Abstract
Prognosis in relapsed and refractory acute myeloid leukemia (R/R AML) patients is dismal, with no satisfactory and standard salvage chemotherapy regimen. We performed a systematic review in order to analyze the clinical outcomes reported with conventional chemotherapy schemes in adult patients with R/R AML. To have a better understanding of the R/R ground, we included studies in R/R AML adult population at any disease stage (i.e., primary refractory as well as first relapse or beyond). Study selection included a total number of 157 out of 850 records, with a wide variety of schedules. Furthermore, only 24 studies were randomized clinical trials (RCTs), being the majority of the studies retrospective analyses in small cohorts. This review reveals that several intensive regimens (cytarabine + mitoxantrone + etoposide or gemtuzumab, and cytarabine + purine analogue ± antracycline) achieve relatively high complete remission (CR) rates (44 to 59.4%). However, most of these schemes did not obtain substantial CR duration (4.9 to 9.8 months) or overall survival (6.2 to 8.7 months). In unfit/vulnerable patients non-intensive approaches are recommended to control disease progression and minimize treatment-related mortality. A better knowledge of the prognostic factors, more effective and less toxic combinations using conventional and new therapies, as well as improvements in allo-HSCT procedure and timing, could play a role to improve the clinical outcomes in the future. Clinical trials should be the first treatment option in R/R AML, both in fit and unfit patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although 60–80% of acute myeloid leukemia (AML) adult patients achieve complete remission (CR) after the first induction chemotherapy, roughly 20% will show primary refractory disease and more than 50% will relapse [1, 2]. Despite salvage treatment, the clinical outcomes of these patients are poor, but acceptable survival rates are achievable depending on prognostic factors and intensity of treatment. The goal of salvage therapy is to achieve a CR in order to perform an allogeneic hematopoietic stem cell transplant (allo-HSCT), which appears to be the most curative therapy in this setting [1]. However, many patients will not proceed to allo-HSCT because of salvage therapy failure or because of inadequate fitness for this procedure. Furthermore, many frail patients will not receive an intensive chemotherapy with a curative intention, enabling the use of non-intensive approaches.
Information about therapy, outcomes, and prognostic factors in the relapsed/refractory (R/R) setting is derived from phase 1 to 3 clinical trials (the latter are very scarce) or from collaborative group registries and protocols, and no standard salvage treatment is established to obtain CR after resistance or relapse [2,3,4,5,6,7,8,9,10,11,12,13]. It is generally accepted that the enrollment in clinical trials using novel therapies could be the best option in this setting, although the efficacy of these treatments remains unclear, still under evaluation, and non-available for the vast majority of R/R AML patients. The aim of this study is to perform a systematic review of the literature to analyze the clinical outcomes reported with all the available conventional chemotherapy regimens in adult patients with R/R AML.
Materials and methods
Search strategy and selection of studies
This systematic review was conducted and reported in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) guidelines [14] by two independent authors (JMV and PM).
We searched the following databases without restrictions: MEDLINE, Cochrane Central Register, EMBASE, Web of Science and Database of Abstracts of Reviews of Effects (DARE), ProQuest Medical Library, and EBSCOhost Online Research Databases. We also hand searched the reference lists of important studies and reviews. The literature last search was on 2 May 2017.
Similar keywords were used in different databases: “acute myeloid leukemia” and relapse (or recurrence or recrudescence or resistance or “salvage therapy” or “salvage treatment”) and “Clinical Trial” [Publication Type] not “acute promyelocytic leukemia” not “Clinical Trial, Phase I” [Publication Type].
Study selection was conducted by both authors independently. In case of disagreement, a third reviewer (DMC) decided. Studies that fulfilled the following criteria were included: (1) AML studies using conventional chemotherapy agents for R/R adult AML patients, (2) studies evaluating one or more salvage therapies individually, and (3) studies including effectiveness variables, at least complete remission (CR) rate. Studies that included patients with promyelocytic leukemias and exclusively pediatric or elderly patients were excluded. Furthermore, studies performed in targeted therapy/small molecules cohorts and studies including donor lymphocyte infusions were excluded.
Data extraction
The following data was extracted (summarized in Tables 1, 2, 3, 4, 5, and 6): study design, chemotherapy schedule, AML status (especially the number of R/R patients included), median age, clinical response, and survival rates. The induction outcomes collected were as follows: CR and early death (ED). The CR rate reported for each study summarized in one term the CR rate reported in the study, as well as the CR with incomplete blood count recovery (CRi) and CR without platelet recovery (CRp), because CRi and/or CRp were only reported separately in 21 of the last studies. The CR rates of the subgroups of relapsed, refractory, early relapse (ER) in patients with first CR (CR1) ≤ 6–12 months, late relapse (LR) in patients with > 1 year of CR1, second or beyond relapse or refractory relapse (≥2ndR), and relapse after HSCT, were calculated when this data was provided by the primary sources. We included in the ED rate the cases of induction death, aplastic death, and toxic death reported in a reduced number of studies. The survival rates included were overall survival (OS), disease-free survival (DFS), event-free survival (EFS), and relapse-free survival (RFS). The median OS (mOS) and CR durations (mCRD) were reported in months, and they were estimated in months in the cases that they were reported in days (1 month = 30 days) or weeks (1 month = 4.3 weeks). To better describe the reported series, we showed in the “Results” section the weighted mean and the ranges of CR (wmCR), mOS (wmOS), and mCRD (wmCRD) of different studies adjusted by the sample size, unless more than four studies analyzed the same regimen outcomes.The weighted mean was calculated by summing the product of each variable by its sample size of the different studies and dividing the result by the sum of all the sample sizes. Furthermore, we have represented the CR rates and mOS obtained with the different salvage therapies with boxplot diagrams when we have data from at least four studies (IBM SPSS Statistics version 22, IBM Corp., Chicago, IL, USA). The frequency of allogeneic or autologous HSCT after salvage regimen was also extracted. The studies with less than 40 patients are not shown in Tables 1, 2, 3, 4, 5, and 6, with the exception of the schemes with less than three published studies which were maintained in the tables. The full versions of Tables 1, 2, 3, 4, 5, and 6 were included in the Supplemental Material (Supplemental Tables 1–6).
Results
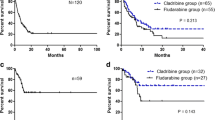
Systematic search obtained 783 citations from databases and journals and 67 records identified through other sources (Fig. 1). Of the 190 citations selected for full reading, only 157 fulfilled the inclusion criteria and were included (all in English). Reviewers showed an excellent agreement in study selection (kappa = 0.91). The differences in CR and mOS between the main salvage therapies could be visualized with boxplot diagrams in the Figs. 2 and 3.
Boxplot diagram of the complete remission rate of the different salvage therapies. The simple size for each scheme, excluding the outliers, was as follows: HIDAC 350; IDAC 686; MITO + Ara-C 801; AMSA + Ara-C 264; MEC 827; MIDAM 326; FLA 206; FLAG 402; CLAG 241; FLAG-IDA intermittent infusion 539; FLAG-IDA CI 135; CLOFA 369; CARBO 143; AZA 537; hypomethylating agents (AZA or DAC) 868; GO 462. The outliers are identified with the reference and two different markers: small circle for “out” values and asterisk for “far out” or “extreme values” (more than three times the height of the boxes)
Boxplot diagram of the median overall survival reported of the different salvage therapies. The simple size for each scheme, excluding the outliers, was as follows: HIDAC 248; IDAC 599; MITO + Ara-C 578; AMSA + Ara-C 172; MEC 536; MIDAM 188; FLA 147; FLAG 219; CLAG 221; FLAG-IDA intermittent infusion 527; FLAG-IDA CI 135; CLOFA 252; AZA 537; GO 358. The outliers are identified with the reference and two different markers: small circle for “out” values and asterisk for “far out” or “extreme values” (more than three times the height of the boxes)
Cytarabine monotherapy regimens
Eleven of the selected citations included Ara-C monotherapies with intermediate or high doses (from 500 mg/m2 to 3 g/m2 every 12 h) in the schedules analyzed (Table 1) [8, 15,16,17,18,19,20,21,22,23,24], frequently employed as a comparator of new schemes in randomized clinical trials (CFTs). The results observed in these cohorts were wmCR rate of 23.1% (range 12–32%), wmCRD of 6.3 months (range 0.9 to 11.9), and wmOS 5.8 months (range 3.6 to 8) only reported in 6 studies [16, 18,19,20,21,22]. We should mention that the first study using a high dose of Ara-C (HiDAC) of 3 g/m2/12 h was performed in a small cohort of younger R/R patients showing a higher CR rate of 47%, but the mCRD was 5 months [15].
