Abstract
Antimicrobial stewardship is of major importance in patients with febrile neutropenia (FN). In this study, we aimed to investigate the trends in resistance and the relationship with mortality rates in patients with FN. The single-center surveillance data of inpatients with FN and diagnosed as microbiologically confirmed bloodstream infections (BSIs) between 2006 and 2016 were reviewed retrospectively. A total of 950 episodes in 552 patients with BSIs were analyzed. Of whom, 55.9% were male, the median age was 43 years, and 35.6% had acute myeloid leukemia. In total, 1016 microorganisms were isolated from blood cultures. Gram-negatives accounted for 42.4% (n = 403) of the episodes. Among Gram-negatives, Enterobacteriaceae accounted for 346 (86%) (E. coli, n = 197; 34% extended-spectrum β-lactamases (ESBL) producers, and Klebsiella spp., n = 120; 48.3% ESBL producers). Also, 24 (20.0%) of Klebsiella spp. had carbapenemase activity. There were 6 (5.0%) colistin-resistant Klebsiella spp. Thirteen (26.5%) of Pseudomonas spp. and 17 (60.7%) of Acinetobacter spp. had carbapenemase activity. There were 2 (5.6%) colistin-resistant Acinetobacter spp. The 30-day mortality rates were 12.0%, 21.5%, 34.6%, and 29.0% in BSIs due to Gram-positive, Gram-negative bacterial, fungal, and polymicrobial etiology respectively (p = 0.001). BSIs with ESBL-producing (p = 0.001) isolates, carbapenem (p < 0.001), and colistin-resistant isolates (p < 0.001) were associated with increased mortality risk. The tremendous rise in resistance rates among Gram-negatives is dreadfully related to increasing mortality and leads to sharp shifts toward extreme restrictions of unnecessary antibiotic uses. Antimicrobial stewardship in patients with FN requires vigilance and tailoring of treatment upon local surveillance data.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Infections that develop in neutropenic patients are very important in terms of mortality and morbidity. Febrile neutropenia (FN) is a common and serious complication of chemotherapy in patients with hematological malignancies. Due to the suppression of symptoms and signs in this group, the only indicator of the infection may be fever [1,2,3]. Because of that, adequate and sufficient antimicrobial treatment should be immediately started. The microorganisms isolated from febrile neutropenic patients (FNPs) are different when compared with immunocompetent hosts. Also, they have different features particularly in terms of antimicrobial susceptibilities. These differences significantly affect empirical antimicrobial treatment preference.
The rise of resistant microorganisms underlines the need to learn more about epidemiology and infection control. Therefore, data of the locally prevalent pathogens and their susceptibilities are very important. In addition, antimicrobial resistance has been a fundamental problem in the neutropenic group in recent years. Besides increasing the rates of mortality and morbidity, the problem increases healthcare costs, extends the duration of hospital stay, and delays the administration of chemotherapy by the treatment failure [1,2,3].
The objective of this study is to investigate the relationship between antimicrobial resistance patterns of microorganisms in blood cultures from FNPs and their mortality rates. Accordingly, the policies of appropriate empirical antimicrobial usage would be determined through that investigating.
Methods
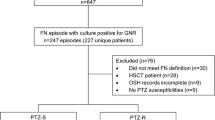
We conducted a single-center retrospective surveillance study of hospitalized FNPs with hematological malignancies and bloodstream infections (BSIs) that have been followed up by Infectious Diseases and Clinical Microbiology Department in collaboration with Hematology Department of Internal Medicine, from 2006 to 2016.
A patient who has both an absolute neutrophil count (ANC) of ≤ 500 cells/mm3 or an ANC that is expected to decrease to ≤ 500 cells/mm3 within 48 h and a fever of ≥ 38.0 °C at least sustained over an hour or a (single measure) fever of ≥ 38.3 °C at oral temperature measurement determined as a febrile neutropenic [3].
