Abstract
Laboratory and clinical studies support the concept that heparins, particularly the low molecular component, may serve as an inhibitor of angiogenesis, providing anti-neoplastic effects. Further, treatment with low molecular weight heparin (LMWH) may provide prophylaxis for thromboembolic events (TEE), in glioblastoma (GBM) patients. Dalteparin (5,000 U sub-Q daily) was given with and after conventional radiotherapy to newly diagnosed GBM patients. Forty-five patients were accrued between 5/02 and 9/04; 3 were ineligible. At time of progression, patients could continue dalteparin in addition to standard regimens. Pretreatment characteristics included: median age 61 (range 26–78); ECOG Performance status: 0 = 38%, 1 = 57%, 2 = 5%; gross total resection 45%. There were no grade 3/4 bleeding or thrombocytopenic events, and no TEE occurred while on dalteparin. Median time on dalteparin was 6.3 months, median time to progression was 3.9 months; median survival was 11.9 months. There was no significant improvement in survival when compared to the RTOG GBM database (with various radiation/drug doublets including BCNU) using recursive partitioning analysis. Historically the incidence of TEE in GBM patients is ∼30%. As this study suggests dalteparin reduces the incidence of TEE, and does not have significant overlapping toxicities with most other drugs; its testing in a combined modality approach with other medications may be warranted in future trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Meta-analysis has suggested reduced mortality in cancer patients receiving low molecular weight heparin (LMWH) compared with patients receiving standard heparin, and this benefit is not consequent to reduced thromboembolism [1]. Mechanistically, the potential anti-neoplastic properties of LMWH include anti-angiogenisis [2, 3], effects on cellular matrix [4, 5], and reduced cell proliferation [6]. In this regard, it is of interest to note that based on preclinical studies, anti-angiogensis agents can putatively serve as radio-sensitizers [7, 8]. As Glioblastoma multiforme (GBM) is among the most vascular of all neoplasms, (and abundantly express vascular endothelial growth factor and platelet-derived growth factor [9]) the use of LMWH as a therapeutic adjunct to radiotherapy was viewed as worthy of clinical testing.
Additionally, it was recognized at the onset of clinical trial design that patients with GBM were highly predisposed to thromboembolic phenomena [10–20]. Thus, it was further hypothesized that the administration of dalteparin, a LMWH, might provide prophylaxis for TEE. Hence, the careful monitoring of the incidence of TEE was an important secondary objective of study.
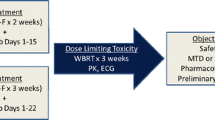
Based on the aforementioned considerations, the Eastern Cooperative Oncology Group (ECOG) initiated in 2002 a phase II study (E1F01) of dalteparin (given during and post-radiotherapy) for newly diagnosed patients with GBM. This report summarizes the results of this phase II trial.
Patients and methods
Eligibilty
To be eligible for the protocol, patients were required to have histologically proven supratentorial GBM with an estimated survival of at least 8 weeks, and ECOG Performance Status of 0,1, or 2. Patients were required to have had pre- and post-operative contrast enhanced MRI or CT scan prior to the initiation of radiotherapy. Patients had to have recovered from surgery. Laboratory requirements included: absolute neutrophil count ≥ 1,500/mm3, platelets ≥ 100,000 mm3, creatinine ≤ 2.0+ mg/dl, bilirubin ≤ 2.5 mg/dl, Hgb ≥ 10 gm/dl, SGPT or SGOT ≤ 3 × normal range, PT/aPTT < 1.5 × ULN. Patients were required to have a negative stool guiac within 2 weeks prior to registration; if stool guiac was positive, the patient was required to have a negative endoscopy. Patients could not have known hypersensitivity to dalteparin, heparin, or pork products. Patients with a prior history of heparin-induced thrombocytopenia were excluded. A history of peptic ulcer disease or hematuria in the previous 6 months was regarded as exclusion factors. Patients with a history of coagulopathies or TEE were excluded to study entry. (Details regarding peri-operative prophylaxis for TEE were not obtained as part of the study.) Patients were required not to receive ongoing or concurrent aspirin or anti-coagulation therapy. Routine central venous catheter flushing was permitted. Patients could not have an active infection, including HIV positivity or AIDS-related illness. Intracranial or intraoccular hemorrhage (unless related to surgery) or retinal detachment within the prior 6 months resulted in exclusion. Patients could not have uncontrolled hypertension, unstable angina, symptomatic congestive heart failure, myocardial infarction within the previous 6 months, or uncontrolled cardiac arrhythmia. Concurrent malignancy under treatment was an exclusion factor. Women could not be pregnant or breast-feeding due to potential damaging effects of the therapies on the fetus and/or breast-fed infant. Women of childbearing potential and sexually active males had to agree to use an accepted and effective method of contraception (hormonal or barrier methods, abstinence) prior to study entry and for the duration of the study. All patients signed a study-specific consent form prior to registration. The study required IRB approval at participating institutions.
