Abstract
In recent years, an explosion of novel agents has shifted the treatment paradigm for patients with acute myeloid leukemia. The optimal place in therapy for many of these novel agents remains unknown due to limited guidance from national guidelines and the way these agents were studied prior to entering the market. A critical evaluation of the literature and incorporation of oncology stewardship principles can be helpful in determining an optimal place for these agents while being mindful of the overall cost that is associated with therapies. The purpose of this review is to critically evaluate the efficacy and safety data for five controversial agents and provide examples of the use of stewardship practices in determining their place in the treatment of acute myeloid leukemia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the last 50 years, the armamentarium for the management of acute myeloid leukemia (AML) has been limited. Since the introduction of standard-dose cytarabine and an antracycline (7 + 3) induction therapy in 1973, there have been a small number of agents that have demonstrated a survival benefit for the treatment of this disease[1]. Furthermore, since the 1990s, the survival curve for patients with AML has been essentially stagnant [2]. The introduction of anti-mold prophylaxis, dose optimization of daunorubicin to 90 mg/m2, and high-dose cytarabine (HIDAC) consolidation are among the few treatment modalities that have improved survival [3,4,5]. While 7 + 3 induction therapy results in remission rates of 60–70% in patients 60 years old or younger, many patients relapse, usually within a median of 4 to 10 months [6,7,8]. The 5-year survival rate for patients with AML is poor at approximately 28.7%, and outcomes in the relapsed/refractory (R/R) setting are even worse [2].
Over the last 3 years, there have been a myriad of new agents entering the market, thus providing increased options for patients based on disease characteristics. From 1969 to 2020, 16 drugs were approved for the treatment of AML, of which more than half have been approved since 2017 (Fig. 1). While the explosion of new approvals is encouraging, the optimal place in therapy for these therapeutics has not been solidified. The National Comprehensive Cancer Network (NCCN) AML guidelines provide a menu of the currently available therapies, with limited recommendations for use of one agent over another [9, 10]. While the NCCN guidelines do denote when treatments listed are based on category 1 level evidence (defined as uniform consensus, based on a high level of evidence), this designation does not account for limitations in study design that may limit the external validity of individual study findings [9]. The European Society for Medical Oncology (ESMO) guidelines provide levels of evidence (trial, cohort studies, case–control studies, expert opinion) and grades (quality of evidence and magnitude of benefit) for each recommendation, and in instances where there are multiple novel drug combinations, it does prioritize some recommended treatments. Nonetheless, it also fails to account for significant study design limitations that may impact the applicability of results for some of the agents recommended [10]. At the individual patient level, a thorough evaluation of available literature is necessary to ensure the most efficacious and safe therapies are chosen. At the global level, critically evaluating the literature to determine place in therapy provides the opportunity for providers to shape demand of therapeutics, as demonstrated by oncologists at Memorial Sloan Kettering [11, 12]. In this instance, oncologists released a public statement about their refusal to utilize ziv-aflibercept for colorectal cancer based on similar efficacy with lower tolerability and increased cost compared to standard of care bevacizumab, and subsequently the price of ziv-aflibercept was decreased.
Globally, drug prices are rising, with the wholesale acquisition costs (WAC) of recently approved AML therapeutics ranging from $20,000 to more than $100,000. The wholesale acquisition cost is the price paid by a wholesaler to drug manufacturers and does not reflect discounts or rebates negotiated by private payers. The WAC is generally applicable and publicly available and therefore will be used throughout this review to assess financial impact of novel therapies. The high costs of newly approved therapies do not correspond to improved survival outcomes, as reflected by a cost–benefit analysis conducted by Vokinger et al. [13]. Healthcare providers therefore have a responsibility to utilize their expertise to shape demand and by doing so create an incentive for the industry to decrease drug prices. This responsibility starts with an in-depth evaluation of the quality of the evidence brought forth for incorporation of new agents.
We define oncology stewardship as a set of coordinated strategies to improve the use of antineoplastic agents with the goal of enhancing patient outcomes while reducing financial toxicity. The purpose of this review is to apply the principles of oncology stewardship to critically evaluate the efficacy and safety data that contributed to the approval of five controversial agents in the upfront treatment of AML within the context of specific disease subtypes to ultimately identify the appropriate place in therapy, if any, for these agents. This review is not all inclusive or comprehensive, but rather these same principles can be applied to other classes of medications not covered in this review, including isocitrate dehydrogenase (IDH) inhibitors and FMS-like tyrosine kinase 3 (FLT3) inhibitors, and the treatment of R/R AML.
Core binding factor (CBF) AML
Patient case
A 54-year-old woman presented to her local hospital with right-inguinal pain. A complete blood cell count revealed a white blood cell count (WBC) of 23 K/µL, thrombocytopenia, and the presence of 40% blasts. The patient was transferred to a larger academic medical center where a bone marrow biopsy was performed which revealed 100% cellularity with 65% myeloid blasts, consistent with AML. Fluorescent in situ hybridization (FISH) was also performed and revealed a RUNX1T1/RUNX1 fusion gene indicating the presence of a t(8;21)(q22;q22) translocation which was later confirmed via conventional cytogenetics. The patient was deemed fit for intensive induction, and the experienced hematologist on service recommended induction with daunorubicin 90 mg/m2 and cytarabine 100 mg/m2 in “7 + 3” fashion. The hematology fellow recommended the addition of gemtuzumab ozogamicin per the newest NCCN guideline recommendations. Should the seasoned attending “GO with the flow” and incorporate this novel agent in the treatment of CBF AML?
CBF AML is defined as inv(16), t(16;16), or t(8;21), irrespective of blast count [14]. Among patients with AML, those with CBF AML have the most favorable outcomes. For patients with CBF AML receiving optimal treatment with 7 + 3 (daunorubicin 90 mg/m2) followed by HIDAC consolidation, outcomes look relatively advantageous, with long-term overall survival (OS) rates ranging from 65 to 85% [4, 15, 16].
Gemtuzumab ozogamicin
Gemtuzumab ozogamicin (GO) is an antibody drug conjugate of an anti-CD33 antibody covalently attached to calicheamicin, a cytotoxic antibiotic agent [17]. CD33 is expressed on up to 90% of AML blasts [18, 19]. After the conjugate binds CD33, it is rapidly internalized, releasing ozogamicin which binds to the minor groove of DNA, inducing double-strand cleavage and subsequent apoptosis [20].
Gemtuzumab ozogamicin received accelerated FDA approval based on a 30% overall response rate demonstrated in phase 2 studies in relapsed AML, with confirmatory phase 3 data pending [21, 22]. The SWOG S0106 study randomized newly diagnosed patients to 7 + 3 with or without gemtuzumab 6 mg/m2 on day 4 [23]. Considering the patient population included in this study was 18–60 years old and the demonstrated overall survival benefit to utilizing 90 mg/m2 of daunorubicin in patients up to age 65, the anthracycline dose utilized in both arms of this study was suboptimal (daunorubicin 60 mg/m2 in the 7 + 3 arm and 45 mg/m2 in the 7 + 3 + GO arm) [4, 24]. The CR rate was 69% with GO versus 70% without GO (p = 0.59) and the 5-year OS rate was 46% with GO versus 50% without GO (p = 0.85). Median OS was 41 months for the arm that incorporated GO and 61 months for the standard of care arm (p = 0.59). Furthermore, there was a significantly higher rate of early mortality in patients who received GO with 17 deaths within 30 days, versus only 4 deaths in patients who did not receive GO. The study was prematurely closed due to no difference in CR rates and a higher incidence of fatal toxicities in the GO arm. The drug was subsequently removed from the market in June 2010 due to lack of benefit and increased induction mortality.
In 2014, a meta-analysis was published which included five randomized trials conducted from 2002 to 2010, where GO was given in combination with intensive induction chemotherapy (Table 1) [25]. While there was no difference in overall survival among all patients (5-year overall survival 35.6% vs 32.2%), adding GO to induction chemotherapy led to a significant improvement in overall survival specifically for patients with favorable risk cytogenetics (5-year overall survival 55.2% without GO vs 76.3% with GO; HR 0.47, p = 0.0005). The survival rate in patients with favorable risk cytogenetics who did not receive GO in this pooled analysis, however, is much lower than historically reported survival rates with standard chemotherapy of 65–85% [15, 16]. In addition, patients with favorable risk cytogenetics made up a very small proportion of the population analyzed across studies, ranging from 3 to 16% in the studies that included favorable risk patients [23, 26,27,28]. Most significantly, one study only included patients with intermediate-risk cytogenetics [29]. The ESMO guidelines acknowledge that GO dosing recommendations are derived from ALFA-0701 and that because of its inclusion of only 9 patients with favorable risk cytogenetics in the study, the optimal dosing for efficacy is unknown [10]. Furthermore, the definition of favorable risk cytogenetics varied considerably between the studies as some studies only included those with core binding factor AML as favorable risk, whereas others incorporated molecular markers. Based on the 2017 ELN criteria, patients with NPM1 mutations without FLT3-ITD mutations are considered favorable risk [30]. However, of the patients included in the meta-analysis, less than half had NPM1 mutation data available. Subgroup analyses should never be more than hypothesis generating results that are subsequently studied in a homogeneous population that is appropriately randomized given that, unless stratification occurs as part of study methodology, the subgroups do not represent a randomized sample with regard to patient and disease characteristics. To complicate things further, the differing definitions of favorable risk across studies create a heterogeneous subgroup to evaluate benefit in. Additional limitations of these studies include the chemotherapy backbones and consolidation regimens utilized (Table 1). Induction regimens included variations of 7 + 3 such as 10 + 3, and additional agents such as etoposide which has not demonstrated additional benefit in AML [31, 32]. HIDAC consolidation was not standard in all of these studies, which has previously demonstrated a survival benefit in patients with CBF AML [33]. Furthermore, among those that did include HIDAC consolidation, the number of cycles was less than the standard 3–4 cycles of HIDAC consolidation, which has demonstrated a benefit over 0–2 cycles in patients with CBF AML [34,35,36]. Altogether, the signal from this collection of studies is not sufficient to argue for the addition of GO to treatment for young, favorable-risk patients.