In general, the HiDAC schedules showed higher wmCR rate of 28% (range 12–47%) [8, 15, 16, 18, 19, 23] than intermediate doses of Ara-C (IDAC), 1 g/m2/12 h or 500 mg/m2/12 h, with mCR rate of 20.6% (range 19–25%) [8, 17, 20,21,22]. However, Estey et al. did not obtain differences between HiDAC and IDAC cohorts in a retrospective non-RCT (CR 23 and 25%) [8]. A study analyzed the use of Ara-C continuous infusion (CI) in a small relapsed cohort obtaining poor results (CR 12%) [24].
Anthracycline plus cytarabine-based regimens
Thirty-eight studies based on these regimens were included (Table 2) [4, 5, 7, 15, 19,20,21,22, 25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57]. The most studied combination was mitoxantrone plus Ara-C (17 studies) [4, 5, 19, 25,26,27,28,29, 39,40,41, 43, 46, 47, 50,51,52]. This scheme showed a wmCR rate of 50% (range: 32–79%), wmCRD of 4.8 months (range 2.9–12), and wmOS of 5.4 months (range 3–12). Other anthracyclines were used in combinations with Ara-C:
-
Daunorubicin (two studies), with CR rates from 33 to 59% [15, 30].
-
Amsacrine (seven studies), with a wmCR rate of 54.3% (range 46–75%) [7, 27, 42, 44, 48, 49, 53].
-
Idarubicin (four studies), with CR rates from 35 to 60% [31, 32, 45, 55].
-
Aclarubicin (four studies), always plus granulocyte colony-stimulated factor (G-CSF), with CR rates from 51 to 83% [33, 34, 54, 57].
-
Liposomal daunorubicin (three studies), with CR rates from 7 to 47% [35, 36, 56].
-
Liposome-encapsulated fixed-molar-ratio formulation of Ara-C plus daunorubicin (one study), with CR rate of 37% [37].
The published evidence did not report superiority of any of the anthracyclines, although the experience with mitoxantrone is more extensive. A RCT compared two schedules combining HiDAC with two different anthracyclines, mitoxantrone and amsacrine [27]. Both regimens showed similar CR rates (58 vs. 46%) and mOS (12 vs. 8 months), but severe gastrointestinal toxicity was significantly higher with amsacrine (27 vs. 4%, p = 0.021). A retrospective study from the French AML Intergroup performed in a subgroup of core-binding factor (CBF) AML in first relapse showed the highest CR rate of 88% with combinations of Ara-C and different anthracyclines [38].
Anthracycline plus cytarabine plus third-agent based regimens
The addition of a third neoplastic agent, usually etoposide, to the Ara-C plus anthracycline combination has been broadly used (Table 3) [34, 38, 58,59,60,61,62,63,64,65,66,67,68,69,70,71,72, 74,75,76,77,78,79,80,81,82]. The combination of mitoxantrone, etoposide, and Ara-C (MEC or EMA schemes) is the most reported with a wmCR rate of 52.5% (range 24–68%), wmCRD of 5.3 months (range 1.5–12), and wmOS of 6.8 months (range 2.1–10.1) [58,59,60,61,62,63,64,65,66,67, 79,80,81,82]. The addition of G-CSF did not modify the efficacy of MEC scheme in one non-RCT and two RCTs [59, 60, 63]. Similar schemes with other anthracyclines plus etoposide and Ara-C have been tested, including idarubicin (one study) [68], daunorubicin (two studies) [69, 70], amsacrine (one study) [71], and aclarubicin (one study) [34], with CR rates from 33 to 71%.
The MIDAM combination of mitoxantrone, Ara-C, and gemtuzumab ozogamicin (GO) was analyzed in five different retrospective studies, with a wmCR rate of 59.4% (range 53–88) and wmOS of 12.6 months (range 7.2–16) [38, 75,76,77,78]. In this analysis, we excluded the study of Hospital MA et al. performed only in R/R CBF-AML, obtaining a 88% CR rate and an OS at 5 years of 65% (65% of patients received HSCT) [38]. The most recent study compared the use of GO as a single dose or fractionated in three doses, showing a non-significant better results with fractionated scheme [77]. A new scheme combining HiDAC, mitoxantrone, GO and all-trans retinoic acid (ATRA) in AML refractory to first induction reported CR rate of 51% and mOS of 16 months [78].
Other schemes were tested in a single study, combining Ara-C plus anthracyclines with vincristine [73], dacarbazine [74], or decitabine [72].
Purine analogue plus cytarabine-based regimens
Purine nucleoside analogs have shown a synergistic interaction with Ara-C through increasing the Ara-C intracellular accumulation, [8, 104, 106], and the addition of G-CSF has been related to higher Ara-C-mediated cytotoxicity [168]. Our search obtained 48 studies combining purine analogs with Ara-C-based schedules (Table 4) [8, 21, 32, 41, 67, 70, 83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123, 169].
-
Fludarabine + Ara-C regimens
Thirteen studies included combinations of fludarabine and Ara-C with or without G-CSF, schemes usually called FLA and FLAG, respectively [8, 70, 83,84,85,86, 88, 106,107,108,109,110, 123], showing a wmCR rate of 45.3% (range 19–63%), wmCRD of 9.8 months (range 2.3–17.1), and wmOS of 7.2 months (range 3.2–14.3). Despite the differences observed between wmCR rates of FLA (28.8%, range 19–39%) [8, 70, 85, 86, 123] and FLAG (53.3%, range 20–63%) [70, 83, 84, 86, 88, 106,107,108,109,110], the only two studies comparing both schemes did not show significant differences in CR, DFS, or OS [70, 86].
-
Cladribine + Ara-C regimens
Six studies included schemes of cladribine and Ara-C, always combined with G-CSF (CLAG) [67, 89, 90, 111, 121], with the exception of one study with CLA [104]. The CLAG scheme showed wmCR rate of 45.5% (range 38–52%), wmCRD of 6 months (range 5.2–7.4), and wmOS of 6.8 months (range 5.6 to 7.9) [67, 89, 90, 111, 121].
-
Fludarabine + Ara-C + idarubicin regimens (FLAG-IDA)
Eleven studies reported FLAG-IDA with Ara-C intermittent infusion [32, 91, 92, 95, 113,114,115, 118] or Ara-C in CI (CI-FLAG-IDA) [88, 94, 120]. The outcomes of FLAG-IDA schedule were better than CI-FLAG-IDA, showing higher CR rate (weighted mean 52.9%, range 42–69 vs. 34.3%, range 31–37%), mCRD (16, range 3.4–16.8 vs. 6.2, range 4–11.5 months) and mOS (8.4, range 6.7–11 vs. 4.1, range 2.5–5.6 months). On the other hand, a study using FLAG-IDA/FLAG/FLAG plus liposomal daunorubicin in seven relapsed AML patients after HSCT, reporting CR of 86% and mCRD and mOS of 14 months [113]. Besides, a recent large retrospective study comparing FLAG-IDA with FLAGO-IDA (adding GO) suggested equivalent results with both schemes in CR rate (50.4 vs. 60.5) and OS (8.4 months in both arms) [95].
