Abstract
Purpose
Sorafenib (Nexavar®) is an oral multi-kinase inhibitor that inhibits Raf serine/threonine kinases and receptor tyrosine kinases involved in tumor growth and angiogenesis. Sorafenib has demonstrated preclinical and clinical activity against several tumor types, as a monotherapy and in combination with other anti-cancer agents.
Methods
This review summarizes the safety, pharmacokinetics, and anti-tumor activity of sorafenib combined with other targeted agents or cytotoxics from a series of Phase I/II trials in approximately 600 patients with advanced solid tumors.
Results
Sorafenib in combination with other agents was generally well tolerated, and most adverse events were mild to moderate in severity. Frequent drug-related toxicities were dermatologic, gastrointestinal, or constitutional. Most trials supported sorafenib 400 mg bid as the recommended dose for combination. Sorafenib generally had little effect on the pharmacokinetics of coadministered agents and vice versa. Preliminary anti-tumor activity was observed; overall disease control rates (partial response plus stable disease) ranged from 33 to 92%. Particularly promising activity was observed in patients with melanoma, hepatocellular carcinoma, and non-small-cell lung cancer receiving sorafenib plus paclitaxel/carboplatin, doxorubicin, and gefitinib, respectively.
Conclusions
Sorafenib demonstrated a good safety profile and encouraging anti-tumor effects when coadministered with other agents in patients with advanced solid tumors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dysregulation of the Raf/MEK/ERK pathway, which is involved in cellular proliferation, survival, and differentiation, is implicated in the development of solid tumors [1] and is therefore a logical strategy for inhibiting malignant tumor cell proliferation and survival. The oral multi-kinase inhibitor sorafenib (Nexavar®; Bayer Pharmaceuticals Corporation, Onyx Pharmaceuticals) targets the Raf serine/threonine kinases (Raf-1, wild-type B-Raf, and b-raf V600E) and the vascular endothelial growth factor receptor (VEGFR)-1/-2/-3, platelet-derived growth factor receptor-β (PDGFR-β) and Flt-3, c-Kit, and p38 tyrosine kinases [2].
In Phase II/III clinical trials, single-agent sorafenib significantly prolonged progression-free survival (PFS) two to fourfold versus placebo in patients with advanced renal cell carcinoma (RCC), a historically chemoresistant tumor with a particularly poor prognosis [3, 4]. Furthermore, sorafenib treatment was associated with an estimated 28% reduction in mortality risk over placebo (P = 0.018; hazard ratio: 0.72) in the first survival analysis of a large, randomized, controlled Phase III trial in RCC [3]. Compared with standard chemotherapies that are associated with alopecia, anemia, neutropenia, renal or neurologic side-effects, single-agent sorafenib at 400 mg twice daily (bid) was found to be generally well tolerated throughout the Phase I–III clinical trial program [3–6]. The majority of adverse events was mild to moderate in severity, followed a predictable course, and was manageable [3–6]. The most frequently reported drug-related adverse events were dermatologic [hand–foot skin reaction (HFSR), rash/desquamation], gastrointestinal (diarrhea), and constitutional (fatigue) [3, 5, 6]. Severe biochemical abnormalities, myelosuppression, hematologic, cardiovascular, hepatic, and renal toxicities were rarely reported [5]. Across the clinical program, treatment-emergent hypertension at any grade was observed in 5–17% (<5% at grade 3 or 4) of patients receiving sorafenib 400 mg bid [3, 5]. However, hypertension was manageable with interventional anti-hypertensive drugs [3]. Similarly, although dermatologic adverse events occurred in just over twice as many patients receiving sorafenib compared with those on placebo, these toxicities were generally reversible and resolvable with topical therapies, dose modification, or treatment interruption [3]. The excellent tolerability profile of sorafenib suggests that it could be combined with other anti-tumor agents, including cytotoxic agents that are usually associated with higher levels of toxicities, as well as other targeted therapies [7]. Evidence from several human tumor xenograft models suggests that the anti-tumor activity of a wide variety of chemotherapeutic agents, including doxorubicin, paclitaxel, cisplatin, docetaxel, and gemcitabine, is enhanced by concomitant inhibition of Raf expression [8, 9].