ALFA-0701 was the only study included in the meta-analysis where an overall survival benefit was observed in the subgroup of patients with favorable-risk cytogenetics. This was an open-label phase 3 study that randomized treatment-naïve patients to 7 + 3 with or without GO [28]. Only 3% of patients had favorable-risk cytogenetics (n = 9), which was defined as patients with core binding factor leukemia. Overall survival was not significantly different among patients with favorable-/intermediate-risk cytogenetics who received GO compared to the control arm, HR 0.59 (95% CI 0.32–1.09). While this initial analysis, with a median follow-up period of 14.8 months, demonstrated a statistically significant 2-year survival benefit with GO for the entire group (53.2% with GO versus 41.9% without; HR 0.69, p = 0.0368), in the final analysis of the data, the survival benefit with the addition of GO was lost (median follow-up of 47.6 months in the GO arm and 41 months in the control arm) [28, 37]. The long-term follow-up results of the ALFA-0701 study were not included in the meta-analysis due to contractual arrangements with the supplying company [25]. This demonstrates the importance of long-term follow-up to confirm outcomes when incorporating novel therapies into practice. With the loss of a survival benefit in the long-term follow-up, there are zero randomized trials demonstrating an OS benefit with GO. Nonetheless, in September 2017, GO was re-approved by the FDA for patients with CD33 + de novo or R/R AML.
Along with an unproven benefit in efficacy, the addition of gemtuzumab to intensive chemotherapy also represents an increased risk of toxicity. In the AML15 study, the dose of idarubicin was decreased due to prolonged thrombocytopenia, which the authors did not attribute to GO [32]. However, in a separate publication, the authors report that patients who received GO had a significantly higher platelet transfusion requirement (mean 18.9 units versus 13.7 units) [27]. Furthermore, gemtuzumab is associated with a significant safety concern for veno-occlusive disease/sinusoidal obstruction syndrome (VOD/SOS). The mechanism of GO-induced sinusoidal damage is thought to be secondary to unconjugated calicheamicin because the hydrolyzable linker is relatively unstable and CD33-mediated uptake by cells of the liver which express CD33, including Kupffer cells, sinusoidal epithelial cells, and stellate cells [38, 39]. In ALFA-0701, 6 patients in the GO group developed VOD/SOS (4.6%), including 2 patients in which the complication was fatal. While 2 patients in the control arm also experienced VOD/SOS, both of these patients actually received GO during the follow-up phase of the study, as part of a compassionate use program [37].
Recommendations for use
Guidelines support the use of GO upfront in patients with favorable-risk (NCCN, ESMO: CBF, optional for other favorable) or intermediate-risk (NCCN, ESMO: optional) disease who can tolerate intensive induction and for those without actionable mutations who cannot tolerate intensive induction (NCCN) [9, 10]. A thorough review of currently available literature does not support the role of GO in any setting and in fact suggests that this addition may result in increased toxicity and increased costs (Table 3). The findings of the meta-analysis are hypothesis generating. The role of GO should be explored in CBF AML patients, in a randomized controlled trial compared to standard of care, including standard of care dosing of daunorubicin and up to 4 cycles of HIDAC consolidation. A proposed treatment algorithm for newly diagnosed patients able to tolerate intensive induction, including CBF AML, is provided in Fig. 2. Of note, the ESMO guidelines recommend cytarabine 1.5 g/m2 for patients age < 60–65 years and 1 g/m2 for patients ≥ 60–65 years based on a review published in 2013 [10, 40]. However, significant limitations exist to the data presented in the review, including the use of double induction, additional agents in consolidation (i.e., mitoxantrone), and HIDAC courses with much higher total doses (20–36 g/m2 for each course of consolidation) [41, 42]. The authors of this review acknowledge that cytarabine dosing and number of consolidation courses are controversial, but outcomes with HIDAC 3 g/m2 Q12h for 3 days (dose adjusted for age) are favorable [43].
Unfavorable risk cytogenetics and TP53-mutated AML
Patient case
A 51-year-old man with no significant past medical history presented to his primary care physician with 2–3 weeks of intermittent fevers, mild epistaxis, sore throat, and malaise. A CBC was drawn which revealed a WBC count of 82.5 K/µL and 12% blasts. Given concern for AML, a bone marrow biopsy was performed and showed 95% cellularity with 45% myeloid blasts. Conventional cytogenetics revealed a complex karyotype. The hematology/oncology fellow recommended the use of HMA and venetoclax, citing a podcast he recently listened to that discussed the use of this combination in patients with complex cytogenetics. Is this the most appropriate treatment for this patient?
Complex cytogenetics and TP53 mutations are independent predictors of poor survival outcomes in patients with AML [44]. Despite the dismal outcomes in these patients, available novel therapies have not demonstrated significant improvements in survival outcomes. Current guidelines recommend enrollment in a clinical trial for patients with TP53 mutations or complex cytogenetics [14].
Hypomethylating agents (HMA)
While hypomethylating agents have been approved since the early 2000s, a brief discussion on HMA monotherapy is warranted for a comprehensive understanding of their use in combination with newly approved agents. Azacitidine and decitabine are cytidine analogs which are incorporated into DNA, and RNA in the case of azacitidine. The compounds limit DNA methylation through irreversible binding to DNA methyltransferases (DNMT) after incorporation into newly synthesized DNA. Hypomethylation allows for the expression of previously methylated and silenced genes necessary for tumor suppression and cancer cell differentiation [45, 46].
A study by Welch et al. is often cited as support for the use of decitabine in patients with TP53 mutations [47]. The authors conducted a prospective, uncontrolled single-arm study to determine whether any mutations correlated with response to decitabine. Patients with AML who were age ≥ 60 years, relapsed AML, or transfusion-dependent MDS were included and received a 10-day course of decitabine. The authors demonstrated an overall response rate (CR, complete remission with incomplete count recovery, morphologic complete remission) in 21 of 21 patients (100%) with TP53 mutations, compared to only 32 of 78 patients (41%) who were wild-type. TP53 acts as a tumor suppressor, important for regulating cellular response to DNA damage and other stressors [48]. Loss of function TP53 mutations result in the loss of tumor suppressor activity. Theoretically, hypomethylating agents may be favorable for TP53 mutations as it inhibits methyltransferase, thereby allowing the expression of tumor suppressor genes. However, the 100% response rate with decitabine in patients with TP53 mutations should be interpreted with caution. Based on the author’s definition of overall response, patients with an ablated marrow were included in the response rate. Including only patients with a CR/CRi, the response rate was 62% in patients with TP53 mutations, which while lower than 100% was still higher than that demonstrated with wild-type. Furthermore, only a very small number of patients included in the study had TP53 mutations (21/116, 18%). This total N is further reduced as 9 patients (43%) with TP53 mutations had MDS rather than AML. It is difficult for any conclusions to be more than hypothesis generating due to the small sample size. Furthermore, durability is not well described and therefore conclusions on duration of response cannot be made.
HMA and Venetoclax therapy
Venetoclax inhibits the anti-apoptotic protein BCL2. In normal cells, in response to an apoptotic signal, BH3 proteins bind to anti-apoptotic proteins, resulting in the release of mediators of apoptosis, including BAX and BAK, leading to mitochondrial outer membrane permeabilization and the release of cytochrome c, ultimately triggering apoptosis [49]. Venetoclax is thought to have activity in cells that have a relative dependence on BCL2 for survival, as in some AML cells [50, 51].
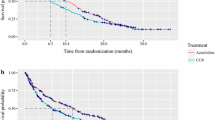
Combination azacitidine and venetoclax was compared to azacitidine and placebo in a randomized, double blind, placebo-controlled, multicenter, phase 3 study [52]. Patients with newly diagnosed AML who were considered ineligible for standard induction therapy due to coexisting conditions or age above 75 were included. Median OS was 14.7 months with venetoclax compared to 9.6 months with azacitidine monotherapy (p < 0.001). Complete remission was achieved in 36.7% and 17.9% of patients, and the duration of complete remission was 17.5 months and 13.3 months in the venetoclax and azacitidine monotherapy groups, respectively. Outcomes in patients with poor-risk cytogenetics were poor in both groups with a median OS of 7.6 months with venetoclax and 6.6 months with azacitidine monotherapy, indicating a need for more optimal therapy in these patients. Specifically for patients with TP53 mutations, the CR/CRi rate was 55.3% with venetoclax versus 0% with azacitidine alone, a stark contrast to the 100% response rate demonstrated with single agent decitabine discussed previously [47]. This is unlikely attributable to inherent differences between azacitidine and decitabine, but rather highlights the limitations of drawing conclusions in the setting of a small sample size. In the venetoclax arm, 72% of patients had treatment interruptions related to adverse events, compared to 57% with azacitidine monotherapy. Furthermore, 53% of venetoclax patients had dose interruptions, including delays and a reduction from 28 to 21 days of venetoclax per cycle, compared to only 28% of placebo patients, indicating there is room to optimize the venetoclax dosing strategy.
A recently published single-center, phase 2 trial reported on outcomes with the use of combination decitabine and venetoclax [53]. Similarly to the azacitidine/venetoclax study, patients with newly diagnosed AML who were considered ineligible for intensive induction were included, in addition to patients with untreated or treated secondary AML, and R/R AML. Among patients with newly diagnosed AML, 47% had poor-risk cytogenetics and 30% had TP53 mutations. The response rate was 89% and median OS was 18.1 months in newly diagnosed patients. Because of the success reported with decitabine in TP53 mutations, the combination of an HMA with venetoclax has subsequently been explored in this population. Kim et al. performed a post hoc analysis of patients with TP53 mutations versus wild-type who received frontline decitabine and venetoclax as part of the phase 2 trial and also compared outcomes to a historical control who received single agent decitabine [54]. Patients with TP53 mutations were found to have significantly worse outcomes compared to wild-type, with a CR/CRi rate of 57% versus 77% and median OS of 5.2 months versus 19.4 months. Furthermore, venetoclax-based combination demonstrated no improvement in survival for patients with TP53 mutations, with a median OS of 5.2 months, compared to 4.9 months with 10-day decitabine alone.
Poor outcomes with venetoclax-based combinations in patients with TP53 mutations were again demonstrated by DiNardo et al., who included patients who received an HMA or LDAC and venetoclax treated on 1 of 2 clinical trials and tried to correlate molecular markers and response [55]. The authors found that roughly 1/3 of primary refractory patients and 1/3 of relapsing patients had TP53 mutations. Furthermore, they identified TP53 mutations as one of the primary resistance mechanisms for patients treated with venetoclax-based combinations.