-
Fludarabine + Ara-C + mitoxantrone regimens
The MITO-FLAG scheme was reported in three studies [96, 97, 112], in two of them comparing the administration in bolus and in CI of Ara-C [97, 112], with CR rates between 43 and 80% and mOS between 6.6 and 7.1 months. The significant improvement in CR rate of bolus infusion against CI observed in the first non-RCT [112] (80 vs. 43%), was not reproduced in a later RCT [97] (54 vs. 43%). The mOS of both arms in the two studies was similar (6.8 months in both arms [112] vs. 7.1 and 6.1 months [97]).
-
Fludarabine + Ara-C + daunorubicin regimens
This combination was employed in three cohorts [98, 99, 119], showing CR rates ranged from 47 to 53% and mOS from 5.8 to 9 months. The most recent report combined this scheme with G-CSF [99], without significant differences with the previous outcomes observed (CR 53% and OS 9 months).
-
Cladribine + Ara-C + mitoxantrone regimens
Four studies used the MITO-CLAG scheme (cladribine + Ara-C + mitoxantrone + G-CSF) [90, 100, 101, 121], showing CR rates of 39–58%, mCRD of 5.5 months (only reported in one study [121]) and mOS of 5.5–9 months. No clear differences were observed between CLAG and MITO-CLAG regimens in two comparative studies [90, 121].
-
Fludarabine + Ara-C + other agent regimens
Other combinations of fludarabine and Ara-C with a third component different from anthracyclines have been analyzed [85, 92, 116]. The scheme fludarabine, Ara-C, and topotecan obtained a CR rate of 35%, mCRD of 5.2 months, and mOS of 5.2 months [116]. Different combinations with GO obtained similar results in two studies [85, 92], with a CR rate of 27–29%, mCRD of 8.3 months, and mOS of 5–7.4 months. The addition of GO to FLAG [85] and FLAG-IDA [92] apparently did not improve the CR and OS in two non-RCT.
-
Clofarabine + Ara-C regimens
Nine studies reported the use of clofarabine plus Ara-C schemes, obtaining a wmCR rate of 44.2% (range 9–55%), wmCRD of 7.6 months (range 3.2–10.6), and wmOS of 6.2 months (range 3–9) [21, 87, 102, 103, 105, 115, 117, 122, 169]. A dose-finding prospective trial combined clofarabine, Ara-C, and idarubicin with CR 48% and mCRD 10.6 months, whereas the combination of clofarabine and idarubicin showed CR 13% and mCRD 4.4 months [105]. The combination of clofarabine and Ara-C was compared with IDAC in a RCT, showing a significant increase in CR with the addition of clofarabine (35 vs. 18%), but the same OS (6.6 vs. 6.3 months) [21]. A retrospective study performed in a cohort of R/R AML patients who declined or were ineligible for a clinical trial showed lower efficacy outcomes than clinical trials with clofarabine alone or in combination with Ara-C (CR 11 vs. 19%; OS 3 months in both arms) [103].
Other intensive combinations
Other intensive chemotherapy combinations have been evaluated in R/R AML (Table 5) [16, 18, 20, 22, 23, 36, 38, 39, 90, 104, 105, 124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153].
-
Monotherapies
Sixteen studies analyzed different monotherapies, in most of the cases of active components of effective combinations, obtaining modest outcomes, usually lower than standard intensive combinations [22, 23, 39, 104, 124,125,126,127,128,129,130,131,132, 148,149,150]. Monotherapies with anthracyclines obtained limited results, with CR rates of 13% with amsacrine [23], 16–26% with idarubicin [125], and 8–44% with mitoxantrone [23, 126, 127]. Five studies analyzed the efficacy of carboplatin monotherapy, showing wmCR of 15.7% (range 0–30%) and wmCRD of 3.6 months (range 3.5–6) [128, 129, 148,149,150]. Worse outcomes were reported with the monotherapy of cladribine, without achieving any CR in two different studies [104, 130].
Elacytarabine, an elaidic acid ester of Ara-C, was tested in two studies in R/R AML patients reporting CR rates from 23 to 44%, mCRD of 5.1 months and mOS from 3.5 to 4.7 months [131, 132]. The RCT by Roboz et al. did not show improvements in CR or survival in comparison to the investigator’s choice control arm (HiDAC, MEC, FLAG, FLAG-IDA, decitabine, azacitidine, hydroxyurea, or supportive care) [131].
-
Ara-C + other agents
Eight studies evaluated other Ara-C combinations [16, 18, 20, 36, 38, 90, 133, 151]. A RCT demonstrated that HiDAC plus native asparaginase was superior to HiDAC alone (CR rate 38 vs. 24%, and OS 7.9 vs. 3.6 months) in patients younger than 60 years [16]. The combination of Ara-C with etoposide showed CR rates from 38 to 56% [18, 133, 151]. In a RCT, HiDAC plus etoposide did not show significant improvements against HiDAC (CR 38 vs. 31%; OS 5.2 vs. 3.7 months). A later study reported higher CR rate of 56% with IDAC and etoposide [133].
Other combinations with Ara-C have been tested, such as laromustine showing higher CR than Ara-C monotherapy (35 vs. 19%), but no differences in mOS (4.2 vs. 5.8 months) [20]. Combinations of Ara-C plus GO were reported in two studies [36, 38], one of them was non-representative of R/R AML (only in CBF-AML) and was previously commented [38]. The other study compared Ara-C plus GO with Ara-C plus cyclophosphamide and topotecan, resulting both ineffective schemes (CR 12 vs. 4; OS 3.7 vs. 3.8 months) [36]. A recent publication reported the use of MEC followed by decitabine after 5 days break (priming) showing CR 31% and OS 4.9 months [90].
IDAC plus vosaroxin was evaluated in the largest RCT in R/R AML, demonstrating better CR rate than IDAC (CR 37 vs. 19%) [22]. The OS in the entire cohort showed a trend to higher OS in vosaroxin group (OS 7.5 vs. 6.1 months, p = 0.06), with a significant improvement among patients 60 years of age and older.
-
Anthracyclines + other agents
These combinations have been tested in 12 studies [105, 127, 134,135,136,137,138,139,140,141, 152, 153]. Six non-comparative studies analyzed the use of anthracyclines with etoposide, mitoxantrone in 4 [134, 135, 152, 153] and aclarubicin in 2 [136, 137]. The outcomes observed in these small and relatively young cohorts were similar for mitoxantrone and aclarubicin (CR 16–45 and 24–40%; mCRD 3.5–15 and 0.8–7.5 months; mOS 3–8 and 3.2 months). A later study in only five patients obtained a CR of 60% with the addition of GO to mitoxantrone and etoposide scheme [138].
Combinations of anthracyclines and purine analogs without Ara-C were poorly studied [105, 139]. No patients obtained CR with the schemes of cladribine plus daunorubicin or cladribine monotherapy in a small cohort [139]. The scheme clofarabine plus idarubicin was noteffective either (CR 13%; mCRD 4.4 months) [105]. On the other hand, combinations of anthracyclines with a pyrimidine analog gemcitabine showed a CR rate of 11% with mCRD of 3 months [140].
