Abstract
Post-transplant lymphoproliferative disorders (PTLD) exclusively affecting the central nervous system—primary CNS-PTLD (pCNS-PTLD)—are rare. There is no standard therapy, and previous case series have included heterogeneous treatment approaches. We performed a retrospective, multi-centre analysis of 14 patients with pCNS-PTLD after solid organ transplantation (SOT) treated in the prospective German PTLD registry with reduction of immunosuppression (RI), whole-brain radiotherapy (WBRT), and concurrent systemic rituximab between 2001 and 2018. Twelve of fourteen patients were kidney transplant recipients and median age at diagnosis was 65 years. Thirteen of fourteen cases (93%) were monomorphic PTLD of the diffuse large B-cell lymphoma type, and 12/13 were EBV-associated. The median dose of WBRT administered was 40 Gy with a median fraction of 2 Gy. The median number of administered doses of rituximab (375 mg/m2) IV was four. All ten patients evaluated responded to treatment (100%). Median OS was 2.5 years with a 2-year Kaplan–Meier estimate of 63% (95% confidence interval 30–83%) without any recorded relapses after a median follow-up of 2.6 years. Seven of fourteen patients (50%) suffered grade III/IV infections under therapy (fatal in two cases, 14%). During follow-up, imaging demonstrated grey matter changes interpreted as radiation toxicity in 7/10 evaluated patients (70%). The combination of RI, WBRT, and rituximab was an effective yet toxic treatment of pCNS-PTLD in this series of 14 patients. Future treatment approaches in pCNS-PTLD should take into account the significant risk of infections as well as radiation-induced neurotoxicity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Post-transplant lymphoproliferative disorders (PTLD) are a rare but serious complication of immunosuppression after solid organ transplantation (SOT). PTLD exclusively affecting the central nervous system—primary CNS-PTLD (pCNS-PTLD)—are a still rarer subgroup epidemiologically associated with kidney transplantation, the use of immunosuppression including the antimetabolite mycophenolate, and a latency of years from transplantation to diagnosis [1, 2]. The most common histological subtype is diffuse large B-cell lymphoma (DLBCL) [1,2,3]. Epstein-Barr virus (EBV) is one of the major factors in the pathogenesis of PTLD [4]. It is detectable in systemic PTLD after SOT in about 50% of cases (referred to as EBV-association), most of which occur in the first 2 years after transplantation [5, 6]. In contrast, rates of EBV-association in pCNS-PTLD, which occur later after transplantation, are > 90% [1,2,3, 7]. While EBV protein expression is similar to systemic EBV-associated PTLD (type III latency pattern and lytic transcripts), distinct microRNA profiles have been identified in pCNS-PTLD in comparison with both EBV-associated and EBV-negative systemic PTLD [8].
Current treatment of primary CNS lymphoma in the immunocompetent is based on the results of randomized clinical trials [9, 10] and involves induction with intravenous high-dose methotrexate, cytarabine, thiotepa, and rituximab IV, followed by consolidation with either high-dose thiotepa-based chemotherapy and autologous stem cell transplantation or whole-brain radiotherapy (WBRT) [11]. The use of WBRT consolidation remains controversial [11, 12].
Case reports and small retrospective case series are the only source of evidence regarding the treatment of pCNS-PTLD [13, 14]. Treatment modalities range from reduction of immunosuppression (RI) [15], antiviral therapy [3], rituximab monotherapy [16], chemotherapy, and WBRT [1, 7] to the use of EBV-specific T-cells [17]. In addition, the successful use of intrathecal rituximab has been reported in children after haematopoietic stem cell transplantation [18, 19]. However, while there have been reports of successful treatment of single cases of pCNS-PTLD with low-intensity therapy such as RI only [15] and rituximab monotherapy [16], in a larger series, 5/6 patients treated with RI only and 3/8 treated with rituximab monotherapy progressed [1]. In this largest case series published to date (n = 84), treatment was highly heterogeneous, but included RI in 93% of patients and rituximab and HD methotrexate as the most common drug regime. Median OS was reported as 17 months. Cavaliere et al. reported a median OS of 25.4 months for the seven patients (out of a total of 34) in their pCNS-PTLD series who had been treated with WBRT ± other modalities [7].
Our goal was to evaluate the efficacy and toxicity of RI combined with WBRT and concurrent systemic rituximab in a cohort of uniformly treated patients reported to the prospective German PTLD registry.