Only adult patients (≥ 18 years of age) were included in this study. All of the blood cultures were obtained from FNPs with hematological malignancies. The microorganisms were determined at the Infectious Diseases and Clinical Microbiology Laboratory. The samples that represented BSIs included peripheral blood and blood drawn through catheters. At least 2 positive cultures or one positive culture and presence of focus were required to define a bacteremia due to coagulase-negative staphylococci (CoNS), Corynebacterium spp., and Propionibacterium acnes as a BSI. The blood cultures were performed using the BACTEC (Becton Dickinson, Franklin Lakes, NJ, USA) automated system. Organisms were identified according to conventional procedures. The choice of antibiotic disks used was determined by the European Committee on Antimicrobial Susceptibility Testing (EUCAST) guidelines. Antibiotic susceptibility testing was performed on Mueller-Hinton agar by the Kirby Bauer’s disc diffusion method and additionally by the e-test method if required.
Microorganisms were classified by detecting the antimicrobial susceptibility profile. Multi-drug resistance (MDR) was defined as acquired nonsusceptibility to ≥ 3 different antimicrobial classes. Episodes that have identical antibiograms obtained from a single patient during the same hospitalization were accounted for once. The demographic data including age, sex and the type of underlying malignancy, culture results, use of empirical antibiotherapy, and presence or absence of central venous catheter-related BSIs were recorded and assessed. The clinical impact of the antimicrobial resistance was demonstrated by use of the epidemiological data. Mortality rates were defined as all-cause mortality up to 7 days and 30 days after BSIs.
The SPSS 21 (Chicago, IL) package program was used for statistical analysis. Univariate statistical analysis including Student’s t test was used for continuous data. Chi-square and Fisher’s exact test were used for categorical data. p values of < 0.05 were considered significant.
Results
A total of 950 episodes of BSIs in 552 patients were recorded. Of whom, 55.9% were male. The median age was 43 years (mean±sd 59.5 ± 15.9), and 35.6% had acute myeloid leukemia. In total, we isolated 1016 microorganisms. Gram-negative bacteria accounted for 403 (42.4%); Gram-positive bacteria accounted for 459 (48.3%). The remaining BSIs were polymicrobial and fungal in 6.5% (n = 62) and 2.7% (n = 26) of the episodes respectively. There was only 1 anaerobic isolate in these episodes. The distributions of these microorganisms causing BSIs and mortality rates are presented in Table 1.
Among 1016 microorganisms, the most common isolates were Staphylococcus spp. (n = 410, 40.4%), Escherichia coli (n = 197, 19.4%), and Klebsiella spp. (120, 11.8%). Staphylococcus spp. was the most common Gram-positive organism. They accounted for 80.8% of all Gram-positive isolates, with 26 Staphylococcus aureus and 384 CoNS. There were 51 (10%) isolates belonging to Enterococcus spp. and 31 (6.1%) to alpha-hemolytic streptococci. A total of 128 isolates among 62 episodes of polymicrobial BSIs were recorded. Gram-positive, Gram-negative, and fungal isolates were found in 39.1% (n = 50), 57.9% (n = 73), and 3.9% (n = 5) of polymicrobial BSIs respectively. The most frequent isolates of Gram-positive and Gram-negative bacteria in polymicrobial BSIs were CoNS (n = 23, 18.0%) and Escherichia coli (n = 23, 18.0%) respectively.
Methicillin resistance was observed in 19.2% of S. aureus isolates and 84.6% of CoNS isolates. All these isolates except Enterococcus spp. were sensitive to vancomycin and teicoplanin. Among Enterococcus spp., vancomycin resistance was 21.6% (Table 2).
Escherichia coli, Klebsiella spp., and Pseudomonas spp. were the most common Gram-negative organisms. Among Gram-negatives, Enterobacteriaceae accounted for 346 (86%) (E. coli, n = 197; 34% extended-spectrum β-lactamases (ESBL) producers, Klebsiella spp., n = 120; 48.3% ESBL producers). Also, 24 (20.0%) of Klebsiella spp. had carbapenemase activity. There were 6 (5.0%) colistin-resistant Klebsiella spp. There were 17 inducible beta-lactamases (IBL) producing Gram-negatives. Non-fermenters accounted for 119 (29.3%). Thirteen (26.5%) of Pseudomonas spp. and 17 (60.7%) of Acinetobacter spp. had carbapenemase activity. There were 2 (5.6%) colistin-resistant Acinetobacter spp. Among non-fermentatives, multi-drug-resistant (MDR) organisms constituted 60.7% of Acinetobacter spp. and 26.5% Pseudomonas spp. isolates in blood cultures. Percentages of the resistance patterns in Gram-negatives by years are demonstrated in Figs. 1 and 2. Among Gram-negatives, resistance rates were colistin 1.7% and carbapenem 13.6%. Gram-negative bacteria exhibited resistance to carbapenems and colistin after 2009 and 2011 respectively.