Treatment
Radiation
A total dose of 59.4 Gy in 33 fractions over 7 weeks was delivered with a combination of large initial and cone-down boost field techniques. For the first 45 Gy/25 fractions, the treatment volume included the volume of contrast-enhancing lesion and surrounding edema on pre-operative CT/MRI scan plus a 2 cm margin. If no edema was present, the margin was 2 cm. After 45.0 Gy, the treatment volume included the contrast-enhancing lesion (without edema) on the pre-surgery MRI/CT scan plus a 2 cm margin.
Dalteparin
Drug was initiated on day 1 of radiotherapy at a daily dose of 5000 units subcutaneously (0.2 ml) up to a planned 24 months. At progression patients could continue dalteparin. Concurrent with continuation of dalteparin, patients could have received standard or investigational cytotoxic chemotherapy. Concurrent administration of immunomodulators or cytostatic investigational therapies such as matrix metalloprotease inhibitors or anti-angiogenic agents was not permitted due to the potential to confound any cytostatic effects of the dalteparin.
Duration of treatment
Patients were to continue protocol treatment until: completion of 24 months of dalteparin (dalteparin could be continued beyond 24 months at the discretion of the investigator.); development of a clinically relevant thromboembolic event requiring treatment; an adverse event dictating cessation of treatment at the discretion of the primary investigator; the physician felt that it was in the best interest of the patient to stop treatment; the patient chose to discontinue treatment, became pregnant, was non-compliant, lost to follow-up; the patient developed a clinically relevant prolonged PT or a PTT, or dalteparin-related thrombocytopenia. If a patient discontinued protocol therapy early, they were followed for response until progression and survival for up to 5 years from study entry.
Dose modifications
No dose modifications were allowed.
Supportive care
Tylenol or narcotics could have been used for pain. Non-steroidal anti-inflammatory drugs including aspirin were not allowed during the treatment period.
Patient assessment
An assessment of patient’s tumor status was made at baseline, every 3 months during and following treatment until 2 years from study entry, and then every 6 months until 5 years from study entry. A complete response was defined as disappearance of entire tumor on CT or MRI with the patient off all steroids with a stable or improving neurological exam. The response must have a 4-week duration. A partial response required a 50% reduction (calculating the maximal cross-sectional in two separate axes on stable or decreasing steroids) with a duration of at least 4 weeks. Stable disease was defined as <50% reduction in tumor size, or increases <25%. Progressive disease was defined as a new brain lesion, or progressive neurological deterioration, or a 25% increase in cross-section area of the tumor. Assessments of, including neurological exam, performance status (KPS), overall health, adverse event experience, with special provisions outlined in the protocol for assessment of thromboembolic events [see Appendix IV of the protocol, which is available online (http://www.ecog.org), or at the request of the corresponding author, HIR] were made at baseline, monthly during treatment, at end of treatment, then every 3 months until 2 years from study entry, then every 6 months until 5 years from study entry. Toxicity was graded using the NCI Common Toxicity Criteria (available online: http://www.ctep.cancer.gov). Patients were required to keep drug diaries; syringes were counted by study monitors at patient visits.
Study design and statistical methods
Study design
The primary endpoint of this study was to determine if treatment with dalteparin with conventional radiotherapy improves the median survival in adults with newly diagnosed GBM. Through a collaborative effort, survival data from E1F01 was sent to The RTOG for a historical control analysis. The RTOG RPA has shown that the survival of malignant glioma patients is highly influenced by prognostic factors [age, histology, mental status, KPS, symptom duration, extent of surgery, neurological class, and RT dose] [21]. GBM patients on E1F01 were required to have a KPS of at least 60 (equivalent to an ECOG PS of 0–2), and would therefore fall into RPA classes III, IV, or V, which historically have an MST of 17.9, 11.1, and 8.9 months, respectively [21]. As of the writing of this statistical section the RTOG GBM database contained 1,027 RPA class III through V patients with a breakdown of 20, 49, 31%, respectively. Using the Dixon-Simon method for calculating sample size for the comparison of survival against a historical control [22], a sample size of 68 evaluable RPA class III, IV, and V patients accrued over 6 months followed over an additional 18 months, would ensure at least 80% probability of detecting a minimum of 50% improvement in MST compared with the RTOG glioma database (50% improvement in MST compared with 11 months) at the 0.05 significance level (one-sided). Adjustment for a 5% ineligibility rate resulted in a planned accrual goal of 72 patients.