Materials and methods
Study design and patients
The German PTLD registry database identified 42 patients with CNS involvement of PTLD, including 29 patients with pCNS-PTLD, 3 patients with concurrent systemic and CNS disease, and 10 patients with secondary CNS involvement as progression or relapse of systemic PTLD. We limited this retrospective analysis to 14 patients treated with 1st-line RI, WBRT, and concurrent systemic rituximab at eight German centres between 2001 and 2018. Five of these patients had previously been published as part of a retrospective case series including 84 patients with pCNS-PTLD from Europe and the USA [1].
In the prospective German PTLD registry, patients are reported at diagnosis after informed consent according to the Declaration of Helsinki. There is an option to get centralized treatment advice. The study group’s treatment recommendations for pCNS-PTLD between 2001 and 2018 were RI combined with weekly rituximab (375 mg/m2 IV) concurrent to WBRT or combined with 2–4 cycles of HD methotrexate (2–4 g/m2). The German PTLD registry was approved by the appropriate Ethics committees.
Histology and EBV-association
The diagnosis of PTLD was based on the examination of formalin-fixed, paraffin-embedded tissue, obtained either by stereotactic biopsy or resection. All diagnostic tissue samples including conventional histology as well as immunohistochemistry were reviewed by an expert haematopathologist and classified according to the criteria of the WHO classification [20]. An association with EBV was confirmed by in situ hybridization for Epstein-Barr virus–encoded small RNAs (EBER). Immunohistochemistry for EBV proteins (LMP1, EBNA2, and BZLF-1) was performed to determine EBV latency if sufficient material was available.
Staging, laboratory investigations, and immunosuppression
Disease stage at enrolment was determined through a complete patient history, physical examination, laboratory investigations (including full blood count, serum lactate dehydrogenase activity [LDH], renal and liver function tests, and immunoglobulin (Ig) subclasses), bone marrow biopsy, cerebrospinal fluid analysis, and computed tomography scans of the neck, chest, abdomen, and pelvis. All 14 patients had cranial MRI imaging before histological diagnosis. Intravenous contrast was administered in 10/14 patients. Reporting was not standardized. EBV viral load measurements in blood and cerebrospinal fluid were performed in local laboratories. Lymphocyte differentiation by flow cytometry was performed at the central laboratory in Kiel or in local laboratories. Doses of immunosuppressive drugs were collected as part of the baseline patient documentation. Immunosuppression before the diagnosis of PTLD was defined as immunosuppression at the last routine clinic visit before suspicion of PTLD; immunosuppression after diagnosis were the doses at the start of rituximab treatment, after reduction of immunosuppression.
Treatment
RI was at the discretion of the treating physician and was based on recommendations based on guidelines originally formulated for renal transplant recipients: stop antimetabolites (azathioprine and mycophenolate), reduce calcineurin inhibitors by 25–50%, and maintain corticosteroids [21, 22]. Rituximab was started immediately after diagnosis of CD20-positive PTLD and was administered systemically at a dose of 375 mg/m2 IV weekly until WBRT was completed. WBRT was performed as homogeneous irradiation of the whole cerebrum in analogy to pCNS lymphoma of the immunocompetent [12]. Pneumocystis jirovecii chemoprophylaxis was recommended from start of treatment until B-cell repopulation.
Response evaluation and follow-up
The schedule of final response and follow-up assessments followed local standards, based on the German guidelines for primary CNS lymphoma. Follow-up visits included a complete patient history, physical examination, laboratory investigations (including full blood count, LDH, as well as renal and liver function tests), and brain MRI. Response was evaluated by local radiology or neuro-radiology departments based on the MRI response criteria for primary CNS lymphoma [23]. Further investigations were performed if clinically indicated to determine remission status. Follow-up data was evaluated up to September 2019. Median follow-up was 2.6 years.
Evaluation of neurological sequelae
There was no formal, questionnaire-based assessment of neurological symptoms or activities of daily living either at diagnosis, at restaging, or at follow-up. In order to evaluate long-term neurological treatment toxicity, patient records were reviewed for documented clinical evidence of cognitive deterioration. Furthermore, follow-up cMRI imaging reports were reviewed for evidence of changes associated with WBRT.