Among 31 fungal species, candida isolates were the most common organism. Five of them were in the polymicrobial episodes. The proportion of non-albicans species of candida isolates (n = 21/26) was quite high. Also, there were Trichosporon spp. (n = 3), Aspergillus fumigatus (n = 1), and Fusarium spp. (n = 1).
Piperacillin/tazobactam (34.6%) and carbapenems (34.4%) were found to be the most commonly initiated antibiotics empirically. One hundred thirty-two (13.8%) episodes were in hematopoietic stem cell recipients (HSCR). Acute myeloid leukemia (AML) was the most common diagnosis (35.6%) followed by acute lymphocytic leukemia (ALL) (17.6%) and non-Hodgkin lymphoma (14.3%).
Crude 30-day mortality was 17.7%. The 7-day rate was 12.0. The 30-day mortality rates were 12%, 21.5%, 34.6%, and 29% in BSIs due to Gram-positive, Gram-negative bacterial, fungal, and polymicrobial etiology respectively. The types of microorganisms were found to be related to the mortality rate (p = 0.001).
Among Gram-negatives, the 30-day mortality was significantly associated with the presence of resistance. BSIs with ESBL-producing (p = 0.001) isolates, carbapenem (p < 0.001), and colistin-resistant isolates (p < 0.001) were associated with increased mortality risk. Among Gram-positives, the 30-day mortality was not associated with the presence of resistance. Table 3 shows the relationship between resistance patterns and the 30-day mortality.
Catheter-related BSIs constituted 48.7% (n = 463) of total episodes. The 30-day crude mortality rate was 14.7% (n = 61). The mortality rate was lower in this group (p < 0.002).
While inappropriate empirical treatment was observed in 33.3% (n = 316/950) of BSIs, it was accounted for 39.7% (n = 48/121) of fatal BSIs (p = 0.139). There was an association between the use of carbapenems and mortality (p < 0.001). The mortality rate was the highest (33%) in initiated use of carbapenems. Empirical combination treatment (47.3%) was used in 449 episodes. Mortality was higher in the combination therapy group compared with the monotherapy group (11.8% vs 24.0% p < 0.001). Combination with teicoplanin or vancomycin (n = 389, 40.9%) was the most common choice. Combination with amikacin and combination with antifungals were used in 64 (6.7%) and 116 (12.2) episodes. Combination with more than one agent was used in 64 (6.7%) episodes. The deaths occurred 94 of the patients with acute leukemia (AML n = 63, ALL n = 31) and 35 of the patients with non-Hodgkin lymphoma. There was no significant relationship between underlying malignancy and 30-day mortality (p = 0.085).
Discussion
This study provides new evidence for the critical importance of close-monitorization of local epidemiology in guiding empirical treatment. We have demonstrated the major effect of changing resistance profiles in Gram-negatives on mortality by analyzing 950 episodes of bacteremia in 552 patients with FN. The 30-day mortality rates were 12.0%, 21.5%, 34.6%, and 29.0% in BSIs due to Gram-positive, Gram-negative bacterial, fungal, and polymicrobial etiology respectively. BSIs with ESBL-producing (p = 0.001) isolates, carbapenem (p < 0.001), and colistin-resistant isolates (p < 0.001) were associated with increased mortality risk. Thirty-day mortality was not significantly associated with the presence of resistance in patients with Gram-positive etiology. Catheter-related BSIs constituted 48.7% (n = 463) of total episodes, and the mortality was significantly lower (p < 0.002) in this group.
BSIs are of great importance to FNPs in terms of mortality and morbidity. The reported incidence of BSIs among neutropenic patients is 11–38%, and the crude mortality rate reaches up to 40%. The causative organisms of BSIs have changed over time. In the past, Gram-negative bacteria were more predominant causative agents. But an increasing incidence of Gram-positive bacteria has been reported over the last few decades, particularly from the developed countries [4,5,6].