Based on data supporting worse outcomes in patients with a higher FLT3-ITD allelic ratio, Short et al. explored prognosis with mutant TP53 variant allelic frequency (TP53mut VAF) [56]. The authors found that TP53mut VAF > 40% was associated with significantly worse overall survival, and survival was poor for these patients regardless of treatment strategy. However, patients with TP53mut VAF ≤ 40% treated with a cytarabine-based regimen had significantly better OS compared to those treated with an HMA-based regimen, with a 1-year OS rate of 44% vs 31%, p = 0.04. While this is limited to a retrospective, single-center analysis, it highlights the potential role of incorporating TP53mut VAF into treatment decisions and the need for improved novel therapies in this poor-risk group.
The combination of HMA and venetoclax is increasingly being used in young, fit patients, especially those with poor risk cytogenetics or TP53 mutations [57,58,59,60,61]. Extrapolating these data to young, fit patients is not consistent with the population included in either the combination or single-agent HMA studies. This is particularly important as it is unknown how deep the remissions are long-term. Outcomes with cytarabine and high-dose daunorubicin in young patients overall are very favorable, with a median OS of 34.3 months [4]. While no prospective, head-to-head comparative data is available for intensive chemotherapy versus HMA combinations, particularly for patients with poor-risk cytogenetics, outcomes with intensive chemotherapy in TP53-mutated AML look comparable, with CR rates up to 55% and median OS of 6.8 months [62]. A retrospective, propensity score–matched analysis suggested improved overall survival in patients treated with decitabine and venetoclax compared to intensive chemotherapy, with a median OS 12.4 months vs 5.0 months in patients overall [63]. Patients in the decitabine and venetoclax arm were all treated on the phase 2 trial previously discussed and were therefore considered ineligible for standard induction chemotherapy [53]. Despite inclusion in the intensive therapy arm, as these patients were propensity score matched, they were also older, less fit patients. As intensive chemotherapy is the standard of care, it is on the burden of HMAs and venetoclax to prove superiority over intensive chemotherapy. Previous attempts to extrapolate what has worked in older patients to younger patients have been unsuccessful, as demonstrated with CPX-351 [64, 65].
Recommendations for use
The authors support the frontline use of HMA in combination with venetoclax for patients unable to tolerate intensive therapy. The definition of an unfit patient varies widely among study inclusion criteria. The NCCN guidelines delineate treatment options based on age less than or greater than 60. This arbitrary cutoff for “intensity of therapy” is at odds with the majority of the clinical trials which utilize an age of 75 or identify certain comorbidities that would make a patient ineligible for chemotherapy. In this review, we define a patient to be ineligible for intensive induction based on performance status and treatment goals (i.e., ability to proceed to a curative allogeneic hematopoietic cell transplant). Currently, there is no data to prefer low-intensity therapy in young, fit patients. Novel therapies are needed, specifically for patients with poor-risk disease such as TP53 mutations where outcomes are poor with currently available modalities. A summary of treatment recommendations for patients with unfavorable risk cytogenetics or TP53 mutations is provided in Fig. 3.
Not candidate for intensive remission induction therapy
Patient case
An 82-year-old woman with a past medical history of hypothyroidism and hyperlipidemia presented to her primary care physician for an itchy rash and sore throat. Labs were notable for WBC 56.9 K/µL with 23% blasts and serum creatinine of 1.37 mg/dL. A bone marrow biopsy was performed and showed 80% cellularity with 60% myeloid blasts. Cytogenetic analysis demonstrated 46,XX [20] and molecular diagnostics were as follows: negative for FLT3 ITD, FLT3 D835, IDH1/IDH2 mutations, and positive for NPM1 mutation. Given her age and comorbidities, she was determined not to be a candidate for intensive chemotherapy or allogeneic hematopoietic cell transplant (AlloHCT). Which treatment option would you favor for this patient?
Gemtuzumab ozogamicin
The use of GO has also been studied in older patients ineligible for intensive chemotherapy, in a sequential phase II/III study comparing GO monotherapy to best supportive care [66]. Best supportive care consisted of transfusions, antimicrobials, hydroxyurea, and other medications per institutional guidelines. Patients were included if they were greater than 75 years old or age 61–75 with a WHO performance status (PS) above 2 or unwilling to receive standard chemotherapy. Of note, 35.9% of patients were age 61–75, and overall, only 7.1% of patients had a WHO PS greater than 2. Despite an unfair comparator arm, median OS was 4.9 months for patients who received GO versus 3.6 months for best supportive care. By essentially doing nothing, the difference in overall survival was only 1.3 months.
Recommendations for Use
It is troubling that despite this data confirming there is no overall survival benefit to incorporating GO in regimens utilized for treatment-naïve AML, the FDA approval for this potentially toxic and expensive agent has been unchanged and its use continues to be endorsed by NCCN guidelines, cementing its use in practice, and increasing cost of care without providing incremental and meaningful benefit to patients [9]. It is however reassuring that the ESMO guidelines do not support the use of GO for patients ineligible for standard chemotherapy [10].
Glasdegib
Glasdegib is an oral, small molecular hedgehog pathway inhibitor, which binds to and inhibits smoothened, a transmembrane protein involved in hedgehog signal transduction [67].
Glasdegib received FDA approval in combination with low-dose cytarabine (LDAC) in adult patients with AML who cannot tolerate intensive induction either due to age 75 years or older or comorbidities based on the results of BRIGHT AML 1003 [68]. BRIGHT AML 1003 was an open-label, multicenter, phase 2 study which randomized adults age ≥ 55 years with untreated AML or high-risk MDS to low-dose cytarabine with or without glasdegib. Median overall survival was significantly higher with glasdegib at 8.8 months, compared to 4.9 months with single-agent LDAC (HR 0.51, p = 0.0004). However, in patients with poor-risk cytogenetics, median overall survival was not improved with the addition of glasdegib at 4.7 months, compared to 4.9 months with single-agent LDAC. Furthermore, median treatment duration was only 2.7 months with combination LDAC and glasdegib and 1.5 months with single-agent LDAC. Subsequent systemic therapy including HMA or chemotherapy was received in 44% of glasdegib/LDAC patients and 36.6% of LDAC patients. Based on duration of study therapy received, the numerically higher rate of subsequent therapy in the glasdegib group likely contributed to the higher overall survival observed. In addition, LDAC is not an adequate comparator arm as we know patients have poor outcomes with LDAC and with the advent of contemporary treatment options such as HMA and venetoclax have largely replaced the use of LDAC in older patients or those with comorbidities who cannot tolerate intensive induction therapy.
Subsequently, the long-term results of the BRIGHT AML 1003 study were published, with an additional 20 months of follow-up [69]. In a post hoc analysis of patients with sAML, median overall survival was significantly improved with glasdegib at 9.1 months versus 4.1 months with LDAC alone (p < 0.0001). Among the patients with sAML, only 25% in each arm received prior azacitidine, which is likely reflective of the time period this study was conducted. Nonetheless, median OS was decreased at 7.1 months with glasdegib in patients who received prior HMA. Furthermore, median OS was 7.4 months with glasdegib for patients with sAML who did not receive subsequent HMA. Based on this, it seems that the small benefit with glasdegib over LDAC in sAML is likely due to subsequent therapy with an HMA.
Recommendations for use
Despite the inclusion in the NCCN guidelines and approval by the European Medicines Agency (EMA) for patients without actionable mutations unable to tolerate intensive therapy, the authors do not support the use of glasdegib as it did not demonstrate any additional benefit compared to historical treatment options. The HMA/venetoclax data previously discussed would apply to this patient and should be considered for patients unable to tolerate intensive therapy.
Secondary AML
Patient case
A 70-year-old man sought evaluation from his primary care physician after 12 months of fatigue worsening, dyspnea on exertion, and 30 lbs weight loss. A CBC was drawn and showed a hemoglobin of 6.4 g/dL, WBC count of 1.8 K/µL, and platelets of 262. A bone marrow evaluation revealed 12% blasts and morphology consistent with a myelodysplastic syndrome (MDS-EB2). The patient was started on azacitidine and achieved a response. After 12 cycles without complications, the patient developed pancytopenia and subsequent bone marrow biopsy was consistent with evolution to AML. His hematologist recommended induction with liposomal daunorubicin and cytarabine (CPX-351). The patient presents to your institution for a second opinion.
The incidence of secondary AML (sAML) is 5–25% among patients with AML. Secondary AML consists of therapy-related AML, AML arising from an antecedent hematologic disorder, and AML with myelodysplastic related changes (AML-MRC). AML-MRC is defined as multilineage dysplasia (≥ 50% dysplastic cells in ≥ 2 cell lines), a prior history of myelodysplastic syndrome (MDS), or myelodysplastic/myeloproliferative neoplasm (MDS/MPN), or specific cytogenetic abnormalities, per the 2016 revision to the World Health Organization classification [70]. Compared to de novo AML, patients with sAML have an inferior RFS and OS [71, 72]. The specific prognosis of patients with AML-MRC subcategory of sAML differ based on whether this classification is made based on morphology alone or due to specific cytogenetic abnormalities or a known antecedent diagnosis of a bone marrow failure disorder consistent with the designation. A retrospective study evaluating outcomes based on AML-MRC diagnostic criteria demonstrated that patients with multilineage dysplasia alone had significantly better survival outcomes compared to those with specific cytogenetic abnormalities [73]. Table 2 describes the efficacy of available treatment options for secondary AML.
CPX-351
CPX-351 is a liposomal encapsulation of cytarabine and daunorubicin that maintains the most optimal synergistic 5:1 ratio of cytarabine to daunorubicin, as identified by in vitro studies [74]. Multi-drug resistant protein 1/ P-glycoprotein (MDR1/P-gp) overexpression in leukemia cells and resulting drug substrate efflux is a well-demonstrated mechanism of chemotherapy resistance in AML, and MDR1 expression increases with age [75, 76]. P-gp expression is more common in secondary AML, compared to de novo AML [77]. Reduced accumulation of daunorubicin in AML blast cells in vitro has been demonstrated with high P-gp expression [78]. Theoretical advantages of the liposomal formulation are preferential accumulation of the drug in the bone marrow and the ability to overcome resistance mechanisms such as P-gp efflux, although presumably once the daunorubicin is released from the liposome, it can be effluxed out [79].