Secondary endpoints included documenting all toxicities, with special concern for TEE. It was estimated (from the available literature) that over the course of the study 30% of the enrolled patients would develop a thromboembolic event prior to death. With a planned cohort of 72 patients (included all patients as it was a toxicity endpoint), there was 81% power to detect a decrease from 30 to 15% in TEE using a two-sided 0.05 exact test for a single proportion.
Statistical methods
The Kaplan–Meier method was used to estimate time to progression and survival distributions. Confidence intervals for median time to progression and survival were calculated using Greenwood’s formula [23]. Analysis of baseline characteristics and outcome excluded ineligible patients (therefore, n = 42 for these analyses). Toxicity summaries considered all patients who received treatment.
Results
Administrative information
E1F01 opened on May 9, 2002 was suspended on July 11, 2002 due to drug shortage and re-opened on August 8, 2002. With the release of the results from Stupp et al. [24] at the 2004 American Society of Clinical Oncology Meeting introducing temozolomide as standard of care for patients with newly diagnosed GBM, reaching the original accrual goal of 72 patients within a reasonable time-frame was not realistic. After entering 45 of the 72 patients, the study closed in September 2004. Three patients were classified as ineligible [i.e., secondary to: history of DVT/needed treatment for DVT at baseline (n = 2); receiving treatment at baseline which affects clotting time (n = 1)] leaving 42 analyzable patients. Patient characteristics: Table 1 shows the patient characteristics at baseline.
Compliance with dalteparin and radiation
All but 2 of the 42 eligible patients received 59.4 Gy radiation therapy: one patient received 58.6 Gy and the other stopped radiation due to progression and had received 55.8 Gy. Time on dalteparin ranged from 1.2 to 25.4 months, with a median time of 6.3 months. The most common reason for discontinuing dalteparin was progressive disease (see Table 2).
Toxicity
There were no reports of grade 3/4 bleeding or thrombocytopenia related to dalteparin pre- or post-progression. There were local site reactions to dalteparin in up to 71% of patients pre- and post-progression. Two patients experienced, at worst, grade 3 toxicities ascribed to radiation, i.e., headache and depressed level of consciousness. There was a reported 67% incidence of alopecia, and 51% incidence of skin-related reaction (grade 1 or 2); other minor toxicities included hearing disturbance (4%); taste disturbance (4%); nausea/vomiting (15%); neurological disturbance (15%). There were no late (i.e., 90 days post-radiation) grade 3 or 4 radiation toxicities observed; there were four instances of grade 1 or 2 local skin reactions.
Thromboembolic events
Two patients developed TEE while being followed on study; neither patient was receiving dalteparin at the time of the event. No patient developed a TEE while receiving dalteparin.
Response and progression
Tumor decreased by at least 50% (partial response) in 1 patient, disease stabilized in 25 patients, and for 13 patients there was disease progression without a response. Three patients had disease unevaluable for response including: death prior to first tumor evaluation; non-compliant with treatment; no measurements available.
As of the writing of the report, 40 of 42 patients had progressed. Median time to progression was 3.9 months with a 95% confidence interval of 3 to 6 months. Six-month progression free survival was 24%.
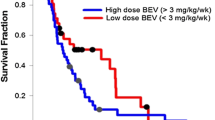
Survival
As of the writing of this report, median survival was 11.9 months with a 95% confidence interval of 10 to 14 months. One patient remains alive at 31.5 months after registration. Of the 41 patients who have died, 91% died due to disease, 7% of medical complications unrelated to therapy and 2% of un-established cause. Figure 1 shows the survival curve.
One question we wished to address in the context of the study was whether there was a difference in survival if a patient stopped dalteparin at first progression versus continued use?