Combinatorial targeting of multiple points upstream and downstream in several signaling pathways is important for inhibition of tumor proliferation and induction of apoptosis, and thus provides a rationale for combining sorafenib with other targeted agents. Furthermore, combining drugs that have different mechanisms of action may enhance anti-tumor activity by overcoming mechanisms of drug resistance [10]. Preliminary preclinical studies with sorafenib in combination with gefitinib, vinorelbine, gemcitabine, and irinotecan have not demonstrated a significant increase in toxicity above that expected for either agent alone [11, 12]. Sorafenib did not abrogate the anti-tumor activity of coadministered gefitinib or vinorelbine in non-small-cell lung cancer (NSCLC) xenograft models [11]. In a colon tumor xenograft model, sorafenib plus irinotecan did not produce greater toxicity than expected for either agent alone, and did not reduce the efficacy of irinotecan [12]. Contrastingly, dose reductions of both sorafenib and doxorubicin were required for concomitant administration of these agents in a breast xenograft model [11].
Based on these data, a series of dose-ranging trials was undertaken to assess the safety, pharmacokinetics, and anti-tumor activity of sorafenib in combination with anti-cancer agents, including chemotherapies, immunotherapies, and other targeted agents. A review of these data from sorafenib combination trials is provided.
Sorafenib combination with anti-cancer therapies
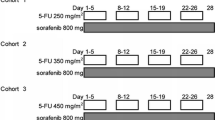
Data are available from 19 Phase I/II open-label, uncontrolled clinical trials conducted in over 600 patients investigating sorafenib in combination with other agents (Table 1). In general, Phase I studies consisted of a dose-escalation part in patients with refractory solid tumors followed by an extension part, administering the maximum tolerated dose (MTD) to patients with a specific tumor type.
Safety
Dose-limiting toxicities
Common dose-limiting toxicities (DLTs) were HFSR and diarrhea, and these generally occurred at higher dose levels (Table 2) [13–17]. Less-frequent DLTs consisted of fatigue [18], hyperuricemia [17], rash [19], and asthenia [20]. The MTD was not reached in many of the combination trials [13, 14, 16–18, 20–22]. With the exception of the bevacizumab combination [23, 24], trials generally supported a dosing schedule of continuous oral sorafenib 400 mg bid. Sorafenib 200 mg bid plus bevacizumab 5 mg/kg was the MTD [23, 24]; dose-limiting hypertension, proteinuria, thrombocytopenia, and elevated lipase were reported in patients receiving sorafenib plus bevacizumab 10 mg/kg [23, 24]. In the trials in which full doses of both agents could be administered without reaching the MTD, the most frequently reported DLTs were dermatologic and gastrointestinal symptoms. Five of 22 patients (23%) receiving sorafenib 400 mg bid plus doxorubicin experienced reversible dose-limiting HFSR that was considered sorafenib related [14]. Two patients (10%) in the hepatocellular carcinoma (HCC) extension cohort receiving sorafenib plus doxorubicin had sorafenib-related dose-limiting HFSR that resolved after dose reduction or temporary treatment discontinuation [13]. Only one of seven patients (14%) receiving sorafenib (400 mg bid) and gemcitabine (1,000 mg/m2) developed grade 3 fatigue that was dose limiting [18]. None of the other 19 patients in the dose-escalation phase or the 23 patients in the pancreatic extension cohort had DLTs [18]. Only two DLTs of sorafenib-related grade 3 diarrhea occurred in two patients (5%) who received the 400 mg bid dose, in combination with oxaliplatin [16]. Furthermore, only one DLT (grade 3 asthenia) was observed in one patient (8%) receiving sorafenib (400 mg bid) plus interferon-α2a (9 MIU three-times weekly) [20]. In melanoma patients, only one DLT (grade 3 HFSR) was reported out of a total of 15 patients receiving sorafenib (400 mg bid) plus dacarbazine (DTIC) (1,000 mg/m2) [15]. Only two DLTs were reported with sorafenib plus erlotinib (grade 3 hypophosphatemia and grade 2 diarrhea/anorexia) and, therefore, the recommended dose of this combination was sorafenib 400 mg bid plus erlotinib 150 mg qd (Table 2) [25].