Statistical analysis
OS was defined from start of treatment to death from any cause. Progression-free survival (PFS) was defined from start of treatment to disease progression or death from any cause. Exploratory analyses were performed using two-sided stratified log-rank tests. The two-sided significance level was set at 0.05 and statistical tests were performed using IBM SPSS 22.0.0.0.
Results
Patients
Baseline patient characteristics are summarized in Table 1. Median age at diagnosis of PTLD was 65 years (range 39–78). Nine out of 14 patients (64%) were female. Out of 14 patients, twelve were kidney, one liver, and one kidney/pancreas transplant recipients. Median time from transplantation to PTLD was 15.1 years. All 14 cases occurred more than 1 year after the last transplantation. Median serum creatinine at diagnosis was 2.4 mg/dl (range 0.8–3.6) and elevated above the upper limit of normal in 12/13 patients (92%). Serum immunoglobulin classes were measured at diagnosis in 7/14 patients: IgG levels were below the lower limit of normal (700 mg/dl) in 5/7 (71%) patients. IgA and IgM levels were below the lower limits of normal (70 and 40 mg/dl, respectively) in 3/7 patients (43%) each. Lymphocyte differentiation was performed at diagnosis in 6/14 patients: CD19 + lymphocyte counts were below 100/μl in 3/6 patients (50%) and CD8 + lymphocyte counts were below 200/μl in 4/6 patients (66%) ECOG performance status was ≤ 2 in 12/13 patients (92%). Four of eleven patients (36%) had an elevated serum LDH activity at diagnosis.
Disease characteristics
Baseline disease characteristics are summarized in Table 2. The vast majority of cases (13/14, 93%) were of DLBCL type, and 12/13 evaluated were EBV-associated. Seventy-eight percent (7/9) of examined cases showed expression of EBNA-2, and 67% (6/9) expression of BZLF-1. Cranial MRI scans demonstrated contrast-enhancing (9/9) lesions with perifocal edema (10/11), where reported. Six of fourteen patients (43%) had a single disease manifestations in the CNS, and 5/14 patients (36%) had more than five. Central necrosis was reported in 3/14 cases. Appearance on fluid-attenuated inversion recovery (FLAIR) sequences was hyperintense in 5/6 cases reported. The reports of appearance on T1- and T2-weighted imaging were variable: T1-weighted imaging was reported as either inhomogeneous (2/3) or not hyperintense (1/3), and T2-weighted imaging was reported as hyperintense (2/5), inhomogeneous (2/5), or not hyperintense (1/5). Differential diagnoses based on imaging were broad and included PTLD in 2/14 cases. Most likely, diagnoses (if listed) were CNS tumour/malignancy (5 cases, all 1–3 lesions), infection (4 cases, all > 5 lesions), and metastases (3 cases, single lesion in 2 cases, > 5 in one case). In two cases, imaging was described as not typical for lymphoma. Meningiosis defined as evidence of PTLD in a cytological examination of cerebrospinal fluid (CSF) was present in none of the patients. EBV DNA was present in the peripheral blood of 5/7 patients (71%) and in the CSF of 4/7 patients (57%). EBV viral load at diagnosis was not performed in the remaining seven patients.
Immunosuppression
Maintenance immunosuppression before and after diagnosis of PTLD is listed by drug class and individual drug in Table 3. All patients received the antimetabolite mycophenolate before diagnosis of PTLD. Only four patients continued mycophenolate after diagnosis. Five out of 14 patients (36%) were started on immunosuppression with an mTOR-inhibitor (everolimus in four patients and rapamycin in one patient) after diagnosis of PTLD.
Treatment administered
The median dose of WBRT administered was 40 Gy (range 14.4–45 Gy), with a median fraction of 2 Gy (range 1.5–2 Gy). Three of fourteen patients received a local boost to the tumour. The median number of administered doses of rituximab IV was 4 (range 2–8) Four patients died before completion of scheduled therapy. They included all three patients who received less than 37.5 Gy, as well as all three patients who received less than four applications of rituximab. With the exception of one patient who had previously been treated with systemic cyclophosphamide IV for cerebral vasculitis later diagnosed as pCNS-PTLD, none of the patients received any additional first- or second-line treatment of pCNS-PTLD. In this particular case, the local pathology report and reference neuropathologist diagnosed an inflammatory, necrotizing CNS process, likely cerebral vasculitis, but noted that lymphoma could not be excluded. The diagnosis of pCNS-PTLD was established independently by two additional reference pathologists (specializing in vasculitis and lymphoma, respectively), based on examination of the initial biopsy material. These examinations included morphology, immunohistochemistry, molecular analyses demonstrating B-cell oligoclonality, and EBER-ISH, which established EBV-association.