While the epidemiology of BSIs comprised predominantly Gram-negative bacteria in FNPs in the 1960s–1970s, Gram-positive strains started to dominate in the mid-1980s worldwide. Also, it was noticed that BSIs developed by Gram-negative agents were associated with high mortality due to MDR strains [7]. Because of the epidemiological alteration, close monitoring changes in etiology and resistance patterns have been much more important to ensure the best empirical coverage.
In our study, CoNS (35.5%, n = 361) and Enterobacteriaceae (34%, n = 346) were the most common causes. While Gram-negative strains were the most common pathogens in some studies conducted before 2005, Gram-positive strains became the most common pathogens after 2005. In the study of Mikulska et al. [8], the rates of Gram-positive and Gram-negative isolates were 60% and 40%, respectively. The main pathogens of bacteremia were CoNS (25%) and Enterobacteriaceae (24%) respectively. In the same study, the questionnaire report of the European Conference on Infections in Leukemia (ECIL) participants showed that the median rates of Gram-positive and Gram-negative bacteria were 55% and 45%, respectively. And the most common pathogens were Enterobacteriaceae (30%) and CoNS (24%).
In the early 2000s, an increase in Gram-positive and a decrease in Gram-negative BSIs have been observed in general [9, 10]. This shift toward Gram-positives may possibly be related to the administration of the application of chemotherapy regimens leading to severe mucosity, fluoroquinolone prophylaxis, and the widespread use of indwelling catheters and other portal devices. However, in some centers, this trend has once again reversed, and in recent years Gram-negative bacteria have become more common than Gram-positives [11,12,13,14]. In the study of Mikulska et al., fluoroquinolone prophylaxis was associated with lower rate BSIs, but did not have an effect on mortality [15]. Our institute uses prophylaxis for the prevention of BSIs among patients with hematological malignancies. This explains Gram-positive predominancy in our institute. But the use of prophylaxis is generally restricted with patients who have prolonged neutropenia. Rönkkö et al. showed that fluoroquinolone prophylaxis in selected patients with high risk decreased Gram-negative BSIs [16]. Therefore, overall, there was no sharp shift but an increase from 44.9 to 48.3% in BSIs developed with Gram-negatives after 2010. Gram-negative bacteria were isolated more frequently in blood cultures in 2011 and 2014. But Gram-positives rebecame more common in the following years.
Gram-negative rods that cause BSIs in FNPs are the predominant organisms of the gastrointestinal tract. BSIs caused by these microorganisms are usually associated with disruption of mucosal integrity. Enterobacteriaceae are the most common cause of Gram-negative BSIs. Other Gram-negatives (e.g., Pseudomonas spp., Acinetobacter spp.) appear to be important pathogens in the hematology population. CoNS are described as skin normal flora members and generally considered to be contaminants when isolated in blood cultures [17]. However, these organisms may also be responsible for clinically important nosocomial bacteremia (particularly catheter-related). CoNS have been reported as the most commonly isolated Gram-positive bacteria in the blood cultures of neutropenic patients in various studies. Similarly, in our study, CoNS (35.5%) was the most frequently isolated Gram-positive bacteria in blood cultures. Among Gram-positives, S. aureus was much less frequent (n = 26, 5.1%) than CoNS. Also, methicillin-resistant S. aureus (MRSA) was low (n = 5, 1.0%) in our study. While the rate of Gram-positive bacteria was higher, the mortality rates were found to be lower compared with Gram-negatives in our study. It may be due to the fact that the Gram-positive pathogens were frequently CoNS and catheter-related. Also, the patients generally received early effective treatment for Gram-positives such as vancomycin or teicoplanin in the presence of clinical indications including suspected catheter-related BSI, soft-tissue infection, pneumonia, or hemodynamic instability.