Adverse event profiles
The sorafenib combination studies were generally well tolerated; in most studies, tolerability profiles were similar to those expected with each agent as a monotherapy [15–18, 25–28]. Only sorafenib in combination with the monoclonal antibody against VEGF, bevacizumab, was associated with greater than expected toxicity based on the safety profile of the individual agents [23, 24]. This combination appeared to increase the toxicity above that reported for the single agents. The most common adverse events with sorafenib 200 mg bid plus bevacizumab 5 mg/kg were hypertension, HFSR, leukopenia and infection. All patients had elevated alanine aminotranferease (ALT) and aspartate aminotransferase (AST), rhinorrhea, fatigue, anorexia, weight loss, and neuropathy at grade 1 or 2 [23, 24]. In the majority of other trials, frequent drug-related adverse events were dermatologic (HFSR, rash/desquamation, and alopecia), gastrointestinal (diarrhea and nausea), or constitutional (fatigue) and most were grade 1 or 2 in severity. The overall incidence of grade 1 or 2 HFSR was greater (approximately 50 vs. 25%) in patients receiving sorafenib 400 mg bid versus 200 mg bid when combined with gefitinib, oxaliplatin, doxorubicin, or DTIC [14–16, 21]. The most common grade 3 or 4 drug-related adverse events were dermatologic (HFSR, rash/desquamation) and gastrointestinal toxicities (diarrhea, vomiting), which are typical of sorafenib, or bone marrow suppression (neutrophils/granulocytes/leukocytes and febrile neutropenia), which is commonly associated with standard chemotherapy.
Importantly, the adverse events observed in these combination trials with cytotoxic chemotherapy rarely overlapped with those more commonly associated with sorafenib. High-dose docetaxel is associated with neutrophil- and leukocyte-related toxicities [29]. In patients with advanced melanoma receiving sorafenib plus temozolomide, the majority of toxicities could be attributed to either therapy [30], whereas increases in the incidence of constitutional and gastrointestinal toxicities in interferon-α2b combination studies were typical of interferon-α2b treatment [31, 32]. Together, these studies suggest that sorafenib has the potential to be combined with a variety of chemotherapies and targeted agents.
Pharmacokinetics
Sorafenib generally had little effect on the pharmacokinetics of coadministered agents and vice versa (Table 3) [16–18, 20, 33]. Increases were observed in drug exposures of doxorubicin, irinotecan, and docetaxel, in combination with sorafenib [13, 14, 22]. These findings were neither generally dose related nor were they associated with increased clinical toxicity, and thus were not considered clinically meaningful. Although sorafenib pharmacokinetics were not influenced significantly by concomitant doxorubicin, slight increases in doxorubicin and doxorubicinol Cmax and AUC values were observed with sorafenib 400 mg bid (given as 50 mg tablets) [13, 14], but these alterations were not associated with an increase in myelosuppression. No significant change in doxorubicin exposure was observed when coadministered with either sorafenib 400 mg bid given as 200 mg tablets, or with lower doses of sorafenib (100 or 200 mg bid) [13, 14]. Coadministration of sorafenib (100 or 200 mg bid) and irinotecan (125 mg/m2) did not substantially alter the clinical tolerability of either drug. Increased exposure to irinotecan and its metabolite SN-38 was reported with the combination of irinotecan 125 mg/m2 or 140 mg (fixed dose) with sorafenib 400 mg bid, but did not appear to increase clinical toxicity, suggesting that this is not a clinically significant effect. Irinotecan 140 mg (fixed dose) had a negligible effect on the pharmacokinetics of sorafenib [22].