Four patients were excluded from this analysis: 2 of the 42 patients’ disease did not progress and 2 patients stopped dalteparin at least 7 months prior to first progression. Survival was calculated from time of first progression to death or date last known alive. Twenty-two of 38 patients continued dalteparin after first progression. (Note that 4 of these 22 did discontinue after their 2nd or 3rd progressions and are counted as such in Table 2). Median survival for those who stopped dalteparin at first progression versus continuation of drug was 3.2 versus 7.8 months, respectively. Table 3 shows the treatment received at progression, as reported by the institutions, sub-divided by those patients who stopped or continued dalteparin at first progression.
RTOG recursive partitioning analysis
The three RPA classes used in E1F01 were as follows: Class III: age < 50, KPS 90–100;Class IV: age < 50, KPS < 90, or age ≥ 50, KPS 70–100, partial/total resection, normal neuro-function; Class V: age ≥ 50, KPS 70–100, partial/total resection, abnormal neuro-function, or age ≥ 50, KPS 70–100, biopsy only, RT dose > 54.4 Gy, or age ≥ 50, KPS < 70, normal mental status. The distribution of Class III, IV, and V for E1F01 was as follows: 9, 62, 29%, respectively (compared with 20, 49, and 31% in Class III, IV, and V, respectively, in the current RTOG RPA database). Comparing E1F01 to the RTOG database, there was no significant improvement in survival (one sided P-value = 0.47 log rank test).
Discussion
The genesis of this study related to the literature summarized earlier relating anti-proliferate effects to anticoagulation, as well as its putative benefit of LMWH for TEE prophylaxis in GBM patients. Consistent with this, a recent preclinical study [25] linked up-regulated tissue factor expression by wtEGFR and EGFRvIII and the prothrombotic events that occur in the progression of GBM.
To optimally evaluate the potential anti-neoplastic effect of dalteparin in this trial we applied the RTOG RPA analysis. The application of the RTOG RPA analysis provided a systematic comparison of the data obtained in this phase II study to a matched and reproducible historical control [21, 26]. The results derived from this study (see Fig. 1) do not exhibit a substantial difference in comparison to previous RTOG studies of newly diagnosed GBM patients receiving radiation therapy and various adjuvant drugs including BCNU.
It is of interest to note that when this study was designed, investigators were provided the option of continuing dalteparin after disease progression. The rationale for this related to its potential use as an anti-angiogenesis agent, i.e., to slow disease progression, as well as use for deep vein thrombophlebitis (DVT) prophylaxis. Relative to this (as reviewed in results) 22 of 38 patients continued dalteparin post-first progression. Median survival for those who stopped dalteparin at first progression versus continued use was 3.2 and 7.8 months, respectively. This analysis is confounded by several factors and should be interpreted with caution. Patients could receive other treatment at progression, as outlined in the protocol, with or without the continuation of dalteparin. The patients who stopped dalteparin at first progression may have been too sick to receive other treatment. For those patients who continued dalteparin at first progression, their survival could be confounded by the varying lengths that they continued dalteparin and/or by any of the other treatments they received. Table 3 summarizes treatments delivered after disease progression, and suggests an imbalance in active “salvage” therapy employed in the groups.
The secondary endpoint of this study was the development of thromboembolic disease. Relative to this, glioma patients are highly predisposed to thromboembolic phenomena. Brisman and Mendell [10] demonstrated an 8.4% incidence of pulmonary emboli, (which is almost three times the incidence seen in non-malignant neurosurgical patients). Similarly the incidence of DVT in such patients is 27.5% compared to 17% in a control neurosurgical group [11]. Ruff and Posner [27] noted a 31% incidence of confirmed DVT in 264 glioma patients. Sawaya et al. [12] using I-fibrinogen scanning, demonstrated DVTs in 60% of GBM patients; the presence of TEE did not correlate with ambulatory status, time of surgery, length of operation, or occurrence in a paretic limb. Sawaya and Highsmith [13] have suggested malignant brain tumors release a factor responsible for this predisposition to coagulopathy. Previous work suggesting increased platelet adhesiveness in malignant brain tumors is consistent with this supposition [14, 16]. More recent work by Iberti et al. [17] supports the concept of an increased coagulable state of brain tumor patients [17, 18]. Ultimately, as our trial concluded, there were no thromboembolic problems in patients actively receiving dalteparin. As discussed above, the expected incidence in a prospectively followed population of GBM patients should be of the order of ∼30%.