In 2014, a multicenter, open-label, phase 2 study was published comparing CPX-351 to 7 + 3 (daunorubicin 60 mg/m2) in patients age 60 to 75 years with newly diagnosed AML. The primary endpoint was complete response, defined as the combined rate of CR + CRi (neutrophils < 1000/mcL or platelets < 100,000/mcL). In the CPX-351 arm, 38.8% of patients had sAML, compared to 46.3% in the 7 + 3 arm. The CR/CRi rate was 66.7% with CPX-351 compared to 51.2% with 7 + 3, p = 0.07. The CR rate was no different between arms at 48%; therefore, differences in the primary endpoint were likely due to increased attainment of a CRi with CPX-351. The authors found no significant difference in median overall survival in the overall population of patients who received CPX-351 versus 7 + 3, with a median overall survival of 14.7 months versus 12.9 months, respectively. However, upon subgroup analysis, in patients with sAML, the median overall survival was 12.1 months with CPX-351, compared to 6.1 months with 7 + 3 (p = 0.01) [80]. As patients with secondary AML made up a minority of patients included, a phase 3 study was warranted to confirm these results.
In 2018, Lancet et al. published a randomized, phase 3, open label study comparing CPX-351 to conventional 7 + 3 in patients aged 60–75 years with secondary AML [81]. The authors defined sAML as therapy-related AML, AML with antecedent MDS or CMML, or AML with MDS-related cytogenetic abnormalities, per WHO 2008 criteria. Patients were randomized to CPX-351 or standard cytarabine and daunorubicin (7 + 3) and could receive up to two cycles of induction, followed by consolidation with up to two cycles of CPX-351 or 5 + 2. The primary endpoint was overall survival. When compared to 7 + 3, treatment with CPX-351 resulted in higher CR/CRi attainment which translated to an overall survival benefit (CR/CRi 47.7% vs. 33.3% p = 0.016 and median OS 9.56 mo vs. 5.96 mo p = 0.003). Interestingly, in previous studies that examined outcomes with 7 + 3 in sAML, response rates have been reported in the range of 40–60% which is higher than noted in this phase 3 trial [24, 82,83,84].
There are several limitations with the study design and interpretation of the results which limits the ability to extrapolate the results from the CPX-351 studies to practice. This study specifically evaluated use in patient age 60––75 years old and excluded those with AML-MRC based on morphology alone. Nonetheless, the FDA granted broad approval including patients of all ages and all AML-MRC classifications [85]. Consolidation with 5 + 2 is not a commonly utilized consolidation strategy in the USA, as many institutions favor a dose-adjustment to high-dose cytarabine therapy for consolidation in this age group of patients [82, 86]. In patients who proceed to transplant, the median survival was not reached in the CPX-351 group versus 10.25 months in the 7 + 3 group. However, it is important to consider patients’ disease control prior to transplant. At the time of transplant, 38% of 7 + 3 patients had active disease, compared to only 23% of the CPX-351 group. In practice, it is uncommon to take patients to transplant with active disease due to the high degree of disease-related mortality [87,88,89,90]. Finally, the way adverse events were reported in this study may be misleading. Because patients in the CPX-351 arm were on treatment longer and therefore had a longer duration to report adverse events, the authors reported adverse events per patient year. This assumes that the risk of an adverse event is constant over time. The median rate of adverse events per patient-year was higher in the 7 + 3 group at 87.22% versus 75.68% with CPX-351. However, the median time to count recovery was longer in the CPX-351 arm, with a median time to neutrophil recovery of 35 days with CPX-351 and 29 days with 7 + 3, indicating that patients who received CPX-351 were on therapy longer because they were cytopenic longer.
Historical studies have demonstrated that outcomes with 7 + 3 are suboptimal for sAML [24]. Potential limitations with the use of anthracyclines in sAML include additional toxicity as patients with sAML may be less able to tolerate intensive therapy due to age, prior treatment history, and decreased efficacy secondary to P-gp efflux. As discussed above, P-gp expression is more common in secondary AML, and studies have demonstrated a decreased accumulation of daunorubicin in AML cells with high P-gp expression, in vitro. CPX-351 is thought to overcome P-gp efflux based on its liposomal formulation [79, 91]. However, numerically the difference between drug uptake in vitro was very small (1.09 ± 0.21 ng with free-drug vs 1.76 ± 0.10 ng with liposomal daunorubicin) and once the individual drugs are released intracellularly, daunorubicin can still be effluxed by P-gp [91]. Alternatively, P-gp efflux can be avoided with the utilization of regimens that are not P-gp substrates, including HIDAC-based regimens. A multicenter, retrospective, real-world study demonstrated no difference in efficacy outcomes for patients with sAML who received HIDAC-based regimens (combinations of purine analog and daily doses of high-dose cytarabine) compared to CPX-351, with a median overall survival of 10.1 months versus 10.6 months, respectively [92]. The primary endpoint CR/CRi was non-inferior with HIDAC-based therapy, with a CR/CRi of 62.7% for HIDAC-based therapy and 47.9% with CPX-351. Treatment with CPX-351 was associated with a significantly higher rate of confirmed infections (74.5% vs 56%) and a significantly longer time to count recovery. Time to ANC recovery was 18 days with HIDAC-based treatment compared to 36 days with CPX-351. Time to platelet recovery was 23 days with HIDAC-based treatment compared to 38 days with CPX-351.
For patients with an antecedent hematologic disorder, it is not uncommon for patients to have had prior therapy with an HMA prior to transformation to AML. Talati et al. evaluated outcomes in patients with sAML who had prior HMA treatment for an antecedent hematologic malignancy and later received induction chemotherapy upon AML transformation [86]. Interestingly, this study demonstrated that longer durations of prior HMA exposure were associated with decreased response rates to CPX-351 upon AML transformation, with a CR/CRi of 64.3% with < 4 cycles of HMA and only 25% for > 4 cycles. In contrast, a HIDAC-based regimen maintained its response rate regardless of prior HMA exposure, with a CR/CRi of 56.5% vs 50%. Median overall survival was poor among all patients who received > 4 cycles of prior HMA (5.47 months cladribine-based ± mitoxantrone (CLAG/M), 8.67 months 7 + 3, and 5.47 months CPX-351), demonstrating a need for new agents for sAML patients following prior HMA failure [92]. Because the phase 3 trial demonstrated no benefit with CPX-351 in patients who received prior HMA for MDS, the ESMO guidelines recommend against the use of CPX-351 in this patient population and instead recommend a clinical trial [10, 81]. Interestingly, the analysis by Talati et al. showed a fairly high 30-day mortality with high-intensity chemotherapy regimens containing anthracycline (7 + 3 = 8% and CLAG/M = 12%). In contrast, Benitez et al. demonstrated a 30-day mortality of 1.3% with HIDAC-based regimens which omitted the use of anthracyclines, indicating that the use of anthracyclines only further contributes to toxicity in these patients.
In addition to HIDAC-based regimens, the combination of an HMA and venetoclax is a potential option for patients with sAML, including those who received prior HMA for MDS. As discussed previously, in addition to patients with de novo AML, patients with sAML were included in the phase 2 trial of combination decitabine and venetoclax [53]. An overall response rate was demonstrated in 12 of 15 patients (80%) with untreated sAML and 17 of 28 patients (61%) with treated sAML. The median duration of response for patients who received 4 or more cycles of prior HMA was 9.8 months. For patients who received four or more prior cycles of hypomethylating agents, the CR/CRi was 37% with decitabine and venetoclax. As discussed above, the response rate with CPX-351 in patients who had received at least 4 cycles of HMA was only 25%. While cross-trial comparisons are challenging due to heterogeneity, patients with sAML who progressed on HMA are a relatively homogenous population.
Furthermore, Ball et al. analyzed outcomes in patients who received combination HMA and venetoclax after HMA failure in a retrospective analysis of patients with MDS [93]. The authors defined HMA failure as a lack of response after 4 cycles of HMA, progressive disease after at least 2 cycles of HMA, or progressive disease after achieving a response. An overall response rate was demonstrated in 9 of 12 patients (75%) who had not received prior HMA, 10 of 16 patients (62%) who received less than 4 cycles of prior HMA, and 7 of 16 patients (44%) who failed. Of note, overall response included patients who had a CR, with or without hematologic improvement. Median overall survival was 19.5 months for all patients and 11.4 months for patients with HMA failure prior to initiating combination HMA and venetoclax. As this is a retrospective study, there is likely major selection bias in who received HMA and venetoclax following HMA failure. However, based on this data, it may be reasonable to switch a patients HMA and add venetoclax, but CR rates are lower.
Recommendations for use
The NCCN guidelines recommend the use of CPX-351 in patients of all ages with therapy-related AML, antecedent MDS/CMML, or AML-MRC that can tolerate intensive induction, despite the inclusion of only patients age 60 to 75 years and the exclusion of patients with AML-MRC based on morphology in the phase 3 study. This approach is associated with significant toxicity and high cost (Table 3). In contrast, despite European approval independent of age, the ESMO guidelines recommend CPX-351 in patients aged ≥ 60 years with therapy-related AML or AML-MRC [10]. Because of the limitations of the phase 3 study, prolonged time to count recovery, and poor outcomes in patients who have received prior HMA, the authors of this review recommend a non-anthracycline containing HIDAC-based induction with regimens such as FLAG (fludarabine and cytarabine) or CLAG (cladribine and cytarabine) or the combination of HMA and venetoclax in this patient population. If CPX-351 is utilized as an induction strategy, it is recommended to be limited to patients who have not been extensively pretreated with HMA therapy. Finally, for patients who are classified as AML-MRC by morphology alone, data suggest that this subgroup may be treated as de-novo AML. A summary of treatment recommendations for patients with sAML is provided in Fig. 4.