Efficacy
Anti-tumor activity
Anti-tumor activity for mixed-tumor studies and single-tumor studies are presented in Tables 4 and 5, respectively. Overall disease control rates (partial response plus stable disease) ranged from 33 to 92% across these trials. Sorafenib plus paclitaxel/carboplatin showed particularly promising activity in metastatic melanoma patients: one (∼1%) complete response, a partial response rate of 26%, and a stable disease rate of 58% (disease control rate of 84%) were reported [26]. In addition, 13–17% of melanoma patients achieved a partial response and 53–61% of patients had stable disease (disease control rate of 66–78%) with sorafenib in combination with DTIC [15, 28]. Although few trials in advanced melanoma describe PFS, the median PFS of 8.8 months reported with sorafenib plus carboplatin/paclitaxel compares favorably with that reported for DTIC/cisplatin/interferon-α2a with or without interleukin-2 (3.9 and 3.0 months, respectively) [26, 34]. In a subpopulation of NSCLC patients, sorafenib plus carboplatin/paclitaxel also demonstrated a relatively high level of partial responses and disease stabilizations (27 and 47%, respectively), as well as a median PFS of almost 5 months [27]. The combination of sorafenib and doxorubicin appeared promising in advanced HCC, with 67% of patients in an extension cohort achieving stable disease [13]. Partial responses were reported in two heavily pretreated ovarian cancer patients (11%) treated with sorafenib (400 mg bid cohort) plus gemcitabine in the dose-escalation part of the trial. Both patients had received previous taxane, platinum, and anthracycline therapies [18]. A relatively high level of disease stabilization was achieved with sorafenib plus gemcitabine in the dose-escalation phase in patients with mixed solid tumors and in the MTD expansion cohort in patients with pancreatic cancer (63 and 57%, respectively) [18]. This combination demonstrated anti-tumor activity in a recent Phase II study in epithelial ovarian cancer patients, with approximately two-thirds of patients achieving partial response or stable disease, and a median time to progression of 7.6 months [35]. Sorafenib combined with the epidermal growth factor receptor (EGFR) inhibitor gefitinib demonstrated encouraging anti-tumor activity in NSCLC patients, with 63% achieving stable disease (median duration 20.4 weeks) (Table 5) [21]. Similarly, sorafenib plus another EGFR inhibitor, erlotinib, produced partial responses in 23% of patients and stable disease in 62% [25]. A relatively high disease stabilization rate (42–75%) was also reported in patients with solid tumors who received sorafenib combined with bevacizumab (Table 4) [23, 24]. Four of 14 patients with epithelial ovarian cancer achieved partial responses with sorafenib plus bevacizumab [23]. Fistula formation was observed in areas of rapid tumor regression in three ovarian cancer patients, two of whom achieved partial response [23]. In metastatic RCC patients in the first- and second-line setting, sorafenib plus interferon-α2b generated response rates that were greater than either agent alone: two complete responses were reported and approximately one third of patients achieved partial response [31, 32].
Discussion
Sorafenib in combination was generally safe and well tolerated in patients with advanced, progressive solid tumors, including RCC, melanoma, HCC, and colorectal cancer (CRC), with little evidence of clinically relevant drug–drug interactions. The reported safety and tolerability profiles associated with sorafenib in combination with other anti-cancer agents are encouraging and consistent with the results of the preclinical combination studies [11, 12].
The safety profile observed in the Phase I/II combination trials was similar to that reported in Phase I trials of single-agent sorafenib [36]. The most frequently observed adverse events included HFSR, rash, diarrhea, and fatigue, which were mostly mild to moderate in severity, and most tended to occur at higher doses of sorafenib. In a pooled safety analysis from four Phase I trials, the occurrence of skin toxicity or diarrhea in patients receiving sorafenib at doses ranging 300–600 mg bid is correlated with a longer time to tumor progression [36]. The optimal dose of sorafenib plus bevacizumab has yet to be established. Potential synergistic inhibitory effects on the VEGF/VEGFR pathway may be responsible for the apparent increased level of toxicities (e.g. hypertension, proteinuria, and thrombocytopenia), observed with sorafenib plus bevacizumab, above those reported for at least equal doses of single agents [23, 24]. Despite this, sorafenib appears to be easily combined with many other treatments due to its favorable safety profile on a continuous administration schedule and its convenient oral route of administration.
Generally, there were no clinically relevant pharmacokinetic drug–drug interactions when sorafenib was combined with other anti-cancer agents. Exposure to doxorubicin, irinotecan, and docetaxel did increase when combined with sorafenib; however, this effect was not accompanied by any significant increase in clinical toxicity. Interactions at the level of hepatic metabolism and elimination may account for the observed increase in drug exposure of these agents.
Multiple signaling pathways contribute to tumor growth and angiogenesis. Therefore, combining agents with different mechanisms of action may enhance anti-tumor activity through horizontal and/or vertical inhibition of multiple tumorigenic pathways [37]. For example, sorafenib plus an EGFR inhibitor (e.g. erlotinib or gefitinib) may achieve vertical inhibition of the Raf/MEK/ERK pathway by targeting both Raf and the EGFR in tumor cells. A horizontal inhibition of signaling pathways may be achieved through inhibition of Raf, PDGFR, and VEGFR with sorafenib and the anti-VEGF monoclonal antibody bevacizumab.