In Europe’s southeast, Israeli and Turkey, the rates of resistance in Gram-negative bacteria have been observed to be high [8]. Noteworthy data for Gram-negative bacteria was the detection of carbapenem-resistant Enterobacteriaceae (CRE) (K. pneumoniae, E. coli), which was virtually absent in the late 1980s and reached 9.5% of patients in 2010–2011 [18]. Also, antimicrobial-resistant strains among these Gram-negatives have increased. In a study, the incidence of BSIs due to carbapenem-resistant K. pneumoniae increased 6-fold between 2010 and 2013 in HSCR [19]. In another study, carbapenem-resistance rate was 9% during neutropenia. In our country, carbapenem-resistant Gram-negatives emerged after 2010 as well. In our study, while carbapenem resistance was not found before 2010, it was found to be 6.5% in E. coli and 32.8% in Klebsiella spp. after 2010.
Pseudomonas spp. and Acinetobacter spp. have emerged as prominent MDR bacteria all over the world. Also in our study, the rates of these MDR organisms increased year by year. In a multicenter study conducted in Italy, 71% of the microorganisms had MDR [20]. In our study, the rates of carbapenem resistance and MDR were not detected in Pseudomonas spp. before 2010, but it was found to be 40% after 2010. A. baumannii is often resistant to cephalosporins or carbapenems and has emerged as a common pathogen isolated in BSIs in neutropenic patients [21]. There are some studies showing high antimicrobial resistance to Acinetobacter spp. in neutropenic patients. An increase in the rate of MDR A. baumannii has been observed with an increase in the prevalence of Acinetobacter spp. [22, 23]. In our study, MDR and carbapenem resistance before and after 2010 was found to be 15.7% and 82.3%, respectively.
Mortality rates in neutropenic patients have decreased from 25% in the late 1970s to 6% in recent years [24]. Generally, Gram-positive BSIs result with lower mortality compared with Gram-negative BSIs [25, 26]. In our study, crude mortality due to Gram-positive microorganisms was found to be 12.0%, while it was 23.6% in Gram-negatives. The rising in resistant Gram-negatives leads to an increase in mortality rates. Antibiotic resistance forces clinicians to select appropriate empirical antimicrobial agents in neutropenic patients with serious infections. However, unnecessary broad-spectrum antibiotic use results in higher resistance and mortality rates in both the general population and neutropenic patients. In the Italian cohort, infections caused by ESBL-producing isolates of hematology patients were associated with a 9-fold increased mortality risk [27]. In our study, the development of BSIs with ESBL-producing Gram-negative bacteria was associated with approximately 2.8-fold increased mortality risk (p = 0.001).
Also, CRE infections have become a major problem worldwide. In the study of Righi et al., it was associated with both high morbidity and mortality compared with susceptible microorganisms [28]. In the study of Gedik et al., they showed a mortality rate of 50% for carbapenem-resistant Gram-negatives in neutropenic patients [11]. In our study, the development of BSIs with CRE was associated with 10.8-fold increased mortality risk (p < 0.001). Colistin-resistant Gram-negative rods were associated with 27.5-fold increased mortality risk (p < 0.001). After these results, we modified our empirical treatment approach of FN by restricting unnecessary use of antibiotics, particularly carbapenems. Although it is difficult to implement because of a growing number of antimicrobial resistance, continuity is essential. In our center, we started to reserve primary administration of carbapenems for clinically unstable patients with colonization or previous infection by MDR microorganisms. Also, we restricted long duration indwelling catheters which may cause BSIs with antimicrobial resistant microorganisms.
In addition, our study was consistent with the study of Albiger et al. showing that the mortality rate was higher in polymicrobial BSIs (19% vs 12%; p = 0.07) compared with monomicrobial infections (p = 0.017) [29].
Our study has several limitations. First, it was conducted in a single center. Second, the study was retrospective. Third, we did not consider underlying comorbid diseases as risk factors and we did not run a multivariate regression analysis.
This study has also several strengths. First, this study showed the epidemiological changes including numerous patients over ten years. Second, this study has good generalizability because the results are broadly applicable to many different types of individuals and situations, even if differences in applications of the antimicrobial treatment and prophylaxis, infection control policies, and resistance patterns of microorganisms between centers affect the results.