Hypomethylating agents, decitabine, and azacitidine, in combination with anthracyclines were tested in two trials [127, 141]. Mitoxantrone plus azacitidine showed lower CR rates than the monotherapy with mitoxantrone (CR 15 vs. 28%) in a mixed cohort of acute nonlymphocytic leukemia (ANLL) and chronic myeloid leukemia in myeloid blast phase (CML-BP) [127]. The combination of decitabine with amsacrine or idarubicin showed CR rates of 27 and 45%, respectively [141].
-
Carboplatin + other agents
The limited efficacy observed with carboplatin CI monotherapy was intended to be improved with the addition of other drugs in six different studies [142,143,144,145,146,147]. The combination with etoposide showed CR 40% [142], but in another study, no CR was observed in a cohort of seven patients [143]. The triple therapy with carboplatin CI, etoposide, and Ara-C was analyzed in two studies with contradictory results, showing CR rates from 12 [145] to 50% [144]. In vitro synergistic and additive effects between carboplatin and anthracyclines were tested in a RCT comparing the combination of carboplatin CI with idarubicin and mitoxantrone, obtaining similar results (CR 29 vs. 28%; OS 2 vs. 2.5 months) [146]. Finally, a quadruple therapy called MECA (mitoxantrone CI + etoposide + carboplatin CI + Ara-C) achieved CR rate of 32% and mOS of 8.5 months [147].
Non-intensive approaches
Different non-intensive salvage therapies have been employed, especially for unfit patients (Table 6) [40, 103, 154,155,156,157,158,159,160,161,162,163,164,165,166,167].
-
Ara-C non-intensive regimens
Low dose of Ara-C administered subcutaneously was tested in two different studies, in monotherapy [154] and combined with ATRA [155], in both cases with high CR rates (44 and 49%).
-
GO monotherapy
Monotherapies of GO using different dosages (1.5 to 9 mg/m2 administered 1 or 3 days) were tested in four non-RCTs in elderly patients [40, 156, 157, 164], showing a wmCR rate of 21.1% (range 26–33%), wmCRD of 6.1 months (range 5–11), and wmOS of 5.4 months (range 4–8.4). A large cohort treated with GO monotherapy did not obtain better OS at 6 weeks in comparison to a historical cohort treated with Ara-C CI and mitoxantrone (OS 89 vs. 95%), although GO showed significantly fewer total hospital days [40]. In a dose-finding trial in a small cohort of R/R AML the CR rate was 21%, with mCRD of 6 months and mOS of 2 months [164]. Similar results were observed in a large cohort treated with GO 9 mg/m2 obtaining CR rate of 26%, mCRD 5.2 months and mOS of 4.9 months [156]. A slight increase in CR rate was reported in a cohort of first relapsed AML treated with fractionated GO 3 mg/m2 × 3 days (CR of 33%), with mCRD 11 months and mOS 8.4 months [157].
-
Clofarabine monotherapy
Only one study reported the use of clofarabine in monotherapy in R/R elderly patients, showing similar poor results than clofarabine combination with Ara-C (CR 11 vs. 19%; OS 3 months in both arms) [103].
-
Hypomethylating agents
Five non-RCTs analyzed the role of azacitidine monotherapy in R/R AML patients [158,159,160, 165, 166], obtaining a wmCR rate of 16.9% (range 0–60%), wmCRD of 2.9 months (range 6–11.9), and wmOS of 7.3 months (range 2.9–14.1). Besides, two studies evaluated the use of decitabine monotherapy [160, 161]. The first published report in ten patients relapsed after HSCT showed 60% CR and mOS of 14.1 months) [165]. In a small cohort of 20 elderly patients, no CR was obtained and mOS was 2.9 months [166]. In two later large cohorts of elderly patients, the CR rates were 21 to 17%, with mCRD of 6–11.9 months and mOS of 8.4–9 months [158, 159]. These outcomes were reproduced in a large multicentric retrospective study showing a CR rate of 16% and mOS of 6.4 months in a cohort of 656 R/R AML patients treated with azacitidine or decitabine, without differences according to the agent [160]. Another study evaluated the employment of decitabine monotherapy and combined with GO with similar results (CR 16% in both arms; OS 7 months) [161].
A non-intensive combination of azacitidine, ATRA, and valproic acid was tested in a single study showing CR 15% and mOS 2.9 months [162]. Valproic acid demonstrated in vitro an additive or synergistic effect added to a DNA methyltransferase inhibitor such as azacytidine [170].
-
Decitabine + GO regimens
The schedule decitabine plus GO in R/R AML was evaluated in three different studies [161, 163, 167]. This scheme obtained positive results in a small cohort (CR 46%; OS 6 months), probably related relatively young age of patients and because more than a half of patients were relapsed after HSCT, subgroup with better prognosis [167]. In a phase II study, the combination of decitabine and fractionated GO showed lower OS than decitabine alone (3.6 vs. 7 months) and CR rate of 16% combining both arms [161]. These results were reproduced in another elderly cohort, with CR/CRi rate of 24% and mCRD 5.8 months [163].
Role of priming
The role of priming with G-CSF in AML chemotherapy continues being controversial yet, including de novo AML [168, 171]. In 40 studies included in this review, the priming with G-CSF was part of the schedule [33, 34, 41, 54, 57, 59, 60, 63, 64, 67, 70, 83, 84, 86,87,88,89,90,91,92,93,94,95,96,97, 99,100,101, 106,107,108,109,110,111,112,113,114, 118, 120, 121]. Five studies of the anthracycline plus cytarabine-based regimens added hematopoietic growth factors. One of them combined Ara-C, mitoxantrone, and granulocyte-macrophage-CSF (GM-CSF) without a significant improvement [41]. On the other hand, four studies reported the use of CAG regimen (low dose Ara-C, aclarubicin, G-CSF) with positive results, but no RCT demonstrated the superiority of this approach [33, 34, 54, 57]. Six studies comparing a schedule of Ara-C, anthracyclines and etoposide with and without G-CSF or GM-CSF did not show any improvement by use of priming [34, 59, 60, 63, 64, 70].
Most of the studies with purine analogue plus cytarabine-based regimens employed G-CSF priming in their schedules, although the benefit of this strategy has not been clearly demonstrated [41, 67, 70, 83, 84, 86,87,88,89,90,91,92,93,94,95,96,97, 99,100,101, 106,107,108,109,110,111,112,113,114, 118, 120, 121]. Two studies compared the efficacy of FLA and FLAG schemes, one RCT [70] and one retrospective comparison [86], and in both cases, no differences were observed in any CR, DFS, and OS. Between CLA and CLAG schemes were not a direct comparison, but the only published study with CLA [104] showed lower efficacy than the five studies with CLAG [67, 89, 90, 111, 121]. In combinations including anthracyclines, such FLAG-IDA, MITO-FLAG, or MITO-CLAG, the G-CSF is always part of the standard treatment, and comparative studies analyzing the benefit of priming were not published.