Drug resistance to cytotoxics, such as doxorubicin and docetaxel, is a common clinical problem limiting their effectiveness, especially as single agents. Data suggest that conventional therapies exert their cytotoxic activities primarily by inducing apoptosis in tumor cells, and that resistant cells adopt mechanisms to evade apoptotic pathways [38]. One mechanism of chemoresistance may involve the overexpression of anti-apoptotic molecules, such as Bcl-2 [39]. Recent evidence suggests that synergism between Bcl-2 and Raf-1 may enhance the suppression of apoptosis [39]. Sorafenib can induce apoptosis in vitro in a variety of human cancer cell lines by enhancing the proteasomal degradation of Bcl-2 family member, Mcl-1 [40]. Thus, downregulation of anti-apoptotic molecules may help sensitize tumor cells to chemotherapy. Expression of the multidrug resistance 1 (mdr-1) gene is associated with solid tumors that have a high level of intrinsic or acquired chemoresistance [41]. The effects of Raf in regulating the mdr-1 gene and on regulating the sensitivity of tumor cells to chemotherapy-induced cell death suggest that drug resistance may be reduced with a Raf inhibitor, such as sorafenib [42]. Raf-1 activation has also been associated with potent inhibition of apoptosis, leading to cell survival [43]. Downregulating B-Raf expression using small interfering RNAs inhibits MEK/ERK activation and cell growth, and induces apoptosis in melanoma cell lines [44].
Anti-tumor activity with sorafenib combinations was equivalent to or potentially better than with either drug alone. Anti-tumor activity with sorafenib plus DTIC or paclitaxel/carboplatin was encouraging in advanced melanoma, with disease control rates of up to 78 and 84%, respectively [15, 19, 26]. These data compare favorably with DTIC or paclitaxel/carboplatin alone, in which partial responses were obtained in 10 [45] and 20% [46] of advanced melanoma patients, respectively. A Phase II trial of carboplatin/paclitaxel in melanoma patients demonstrated a low overall response rate of <10% [47]. Therefore, it is possible that the improved anti-tumor activity reported with sorafenib plus carboplatin/paclitaxel results from a synergistic interaction between these agents. In NSCLC patients, a stable disease rate of 63% was reported when treated with sorafenib combined with the targeted agent gefitinib [21]. Furthermore, sorafenib plus the targeted agent bevacizumab produced disease stabilization in 42–75% of patients with a variety of solid tumors [23, 24].
Some patients who were refractory to single-agent chemotherapy demonstrated improved tumor response when the same chemotherapy was administered in combination with sorafenib [16, 18]. For example, a high proportion of CRC patients who received sorafenib plus oxaliplatin in an extension study had stable disease, despite these patients showing previous resistance to oxaliplatin monotherapy [16]. Two heavily pretreated ovarian cancer patients, refractory to taxanes, platinum-containing chemotherapies, and anthracyclines, achieved partial responses with sorafenib plus gemcitabine [18]. Furthermore, a patient with recurrent nasopharyngeal carcinoma in the dose-escalation cohort, who was previously minimally responsive to gemcitabine treatment, had stable disease for >1 year when receiving gemcitabine plus sorafenib [18]. These findings could be attributable to sorafenib sensitizing previously treatment-refractory patients to the coadministered agents.
In addition to sorafenib’s pro-apoptotic effect, its anti-angiogenic properties may render tumors more susceptible to chemotherapy by altering the vasculature. Inhibiting tumor angiogenesis can enhance delivery of cytotoxic agents by affecting the vasculature, and thereby increase the effectiveness of concomitant chemotherapy [48]. Tumor blood vessels formed under the influence of VEGF are disorganized and leaky, with high interstitial pressure, which reduces access to chemotherapies [49]. Inhibiting VEGF can reduce vessel abnormality and increase the permeability of the tumor to chemotherapies [48]. Therefore, the combination of bevacizumab plus sorafenib is an attractive therapeutic strategy because of their potentially synergistic effects on the vasculature and tumor.
Overall, sorafenib has a promising safety profile and demonstrates encouraging anti-tumor effects in combination with other anti-cancer agents in patients with several solid tumor types. In general, sorafenib at the full-recommended dose of 400 mg bid does not increase the risk of clinical toxicity of combination therapy above that expected for either agent alone. Results from these studies suggest that sorafenib in combination with other cytotoxics or targeted agents are potentially valuable new treatment alternatives for patients with advanced solid tumors.