Treatment outcome
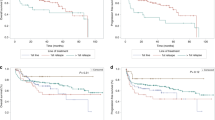
All ten patients evaluated had responded to treatment. Of four patients not evaluated, three had died before completion of treatment and one 75-year-old patient with multiple comorbidities did not return to the treating teaching hospital for restaging. One of the four patients who had died before completion of therapy had already been re-staged and had reached a partial response (PR). Four out of the ten patients evaluated (40%) had a complete response (CR), and six (60%) had a PR. Median OS was 2.5 years (Fig. 1) with a 2-year Kaplan–Meier estimate of 63% (95% confidence interval [95% CI], 30–83%). There were no recorded relapses among the 14 patients. Median PFS was therefore identical to OS (median 2.5 years, 2-year Kaplan–Meier estimate of 63% [95% CI, 36–89%]). Overall, eight out of 14 patients included died during the follow-up period. Causes of death were pneumonia in two patients; unknown in two cases; and one case each of aspiration, pulmonary embolism, sepsis, and cerebral oedema (in a patient undergoing radiotherapy who had been transferred to intensive care due to pneumonia).
Toxicity
Seven out of 14 patients (50%) suffered grade III/IV infections under therapy. These included four cases of pneumonia (including one case of Pneumocystis jirovecii) and four cases of sepsis. Infections under therapy were fatal in two cases (14%). Leukocyte counts were in or above the normal range in 5/6 patients with available data throughout the infection. Only one patient had mild leukopenia after developing streptococcal sepsis. During follow-up, cMRI demonstrated grey matter changes in T2/FLAIR sequences interpreted as radiation toxicity in seven out of ten evaluated patients (70%). This included 6/7 (86%) of evaluated women and 1/3 (33%) of evaluated men. In five out of ten patients (50%, all female, thus 5/7 (71% of females), there was anecdotal evidence in the medical records of cognitive deterioration, such as a deteriorating ability to remember and attend follow-up appointments, reports from relatives, or the necessity of nursing home care. One patient received a formal diagnosis of psychoorganic syndrome. In two patients, such deterioration was triggered by additional medical events (hip replacement surgery and Varicella zoster encephalitis, respectively).
Outcome in patients switched to mTOR-inhibitors
There was no significant difference in overall survival between five patients started on mTOR-inhibitors and the remaining nine patients (p = 0.578). Both fatal infections under therapy occurred in patients switched to mTOR-inhibitors.
Discussion
This retrospective multi-centre analysis is the largest published to date investigating RI, WBRT, and rituximab in pCNS-PTLD. In contrast to previously combined series [1, 7], a homogeneously treated cohort allows the assessment of a single treatment approach. All diagnoses were reviewed by specialized haematopathologists through the German PTLD study group’s reference pathology scheme.
Our series confirms previous epidemiological observations, such as the high prevalence of kidney SOT recipients (93%), the long latency period from the last transplantation (median 15.1 years), and the association with mycophenolate as maintenance immunosuppression (100%) [1,2,3]. The same is true for the prevalence of EBV-association (93%) and the pattern of EBV protein expression [3, 8]. To our knowledge, this is the first study of immunoglobulin levels and lymphocyte subsets in patients with pCNS-PTLD, even though data is only available in six and seven patients, respectively. Hypogammaglobulinaemia was present in 71% of evaluated patients and has been previously identified as a risk factor for infection in kidney transplant recipients [24]. In addition, absolute CD19 + B-cell and CD8 + T-cell counts were below the reference ranges in half of the evaluated patients before the start of treatment.
With an overall response rate of 100% of evaluated patients and no relapses in the follow-up period, this case series demonstrates that the combination of WBRT and rituximab is an effective treatment of pCNS-PTLD. Given that all patients who completed radiotherapy received at least 37.5 Gy, this does not allow any correlations between radiation dose and outcomes. Similarly, all patients were treated with rituximab. However, the excellent disease control in the present series supports the hypothesis that the efficacy of rituximab IV in pCNS lymphoma of immunocompetent patients as demonstrated in the IELSG32 trial applies to pCNS-PTLD as well [9]. On the other hand, we could not demonstrate any clinical benefit for the five patients started on immunosuppression with an mTOR-inhibitor compared to the remaining nine patients.