Discussion
To our knowledge, this is the first systematic review analyzing the outcomes after salvage regimens using conventional chemotherapy agents in R/R AML patients. Leopold et al., published in 2002 a systematic review on this topic, but the authors only included AML patients at first relapse [172]. In addition, other authors have critically reviewed the literature on the R/R AML setting without a systematic search [173,174,175]. Our study selection included 157 out of 850 records, with a wide variety of schedules, revealing that there is still no recognized standard treatment in R/R AML. Several regimens have achieved relatively high CR/CRi rates, but none of them obtained outstanding CR duration or increased survival rates. In general, the reviewed manuscripts were retrospective analyses performed in small cohorts, with only few studies with high methodological quality, such as RCTs. Besides, there is a lack of evidence in the real-life population, and we can even raise the question on whether to administer or not any salvage regimen for a subset of patients with demonstrated poor prognosis (i.e., del 17p or P53mut [176], or unfit/vulnerable subjects). Furthermore, the high variability in the study design and the inclusion criteria makes challenging to perform comparisons between studies. This systematic review was restricted to explore the outcomes using only conventional chemotherapy agents, which are still the backbone of salvage regimens out of an experimental context. Nevertheless, to have a better understanding of the R/R ground, we included studies in R/R AML adult population at any disease stage (i.e., primary refractory as well as first relapse or beyond). Regarding the great heterogeneity among type of analyzed R/R patients, we note that (1) there are few data on outcomes of patients at second or beyond R/R episode [25, 28, 33, 46, 59, 61, 68, 84, 87, 97, 107, 115, 122, 125, 135, 141, 145, 146, 169], and (2) there is no consensus when referring to primary refractory disease (i.e., after 1 or 2 cycles of induction? should a PR after cycle 1 be considered as resistance?). In this regard, the recently published ELN guidelines recommend considering a primary refractory disease only after two induction cycles, irrespectively of the schedule used in the second cycle [1]. Although this recommendation could be useful to standardize definitions for clinical trials, they are not reflecting what has been considered in the clinical practice in the past decades.
A rational decision algorythm to recommend conventional salvage therapies versus experimental approaches (i.e., clinical trial or sequential allo-HSCT) could be using several prognostic factors related to dismal outcome under standard approaches [2,3,4,5,6,7,8,9,10,11,12], or even better using some of the available scoring systems to predict OS (e.g., scores by GOELAMS, PETHEMA, and HOVON) [76, 95, 177]. The main adverse factors included in those scoring systems were older age, shorter CR1 duration, unfavorable cytogenetics, mutated FLT3-ITD, and previous HSCT. In addition, significant lower CR rates were reported in R/R AML patients older than 60 years [3,4,5,6,7, 16, 178], as well as in those with shorter CR1 duration [3, 7,8,9, 178] and unfavorable karyotype [7, 10,11,12]. We observed in almost all studies better CR rate in LR (wmCR 58.2%) than ER patients (wmCR 31.1%), and refractory patients (wmCR 34.5%) [8, 17, 18, 22, 25, 31, 33, 47, 48, 58, 61, 69, 76, 83, 84, 86, 87, 95,96,97, 163, 169], but again, the inconsistency of the definitions for refractoriness and LR vs. ER, as well as the diversity of chemotherapy regimens applied, precludes from any clear statement. Interestingly, the CR rate reported in first R/R (wmCR of 50.8% in relapsed and 34.5% in refractory patients) versus ≥2ndR episodes (wmCR 49.2%) showed high variability, obtaining worse [28, 59, 61, 87, 122, 125, 135, 146], similar [33, 84, 169] or even better [25, 46, 59, 68, 97, 107, 115, 141, 145] responses in ≥2ndR patients. On the other hand, the HOVON group found worse outcomes in patients relapsing after HSCT, probably due to a higher cumulative toxicity, more aggressive leukemia, and less alternative therapies [177]. In contrast, our review reveals a wmCR of 59.8% in patients relapsing after HSCT, whereas the wmCR rates of relapsed and refractory patients were 53 and 47.5%, respectively [58, 68, 84, 95, 106, 107, 109, 113, 165, 167]. By the way, Bergua et al. explained the better CR and OS in first R/R episodes experienced after an allo-HSCT by the host immunosuppressive effect of FLAG-IDA [146], which could induce graft-versus-host/leukemia disease and full-donor chimerism [113, 179].
Regarding the weighted mean of CR and ED rates after intensive salvage regimens, in our opinion, this review shows that the following regimens have the more acceptable results: AMSA plus Ara-C (54.3 and 6.8%) [7, 27, 42, 44, 48, 49, 53], MEC (52.5 and 8.3%) [58,59,60,61,62,63,64,65,66,67, 79,80,81,82], MIDAM (59.4 and 5.7%) [38, 75,76,77,78], FLAG (53.3 and 8.7%) [8, 70, 83,84,85,86, 88, 106,107,108,109,110, 123], CLAG (45.5 and 9.4%) [67, 89, 90, 111, 121], FLAG-IDA intermittent infusion (52.9 and 13.4%) [32, 88, 91, 92, 94, 95, 113,114,115, 118, 120], and clofarabine plus Ara-C (44.2 and 14.3%) [21, 87, 102, 103, 105, 115, 117, 122, 169], while others apparently may offer suboptimal rates related to lower efficacy or higher toxicity, e.g., HiDAC (28 and 29%) [8, 15, 16, 18, 19, 23], mitoxantrone plus Ara-C (50 and 25.2%) [4, 5, 19, 25,26,27,28,29, 39,40,41, 43, 46, 47, 50,51,52], iDAC (20.6 and 12.8%) [8, 17, 20,21,22], and hypomethylating agents (16.5%, ED not reported) [158,159,160,161, 165, 166]. However, despite better CR rates with some optimal regimens, the OS and mCRD obtained with these schemes remain disappointing like others (overall wmOS ranging from 6.2 to 8.7 months, and wmCRD from 4.8 to 9.8 months). The combinations with better long-term results were FLAG-IDA intermittent infusion (wmOS 8.4 months and wmCRD 16 months) [32, 88, 91, 92, 94, 95, 113,114,115, 118, 120] and MIDAM (wmOS 12.6 months) [38, 75,76,77,78]. The possible causes of these poor post-remission outcomes includes the poor quality of the response, the very high rate of relapse (especially when an allo-HSCT is not performed), and the high toxicity-related mortality (especially after a subsequent allo-HSCT).
There is few evidence to select a standard regimen in R/R AML, with only few RCTs published so far, some of them comparing the experimental arm with suboptimal controls (e.g., iDAC)(Supplemental Table 1). Furthermore, the ELN [1] and NCCN [180] clinical guidelines recommend some salvage schemes with scarce supporting literature (e.g., CLAG + mitoxantrone or idarubicin [90, 100, 101, 121], clofarabine ± Ara-C + G-CSF ± idarubicin [21, 87, 102, 103, 105, 115, 117, 122, 169]), or with suboptimal CR rates (e.g., HiDAC [8, 15, 16, 18, 19, 23] or iDAC [8, 17, 20,21,22]). We can raise criticism about these suggested regimens if we aim to achieve a CR to undergo an allo-HSCT. However, these schedules are acceptable if we aknowledge that other regimens achieving “optimal CR” rates did not improve mOS. Actually, a recent retrospective study [181] showed higher CR rate with intensive salvage regimens (Ara-C + anthracyclines, MIDAM or FLAG-IDA) than iDAC scheme (employed as control arm in recent RCTs [21, 22]) (53 vs. 19%), but similar OS (8 vs. 6.1 months). Given these data, we can raise the question about the most relevant study endpoints for R/R AML trials. Although the OS from the initiation of salvage therapy is commonly used, the EFS could be more appropriate to test the efficacy and safety of any regimen. In addition, at least in fit R/R AML patients, the rate of CR/CRi and the feasibility of a subsequent allo-HSCT should be considered as secondary endpoints. Regarding the use of priming with growth factors in R/R AML, it has been widely studied, with contradictory results [33, 34, 41, 54, 57, 59, 60, 63, 64, 67, 70, 83, 84, 86,87,88,89,90,91,92,93,94,95,96,97, 99,100,101, 106,107,108,109,110,111,112,113,114, 118, 120, 121].