Future directions
Given the complexity of the interactions between tumor cells and their environment, and the variety of pro-angiogenic and/or growth-promoting (autocrine) factors that tumors can produce, there is a strong rationale to combine agents with different mechanisms of action. The results from the trials reported here have led to the initiation of other combination clinical trials to evaluate sorafenib in a variety of solid tumor types. Sorafenib in combination with the chemotherapy gemcitabine or EGFR tyrosine kinase inhibitor, erlotinib, is being evaluated as first-line treatment in an ongoing Phase II trial in elderly patients or patients with a performance status of 2 affected by advanced NSCLC [50]. A Phase II trial with sorafenib combined with the anti-VEGF monoclonal antibody bevacizumab is also underway. Phase III trials have recently been initiated with sorafenib plus carboplatin/paclitaxel in advanced melanoma and NSCLC patients. The promising combination data now available for several targeted agents, and their late stage of clinical development, also raises questions about how best to optimize their use in the clinic. Optimal dosages and treatment schedules (i.e. concomitant or sequential administration of combination therapies) need to be investigated. Whether these combinations offer a PFS or overall survival benefit must still be determined. Finally, the development of appropriate biomarkers to facilitate patient selection and to monitor response to combinations of targeted therapies is also an important area for further translational research.
References
Downward J (2003) Targeting RAS signalling pathways in cancer therapy. Nat Rev Cancer 3:11–22
Wilhelm SM, Carter C, Tang L et al (2004) BAY 43-9006 exhibits broad spectrum oral anti-tumor activity and targets the Raf/MEK/ERK pathway and receptor tyrosine kinases involved in tumor progression and angiogenesis. Cancer Res 64:7099–7109
Escudier B, Eisen T, Stadler WM et al (2007) Sorafenib in advanced clear-cell renal-cell carcinoma. N Engl J Med 356:125–134
Kane RC, Farrell AT, Saber H et al (2006) Sorafenib for the treatment of advanced renal cell carcinoma. Clin Cancer Res 12:7271–7278
Strumberg D, Clark JW, Awada A et al (2007) Safety, pharmacokinetics, and preliminary antitumor activity of sorafenib: a review of four phase I trials in patients with advanced refractory solid tumors. Oncologist 12:426–437
Ratain MJ, Eisen T, Stadler WM et al (2006) Phase II placebo-controlled randomized discontinuation trial of sorafenib in patients with metastatic renal cell carcinoma. J Clin Oncol 24:2505–2512
Chatelut E, Delord JP, Canal P (2003) Toxicity patterns of cytotoxic drugs. Invest New Drugs 21:141–148
Mewani RR, Tang W, Rahman A et al (2004) Enhanced therapeutic effects of doxorubicin and paclitaxel in combination with liposome-entrapped ends-modified raf antisense oligonucleotide against human prostate, lung and breast tumor models. Int J Oncol 24:1181–1188
Pei J, Zhang C, Gokhale PC et al (2004) Combination with liposome-entrapped, ends-modified raf antisense oligonucleotide (LErafAON) improves the anti-tumor efficacies of cisplatin, epirubicin, mitoxantrone, docetaxel and gemcitabine. Anticancer Drugs 15:243–253
Mickisch GH (1994) Chemoresistance of renal cell carcinoma: 1986–1994. World J Urol 12:214–223
Vincent P, Zhang X, Chen C et al (2003) Preclinical chemotherapy with the Raf kinase inhibitor BAY 43-9006 in combination with gefitinib, vinorelbine, gemcitabine or doxorubicin. Proc Am Assoc Cancer Res 44:164
Vincent R, Bernando V, Chen C, Zhang X, Carter C (2003) Chemotherapy with BAY 43-9006 in combination with Irinotecan or administered as repeated cycles of therapy against the DLD-1 human tumor xenograft. Clin Cancer Res 44:4469 (Abstract)
Richly H, Kupsch P, Passage K et al (2004) Results of a phase I trial of BAY 43-9006 in combination with doxorubicin in patients with primary hepatic cancer. Int J Clin Pharmacol Ther 42:650–651