Maintenance therapy
Patient case
A 68-year-old man was admitted to a community hospital for pneumonia. Upon admission, a CBC revealed a WBC of 4 K/µL, hemoglobin of 6.3 g/dL, and platelets 98 K/µL. Upon discharge after treatment for infection, he experienced a brief count recovery and then became pancytopenic again. Given persistence of the cytopenias, he was referred for evaluation and a bone marrow biopsy was performed and revealed 23% myeloid blasts with MPO expression, consistent with AML. Cytogenetics demonstrated a normal male karyotype: 46,XY [20] and a microarray found a normal male profile. Myeloid next-generation sequencing found no somatic mutations. He started induction with daunorubicin 60 mg/m2 and cytarabine 100 mg/m2 in the standard 3 + 7 fashion. His course was complicated by neutropenic fevers and a Staph epidermidis bacteremia which was successfully treated. A follow-up bone marrow biopsy was done upon count recovery and revealed the patient was in first complete remission. Given his intermediate-risk karyotype, he was referred for an alloHCT consult. While that work-up was ongoing, he started monthly HIDAC using age-adjusted cytarabine 1500 mg/m2 BID days 1, 2, and 3 and ultimately received 4 cycles. The patient was considered ineligible for transplant due to the unavailability of full-match or haploidentical donors. His primary hematologist is considering starting maintenance therapy with azacitidine given inability to complete curative intent intensive therapy.
Oral azacitidine
Historically, maintenance therapies have demonstrated no survival benefit in AML, with the exception of FLT3 inhibitors in patients with FLT3-ITD mutations [94,95,96,97,98,99,100,101]. Recently, the use of hypomethylating agents for maintenance therapy has been explored. Subcutaneous azacitidine maintenance was compared to observation in patients in CR/CRi after at least two cycles of chemotherapy [98]. Despite an improved disease-free survival with azacitidine, there was no difference in overall survival with a 12-month OS of 84% with azacitidine versus 70% with observation (p = 0.69). A higher percentage of patients in the observation group had unfavorable-risk cytogenetic abnormalities (23% vs 16%). As expected, more than half of the observation patients (n = 32) received post-protocol salvage therapy upon relapse, compared to 9 patients in the azacitidine maintenance group where the options of further therapy were more limited. This study illustrated one conundrum of maintenance therapy in AML which is the decrease in available lines of therapy upon relapse for a disease that is often not curable.
Oral azacitidine maintenance therapy received FDA approval in September 2020 as a result of QUAZAR AML-001 maintenance trial [102]. Patients aged 55 years or older, with intermediate- or poor-risk AML who were not candidates for alloHCT, were randomized to oral azacitidine maintenance or placebo. The trial did not outline specific criteria to define transplant eligibility. Patients were randomized within 4 months of first CR/CRi; however, the study protocol defined a short cutoff for enrollment of 90 days. This is important to highlight because it helps explain the low number of patients who received adequate consolidation therapy. Response was assessed every 3 cycles, and patients with AML relapse (defined as 5–15% blasts in the blood or bone marrow) could receive an increased duration of oral azacitidine maintenance or placebo to 21 days per cycle from the original 14 days. The authors found that azacitidine maintenance demonstrated a survival benefit over placebo, with a median OS of 24.7 months versus 14.8 months, respectively. However, there were significant limitations with the study design which limit the ability to extrapolate these results to practice.
All patients received intensive remission induction with cytarabine and an anthracycline yet were ineligible for transplant. While transplant eligibility criteria were not defined, 65% of patients were considered ineligible based on age. The median age in this study was 68 indicating that 50% of patients were less than 68 years old suggesting the centers included in the study were rather conservative in their approach to transplantation and this would limit external validity. Furthermore, only 80% of patients started consolidation therapy, including 45% who only received one cycle of consolidation therapy. These patients were not too sick or deconditioned to receive further cycles of induction based on ECOG scored reported, but rather based on the timeline from CR/CRi to enrollment, it would have not been possible for patients to receive adequate consolidation with 3–4 cycles. While the optimal number of consolidation cycles remains a highly debated topic dependent on induction regimen and disease characteristics, multiple studies have demonstrated the benefit of 3–4 cycles over 0–2 cycles [34,35,36, 103]. In fact, studies since the 1980s have demonstrated that patients who do not receive any consolidation therapy do significantly worse [6, 104, 105]. A subsequent abstract noted the survival benefit with azacitidine remained regardless of consolidation; however. this survival advantage is limited to the subgroup who received zero cycles of consolidation [106]. Only 6 patients in the azacitidine arm and 13 in the placebo arm received an adequate 3 cycles of consolidation.
Furthermore, 51 patients (21%) in the oral azacitidine arm and 40 patients (17%) in the placebo arm received an escalated 21-day dosing schedule upon AML relapse, with 5–15% blasts, which did not count as an event for progression-free survival. It is arguably unethical to continue current therapy in the azacitidine group in the setting of increasing blasts, and certainly unethical in the placebo group given salvage options exist for these patients. Overall, 65% of patients received subsequent therapy after discontinuing trial treatment. Subsequent treatment was considered low intensity in 61% of the azacitidine arm and 61.5% of the placebo arm, of which about 20% of patients received a hypomethylating agent and for the remaining patients specific subsequent therapy is unknown, but could have included low dose cytarabine and hydroxyurea. Based on these results, it is not known whether there is greater benefit with early initiation of HMA in maintenance or waiting until patients subsequently relapse. Finally, oral azacitidine is not interchangeable with the IV formulation (bioavailability is 11% with oral azacitidine), and there is no data to support the off-label use in combination with venetoclax.
Recommendations for use
The NCCN guidelines support the use of oral azacitidine maintenance in patients with intermediate- or unfavorable-risk disease who decline or are otherwise ineligible for transplant. Oral azacitidine received approval by the European Commission after the most recent ESMO guidelines were published. Due to limitations with the study design, inadequate consolidation, and unknown benefit of HMA maintenance versus HMA at relapse, the authors of this review believe there is currently no role for the use of azacitidine maintenance therapy for patients that have completed a standard HIDAC-based consolidation and oral azacitidine should not replace proper HIDAC consolidation for eligible patients.
Conclusion
In recent years there has been an exponential increase in new drug approvals for AML; however, the quality of data to support these new approvals has some major limitations, including phase 2 study design, suboptimal control arms, inadequate consolidation therapy, selection bias, limited real-world applicability, and surrogate primary endpoints. It is very challenging to extrapolate results to current practice when the current practice is not reflected in the study designs. It is possible that any survival benefit seen may just be attributed to patients not being treated per current standards, which we know improve survival outcomes. While novel agents are needed to improve outcomes for patients with AML, especially those with poor risk cytogenetics, caution should be exercised before replacing current standard of care without adequate data demonstrating superiority to standard of care in the correct population of interest.
Many of these agents and combinations were approved based on overall response rate benefits. Only five drugs/regimens were approved based on overall survival (CPX-351, glasdegib + LDAC, 7 + 3 + midostaurin, gilteritinib, and oral azacitidine). Our goals in AML treatment are to prolong survival and/or improve quality of life, and it is unknown whether improvements in surrogate endpoints achieve one of these two goals. For the few drugs/regimens that utilized overall survival as the primary endpoint, as discussed above, the studies have significant limitations which minimize the suggested survival benefit. Furthermore, for the studies which utilized surrogate endpoints as the basis of approval, multiple recent press releases have demonstrated that subsequent phase 3 studies have not met the primary endpoint of overall survival. This once again reaffirms that surrogate endpoints are poor predictors of what is important to both patients and healthcare providers. In addition, Chen et al. demonstrated that the use of surrogate endpoints speeds up time to drug approval by about 1 year [107]. While this analysis is potentially an oversimplification, it is particularly relevant for disease states like AML, where 5-year survival rates are only 28.7%, and therefore, length of time needed to measure median overall survival is likely even shorter.
In addition to efficacy and toxicity concerns, these novel agents are associated with significant financial toxicity. The high costs of novel anticancer agents are not sustainable (Table 3). Efficacy, safety, and cost considerations are all essential to making treatment decisions and therefore national guidelines should incorporate principles of cost effectiveness. While this review was not comprehensive, employing these principles of oncology stewardship to the treatment of AML can maximize patient outcomes in a financially responsible fashion while preventing exposure to significant toxicities of novel agents.
References
Yates JW, Wallace HJ, Ellison RR, Holland JF (1973) Cytosine arabinoside (NSC-63878) and daunorubicin (NSC-83142) therapy in acute nonlymphocytic leukemia. Cancer Chemother Rep 57(4):485–488
National Cancer Institute Surveillance, Epidemiology, and End Results SEER) Program. Acute Myeloid Leukemia.: https://seer.cancer.gov/statfacts/html/amyl.html Accessed.
Cornely OA, Maertens J, Winston DJ, Perfect J, Ullmann AJ, Walsh TJ et al (2007) Posaconazole vs. fluconazole or itraconazole prophylaxis in patients with neutropenia. N Engl J Med 356(4):348–59. https://doi.org/10.1056/NEJMoa061094
Fernandez HF, Sun Z, Yao X, Litzow MR, Luger SM, Paietta EM et al (2009) Anthracycline dose intensification in acute myeloid leukemia. N Engl J Med 361(13):1249–1259. https://doi.org/10.1056/NEJMoa0904544
Mayer RJ, Davis RB, Schiffer CA, Berg DT, Powell BL, Schulman P et al (1994) Intensive postremission chemotherapy in adults with acute myeloid leukemia Cancer and Leukemia Group B. N Engl J Med. 331(14):896–903. https://doi.org/10.1056/NEJM199410063311402
Cassileth PA, Harrington DP, Hines JD, Oken MM, Mazza JJ, McGlave P et al (1988) Maintenance chemotherapy prolongs remission duration in adult acute nonlymphocytic leukemia. J Clin Oncol 6(4):583–587. https://doi.org/10.1200/JCO.1988.6.4.583
Vaughan WP, Karp JE, Burke PJ (1980) Long chemotherapy-free remissions after single-cycle timed-sequential chemotherapy for acute myelocytic leukemia. Cancer 45(5):859–865. https://doi.org/10.1002/1097-0142(19800301)45:5%3c859::aid-cncr2820450506%3e3.0.co;2-z
Burke PJ, Karp JE, Braine HG, Vaughan WP (1977) Timed sequential therapy of human leukemia based upon the response of leukemic cells to humoral growth factors. Cancer Res 37(7 Pt 1):2138–2146
National Comprehensive Cancer Network. Acute Myeloid Leukemia (Version 3.2021). https://www.nccn.org/professionals/physician_gls/pdf/aml.pdf Accessed.