A seemingly contradictory result (in the context of a phase III study) was reported at ASCO [28]. This trial was planned to enroll 512 patients; it closed prematurely (secondary to lack of drug availability) with 186 malignant glioma patients randomized to dalteparin (5,000 U daily) versus placebo. The primary endpoint was the development of TEE. Although there was a trend for LMWH to decrease TEE, it was not statistically significant (HR = 0.7, 95% CL: 0.37–1.5, P = 0.3). There was also a trend for increased bleeding in the LMWH arm. (In our study, we did not encounter any hemorrhagic events.) Even though there was no significant decrease in TEE, the hazard ratio was impressive at 0.7 in favor of the LMWH arm. It remains speculative whether this hazard ratio would have achieved statistical significance if the study had met its accrual objective. Potential noteworthy differences in these studies may relate to patient populations. Our study was restricted to a GBM cohort (as opposed to all malignant glioma) with a usually good performance status, i.e., 95% ECOG P.S. 0 or 1. As more details regarding their study become available there may be other points for conjecture. At present, the results of these studies taken collectively leave the role of anticoagulant thrombo-embolic prophylaxis as unclear for this group of patients. Definitive conclusions regarding the application of TEE prophylaxis strategies will require further investigation.
Abbreviations
- ECOG:
-
Eastern Cooperative Oncology Group
- GBM :
-
Glioblastoma multiforme
- TEE:
-
Thromboembolic events
- LMWH:
-
Low molecular weight heparin
- RTOG:
-
Radiation Therapy Oncology Group
- KPS:
-
Karnofsky Performance Status
- RPA:
-
Recursive partitioning analysis
- DVT:
-
Deep vein thrombophlebitis
- MST:
-
Median survival time
References
Siragusa S, Cosmi B, Piovella F, Hirsh J, Ginsberg S (1996) Low-molecular-weight heparins and unfractionated heparin in the treatment of patients with acute venous thromboembolism: results of a meta-analysis. J Am Med 100:269–277
Folkman J, Langer R, Linhardt RJ, Haudenschild C, Taylor S (1983) Angiogenesis inhibition and tumor regression caused by heparin or a heparin fragment in the presence of cortisone. Science 221:719–725
Norrby K (1993) Heparin and angiogenesis: A low-molecular-weight fraction inhibits and a high-molecular-weight fraction stimulates angiogenesis systemically. Haemostasis 23(suppl 1):141–149
Bitan M, Mohsen M, Levi E, Wygoda MR, Miao H, Lider O, Svahn CM, Ekre HP, Ishai-Michaeli R, Bar-Shavit R, Vlodavsky I, Peretz T (1995) Structural requirements for inhibition of melanoma lung colonization by heparanase inhibiting species of heparin. Isr J Med Sci 31:106–118
Collen A, Smorenburg SM, Peters E, Lupu F, Koolwijk P, van Noordan C, van Hinsbergh VWM (2000) Unfractionated and low molecular weight heparin affect fibrin structure and angiogenisis in vitro. Cancer Res 60:6196–6200
Castellot Jr JJ, Choay J, Lormeau J, Petitou M, Sache E, Kamovsky MJ (1986) Structural determinants of the capacity of heparin to inhibit the proliferation of vascular smooth muscle cells. II. Evidence for a pentasaccharide sequence that contains a group. J Cell Biol 102:1979–1984
Teicher BA, Holden SA, Ara G, Dupuis NP, Liu F, Yuan J, Ikebe M, Kakeji Y (1995) Influence of an anti-angiogenic treatment on 9L gliosarcoma: oxygenation and response to cytotoxic therapy. Int J Cancer 61:732–737
Wachsberger P, Burd R, Dicker AP (2003) Tumor response to ionizing radiation combined with antiangiogenesis or vascular targeting agents. Clin Cancer Res 9:1957–1971
Dunn IF, Hesse O, Black PM (2004) Growth factors in glioma angiogenesis: FGFs, PDGF, EGF, and TGFs. J Neurooncol 50:121–137
Brisman R, Mendell J (1973) Thromboembolism and brain tumor. J Neurosurg 38:337–338
Kayser-Gatchalian MC, Kayser K (1975) Thrombosis and intracranial tumors. J Neurol 209:217–224
Sawaya R, Zuccarrello M, Elkalliny M, Nishiyama H (1992) Postoperative venous thromboembolism and brain tumors: Part I. Clinical profile. J Neurooncol 14:119–125