There is a consensus to perform an allo-HSCT after the salvage regimen in order to improve the long-term outcomes, although the OS at 4 years does not exceed 20–30% in patients successfully bridged to transplant in CR [182, 183]. Besides, the AMLSG group analyzed the impact of allo-HSCT after first induction failure in 875 patients, showing significant differences in OS at 5 years between allo-HSCT in first CR (48%), direct allo-HSCT (36%) and allo-HSCT in refractory disease after salvage therapy (25%) [184]. Nevertheless, the allo-HSCT option will not be feasible in the majority of patients, by absence of suitable donor or due to limiting comorbidities, especially in old patients. The therapeutic options in elderly unfit patients are limited to non-intensive approaches aiming to control disease progression and minimize treatment-related mortality. In fact, this subset represents the majority of R/R AML patients, for whom the last update of NCCN guidelines [180] recommended hypomethylating agents or low-dose Ara-C, both with a low level of evidence.
Some limitations of this review should be addressed. First, the variability of the definitions of CR rate, R/R and the changes in the laboratory analyses could difficult the comparisons between studies with more than 30 years in the date of publication. Second, the differences in methodology and patient selection of the studies could influence in efficacy reported and it should be interpreted with caution. Third, heterogeneity of the disease between R/R patients, as well as between ER, LR or relapse after HSCT, can mask the real effect of a salvage therapy in a specific subset of patients when it was reported together. Fourth, the impact of prognosis factors (age, performance status, FLT3-ITD or dmCEBPA mutations, etc.) has not been measured in this review, in most of the cases for lack of information in the original articles. Finally, the methodological quality of the majority of the studies included is low, with only a few RCTs.
In conclusion, R/R AML in adult patients is a major challenge. Salvage therapies with conventional antileukemic agents have been employed for decades, none of them achieving outstanding CR rates, long-lasting remissions and acceptable OS. A better knowledge of the prognostic factors, more effective and less toxic combinations using conventional and new therapies, as well as improvements in allo-HSCT procedure and timing, could play a role to improve the clinical outcomes in the future. In our opinion, clinical trials should be the first treatment option in R/R AML, both in fit and unfit patients. In this regard, the PETHEMA group is planning a trial in R/R AML patients, which incorporates a Precision Medicine test to select the salvage regimen according to the ex vivo leukemic sensitivity to conventional chemotherapy agents [185].
References
Döhner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Büchner T, Dombret H, Ebert BL, Fenaux P, Larson RA, Levine RL, Lo-Coco F, Naoe T, Niederwieser D, Ossenkoppele GJ, Sanz M, Sierra J, Tallman MS, Tien HF, Wei AH, Löwenberg B, Bloomfield CD (2017) Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood 129(4):424–427
Walter RB, Othus M, Burnett AK, Lowenberg B, Kantarjian HM, Ossenkoppele GJ, Hills RK, Ravandi F, Pabst T, Evans A, Pierce SR, Vekemans MC, Appelbaum FR, Estey EH (2014) Resistance prediction in aml: analysis of 4601 patients from MRC/NCRI, HOVON/SAKK, SWOC and MD Anderson Cancer Center. Leukemia 29(2):312–320
Keating MJ, Kantarjian H, Smith TL, Estey E, Walters R, Andersson B, Beran M, McCredie KB, Freireich EJ (1989) Response to salvage therapy and survival after relapse in acute myelogenous leukemia. J Clin Oncol 7(8):1071–1080
Sternberg DW, Aird W, Neuberg D, Thompson L, MacNeill K, Amrein P, Shulman LN (2000) Treatment of patients with recurrent and primary refractory acute myelogenous leukemia using mitoxantrone and intermediate-dose cytarabine: a pharmacologically based regimen. Cancer 88(9):2037–2041
Kern W, Aul C, Maschmeyer G, Schönrock-Nabulsi R, Ludwig WD, Bartholomäus A, Bettelheim P, Wörmann B, Büchner T, Hiddemann W (1998) Superiority of high-dose over intermediate-dose cytosine arabinoside in the treatment of patients with high-risk acute myeloid leukemia: results of an age-adjusted prospective randomized comparison. Leukemia 12(7):1049–1055
Rees JK, Gray RG, Swirsky D, Hayhoe FG (1986) Principal results of the Medical Research Council’s 8th acute myeloid leukaemia trial. Lancet 2(8518):1236–1241
Tavernier E, Le QH, Elhamri M, Thomas X (2003) Salvage therapy in refractory acute myeloid leukemia: prediction of outcome based on analysis of prognostic factors. Leuk Res 27(3):205–214
Estey E, Plunkett W, Gandhi V, Rios MB, Kantarjian H, Keating MJ (1993) Fludarabine and arabinosylcytosine therapy of refractory and relapsed acute myelogenous leukemia. Leuk Lymphoma 9(4–5):343–350
Thalhammer F, Geissler K, Jager U, Kyrle PA, Pabinger I, Mitterbauer M, Gisslinger H, Knöbl P, Laczika K, Schneider B, Haas OA, Lechner K (1996) Duration of second complete remission in patients with acute myeloid leukemia treated with chemotherapy: a retrospective single-center study. Ann Hematol 72(4):216–222
Wheatley K, Burnett AK, Goldstone AH, Gray RG, Hann IM, Harrison CJ, Rees JK, Stevens RF, Walker H (1999) A simple, robust, validated and highly predictive index for the determination of risk-directed therapy in acute myeloid leukaemia derived from the MRC AML 10 trial. United Kingdom Medical Research Council’s Adult and Childhood Leukaemia Working Parties. Br J Haematol 107(1):69–79
Weltermann A, Fonatsch C, Haas OA, Greinix HT, Kahls P, Mitterbauer G, Jäger U, Kainz B, Geissler K, Valent P, Sperr WR, Knöbl P, Schwarzinger I, Gleiss A, Lechner K (2004) Impact of cytogenetics on the prognosis of adults with de novo AML in first relapse. Leukemia 18(2):293–302
Kern W, Haferlach T, Schnittger S, Ludwig WD, Hiddemann W, Schoch C (2002) Karyotype instability between diagnosis and relapse in 117 patients with acute myeloid leukemia: implications for resistance against therapy. Leukemia 16(10):2084–2091
Zittoun R, Jehn U, Fière D, Haanen C, Löwenberg B, Willemze R, Abels J, Bury J, Peetermans M, Hayat M et al (1989) Alternating v repeated postremission treatment in adult acute myelogenous leukemia: a randomized phase III study (AML6) of the EORTC Leukemia Cooperative Group. Blood 73(4):896–906
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700
Herzig RH, Lazarus HM, Wolff SN, Phillips GL, Herzig GP (1985) High-dose cytosine arabinoside therapy with and without anthracycline antibiotics for remission reinduction of acute nonlymphoblastic leukemia. J Clin Oncol 3(7):992–997
