthesis can induce dCyd kinase activity [26, 27]. These investigators have shown that the enhanced activity was due to phosphorylation of dCyd kinase activity [28]. We believe that it is likely that a similar mechanism is occurring with clofarabine. It is also possible that the reduction of dCTP levels due to the inhibition of ribonucleotide reductase reduces the intracellular concentration of a potent feedback inhibitor of dCyd kinase, thereby increasing intracellular activity of this enzyme.
An important difference between the effect of clofarabine on the metabolism of T-araC and araC was that clofarabine enhanced the metabolism of araC even when clofarabine was not removed from the culture medium during the araC incubation. It is likely that although clofarabine enhances dCyd kinase activity, it also competitively inhibits the phosphorylation of T-araC by dCyd kinase, because clofarabine is a very good substrate [25] and T-araC is a very poor substrate for this enzyme [15]. AraC is also a very good substrate for dCyd kinase [15] and it should compete well with clofarabine for activation by dCyd kinase. Because the plasma half-life of clofarabine is less than 2 h [29], there should be very little clofarabine in the plasma 24 h after its administration at the time of T-araC administration. Our results indicated that the effect of clofarabine on the metabolism of T-araC in tumor tissue was maintained for up to 48 h. This prolonged effect of clofarabine is an important clinical consideration, as it allows for reasonable scheduling of drugs, such as the every other day treatment used in our studies, and some flexibility in the administration of the two agents.
In summary, T-araC is a promising new anticancer agent that has demonstrated excellent activity against numerous human solid tumor xenografts in mice. Two phase I clinical trials have been conducted with T-araC that demonstrated some clinical activity. T-araC has been licensed to a pharmaceutical company and further clinical studies with this agent are planned. The results of this work provide a strong rationale for clinical trials to test the efficacy of a clofarabine/T-araC combination in the treatment of leukemias, lymphomas, and solid tumors. Finally these studies suggest that this combination would exhibit much greater antitumor activity than that of clofarabine plus araC [5–7].
References
Bonate PL, Arthaud L, Cantrell WR Jr, Stephenson K, Secrist JA III, Weitman S (2006) Discovery and development of clofarabine: a nucleoside analogue for treating cancer. Nat Rev Drug Discov 5:855–863
Faderl S, Gandhi V, Keating MJ, Jeha S, Plunkett W, Kantarjian HM (2005) The role of clofarabine in hematologic and solid malignancies—development of a next-generation nucleoside analog. Cancer 103:1985–1995
Kantarjian HM, Jeha S, Gandhi V, Wess M, Faderl S (2007) Clofarabine: past, present, and future. Leuk Lymphoma 48:1922–1930
Cooper T, Ayres M, Nowak B, Gandhi V (2005) Biochemical modulation of cytarabine triphosphate by clofarabine. Cancer Chemother Pharmacol 55:361–368
Faderl S, Gandhi V, O’Brien S, Bonate P, Cortes J, Estey E, Beran M, Wierda W, Garcia-Manero G, Ferrajoli A, Estrov Z, Giles FJ, Du M, Kwari M, Keating M, Plunkett W, Kantarjian H (2005) Results of a phase 1–2 study of clofarabine in combination with cytarabine (ara-C) in relapsed and refractory acute leukemias. Blood 105:940–947