Conclusion
In conclusion, the tremendous rise in resistance rates among Gram-negatives is dreadfully related to increased mortality and leads to sharp shifts toward extreme restrictions of unnecessary antibiotic uses. Antimicrobial governance programs based on active surveillance data and led by multidisciplinary teams should strictly be applied in such centers in order to improve patient outcomes and overcome the pressure of a forthcoming pan-drug-resistant era.
Abbreviations
- FN:
-
febrile neutropenia
- BSIs:
-
bloodstream infections
- ESBL:
-
extended-spectrum β-lactamases
- MDR:
-
multi-drug resistant
- FNPs:
-
febrile neutropenic patients
- ANC:
-
absolute neutrophil count
- CoNS :
-
coagulase-negative staphylococci
- EUCAST:
-
European Committee on Antimicrobial Susceptibility Testing
- HSCR:
-
hematopoietic stem cell recipients
- AML:
-
acute myeloid leukemia
- ALL:
-
acute lymphocytic leukemia
- ECIL:
-
European Conference on Infections in Leukemia
- CRE:
-
carbapenem-resistant Enterobacteriaceae
References
Freifeld AG, Bow EJ, Sepkowitz KA, Boeckh MJ, Ito JI, Mullen CA, Raad II, Rolston KV, Young JA, Wingard JR, Infectious Diseases Society of America (2011) Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis 52:e56–e93. https://doi.org/10.1093/cid/cir073
Averbuch D, Orasch C, Cordonnier C, Livermore DM, Mikulska M, Viscoli C, Gyssens IC, Kern WV, Klyasova G, Marchetti O, Engelhard D, Akova M, on behalf of ECIL4, a joint venture of EBMT, EORTC, ICHS, ESGICH/ESCMID and ELN (2013) European guidelines for empirical antibacterial therapy for febrile neutropenic patients in the era of growing resistance. Haematologica 98:1826–1835. https://doi.org/10.3324/haematol.2013.091025.DE
Taplitz RA, Kennedy EB, Bow EJ, Crews J, Gleason C, Hawley DK, Langston AA, Nastoupil LJ, Rajotte M, Rolston K, Strasfeld L, Flowers CR (2018) Outpatient management of fever and neutropenia in adults treated for malignancy: American Society of Clinical Oncology and Infectious Diseases Society of America clinical practice guideline update. J Clin Oncol 36(14):1443–1453. https://doi.org/10.1200/JCO.2017.77.6211
Trecarichi EM, Tumbarello M (2014) Antimicrobial-resistant Gram-negative bacteria in febrile neutropenic patients with cancer: current epidemiology and clinical impact. Curr Opin Infect Dis 27:200–210. https://doi.org/10.1097/QCO.0000000000000038
Pagano L, Caira M, Rossi G et al (2012) A prospective survey of febrile events in hematological malignancies. Ann Hematol 91:767–774. https://doi.org/10.1007/s00277-011-1373-2
Wisplinghoff H, Seifert H, Wenzel RP, Edmond MB (2003) Current trends in the epidemiology of nosocomial bloodstream infections in patients with hematological malignancies and solid neoplasms in hospitals in the United States. Clin Infect Dis 36:1103–1110. https://doi.org/10.1086/374339
Gudiol C, Bodro M, Simonetti A, Tubau F, González-Barca E, Cisnal M, Domingo-Domenech E, Jiménez L, Carratalà J (2013) Changing aetiology, clinical features, antimicrobial resistance, and outcomes of bloodstream infection in neutropenic cancer patients. Clin Microbiol Infect 19:474–479. https://doi.org/10.1111/j.1469-0691.2012.03879.x
Mikulska M, Viscoli C, Orasch C, Livermore DM, Averbuch D, Cordonnier C, Akova M, Fourth European Conference on Infections in Leukemia Group (ECIL-4), a joint venture of EBMT, EORTC, ICHS, ELN and ESGICH/ESCMID (2014) Aetiology and resistance in bacteraemias among adult and paediatric haematology and cancer patients. J Inf Secur 68:321–331. https://doi.org/10.1016/j.jinf.2013.12.006