The median OS of 2.5 years is in the range reported by larger previous series (17 months and 47 months, respectively) [1, 7]. However, it is a disappointing outcome given the efficacy of treatment. In the six patients with a known cause of death, four died from infection (pneumonia in two cases, aspiration, sepsis), and the patient who died from cerebral oedema was in intensive care due to pneumonia. Thus, infections appear to be the main cause of mortality in this patient population.
We observed remarkably similar outcomes to a series (n = 13) of pCNS-PTLD treated with a very different approach, namely the combination of rituximab and dexamethasone with the antiviral agents zidovudine and ganciclovir [3]. These included ORR (92%), 2-year OS (76.9%), a lack of relapses, and the role of infections as the most common cause of death.
In contrast to the antiviral treatment approach, RI, WBRT, and rituximab resulted in significant toxicity including grade III/IV infections under therapy in 50% of patients (14% fatal), even higher than the 41% observed in a trial of rituximab followed by CHOP in systemic PTLD [5]. Furthermore, there was evidence of long-term CNS toxicity radiologically and clinically in 70% and 50% of patients, respectively. This was attributed to WBRT based in imaging morphology, but additional effects of viral infections (zoster encephalitis was diagnosed in one case) cannot be excluded in this long-term immunosuppressed cohort. The rates of neurotoxicity are in keeping with observations in immunocompetent patients with pCNS-PTLD who received early WBRT (combinations), particular those > 60 years [25, 26].
High early treatment-related mortality, the majority due to infections, has been described in previous case series of pCNS-PTLD: Evans et al. reported 13% (11/85 patients) [1]. Furthermore, infections were the most common cause of death in the abovementioned case series of combined antiviral treatment [3]. In contrast, a far lower rate of fatal toxicity (6%) was observed in immunocompetent patients undergoing aggressive polychemotherapy for pCNS lymphoma in a clinical trial [9]. The cause is most likely longstanding immunosuppression (median duration 15.1 years in this series), partially reflected in the numerical defects of humoral and cellular immunity discussed above and potentially aggravated by corticosteroid treatment of cerebral edema.
Limitations of this study include its retrospective format, the long recruitment period, and potential biases including selection bias. Median age at diagnosis was 65 years, compared to 43 and 52 years, respectively, in previous case series [1, 7]. In addition, 12/13 patients had an elevated serum creatinine (median 2.4 mg/dl). Both facts suggest a negative selection of patients judged poorly suited for therapy based on high-dose methotrexate.
In summary, the combination of WBRT and rituximab was an effective yet toxic treatment of pCNS-PTLD in this series of 14 patients. We identified numerical defects in humoral and cellular immunity even before the start of treatment and observed that infections were the leading cause of death, while long-term neurotoxicity was observed in at least 50% of patients.
Future treatment approaches in pCNS-PTLD should take into account the significant risk of infections as well as radiation-induced neurotoxicity in these often middle-aged and long-term immunosuppressed patients.
Data availability
Authors elect to not share data.