Capizzi RL, Davis R, Powell B, Cuttner J, Ellison RR, Cooper MR, Dillman R, Major WB, Dupre E, McIntyre OR (1988) Synergy between high-dose cytarabine and asparaginase in the treatment of adults with refractory and relapsed acute myelogenous leukemia—a Cancer and Leukemia Group B Study. J Clin Oncol 6(3):499–508
Estey EH, Plunkett W, Kantarjian H, Rios MB, Keating MJ (1993) Treatment of relapsed or refractory AML with intermediate-dose arabinosylcytosine (ara-C): confirmation of the importance of ara-C triphosphate formation in mediating response to ara-C. Leuk Lymphoma 10(Suppl):115–121
Vogler WR, McCarley DL, Stagg M, Bartolucci AA, Moore J, Martelo O, Omura GA (1994) A phase III trial of high-dose cytosine arabinoside with or without etoposide in relapsed and refractory acute myelogenous leukemia. A Southeastern Cancer Study Group trial. Leukemia 8(11):1847–1853
Karanes C, Kopecky KJ, Head DR, Grever MR, Hynes HE, Kraut EH, Vial RH, Lichtin A, Nand S, Samlowski WE, Appelbaum FR (1999) A phase III comparison of high dose ARA-C (HIDAC) versus HIDAC plus mitoxantrone in the treatment of first relapsed or refractory acute myeloid leukemia Southwest Oncology Group Study. Leuk Res 23(9):787–794
Giles F, Vey N, DeAngelo D, Seiter K, Stock W, Stuart R, Boskovic D, Pigneux A, Tallman M, Brandwein J, Kell J, Robak T, Staib P, Thomas X, Cahill A, Albitar M, O'Brien S (2009) Phase 3 randomized, placebo-controlled, double-blind study of high-dose continuous infusion cytarabine alone or with laromustine (VNP40101M) in patients with acute myeloid leukemia in first relapse. Blood 114(19):4027–4033
Faderl S, Wetzler M, Rizzieri D, Schiller G, Jagasia M, Stuart R, Ganguly S, Avigan D, Craig M, Collins R, Maris M, Kovacsovics T, Goldberg S, Seiter K, Hari P, Greiner J, Vey N, Recher C, Ravandi F, Wang ES, Vasconcelles M, Huebner D, Kantarjian HM (2012) Clofarabine plus cytarabine compared with cytarabine alone in older patients with relapsed or refractory acute myelogenous leukemia: results from the CLASSIC I Trial. J Clin Oncol 30(20):2492–2499
Ravandi F, Ritchie EK, Sayar H, Lancet JE, Craig MD, Vey N, Strickland SA, Schiller GJ, Jabbour E, Erba HP, Pigneux A, Horst HA, Recher C, Klimek VM, Cortes J, Roboz GJ, Odenike O, Thomas X, Havelange V, Maertens J, Derigs HG, Heuser M, Damon L, Powell BL, Gaidano G, Carella AM, Wei A, Hogge D, Craig AR, Fox JA, Ward R, Smith JA, Acton G, Mehta C, Stuart RK, Kantarjian HM (2015) Vosaroxin plus cytarabine versus placebo plus cytarabine in patients with first relapsed or refractory acute myeloid leukaemia (VALOR): a randomised, controlled, double-blind, multinational, phase 3 study. Lancet Oncol 16(9):1025–1036
Vogler WR, Preisler HD, Winton EF, Gottlieb AJ, Goldberg J, Brennan J, Grunwald H, Rai K, Browman G, Miller KB et al (1986) Randomized trial of high-dose cytarabine versus amsacrine in acute myelogenous leukemia in relapse: a Leukemia Intergroup Study. Cancer Treat Rep 70(4):455–459
Spriggs DR, Robbins G, Arthur K, Mayer RJ, Kufe D (1988) Prolonged high dose ARA-C infusions in acute leukemia. Leukemia 2(5):304–306
Hiddemann W, Kreutzmann H, Straif K, Ludwig WD, Mertelsmann R, Donhuijsen-Ant R, Lengfelder E, Arlin Z, Büchner T (1987) High-dose cytosine arabinoside and mitoxantrone: a highly effective regimen in refractory acute myeloid leukemia. Blood 69(3):744–749
Walters RS, Kantarjian H, Keating MJ, Plunkett WK, Estey EH, Andersson B, Beran M, McCredie KB, Freireich EJ (1988) Mitoxantrone and high-dose cytosine arabinoside in refractory acute myelogenous leukemia. Cancer 62(4):677–682
Martiat P, Ghilain JM, Ferrant A, Doyen C, Delannoy A, Chatelain C, Bosly A, Michaux JL, Sokal G (1990) High-dose cytosine arabinoside and amsacrine or mitoxantrone in relapsed and refractory acute myeloid leukaemia: a prospective randomized study. Eur J Haematol 45(3):164–167
Paciucci PA, Cuttner J, Holland JF (1990) Sequential intermediate-dose cytosine arabinoside and mitoxantrone for patients with relapsed and refractory acute myelocytic leukemia. Am J Hematol 35(1):22–25
Hiddemann W, Aul C, Maschmeyer G, Schönrock-Nabulsi R, Ludwig WD, Bartholomäus A, Bettelheim P, Becker K, Balleisen L, Lathan B et al (1993) High-dose versus intermediate dose cytosine arabinoside combined with mitoxantrone for the treatment of relapsed and refractory acute myeloid leukemia: results of an age adjusted randomized comparison. Leuk Lymphoma 10(Suppl):133–137
List AF, Kopecky KJ, Willman CL, Head DR, Persons DL, Slovak ML, Dorr R, Karanes C, Hynes HE, Doroshow JH, Shurafa M, Appelbaum FR (2001) Benefit of cyclosporine modulation of drug resistance in patients with poor-risk acute myeloid leukemia: a Southwest Oncology Group study. Blood 98(12):3212–3220
De La Serna J, Francisco Tomás J, Solano C, García de Paredes ML, Campbell J, Grande C, Diaz-Mediavilla J (1997) Idarubicin and intermediate dose ARA-C followed by consolidation chemotherapy or bone marrow transplantation in relapsed or refractory acute myeloid leukemia. Leuk Lymphoma 25(3–4):365–372
Fiegl M, Unterhalt M, Kern W, Braess J, Spiekermann K, Staib P, Grüneisen A, Wörmann B, Schöndube D, Serve H, Reichle A, Hentrich M, Schiel X, Sauerland C, Heinecke A, Rieger C, Beelen D, Berdel WE, Büchner T, Hiddemann W, German AML Cooperative Group (AMLCG) (2014) Chemomodulation of sequential high-dose cytarabine by fludarabine in relapsed or refractory acute myeloid leukemia: a randomized trial of the AMLCG. Leukemia 28(5):1001–1007
Saito K, Nakamura Y, Aoyagi M, Waga K, Yamamoto K, Aoyagi A, Inoue F, Nakamura Y, Arai Y, Tadokoro J, Handa T, Tsurumi S, Arai H, Kawagoe Y, Gunnji H, Kitsukawa Y, Takahashi W, Furusawa S (2000) Low-dose cytarabine and aclarubicin in combination with granulocyte colony-stimulating factor (CAG regimen) for previously treated patients with relapsed or primary resistant acute myelogenous leukemia (AML) and previously untreated elderly patients with AML, secondary AML, and refractory anemia with excess blasts in transformation. Int J Hematol 71(3):238–244
Zhang X, Li Y, Zhang Y, Chen X, Zhang C, Gao L, Kong P, Liu Y, Wen Q, Zeng Y, Wang Q, Su Y, Wang C, Wang S, Yuan Z, Gao L (2013) Etoposide in combination with low-dose CAG (cytarabine, aclarubicin, G-CSF) for the treatment of relapsed or refractory acute myeloid leukemia: a multicenter, randomized control trial in southwest China. Leuk Res 37(6):657–664
Cortes J, Estey E, O'Brien S, Giles F, Shen Y, Koller C, Beran M, Thomas D, Keating M, Kantarjian H (2001) High-dose liposomal daunorubicin and high-dose cytarabine combination in patients with refractory or relapsed acute myelogenous leukemia. Cancer 92(1):7–14