Faderl S, Verstovsek S, Cortes J, Ravandi F, Beran M, Garcia-Manero G, Ferrajoli A, Estrov Z, O’Brien S, Koller C, Giles FJ, Wierda W, Kwari M, Kantarjian HM (2006) Clofarabine and cytarabine combination as induction therapy for acute myeloid leukemia (AML) in patients 50 years of age or older. Blood 108:45–51
Gidwani P, Ramesh KH, Liu Y, Kolb EA (2008) The combination of clofarabine and cytarabine in pediatric relapsed acute lymphoblastic leukemia: a case report. Chemotherapy 54:120–124
Tiwari KN, Shortnacy-Fowler AT, Cappellacci L, Parker WB, Waud WR, Montgomery JA, Secrist JA III (2000) Synthesis of 4′-thio-β-d-arabinofuranosyl-cytosine (4′-thio-ara-C) and comparison of its anticancer activity with that of ara-C. Nucleosides Nucleotides Nucleic Acids 19:329–340
Waud WR, Gilbert KS, Shepherd RV, Montgomery JA, Secrit JA III (2003) Preclinical antitumor activity of 4′-thio-beta-d-arabinofuranosylcytosine (4′-thio-ara-C). Cancer Chemother Pharmacol 51:422–426
Waud WR, Shepherd RV, Gilbert KS, Tiwari KN, Secrist JA III (2004) Precinical antitumor activity of 4′-thio-β-d-arabinofuranosylcytosine (4′-thio-ara-C, OSI-7836) in human leukemia and lymphoma xenograft models. Proc Am Assoc Cancer Res 45:714
Parker WB, Shaddix SC, Rose LM, Waud WR, Shewach DS, Tiwari KN, Secrist JA III (2000) Metabolism of 4′-thio-β-d-arabinofuranosylcytosine in CEM cells. Biochem Pharmacol 60:1925–1932
Richardson F, Black C, Richardson K, Franks A, Wells E, Karimi S, Sennello G, Hart K, Meyer D, Emerson D, Brown E, LeRay J, Nilsson C, Tomkinson B, Bendele R (2005) Incorporation of OSI-7836 into DNA of Calu-6 and H460 xenograft tumors. Cancer Chemother Pharmacol 55:213–221
Clarke ML, Damaraju VL, Zhang J, Mowles D, Tackaberry T, Lang T, Smith KM, Young JD, Tomkinson B, Cass CE (2006) The role of human nucleoside transporters in cellular uptake of 4′-thio-beta-d-arabinofuranosylcytosine and beta-d-arabinosylcytosine. Mol Pharmacol 70:303–310
Richardson KA, Vega TP, Richardson FC, Moore CL, Rohloff JC, Tomkinson B, Bendele RA, Kuchta RD (2004) Polymerization of the triphosphates of AraC, 2′,2′-difluorodeoxycytidine (dFdC) and OSI-7836 (T-araC) by human DNA polymerase alpha and DNA primase. Biochem Pharmacol 68:2337–2346
Someya H, Shaddix SC, Tiwari KN, Secrist JA III, Parker WB (2003) Phosphorylation of 4′-thio-β-d-arabinofuranosylcytosine and its analogs by human deoxycytidine kinase. J Pharmacol Exp Ther 304:1314–1322
Someya H, Waud WR, Parker WB (2006) Long intracellular retention of 4′-thio-arabinofuranosylcytosine 5′-triphosphate as a critical factor for the anti-solid tumor activity of 4′-thio-arabinofuranosylcytosine. Cancer Chemother Pharmacol 57:772–780
Thottassery JV, Westbrook L, Someya H, Parker WB (2006) c-Abl-independent p73 stabilization during gemcitabine- or 4′-thio-beta-d-arabinofuranosylcytosine-induced apoptosis in wild-type and p53-null colorectal cancer cells. Mol Cancer Ther 5:400–410
Goss G, Siu LL, Gauthier I, Chen EX, Oza AM, Goel R, Maroun J, Powers J, Walsh W, Maclean M, Drolet DW, Rusk J, Seymour LK, Investigational New Drug Program of the National Cancer Institute of Canada Clinical Trials Group (2006) A phase I, first in man study of OSI-7836 in patients with advanced refractory solid tumors: IND.147, a study of the Investigational New Drug Program of the National Cancer Institute of Canada Clinical Trials Group. Cancer Chemother Pharmacol 58:703–710