Richly H, Henning BF, Kupsch P et al (2006) Results of a Phase I trial of sorafenib (BAY 43-9006) in combination with doxorubicin in patients with refractory solid tumors. Ann Oncol 17:866–873
Eisen T, Ahmad T, Marais R et al (2005) Phase I trial of sorafenib (BAY 43-9006) combined with dacarbazine (DTIC) in patients with metastatic melanoma. Eur J Cancer Suppl 3:349
Kupsch P, Henning BF, Passarge K et al (2005) Results of a phase I trial of sorafenib (BAY 43-9006) in combination with oxaliplatin in patients with refractory solid tumors, including colorectal cancer. Clin Colorectal Cancer 5:188–196
Figer A, Moscovici M, Bulconic S et al (2004) Phase I trial of BAY 43-9006 in combination with 5-fluorouracil (5-FU) and leucovorin (LCV) in patients with advanced refractory solid tumors. Ann Oncol 15:iii87 (Abstract 327)
Siu LL, Awada A, Takimoto CH et al (2006) Phase I trial of sorafenib and gemcitabine in advanced solid tumors with an expanded cohort in advanced pancreatic cancer. Clin Cancer Res 12:144–151
Flaherty KT, Lee RJ, Humphries R, O’Dwyer PJ, Schiller J (2003) Phase I trial of BAY 43-9006 in combination with carboplatin (C) and paclitaxel (P). Proc Am Soc Clin Oncol 22:710
Robert C, Lassau N, Angevin E et al (2005) Phase I trial of sorafenib (BAY 43-9006) in combination with interferon alpha 2a in patients with unresectable and/or metastatic renal cell carcinoma and malignant melanoma. Eur J Cancer Suppl 3:254
Adjei AA, Mandrekar S, Marks RS et al (2005) A phase I study of BAY 43-9006 and gefitinib in patients with refractory or recurrent non small cell lung cancer (NSCLC). J Clin Oncol 23:208s
Steinbild S, Baas F, Gmehling D et al (2005) Phase I study of BAY 43-9006 (sorafenib), a Raf kinase and VEGFR inhibitor, combined with irinotecan (CPT-11) in advanced solid tumors. J Clin Oncol 23:3115 (Abstract)
Azad NS, Posadas EM, Kwitkowski VE et al (2006) Increased efficacy and toxicity with combination anti-VEGF therapy using sorafenib and bevacizumab. J Clin Oncol 24:3004 (Meeting Abstracts)
Posadas EM, Kwitkowski V, Liel MS et al (2005) Clinical synergism from combinational VEGF signal transduction inhibition in patients with advanced solid tumors - early results from a Phase I study of sorafenib (BAY 43-9006) and bevacizumab. Eur J Cancer Suppl 3:419
Duran I, Hotte S, Chen E et al (2007) Dual inhibition of the MAPK pathway by combination targeted therapy: a phase I trial of sorafenib (SOR) and erlotinib (ERL) in advanced solid tumors. Eur J Cancer (supp) 4:167
Flaherty KT, Brose M, Schuchter LM et al (2006) Sorafenib combined with carboplatin and paclitaxel for metastatic melanoma: PFS and response versus B-Raf status. Ann Oncol 17:iii33
Schiller JH, Flaherty KT, Redlinger M et al (2006) Sorafenib combined with carboplatin/paclitaxel for advanced non-small cell lung cancer: a phase I subset analysis. J Clin Oncol 24:7194 (Meeting Abstracts)
Lorigan P, Corrie P, Chao D et al (2006) Phase II trial of sorafenib combined with dacarbazine in metastatic melanoma patients. J Clin Oncol 24:8012 (Meeting Abstracts)
Adjei AA, Argiris A, Murren JR (1999) Docetaxel and irinotecan, alone and in combination, in the treatment of non-small cell lung cancer. Semin Oncol 26:32–40
Amaravadi RK, Schuchter LM, Kramer A et al (2006) Preliminary results of a randomized phase II study comparing two schedules of temzolomide in combination with sorafenib in patients with advanced melanoma. J Clin Oncol 24(Part 1):8009 (Meeting Abstracts)
Gollob J, Richmond T, Jones J et al (2006) Phase II trial of sorafenib plus interferon-alpha 2b (IFN-{alpha}2b) as first- or second-line therapy in patients (pts) with metastatic renal cell cancer (RCC). J Clin Oncol 24:4538 (Meeting Abstracts)
Ryan CW, Goldman BH, Lara PN Jr et al (2006) Sorafenib plus interferon-{alpha}2b (IFN) as first-line therapy for advanced renal cell carcinoma (RCC): SWOG 0412. J Clin Oncol 24:4525 (Meeting Abstracts)