Safdar A, Rodriguez GH, Balakrishnan M, Tarrand JJ, Rolston KVI (2006) Changing trends in etiology of bacteremia in patients with cancer. Eur J Clin Microbiol Infect Dis 25:522–526. https://doi.org/10.1007/s10096-006-0173-4
Viscoli C, Castagnola E (2002) Treatment of febrile neutropenia: what is new? Curr Opin Infect Dis 15:377–382. https://doi.org/10.1097/00001432-200208000-00004
Gedik H, Şimşek F, Kantürk A et al (2014) Bloodstream infections in patients with hematological malignancies: which is more fatal – cancer or resistant pathogens? Ther Clin Risk Manag 10:743–752. https://doi.org/10.2147/TCRM.S68450
Samonis G, Vardakas KZ, Maraki S, Tansarli GS, Dimopoulou D, Kofteridis DP, Andrianaki AM, Falagas ME (2013) A prospective study of characteristics and outcomes of bacteremia in patients with solid organ or hematologic malignancies. Support Care Cancer 21:2521–2526. https://doi.org/10.1007/s00520-013-1816-5
Yemişen M, Balkan İİ, Salihoğlu A, Eskazan AE, Mete B, Ar MC, Öngören Ş, Başlar Z, Özaras R, Saltoğlu N, Mert A, Ferhanoğlu B, Öztürk R, Tabak F, Soysal T (2016) Hematopoetik kök hücre nakli alicilarinda kan akim enfeksiyonu ve direnç epidemiyolojisindeki değişim. Turkish J Hematol 33:216–222. https://doi.org/10.4274/tjh.2014.0378
Parodi RL, Lagrutta M, Tortolo M, Navall E, Rodríguez MS, Sasia GF, de Candia LF, Gruvman MA, Bottasso O, Greca AA (2019) A multicenter prospective study of 515 febrile neutropenia episodes in Argentina during a 5-year period. PLoS One 14(10):e0224299. https://doi.org/10.1371/journal.pone.0224299
Mikulska M, Averbuch D, Tissot F, Cordonnier C, Akova M, Calandra T, Ceppi M, Bruzzi P, Viscoli C, Akova M, Aljurf M, Averbuch D, Barnes R, Blennow O, Bochud PY, Bouza E, Bretagne S, Brüggemann R, Calandra T, Carratala J, Cesaro S, Cordonnier C, Cornely O, Dalianis T, de la Camara R, Donnelly P, Drgona L, Duarte R, Einsele H, Engelhard D, Fox C, Girmenia C, Groll A, Heldal D, Larsen JH, Herbrecht R, Hirsch H, Johnson E, Klyasova G, Koskuenvo M, Lagrou K, Lewis RE, Ljungman P, Maertens J, Maschmeyer G, Mikulska M, Nucci M, Padoin C, Pagano L, Pagliuca A, Racil Z, Ribaud P, Rinaldo C, Puechal VR, Roilides E, Robin C, Rovira M, Rupp M, Sanchez S, Schellongowski P, Sedlacek P, Sinko J, Slavin M, Ferreira IS, Styczynski J, Tissot F, Viscoli C, Ward K, Witschi AT (2018) Fluoroquinolone prophylaxis in haematological cancer patients with neutropenia: ECIL critical appraisal of previous guidelines. J Inf Secur 76(1):20–37. https://doi.org/10.1016/j.jinf.2017.10.009
Rönkkö R, Juutilainen A, Koivula I, Vänskä M, Nousiainen T, Jantunen E, Hämäläinen S (2018) Changes in the microbiological epidemiology of febrile neutropenia in autologous stem cell transplant recipients. Infect Dis (Lond) 50(6):436–442. https://doi.org/10.1080/23744235.2017.1420221
Worth LJ, Slavin MA (2009) Bloodstream infections in haematology: risks and new challenges for prevention. Blood Rev 23:113–122. https://doi.org/10.1016/j.blre.2008.10.003
Daitch V, Akayzen Y, Abu-Ghanem Y, Eliakim-Raz N, Paul M, Leibovici L, Yahav D (2018) Secular trends in the appropriateness of empirical antibiotic treatment in patients with bacteremia: a comparison between three prospective cohorts. Eur J Clin Microbiol Infect Dis 37:455–462. https://doi.org/10.1007/s10096-018-3190-1
Girmenia C, Rossolini GM, Piciocchi A et al (2015) Infections by carbapenem-resistant Klebsiella pneumoniae in SCT recipients: a nationwide retrospective survey from Italy. Bone Marrow Transplant 50:282–288. https://doi.org/10.1038/bmt.2014.231