Heuser M, Ofran Y, Boissel N, Brunet Mauri S, Craddock C, Janssen J et al (2020) Acute myeloid leukaemia in adult patients: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 31(6):697–712. https://doi.org/10.1016/j.annonc.2020.02.018
Howard DH, Bach PB, Berndt ER, Conti RM (2015) Pricing in the Market for Anticancer Drugs. J Econ Perspect 29(1):139–162. https://doi.org/10.1257/jep.29.1.139
Bach PB, Saltz LB, Wittes RE (2012) In cancer care, cost matters. New York Times. https://www.nytimes.com/2012/10/15/opinion/a-hospital-says-no-to-an-11000-a-month-cancer-drug.html
Vokinger KN, Hwang TJ, Grischott T, Reichert S, Tibau A, Rosemann T et al (2020) Prices and clinical benefit of cancer drugs in the USA and Europe: a cost-benefit analysis. Lancet Oncol 21(5):664–670. https://doi.org/10.1016/S1470-2045(20)30139-X
National Comprehensive Cancer Network. Acute Myeloid Leukemia (Version 2.2020). https://www.nccn.org/professionals/physician_gls/pdf/aml.pdf Accessed.
Jourdan E, Boissel N, Chevret S, Delabesse E, Renneville A, Cornillet P et al (2013) Prospective evaluation of gene mutations and minimal residual disease in patients with core binding factor acute myeloid leukemia. Blood 121(12):2213–2223. https://doi.org/10.1182/blood-2012-10-462879
Sawler D, Sanford D, Brandwein JM, Sandhu I, Hogge D, Saini L (2017) Two Cycles of Consolidation Chemotherapy Are Associated with Similar Clinical Outcomes to Three Cycles in AML Patients with Favorable Risk Cytogenetics. Blood 130:464
Mylotarg [Package insert]. Philadelphia, PA: Wyeth Pharmaceuticals LLC, a subsidiary of Pfizer Inc; 2017. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/761060lbl.pdf
Dinndorf PA, Andrews RG, Benjamin D, Ridgway D, Wolff L, Bernstein ID (1986) Expression of normal myeloid-associated antigens by acute leukemia cells. Blood 67(4):1048–1053
Griffin JD, Linch D, Sabbath K, Larcom P, Schlossman SF (1984) A monoclonal antibody reactive with normal and leukemic human myeloid progenitor cells. Leuk Res 8(4):521–534. https://doi.org/10.1016/0145-2126(84)90001-8
Ricart AD (2011) Antibody-drug conjugates of calicheamicin derivative: gemtuzumab ozogamicin and inotuzumab ozogamicin. Clin Cancer Res 17(20):6417–6427. https://doi.org/10.1158/1078-0432.CCR-11-0486
Bross PF, Beitz J, Chen G, Chen XH, Duffy E, Kieffer L et al (2001) Approval summary: gemtuzumab ozogamicin in relapsed acute myeloid leukemia. Clin Cancer Res 7(6):1490–1496
Sievers EL, Larson RA, Stadtmauer EA, Estey E, Löwenberg B, Dombret H et al (2001) Efficacy and safety of gemtuzumab ozogamicin in patients with CD33-positive acute myeloid leukemia in first relapse. J Clin Oncol 19(13):3244–3254. https://doi.org/10.1200/JCO.2001.19.13.3244
Petersdorf SH, Kopecky KJ, Slovak M, Willman C, Nevill T, Brandwein J et al (2013) A phase 3 study of gemtuzumab ozogamicin during induction and postconsolidation therapy in younger patients with acute myeloid leukemia. Blood 121(24):4854–4860. https://doi.org/10.1182/blood-2013-01-466706
Löwenberg B, Ossenkoppele GJ, van Putten W, Schouten HC, Graux C, Ferrant A et al (2009) High-dose daunorubicin in older patients with acute myeloid leukemia. N Engl J Med 361(13):1235–1248. https://doi.org/10.1056/NEJMoa0901409
Hills RK, Castaigne S, Appelbaum FR, Delaunay J, Petersdorf S, Othus M et al (2014) Addition of gemtuzumab ozogamicin to induction chemotherapy in adult patients with acute myeloid leukaemia: a meta-analysis of individual patient data from randomised controlled trials. Lancet Oncol 15(9):986–996. https://doi.org/10.1016/S1470-2045(14)70281-5
Burnett AK, Russell NH, Hills RK, Kell J, Freeman S, Kjeldsen L et al (2012) Addition of gemtuzumab ozogamicin to induction chemotherapy improves survival in older patients with acute myeloid leukemia. J Clin Oncol 30(32):3924–3931. https://doi.org/10.1200/JCO.2012.42.2964
Burnett AK, Hills RK, Milligan D, Kjeldsen L, Kell J, Russell NH et al (2011) Identification of patients with acute myeloblastic leukemia who benefit from the addition of gemtuzumab ozogamicin: results of the MRC AML15 trial. J Clin Oncol 29(4):369–377. https://doi.org/10.1200/JCO.2010.31.4310
Castaigne S, Pautas C, Terré C, Raffoux E, Bordessoule D, Bastie JN et al (2012) Effect of gemtuzumab ozogamicin on survival of adult patients with de-novo acute myeloid leukaemia (ALFA-0701): a randomised, open-label, phase 3 study. Lancet 379(9825):1508–1516. https://doi.org/10.1016/S0140-6736(12)60485-1
Delaunay J, Recher C, Pigneux A, Witz F, Vey N, Blanchet O et al (2011) Addition of gemtuzumab ozogamycin to chemotherapy improves event-free survival but not overall survival of AML patients with intermediatecytogenetics not eligible for allogeneic transplantation: results of the GOELAMS AML 2006 IRstudy. Blood 118(21):37–38
Döhner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Büchner T et al (2017) Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood 129(4):424–447. https://doi.org/10.1182/blood-2016-08-733196
Anderson JE, Kopecky KJ, Willman CL, Head D, O’Donnell MR, Luthardt FW et al (2002) Outcome after induction chemotherapy for older patients with acute myeloid leukemia is not improved with mitoxantrone and etoposide compared to cytarabine and daunorubicin: a Southwest Oncology Group study. Blood 100(12):3869–3876. https://doi.org/10.1182/blood-2001-12-0354
Burnett AK, Russell NH, Hills RK, Hunter AE, Kjeldsen L, Yin J et al (2013) Optimization of chemotherapy for younger patients with acute myeloid leukemia: results of the medical research council AML15 trial. J Clin Oncol 31(27):3360–3368. https://doi.org/10.1200/JCO.2012.47.4874
Bloomfield CD, Lawrence D, Byrd JC, Carroll A, Pettenati MJ, Tantravahi R et al (1998) Frequency of prolonged remission duration after high-dose cytarabine intensification in acute myeloid leukemia varies by cytogenetic subtype. Cancer Res 58(18):4173–4179
Byrd JC, Dodge RK, Carroll A, Baer MR, Edwards C, Stamberg J et al (1999) Patients with t(8;21)(q22;q22) and acute myeloid leukemia have superior failure-free and overall survival when repetitive cycles of high-dose cytarabine are administered. J Clin Oncol 17(12):3767–3775. https://doi.org/10.1200/JCO.1999.17.12.3767
Byrd JC, Ruppert AS, Mrózek K, Carroll AJ, Edwards CG, Arthur DC et al (2004) Repetitive cycles of high-dose cytarabine benefit patients with acute myeloid leukemia and inv(16)(p13q22) or t(16;16)(p13;q22): results from CALGB 8461. J Clin Oncol 22(6):1087–1094. https://doi.org/10.1200/JCO.2004.07.012
Burnett AK, Russell NH, Hills RK, Knapper S, Freeman S, Huntly B et al (2021) Defining the Optimal Total Number of Chemotherapy Courses in Younger Patients With Acute Myeloid Leukemia: A Comparison of Three Versus Four Courses. J Clin Oncol 39(8):890–901. https://doi.org/10.1200/JCO.20.01170
Lambert J, Pautas C, Terré C, Raffoux E, Turlure P, Caillot D et al (2019) Gemtuzumab ozogamicin for. Haematologica 104(1):113–119. https://doi.org/10.3324/haematol.2018.188888
Godwin CD, McDonald GB, Walter RB (2017) Sinusoidal obstruction syndrome following CD33-targeted therapy in acute myeloid leukemia. Blood 129(16):2330–2332. https://doi.org/10.1182/blood-2017-01-762419
Boghaert ER, Khandke KM, Sridharan L, Dougher M, DiJoseph JF, Kunz A et al (2008) Determination of pharmacokinetic values of calicheamicin-antibody conjugates in mice by plasmon resonance analysis of small (5 microl) blood samples. Cancer Chemother Pharmacol 61(6):1027–1035. https://doi.org/10.1007/s00280-007-0560-2
Löwenberg B (2013) Sense and nonsense of high-dose cytarabine for acute myeloid leukemia. Blood 121(1):26–28. https://doi.org/10.1182/blood-2012-07-444851