Flaherty KT, Brose M, Schuchter L et al (2004) Phase I/II trial of BAY 43-9006, carboplatin (C) and paclitaxel (P) demonstrates preliminary antitumor activity in the expansion cohort of patients with metastatic melanoma. J Clin Oncol 22:7507 (Abstract)
Keilholz U, Punt CJ, Gore M et al (2005) Dacarbazine, cisplatin, and interferon-alfa-2b with or without interleukin-2 in metastatic melanoma: a randomized phase III trial (18951) of the European Organisation for Research and Treatment of Cancer Melanoma Group. J Clin Oncol 23:6747–6755
Welch S, Hirte H, Schilder RJ et al (2006) Phase II study of sorafenib (BAY 43-9006) in combination with gemcitabine in recurrent epithelial ovarian cancer: A PMH phase II consortium trial. J Clin Oncol 24:5084 (Meeting Abstracts)
Strumberg D, Awada A, Hirte H et al (2006) Pooled safety analysis of BAY 43-9006 (sorafenib) monotherapy in patients with advanced solid tumours: Is rash associated with treatment outcome? Eur J Cancer 42:548–556
Staehler M, Rohrmann K, Haseke N, Stief CG, Siebels M (2005) Targeted agents for the treatment of advanced renal cell carcinoma. Curr Drug Targets 6:835–846
Odabaei G, Chatterjee D, Jazirehi AR et al (2004) Raf-1 kinase inhibitor protein: structure, function, regulation of cell signaling, and pivotal role in apoptosis. Adv Cancer Res 91:169–200
Wang HG, Miyashita T, Takayama S et al (1994) Apoptosis regulation by interaction of Bcl-2 protein and Raf-1 kinase. Oncogene 9:2751–2756
Yu C, Bruzek LM, Meng XW et al (2005) The role of Mcl-1 downregulation in the proapoptotic activity of the multikinase inhibitor BAY 43-9006. Oncogene 24:6861–6869
Kim SH, Lee SH, Kwak NH, Kang CD, Chung BS (1996) Effect of the activated Raf protein kinase on the human multidrug resistance 1 (MDR1) gene promoter. Cancer Lett 98:199–205
Cornwell MM, Smith DE (1993) A signal transduction pathway for activation of the mdr1 promoter involves the proto-oncogene c-raf kinase. J Biol Chem 268:15347–15350
Erhardt P, Schremser EJ, Cooper GM (1999) B-Raf inhibits programmed cell death downstream of cytochrome c release from mitochondria by activating the MEK/Erk pathway. Mol Cell Biol 19:5308–5315
Karasarides M, Chiloeches A, Hayward R et al (2004) B-RAF is a therapeutic target in melanoma. Oncogene 23:6292–6298
Chapman PB, Einhorn LH, Meyers ML et al (1999) Phase III multicenter randomized trial of the Dartmouth regimen versus dacarbazine in patients with metastatic melanoma. J Clin Oncol 17:2745–2751
Hodi FS, Soiffer RJ, Clark J, Finkelstein DM, Haluska FG (2002) Phase II study of paclitaxel and carboplatin for malignant melanoma. Am J Clin Oncol 25:283–286
Zimpfer-Rechner C, Hofmann U, Figl R et al (2003) Randomized phase II study of weekly paclitaxel versus paclitaxel and carboplatin as second-line therapy in disseminated melanoma: a multicentre trial of the Dermatologic Co-operative Oncology Group (DeCOG). Melanoma Res 13:531–536
Ferrara N (2004) Vascular endothelial growth factor as a target for anticancer therapy. Oncologist 9(Suppl 1):2–10
Ferrara N (2005) VEGF as a therapeutic target in cancer. Oncology 69(Suppl 3):11–16
Gridelli C, Rossi A, Mongillo F et al (2007) A randomized phase II study of sorafenib/gemcitabine or sorafenib/erlotinib for advanced non-small-cell lung cancer in elderly patients or patients with a performance status of 2: treatment rationale and protocol dynamics. Clin Lung Cancer 8:396–398
Sosman JA, Flaherty K, Atkins MB et al (2006) A phase I/II trial of sorafenib (S) with bevacizumab (B) in metastatic renal cell cancer (mRCC) patients (Pts). J Clin Oncol 24:3031 (Meeting Abstracts)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Takimoto, C.H., Awada, A. Safety and anti-tumor activity of sorafenib (Nexavar®) in combination with other anti-cancer agents: a review of clinical trials. Cancer Chemother Pharmacol 61, 535–548 (2008). https://doi.org/10.1007/s00280-007-0639-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-007-0639-9