Sawaya R, Highsmith RF (1992) Postoperative venous thromboembolism and brain tumors: Part III. Biochemical profile. J Neurooncol 14:113–118
Nathanson M, Savitsky JP (1952) Platelet adhesive index studies in multiple sclerosis and other neurological disorders. Bull N Y Acad Med 28:462–468
Marras LC, Geerts WH, Perry JR (2000) The risk of venous thromboembolism is increased throughout the course of maligant glioma. Cancer 89:640–646
Millac P (1967) Platelet stickiness in patients with intracranial tumors. BMJ 4:25–26
Iberti TJ, Miller M, Abalos A, Fischer EP, Post KD, Benjamin E, Oropello JM, Wiltshire-Clement M, Rand JH (1994) Abnormal coagulation profile in brain tumor patients during surgery. Neurosurgery 34:389–395
Hamilton MG, Hull RD, Pineo GF (1994) Venous thromboembolism in neurosurgery and neurology patients: a review. Neurosurgery 34:280–296
Sawaya R, Highsmith RF (1988) Brain tumors and the fibrinolytic enzyme system. In: Kornblith PL, Walker MD (eds) Advances in neuro-oncology. Gutura, Mount Kisco, pp 103–157
Shlebak AA, Smith DB (1997) Incidence of objectively diagnosed thromboembolic disease in cancer patients undergoing cytotoxic chemotherapy and/or hormonal therapy. Cancer Chemother Pharmacol 39:462–466
Curran WJ Jr, Scott CB, Horton J, Nelson JS, Weinstein AS, Fishbach AJ, Chang CA, Rotman M Asbell SO, Krisch RE, Nelson DF (1993) Recursive partitioning analysis of prognostic factors in three Radiation Therapy Oncology Group malignant glioma trials. J Natl Cancer Inst 85:704–710
Dixon DO, Simon R (1998) Sample size considerations for studies comparing survival curves using historical controls. J Clin Epidemiol 41:1209–1231
Kaplan EL, Meier P (1958) Nonparametric estimation from incomplete observations. J Am Stat Assoc 53:457–481
Stupp R, Mason WP, Van Den Bent MJ, Weller M, Fisher B, Taphoorn M, Brandes AA, Cairncross G, Lacombe D, Mirimanoff RO (2004) Concomitant and adjuvant temozolomide and radiotherapy for newly diagnosed glioblastoma multiforme. Conclusive results of a randomized phase III trial by the EROTC Brain & RT groups and NICIC Clinical Trials Group. Proc Am Soc Clin Oncol 23:1 (abstract #2)
Rong Y, Durden DL, Van Meir EG, Brat DG (2006) Differential regulation of tissue factor expression by EGFR and EGFRvIII in GBM. Neurooncology 8:401
Seiferheld W, Mehta MP, Delrowe J,MacDonald D, Langer C, Scott C, Currqan WJ, Alfered Yung WK (2002) Five years of glioblastoma multiforme (GBM) phase II trials at the RTOG. Proc Am Soc Clin Oncol 21:71a (abstract #281)
Ruff RL, Posner JB (1983) Incidence and treatment of peripheral venous thrombosis in patients with glioma. Ann Neurol 13:334–336
Perry JR, Rogers L, Laperrier N, Julian J, Geerts W, Agnelli G, Malkin M, Sawaya R, Baker R, Levine M (2007) PRODIGE: a Phase III randomized placebo-controlled trial of thromboprophylaxis using dalteparin low molecular weight heparin (LMWH) in patients with newly diagnosed malignant glioma. J Clin Oncol 25:77s (Abstr 2011)
Acknowledgments
This study was conducted by the Eastern Cooperative Oncology Group (Robert L. Comis, M.D., Chair) and supported in part by Public Health Service Grants CA23318, CA66636, CA21115, CA21076, CA13650; RTOG U10 CA21661, CCOP U10 CA37422, and Stat U10 CA32115 grants from the National Cancer Institute, National Institutes of Health and the Department of Health and Human Services. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Cancer Institute, Kathleen Reader Memorial Research Fund. Dalteparin was supplied by Pfizer (formerly Pharmacia).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Robins, H.I., O’Neill, A., Gilbert, M. et al. Effect of dalteparin and radiation on survival and thromboembolic events in glioblastoma multiforme: a phase II ECOG trial. Cancer Chemother Pharmacol 62, 227–233 (2008). https://doi.org/10.1007/s00280-007-0596-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-007-0596-3