Lee CP, de Jonge MJ, O’Donnell AE, Schothorst KL, Hanwell J, Chick JB, Brooimans RA, Adams LM, Drolet DW, de Bono JS, Kaye SB, Judson IR, Verweij J (2006) A phase I study of a new nucleoside analogue, OSI-7836, using two administration schedules in patients with advanced solid malignancies. Clin Cancer Res 12:2841–2848
Dykes DJ, Abbott BJ, Mayo JG, Harrison SD Jr, Laster WR, Simpson-Herren L, Griswold DP Jr (1992) Development of human tumor xenograft models for in vivo evaluation of new antitumor drugs. Contrib Oncol Basel Karger 42:1–22
Gandhi V, Kantarjian H, Faderl S, Bonate P, Du M, Ayres M, Rios MB, Keating MJ, Plunkett W (2003) Pharmacokinetics and pharmacodynamics of plasma clofarabine and cellular clofarabine triphosphate in patients with acute leukemias. Clin Cancer Res 9:6335–6342
Waud WR, Schmid SM, Montgomery JA, Secrist JA III (2000) Preclinical antitumor activity of 2-chloro-9-(2-deoxy-2-fluoro-beta-d-arabinofuranosyl) adenine (Cl–F-ara-A). Nucleosides Nucleotides Nucleic Acids 19:447–460
Parker WB, Shaddix SC, Chang CH, White EL, Rose LM, Brockman RW, Shortnancy AT, Montgomery JA, Secrist JA III, Bennett LL Jr (1991) Effects of 2-chloro-9-(2-deoxy-2-fluoro-β-d-arabinofuranosyl) adenine on K562 cellular metabolism and the inhibition of human ribonucleotide reductase and DNA polymerases by its 5-triphosphate. Cancer Res 51:2386–2394
Xie C, Plunkett W (1995) Metabolism and actions of 2-chloro-9-(2-deoxy-2-fluoro-beta-d-arabinofuranosyl)-adenine in human lymphoblastoid cells. Cancer Res 55:2847–2852
Parker WB, Shaddix SC, Rose LM, Shewach DS, Hertel LW, Secrist JA III, Montgomery JA, Bennett LL Jr (1999) Comparison of the mechanism of cytotoxicity of 2-chloro-9-(2-deoxy-2-fluoro-β-d-arabinofuranosyl) adenine, 2-chloro-9-(2-deoxy-2-fluoro-β-d-ribofuranosyl) adenine, and 2-chloro-9-(2-deoxy-2,2-difluoro-β-d-ribofuranosyl) adenine in CEM cells. Mol Pharmacol 55:515–520
Spasokoukotskaja T, Sasvári-Székely M, Keszler G, Albertioni F, Eriksson S, Staub M (1999) Treatment of normal and malignant cells with nucleoside analogues and etoposide enhances deoxycytidine kinase activity. Eur J Cancer 35:1862–1867
Csapó Z, Sasvári-Székely M, Spasokoukotskaja T, Talianidis I, Eriksson S, Staub M (2001) Activation of deoxycytidine kinase by inhibition of DNA synthesis in human lymphocytes. Biochem Pharmacol 61:191–197
Keszler G, Spasokoukotskaja T, Sasvári-Székely M, Eriksson S, Staub M (2006) Deoxycytidine kinase is reversibly phosphorylated in normal human lymphocytes. Nucleosides Nucleotides Nucleic Acids 25:1147–1151
Qian M, Wang X, Shanmuganathan K, Chu CK, Gallo JM (1994) Pharmacokinetics of the anticancer agent 2-chloro-9-(2-deoxy-2-fluoro-beta-d-arabinofuranosyl) adenine in rats. Cancer Chemother Pharmacol 33:484–488
Acknowledgment
This work was supported by NCI Grant P01 CA 34200.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure: Clofarabine and T-araC were discovered at Southern Research Institute, which receives licensing fees and royalty payments from the commercial development and use of these agents. Southern Research Institute does distribute some of this money to Drs. Parker and Waud.
Rights and permissions
About this article
Cite this article
Parker, W.B., Shaddix, S.C., Gilbert, K.S. et al. Enhancement of the in vivo antitumor activity of clofarabine by 1-β-d-[4-thio-arabinofuranosyl]-cytosine. Cancer Chemother Pharmacol 64, 253–261 (2009). https://doi.org/10.1007/s00280-008-0862-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-008-0862-z