Cattaneo C, Antoniazzi F, Casari S, Ravizzola G, Gelmi M, Pagani C, D’Adda M, Morello E, Re A, Borlenghi E, Manca N, Rossi G (2012) P. aeruginosa bloodstream infections among hematological patients: an old or new question? Ann Hematol 91:1299–1304. https://doi.org/10.1007/s00277-012-1424-3
Kim SB, Min YH, Cheong JW, Kim JS, Kim SJ, Ku NS, Jeong SJ, Han SH, Choi JY, Song YG, Kim JM (2014) Incidence and risk factors for carbapenem-and multidrug-resistant Acinetobacter baumannii bacteremia in hematopoietic stem cell transplantation recipients. Scand J Infect Dis 46:81–88. https://doi.org/10.3109/00365548.2013.857042
Mikulska M, Del Bono V, Raiola AM et al (2009) Blood stream infections in allogeneic hematopoietic stem cell transplant recipients: reemergence of Gram-negative rods and increasing antibiotic resistance. Biol Blood Marrow Transplant 15:47–53. https://doi.org/10.1016/j.bbmt.2008.10.024
Garnica M, Maiolino A, Nucci M (2009) Factors associated with bacteremia due to multidrug-resistant Gram-negative bacilli in hematopoietic stem cell transplant recipients. Brazilian J Med Biol Res 42:289–293. https://doi.org/10.1590/S0100-879X2009000300010
Beyar-Katz O, Dickstein Y, Borok S, Vidal L, Leibovici L, Paul M, Cochrane Gynaecological, Neuro-oncology and Orphan Cancer Group (2017) Empirical antibiotics targeting gram-positive bacteria for the treatment of febrile neutropenic patients with cancer. Cochrane Database Syst Rev 2017. https://doi.org/10.1002/14651858.CD003914.pub4
Rosa RG, Dos Santos RP, Goldani LZ (2014) Mortality related to coagulase-negative staphylococcal bacteremia in febrile neutropenia: a cohort study. Can J Infect Dis Med Microbiol 25:14–18. https://doi.org/10.1155/2014/702621
Han SB, Bae EY, Lee JW, Lee DG, Chung NG, Jeong DC, Cho B, Kang JH, Kim HK (2013) Clinical characteristics and antimicrobial susceptibilities of viridans streptococcal bacteremia during febrile neutropenia in patients with hematologic malignancies: a comparison between adults and children. BMC Infect Dis 13:. https://doi.org/10.1186/1471-2334-13-273
Trecarichi EM, Tumbarello M, Spanu T, Caira M, Fianchi L, Chiusolo P, Fadda G, Leone G, Cauda R, Pagano L (2009) Incidence and clinical impact of extended-spectrum-β-lactamase (ESBL) production and fluoroquinolone resistance in bloodstream infections caused by Escherichia coli in patients with hematological malignancies. J Inf Secur 58:299–307. https://doi.org/10.1016/j.jinf.2009.02.002
Righi E, Peri AM, Harris PNA, Wailan AM, Liborio M, Lane SW, Paterson DL (2017) Global prevalence of carbapenem resistance in neutropenic patients and association with mortality and carbapenem use: systematic review and meta-analysis. J Antimicrob Chemother 72:668–677. https://doi.org/10.1093/jac/dkw459
Albiger B, Glasner C, Struelens M et al (2015) Carbapenemase-producing Enterobacteriaceae in Europe: assessment by national. Euro Surveill 20. https://doi.org/10.2807/1560-7917.ES.2015.20.45.30062
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Written informed consent was waived, given the retrospective nature of this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kara Ali, R., Surme, S., Balkan, I.I. et al. An eleven-year cohort of bloodstream infections in 552 febrile neutropenic patients: resistance profiles of Gram-negative bacteria as a predictor of mortality. Ann Hematol 99, 1925–1932 (2020). https://doi.org/10.1007/s00277-020-04144-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-020-04144-w