References
Evens AM, Choquet S, Kroll-Desrosiers AR et al (2013) Primary CNS posttransplant lymphoproliferative disease (PTLD): an international report of 84 cases in the modern era. Am J Transplant 13:1512–1522. https://doi.org/10.1111/ajt.12211
Crane GM, Powell H, Kostadinov R et al (2015) Primary CNS lymphoproliferative disease, mycophenolate and calcineurin inhibitor usage. Oncotarget 6:33849–33866. https://doi.org/10.18632/oncotarget.5292
Dugan JP, Haverkos BM, Villagomez L et al (2018) Complete and durable responses in primary central nervous system posttransplant lymphoproliferative disorder with zidovudine, ganciclovir, rituximab, and dexamethasone. Clin Cancer Res 24:3273–3281. https://doi.org/10.1158/1078-0432.CCR-17-2685
Dharnidharka VR, Webster AC, Martinez OM et al (2016) Post-transplant lymphoproliferative disorders. Nat Rev Dis Primers 2:15088. https://doi.org/10.1038/nrdp.2015.88
Trappe R, Oertel S, Leblond V et al (2012) Sequential treatment with rituximab followed by CHOP chemotherapy in adult B-cell post-transplant lymphoproliferative disorder (PTLD): the prospective international multicentre phase 2 PTLD-1 trial. Lancet Oncol 13:196–206. https://doi.org/10.1016/S1470-2045(11)70300-X
Trappe RU, Dierickx D, Zimmermann H et al (2017) Response to rituximab induction is a predictive marker in B-cell post-transplant lymphoproliferative disorder and allows successful stratification into rituximab or R-CHOP consolidation in an international, prospective, multicenter phase II trial. J Clin Oncol 35:536–543. https://doi.org/10.1200/JCO.2016.69.3564
Cavaliere R, Petroni G, Lopes MB et al (2010) Primary central nervous system post-transplantation lymphoproliferative disorder: an International Primary Central Nervous System Lymphoma Collaborative Group Report. Cancer 116:863–870. https://doi.org/10.1002/cncr.24834
Fink SEK, Gandhi MK, Nourse JP et al (2014) A comprehensive analysis of the cellular and EBV-specific microRNAome in primary CNS PTLD identifies different patterns among EBV-associated tumors. Am J Transplant 14:2577–2587. https://doi.org/10.1111/ajt.12858
Ferreri AJM, Cwynarski K, Pulczynski E et al (2016) Chemoimmunotherapy with methotrexate, cytarabine, thiotepa, and rituximab (MATRix regimen) in patients with primary CNS lymphoma: results of the first randomisation of the International Extranodal Lymphoma Study Group-32 (IELSG32) phase 2 trial. Lancet Haematol 3:e217-227. https://doi.org/10.1016/S2352-3026(16)00036-3
Ferreri AJM, Cwynarski K, Pulczynski E et al (2017) Whole-brain radiotherapy or autologous stem-cell transplantation as consolidation strategies after high-dose methotrexate-based chemoimmunotherapy in patients with primary CNS lymphoma: results of the second randomisation of the International Extranodal Lymphoma Study Group-32 phase 2 trial. Lancet Haematol 4:e510–e523. https://doi.org/10.1016/S2352-3026(17)30174-6
Fox CP, Phillips EH, Smith J et al (2019) Guidelines for the diagnosis and management of primary central nervous system diffuse large B-cell lymphoma. Br J Haematol 184:348–363. https://doi.org/10.1111/bjh.15661
Hoang-Xuan K, Bessell E, Bromberg J et al (2015) Diagnosis and treatment of primary CNS lymphoma in immunocompetent patients: guidelines from the European Association for Neuro-Oncology. Lancet Oncol 16:e322-332. https://doi.org/10.1016/S1470-2045(15)00076-5
Zimmermann H, Trappe RU (2013) EBV and posttransplantation lymphoproliferative disease: what to do? Hematology Am Soc Hematol Educ Program 2013:95–102. https://doi.org/10.1182/asheducation-2013.1.95
Dierickx D, Tousseyn T, Gheysens O (2015) How I treat posttransplant lymphoproliferative disorders. Blood 126:2274–2283. https://doi.org/10.1182/blood-2015-05-615872
Valavoor SH, Ashraf Z, Narwal R, Ratnam S (2013) Conservative management of post-transplant central nervous system lymphoma. Int Urol Nephrol 45:1219–1222. https://doi.org/10.1007/s11255-012-0146-8
Patrick A, Wee A, Hedderman A et al (2011) High-dose intravenous rituximab for multifocal, monomorphic primary central nervous system posttransplant lymphoproliferative disorder. J Neurooncol 103:739–743. https://doi.org/10.1007/s11060-010-0425-0
Velvet AJJ, Bhutani S, Papachristos S et al (2019) A single-center experience of post-transplant lymphomas involving the central nervous system with a review of current literature. Oncotarget 10:437–448. https://doi.org/10.18632/oncotarget.26522