Schaich M, Röllig C, Soucek S, Kramer M, Thiede C, Mohr B et al (2011) Cytarabine dose of 36 g/m2 compared with 12 g/m2 within first consolidation in acute myeloid leukemia: results of patients enrolled onto the prospective randomized AML96 study. J Clin Oncol 29(19):2696–2702. https://doi.org/10.1200/JCO.2010.33.7303
Miyawaki S, Ohtake S, Fujisawa S, Kiyoi H, Shinagawa K, Usui N et al (2011) A randomized comparison of 4 courses of standard-dose multiagent chemotherapy versus 3 courses of high-dose cytarabine alone in postremission therapy for acute myeloid leukemia in adults: the JALSG AML201 Study. Blood 117(8):2366–2372. https://doi.org/10.1182/blood-2010-07-295279
Ochs MA, Perissinotti AJ, Marini BL, Burke PW, Bixby DL, Pettit KM et al (2021) Impact of high dose cytarabine dosing strategies in obese patients with acute myeloid leukemia. Leuk Res 102:106517. https://doi.org/10.1016/j.leukres.2021.106517
Papaemmanuil E, Gerstung M, Bullinger L, Gaidzik VI, Paschka P, Roberts ND et al (2016) Genomic Classification and Prognosis in Acute Myeloid Leukemia. N Engl J Med 374(23):2209–2221. https://doi.org/10.1056/NEJMoa1516192
Vidaza [Package insert]. Summit, NJ: Celgene Corporation; 2022. https://packageinserts.bms.com/pi/pi_vidaza.pdf
Dacogen [Package insert]. Rockville, MD: Otsuka America Pharmaceutical Inc.; 2018. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/021790s021lbl.pdf
Welch JS, Petti AA, Miller CA, Fronick CC, O’Laughlin M, Fulton RS et al (2016) TP53 and Decitabine in Acute Myeloid Leukemia and Myelodysplastic Syndromes. N Engl J Med 375(21):2023–2036. https://doi.org/10.1056/NEJMoa1605949
Stengel A, Kern W, Haferlach T, Meggendorfer M, Fasan A, Haferlach C (2017) The impact of TP53 mutations and TP53 deletions on survival varies between AML, ALL, MDS and CLL: an analysis of 3307 cases. Leukemia 31(3):705–711. https://doi.org/10.1038/leu.2016.263
Montero J, Letai A (2018) Why do BCL-2 inhibitors work and where should we use them in the clinic? Cell Death Differ 25(1):56–64. https://doi.org/10.1038/cdd.2017.183
Anderson MA, Huang D, Roberts A (2014) Targeting BCL2 for the treatment of lymphoid malignancies. Semin Hematol 51(3):219–227. https://doi.org/10.1053/j.seminhematol.2014.05.008
Pan R, Hogdal LJ, Benito JM, Bucci D, Han L, Borthakur G et al (2014) Selective BCL-2 inhibition by ABT-199 causes on-target cell death in acute myeloid leukemia. Cancer Discov 4(3):362–375. https://doi.org/10.1158/2159-8290.CD-13-0609
DiNardo CD, Jonas BA, Pullarkat V, Thirman MJ, Garcia JS, Wei AH et al (2020) Azacitidine and Venetoclax in Previously Untreated Acute Myeloid Leukemia. N Engl J Med 383(7):617–629. https://doi.org/10.1056/NEJMoa2012971
DiNardo CD, Maiti A, Rausch CR, Pemmaraju N, Naqvi K, Daver NG et al (2020) 10-day decitabine with venetoclax for newly diagnosed intensive chemotherapy ineligible, and relapsed or refractory acute myeloid leukaemia: a single-centre, phase 2 trial. Lancet Haematol 7(10):e724–e736. https://doi.org/10.1016/S2352-3026(20)30210-6
Kim K, Maiti A, Loghavi S, Pourebrahim R, Kadia TM, Rausch CR et al (2021) Outcomes of TP53-mutant acute myeloid leukemia with decitabine and venetoclax. Cancer. https://doi.org/10.1002/cncr.33689
DiNardo CD, Tiong IS, Quaglieri A, MacRaild S, Loghavi S, Brown FC et al (2020) Molecular patterns of response and treatment failure after frontline venetoclax combinations in older patients with AML. Blood 135(11):791–803. https://doi.org/10.1182/blood.2019003988
Short NJ, Montalban-Bravo G, Hwang H, Ning J, Franquiz MJ, Kanagal-Shamanna R et al (2020) Prognostic and therapeutic impacts of mutant TP53 variant allelic frequency in newly diagnosed acute myeloid leukemia. Blood Adv 4(22):5681–5689. https://doi.org/10.1182/bloodadvances.2020003120
Zeidan AM, Pollyea DA, Borate U, Vasconcelos A, Potluri R, Rotter D, et al (2021) Venetoclax Plus Azacitidine (VEN-AZA) Vs. Intensive Chemotherapy (IC) As Induction for Patients with Acute Myeloid Leukemia (AML): Retrospective Analysis of an Electronic Medical Records (EMR) Database in the United States [abstract]. Blood;Abstract 277.
Chen S, Xie J, Yang X, Shen H, Cen J, Yao L, et al (20210 Venetoclax Plus Decitabine for Young Adults with Newly Diagnosed ELN Adverse-Risk Acute Myeloid Leukemia: Interim Analysis of a Prospective, Multicenter, Single-Arm, Phase 2 Trial [abstract]. Blood. Abstract 35.
Garcia JS, Wolach O, Vachhani P, Zeidner JF, Talati C, Pollyea DA, et al (2021) Comparative Effectiveness of Venetoclax Combinations Vs Other Therapies Among Patients with Newly Diagnosed Acute Myeloid Leukemia: Results from the AML Real World Evidence (ARC) Initiative [abstract]. Blood. Abstract 2328.
Sahasrabudhe KD, Rebechi MT, Huang Y, Behbehani GK, Bhatnagar B, Blachly JS, et al (2021) Effect of High Intensity Chemotherapy Vs Targeted Therapy on Survival in AML Patients Aged 60–75 [abstract]. Blood. Abstract 4125.
Pollyea DA, Winters A, McMahon C, Schwartz M, Jordan CT, Rabinovitch R et al (2022) Venetoclax and azacitidine followed by allogeneic transplant results in excellent outcomes and may improve outcomes versus maintenance therapy among newly diagnosed AML patients older than 60. Bone Marrow Transplant 57(2):160–166. https://doi.org/10.1038/s41409-021-01476-7
Kadia TM, Jain P, Ravandi F, Garcia-Manero G, Andreef M, Takahashi K et al (2016) TP53 mutations in newly diagnosed acute myeloid leukemia: Clinicomolecular characteristics, response to therapy, and outcomes. Cancer 122(22):3484–3491. https://doi.org/10.1002/cncr.30203
Maiti A, Qiao W, Sasaki K, Ravandi F, Kadia TM, Jabbour EJ et al (2021) Venetoclax with decitabine vs intensive chemotherapy in acute myeloid leukemia: A propensity score matched analysis stratified by risk of treatment-related mortality. Am J Hematol 96(3):282–291. https://doi.org/10.1002/ajh.26061
Gaidzik VI, Mayr-Benedikter V, Weber D, et al (2020) Higher Dose of CPX-351 Is Associated with Prolonged Hematologic Recovery: Results from an Interim Safety Analysis of the Randomized, Phase III AMLSG 30–18 Trial. Presented at: 2020 ASH Annual Meeting; December 5–8, Virtual. Abstract 1043.
Przespolewski AC, Talati C, Fazal S, Vachhani P, Sanikommu S, Thota S, et al. (2019) Safety and efficacy of CPX-351 in younger patients < 60 years old with secondary acute myeloid leukemia: An updated analysis. J Clin Oncol. 37 : 15_suppl , e18530-e18530.
Amadori S, Suciu S, Selleslag D, Aversa F, Gaidano G, Musso M et al (2016) Gemtuzumab Ozogamicin Versus Best Supportive Care in Older Patients With Newly Diagnosed Acute Myeloid Leukemia Unsuitable for Intensive Chemotherapy: Results of the Randomized Phase III EORTC-GIMEMA AML-19 Trial. J Clin Oncol 34(9):972–979. https://doi.org/10.1200/JCO.2015.64.0060
Daurismo [Package insert]. New York, NY: Pfizer Inc; 2018. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/210656s000lbl.pdf
Cortes JE, Heidel FH, Hellmann A, Fiedler W, Smith BD, Robak T et al (2019) Randomized comparison of low dose cytarabine with or without glasdegib in patients with newly diagnosed acute myeloid leukemia or high-risk myelodysplastic syndrome. Leukemia 33(2):379–389. https://doi.org/10.1038/s41375-018-0312-9
Heuser M, Smith BD, Fiedler W, Sekeres MA, Montesinos P, Leber B et al (2021) Clinical benefit of glasdegib plus low-dose cytarabine in patients with de novo and secondary acute myeloid leukemia: long-term analysis of a phase II randomized trial. Ann Hematol 100(5):1181–1194. https://doi.org/10.1007/s00277-021-04465-4
Arber DA, Orazi A, Hasserjian R, et al (2016) The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 127(20):2391–2405. Blood. 2016;128(3):462–3. https://doi.org/10.1182/blood-2016-06-721662.
Kayser S, Döhner K, Krauter J, Köhne CH, Horst HA, Held G et al (2011) The impact of therapy-related acute myeloid leukemia (AML) on outcome in 2853 adult patients with newly diagnosed AML. Blood 117(7):2137–2145. https://doi.org/10.1182/blood-2010-08-301713
Borthakur G, Lin E, Jain N, Estey EE, Cortes JE, O’Brien S et al (2009) Survival is poorer in patients with secondary core-binding factor acute myelogenous leukemia compared with de novo core-binding factor leukemia. Cancer 115(14):3217–3221. https://doi.org/10.1002/cncr.24367
Montalban-Bravo G, Kanagal-Shamanna R, Class CA, Sasaki K, Ravandi F, Cortes JE et al (2020) Outcomes of acute myeloid leukemia with myelodysplasia related changes depend on diagnostic criteria and therapy. Am J Hematol 95(6):612–622. https://doi.org/10.1002/ajh.25769
Tardi P, Johnstone S, Harasym N, Xie S, Harasym T, Zisman N et al (2009) In vivo maintenance of synergistic cytarabine:daunorubicin ratios greatly enhances therapeutic efficacy. Leuk Res 33(1):129–139. https://doi.org/10.1016/j.leukres.2008.06.028
Sonneveld P, List AF (2001) Chemotherapy resistance in acute myeloid leukaemia. Best Pract Res Clin Haematol 14(1):211–233. https://doi.org/10.1053/beha.2000.0124
Leith CP, Kopecky KJ, Godwin J, McConnell T, Slovak ML, Chen IM et al (1997) Acute myeloid leukemia in the elderly: assessment of multidrug resistance (MDR1) and cytogenetics distinguishes biologic subgroups with remarkably distinct responses to standard chemotherapy. A Southwest Oncol Group Stud Blood 89(9):3323–3329
da SilveiraJúnior LS, Soares VL, Jardim da Silva AS, Gil EA, Pereira de Araújo MDG, MercesGonçalves CA et al (2020) P-glycoprotein and multidrug resistance-associated protein-1 expression in acute myeloid leukemia: Biological and prognosis implications. Int J Lab Hematol. 42(5):594–603. https://doi.org/10.1111/ijlh.13241
Nooter K, Sonneveld P, Oostrum R, Herweijer H, Hagenbeek T, Valerio D (1990) Overexpression of the mdr1 gene in blast cells from patients with acute myelocytic leukemia is associated with decreased anthracycline accumulation that can be restored by cyclosporin-A. Int J Cancer 45(2):263–268. https://doi.org/10.1002/ijc.2910450210
Brunetti C, Anelli L, Zagaria A, Specchia G, Albano F (2017) CPX-351 in acute myeloid leukemia: can a new formulation maximize the efficacy of old compounds? Expert Rev Hematol 10(10):853–862. https://doi.org/10.1080/17474086.2017.1369400
Lancet JE, Cortes JE, Hogge DE, Tallman MS, Kovacsovics TJ, Damon LE et al (2014) Phase 2 trial of CPX-351, a fixed 5:1 molar ratio of cytarabine/daunorubicin, vs cytarabine/daunorubicin in older adults with untreated AML. Blood 123(21):3239–3246. https://doi.org/10.1182/blood-2013-12-540971
Lancet JE, Uy GL, Cortes JE, Newell LF, Lin TL, Ritchie EK et al (2018) CPX-351 (cytarabine and daunorubicin) Liposome for Injection Versus Conventional Cytarabine Plus Daunorubicin in Older Patients With Newly Diagnosed Secondary Acute Myeloid Leukemia. J Clin Oncol 36(26):2684–2692. https://doi.org/10.1200/JCO.2017.77.6112
Vulaj V, Perissinotti AJ, Uebel JR, Nachar VR, Scappaticci GB, Crouch A et al (2018) The FOSSIL Study: FLAG or standard 7+3 induction therapy in secondary acute myeloid leukemia. Leuk Res 70:91–96. https://doi.org/10.1016/j.leukres.2018.05.011
Bello C, Yu D, Komrokji RS, Zhu W, Wetzstein GA, List AF et al (2011) Outcomes after induction chemotherapy in patients with acute myeloid leukemia arising from myelodysplastic syndrome. Cancer 117(7):1463–1469. https://doi.org/10.1002/cncr.25598
Hulegårdh E, Nilsson C, Lazarevic V, Garelius H, Antunovic P, Rangert Derolf Å et al (2015) Characterization and prognostic features of secondary acute myeloid leukemia in a population-based setting: a report from the Swedish Acute Leukemia Registry. Am J Hematol 90(3):208–214. https://doi.org/10.1002/ajh.23908
Vyxeos [Package insert]. Palo Alto, CA: Jazz Pharmaceuticals; 2017. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/209401s000lbl.pdf
Talati C, Goldberg AD, Przespolewski A, Chan O, Ali NA, Kim J et al (2020) Comparison of induction strategies and responses for acute myeloid leukemia patients after resistance to hypomethylating agents for antecedent myeloid malignancy. Leuk Res 93:106367. https://doi.org/10.1016/j.leukres.2020.106367
Weisdorf DJ, Millard HR, Horowitz MM, Hyare PS, Champlin R, Ho V et al (2017) Allogeneic transplantation for advanced acute myeloid leukemia: The value of complete remission. Cancer 123(11):2025–2034. https://doi.org/10.1002/cncr.30536
Clift RA, Buckner CD, Appelbaum FR, Schoch G, Petersen FB, Bensinger WI et al (1992) Allogeneic marrow transplantation during untreated first relapse of acute myeloid leukemia. J Clin Oncol 10(11):1723–1729. https://doi.org/10.1200/JCO.1992.10.11.1723
Armistead PM, de Lima M, Pierce S, Qiao W, Wang X, Thall PF et al (2009) Quantifying the survival benefit for allogeneic hematopoietic stem cell transplantation in relapsed acute myelogenous leukemia. Biol Blood Marrow Transplant 15(11):1431–1438. https://doi.org/10.1016/j.bbmt.2009.07.008
Wong R, Shahjahan M, Wang X, Thall PF, De Lima M, Khouri I et al (2005) Prognostic factors for outcomes of patients with refractory or relapsed acute myelogenous leukemia or myelodysplastic syndromes undergoing allogeneic progenitor cell transplantation. Biol Blood Marrow Transplant 11(2):108–114. https://doi.org/10.1016/j.bbmt.2004.10.008
Kim HP, Gerhard B, Harasym TO, Mayer LD, Hogge DE (2011) Liposomal encapsulation of a synergistic molar ratio of cytarabine and daunorubicin enhances selective toxicity for acute myeloid leukemia progenitors as compared to analogous normal hematopoietic cells. Exp Hematol 39(7):741–750. https://doi.org/10.1016/j.exphem.2011.04.001
Benitez LL, Perissinotti AJ, Rausch CR, Klaus J, Clark SM, Filtz M et al (2021) Multicenter comparison of high-dose cytarabine-based regimens versus liposomal daunorubicin and cytarabine (CPX-351) in patients with secondary acute myeloid leukemia. Leuk Lymphoma 62(9):2184–2192. https://doi.org/10.1080/10428194.2021.1907378
Ball BJ, Famulare CA, Stein EM, Tallman MS, Derkach A, Roshal M et al (2020) Venetoclax and hypomethylating agents (HMAs) induce high response rates in MDS, including patients after HMA therapy failure. Blood Adv 4(13):2866–2870. https://doi.org/10.1182/bloodadvances.2020001482
Pautas C, Merabet F, Thomas X, Raffoux E, Gardin C, Corm S et al (2010) Randomized study of intensified anthracycline doses for induction and recombinant interleukin-2 for maintenance in patients with acute myeloid leukemia age 50 to 70 years: results of the ALFA-9801 study. J Clin Oncol 28(5):808–814. https://doi.org/10.1200/JCO.2009.23.2652
Löwenberg B, Suciu S, Archimbaud E, Haak H, Stryckmans P, de Cataldo R et al (1998) Mitoxantrone versus daunorubicin in induction-consolidation chemotherapy--the value of low-dose cytarabine for maintenance of remission, and an assessment of prognostic factors in acute myeloid leukemia in the elderly: final report. European Organization for the Research and Treatment of Cancer and the Dutch-Belgian Hemato-Oncology Cooperative Hovon Group. J Clin Oncol 16(3):872–81. https://doi.org/10.1200/JCO.1998.16.3.872
Burchert A, Bug G, Fritz LV, Finke J, Stelljes M, Röllig C et al (2020) Sorafenib Maintenance After Allogeneic Hematopoietic Stem Cell Transplantation for Acute Myeloid Leukemia With. J Clin Oncol 38(26):2993–3002. https://doi.org/10.1200/JCO.19.03345
Roboz GJ, Strickland SA, Litzow MR, Dalovisio A, Perl AE, Bonifacio G et al (2020) Updated safety of midostaurin plus chemotherapy in newly diagnosed. Leuk Lymphoma 61(13):3146–3153. https://doi.org/10.1080/10428194.2020.1805109
Huls G, Chitu DA, Havelange V, Jongen-Lavrencic M, van de Loosdrecht AA, Biemond BJ et al (2019) Azacitidine maintenance after intensive chemotherapy improves DFS in older AML patients. Blood 133(13):1457–1464. https://doi.org/10.1182/blood-2018-10-879866
Russell NH, Hills RK, Thomas A, Thomas I, Kjeldsen L, Dennis M et al (2021) Outcomes of older patients aged 60 to 70 years undergoing reduced intensity transplant for acute myeloblastic leukemia: results of the NCRI acute myeloid leukemia 16 trial. Haematologica. https://doi.org/10.3324/haematol.2021.279010
Foran JM, Zhouxin S, Claxton DF, Lazarus HM, Arber DA, Rowe JM, et al (2019) Maintenance Decitabine (DAC) Improves Disease-Free (DFS) and Overall Survival (OS) after Intensive Therapy for Acute Myeloid Leukemia (AML) in Older Adults, Particularly in FLT3-ITD-Negative Patients: ECOG-ACRIN (E-A) E2906 Randomized Study [abstract]. Blood. Abstract 615.
Blum W, Sanford BL, Klisovic R, DeAngelo DJ, Uy G, Powell BL et al (2017) Maintenance therapy with decitabine in younger adults with acute myeloid leukemia in first remission: a phase 2 Cancer and Leukemia Group B Study (CALGB 10503). Leukemia 31(1):34–39. https://doi.org/10.1038/leu.2016.252
Wei AH, Döhner H, Pocock C, Montesinos P, Afanasyev B, Dombret H et al (2020) Oral Azacitidine Maintenance Therapy for Acute Myeloid Leukemia in First Remission. N Engl J Med 383(26):2526–2537. https://doi.org/10.1056/NEJMoa2004444
Schlenk RF (2016) Is there justification for 4 cycles of consolidation therapy in AML? Best Pract Res Clin Haematol 29(4):341–344. https://doi.org/10.1016/j.beha.2016.10.008
Büchner T, Urbanitz D, Hiddemann W, Rühl H, Ludwig WD, Fischer J et al (1985) Intensified induction and consolidation with or without maintenance chemotherapy for acute myeloid leukemia (AML): two multicenter studies of the German AML Cooperative Group. J Clin Oncol 3(12):1583–1589. https://doi.org/10.1200/JCO.1985.3.12.1583
Cassileth PA, Lynch E, Hines JD, Oken MM, Mazza JJ, Bennett JM et al (1992) Varying intensity of postremission therapy in acute myeloid leukemia. Blood 79(8):1924–1930
Wei A, Roboz GJ, Dombret H, Döhner H, Schuh AC, Montesinos P et al (2020) CC-486 Improves Overall Survival (OS) and Relapse-Free Survival (RFS) for Patients with Acute Myeloid Leukemia (AML) in First Remission after Intensive Chemotherapy (IC), Regardless of Amount of Consolidation Received: Results from the Phase III QUAZAR AML-001 Maintenance Trial. Blood 136(Supplement 1):38–40
Chen EY, Joshi SK, Tran A, Prasad V (2019) Estimation of Study Time Reduction Using Surrogate End Points Rather Than Overall Survival in Oncology Clinical Trials. JAMA Intern Med 179(5):642–647. https://doi.org/10.1001/jamainternmed.2018.8351
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This article does not contain any studies with human participants performed by any of the authors.
Conflict of interest
Kristen Pettit, MD, provides advising for the following companies: Kura Oncology, PharmaEssentia, CTI Biopharma. Anthony J. Perissinotti, PharmD, is a consultant for Servier, Amgen, and Pfizer pharmaceuticals. Bernard L. Marini, PharmD, is a consultant for Servier. None of the other authors has any conflicts of interest to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ochs, M.A., Marini, B.L., Perissinotti, A.J. et al. Oncology stewardship in acute myeloid leukemia. Ann Hematol 101, 1627–1644 (2022). https://doi.org/10.1007/s00277-022-04872-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-022-04872-1