Bonney DK, Htwe EE, Turner A et al (2012) Sustained response to intrathecal rituximab in EBV associated post-transplant lymphoproliferative disease confined to the central nervous system following haematopoietic stem cell transplant. Pediatr Blood Cancer 58:459–461. https://doi.org/10.1002/pbc.23134
Czyzewski K, Styczynski J, Krenska A et al (2013) Intrathecal therapy with rituximab in central nervous system involvement of post-transplant lymphoproliferative disorder. Leuk Lymphoma 54:503–506. https://doi.org/10.3109/10428194.2012.718342
Swerdlow SH, Webber SA, Chadburn A, Ferry JA (2017) Post-transplant lymphoproliferative disorders. In: Swerdlow SH, Campo E, Harris NL et al (eds) WHO classification of tumours of haematopoetic and lymphoid tissues, Revised, 4th edn. International Agency for Research on Cancer, Lyon, pp 453–462
Paya CV, Fung JJ, Nalesnik MA et al (1999) Epstein-Barr virus-induced posttransplant lymphoproliferative disorders. ASTS/ASTP EBV-PTLD Task Force and The Mayo Clinic Organized International Consensus Development Meeting. Transplantation 68:1517–1525
Parker A, Bowles K, Bradley JA et al (2010) Management of post-transplant lymphoproliferative disorder in adult solid organ transplant recipients-BCSH and BTS Guidelines. Br J Haematol 149:693–705. https://doi.org/10.1111/j.1365-2141.2010.08160.x
Abrey LE, Batchelor TT, Ferreri AJM et al (2005) Report of an international workshop to standardize baseline evaluation and response criteria for primary CNS lymphoma. J Clin Oncol 23:5034–5043. https://doi.org/10.1200/JCO.2005.13.524
Fernández-Ruiz M, López-Medrano F, Varela-Peña P et al (2012) Monitoring of immunoglobulin levels identifies kidney transplant recipients at high risk of infection. Am J Transplant 12:2763–2773. https://doi.org/10.1111/j.1600-6143.2012.04192.x
Gavrilovic IT, Hormigo A, Yahalom J et al (2006) Long-term follow-up of high-dose methotrexate-based therapy with and without whole brain irradiation for newly diagnosed primary CNS lymphoma. J Clin Oncol 24:4570–4574. https://doi.org/10.1200/JCO.2006.06.6910
Herrlinger U, Schäfer N, Fimmers R et al (2017) Early whole brain radiotherapy in primary CNS lymphoma: negative impact on quality of life in the randomized G-PCNSL-SG1 trial. J Cancer Res Clin Oncol 143:1815–1821. https://doi.org/10.1007/s00432-017-2423-5
Funding
The German PTLD registry has been supported through a grant from Roche Germany.
Author information
Authors and Affiliations
Consortia
Contributions
HZ, MN, and RUT designed the study. RUT is the principal investigator and takes primary responsibility for the paper. HZ, MN, CP, PR, NB, RMH, IAH, DH, MR, and RUT recruited and treated significant numbers of patients. HZ, MN, and RUT collected, analyzed, and interpreted the data. CP performed, analyzed, and collated radiology studies. MR performed reference flow cytometry. WK and IA performed reference haematopathology. HZ, MN, and RUT wrote the paper. All authors had full access to the final version of the manuscript and agreed to publication.
Corresponding author
Ethics declarations
Ethics approval
The German PTLD registry was approved by the appropriate Ethics committees.
Consent to participate
Patients provided informed consent to the German PTLD registry according to the Declaration of Helsinki.
Conflict of interest
Dr. Zimmermann reports institutional grants from Atara and Roche, and travel support from Atara, Celgene, and Jansen, outside the submitted work. Dr. Hauser reports personal fees or travel support from Astellas, Biotest, Hexal, Neovii, Novartis, and Roche, all outside the submitted work. Dr. Ritgen reports personal fees from Hoffman LaRoche, AbbVie, AstraZeneca, and Jansen, all outside the submitted work. Claudia Pietschmann reports travel support by KS Pharma, outside the submitted work. Dr. Trappe reports institutional grants from Atara and Roche and non-financial support from Roche, Atara, Celgene, Janssen, and AbbVie, all outside the submitted work. All other authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zimmermann, H., Nitsche, M., Pott, C. et al. Reduction of immunosuppression combined with whole-brain radiotherapy and concurrent systemic rituximab is an effective yet toxic treatment of primary central nervous system post-transplant lymphoproliferative disorder (pCNS-PTLD): 14 cases from the prospective German PTLD registry. Ann Hematol 100, 2043–2050 (2021). https://doi.org/10.1007/s00277-021-04548-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-021-04548-2