Litzow MR, Othus M, Cripe LD, Gore SD, Lazarus HM, Lee SJ, Bennett JM, Paietta EM, Dewald GW, Rowe JM, Tallman MS, Eastern Cooperative Oncology Group Leukemia Committee (2010) Failure of three novel regimens to improve outcome for patients with relapsed or refractory acute myeloid leukaemia: a report from the Eastern Cooperative Oncology Group. Br J Haematol 148(2):217–225
Cortes JE, Goldberg SL, Feldman EJ, Rizzeri DA, Hogge DE, Larson M, Pigneux A, Recher C, Schiller G, Warzocha K, Kantarjian H, Louie AC, Kolitz JE (2015) Phase II, multicenter, randomized trial of CPX-351 (cytarabine:daunorubicin) liposome injection versus intensive salvage therapy in adults with first relapse AML. Cancer 121(2):234–242
Hospital MA, Prebet T, Bertoli S, Thomas X, Tavernier E, Braun T, Pautas C, Perrot A, Lioure B, Rousselot P, Tamburini J, Cluzeau T, Konopacki J, Randriamalala E, Berthon C, Gourin MP, Recher C, Cahn JY, Ifrah N, Dombret H, Boissel N (2014) Core-binding factor acute myeloid leukemia in first relapse: a retrospective study from the French AML intergroup. Blood 124(8):1312–1319
Paciucci PA, Cuttner J, Holland JF (1984) Mitoxantrone as a single agent and in combination chemotherapy in patients with refractory acute leukemia. Semin Oncol 11(3 Suppl 1):36–40
Lang K, Menzin J, Earle CC, Mallick R (2002) Outcomes in patients treated with gemtuzumab ozogamicin for relapsed acute myelogenous leukemia. Am J Health Syst Pharm 59(10):941–948
Büchner T, Hiddemann W, Koenigsmann M, Zuehlsdorf M, Woermann B, Boeckmann A, Aguion Freire E, Innig G, Maschmeyer G, Ludwig WD et al (1990) Recombinant human GM-CSF following chemotherapy in high-risk AML. Bone Marrow Transplant 6(Suppl 1):131–134
Peters WG, Willemze R, Colly LP (1986) Results of induction and consolidation treatment with intermediate and high-dose ara-C and m-AMSA containing regimens in patients with primarily failed or relapsed acute leukemia and non-Hodgkin's lymphoma. Scand J Haematol Suppl 44:7–16
Brito-Babapulle F, Catovsky D, Newland AC, Goldman JM, Galton DA (1987) Treatment of acute myeloid leukemia with intermediate-dose cytosine arabinoside and mitoxantrone. Semin Oncol 14(2 Suppl 1):51–52
Peters WG, Willemze R, Colly LP (1988) Results of induction and consolidation treatment with intermediate and high-dose cytosine arabinoside and m-Amsa of patients with poor-risk acute myelogenous leukaemia. Eur J Haematol 40(3):198–204
Harousseau JL, Reiffers J, Hurteloup P, Milpied N, Guy H, Rigal-Huguet F, Facon T, Dufour P, Ifrah N (1989) Treatment of relapsed acute myeloid leukemia with idarubicin and intermediate-dose cytarabine. J Clin Oncol 7(1):45–49
Amadori S, Meloni G, Petti MC, Papa G, Miniero R, Mandelli F (1989) Phase II trial of intermediate dose ARA-C (IDAC) with sequential mitoxantrone (MITOX) in acute myelogenous leukemia. Leukemia 3(2):112–114
Harousseau JL, Milpied N, Briere J, Desablens B, Ghandour C (1990) Mitoxantrone and intermediate-dose cytarabine in relapsed or refractory acute myeloblastic leukemia. Nouv Rev Fr Hematol 32:227–230
Dekker AW, Nieuwenhuis HK, Verdonck LF (1990) Intermediate-dose 1055 cytosine arabinoside and amsacrine. An effective regimen with low toxicity in refractory acute nonlymphocytic leukemia. Cancer 65(9):1891–1894
Jehn U, Heinemann V (1990) Intermediate-dose Ara-C/m-AMSA for remission induction and high-dose Ara-C/m-AMSA for intensive consolidation in relapsed and refractory adult acute myelogeneous leukemia. Haematol Blood Transfus 33:333–338
Sierra J, Grañena A, Bosch F, Carreras E, Martí JM, Urbano-Ispizua A, Rovira M, Rozman C (1992) Mitoxantrone and intermediate-dose cytosine arabinoside for poor-risk acute leukemias: response to treatment and factors influencing outcome. Hematol Oncol 10(6):301–309
Reece DE, Elmongy MB, Barnett MJ, Klingemann HG, Shepherd JD, Phillips GL (1993) Chemotherapy with high-dose cytosine arabinoside and mitoxantrone for poor-prognosis myeloid leukemias. Cancer Investig 11(5):509–516
MacCallum PK, Davis CL, Rohatiner AZ, Lim J, Gupta RK, Whelan JS, Price CG, Evans ML, Amess JA, Leahy M et al (1993) Mitoxantrone and cytosine arabinoside as treatment for acute myelogenous leukemia (AML) at first recurrence. Leukemia 7(10):1496–1499
Jehn U, Heinemann V (1993) Phase-II study of treatment of refractory acute leukemia with intermediate-dose cytosine arabinoside and amsacrine. Ann Hematol 66(3):131–134
Yamada K, Furusawa S, Saito K, Waga K, Koike T, Arimura H, Aoyagi A, Yamato H, Sakuma H, Tsunogake S et al (1995) Concurrent use of granulocyte colony-stimulating factor with low-dose cytosine arabinoside and aclarubicin for previously treated acute myelogenous leukemia: a pilot study. Leukemia 9(1):10–14
De Witte T, Suciu S, Selleslag D, Labar B, Roozendaal K, Zittoun R, Ribeiro M, Kurstjens R, Hayat M, Dardenne M, Solbu G, Muus P (1996) Salvage treatment for primary resistant acute myelogenous leukemia consisting of intermediate-dose cytosine arabinoside and interspaced continuous infusions of idarubicin: a phase-II study (no. 06901) of the EORTC Leukemia Cooperative Group. Ann Hematol 72(3):119–124
Russo D, Piccaluga PP, Michieli M, Michelutti T, Visani G, Gugliotta L, Bonini A, Pierri I, Gobbi M, Tiribelli M, Fanin R, Piccolrovazzi S, Baccarani M (2002) Liposomal daunorubicin (DaunoXome) for treatment of poor-risk acute leukemia. Ann Hematol 81(8):462–466
Wang Y, Li W, Chen S, Qiu H, Sun A, Wu D (2011) Salvage chemotherapy with low-dose cytarabine and aclarubicin in combination with granulocyte colony-stimulating factor priming in patients with refractory or relapsed acute myeloid leukemia with translocation (8;21). Leuk Res 35(5):604–607
Spadea A, Petti MC, Fazi P, Vegna ML, Arcese W, Avvisati G, Aloe Spiriti MA, Latagliata R, Meloni G, Testi AM et al (1993) Mitoxantrone, etoposide and intermediate-dose Ara-C (MEC): an effective regimen for poor risk acute myeloid leukemia. Leukemia 7(4):549–552
Archimbaud E, Fenaux P, Reiffers J, Cordonnier C, Leblond V, Travade P, Troussard X, Tilly H, Auzanneau G, Marie JP et al (1993) Granulocyte-macrophage colony-stimulating factor in association to timed-sequential chemotherapy with mitoxantrone, etoposide, and cytarabine for refractory acute myelogenous leukemia. Leukemia 7(3):372–377
Ohno R, Naoe T, Kanamaru A, Yoshida M, Hiraoka A, Kobayashi T, Ueda T, Minami S, Morishima Y, Saito Y et al (1994) A double-blind controlled study of granulocyte colony-stimulating factor started two days before induction chemotherapy in refractory acute myeloid leukemia. Kohseisho Leukemia Study Group. Blood 83(8):2086–2092
Archimbaud E, Thomas X, Leblond V, Michallet M, Fenaux P, Cordonnier C, Dreyfus F, Troussard X, Jaubert J, Travade P et al (1995) Timed sequential chemotherapy for previously treated patients with acute myeloid leukemia: long-term follow-up of the etoposide, mitoxantrone, and cytarabine-86 trial. J Clin Oncol 13(1):11–18
Vignetti M, Orsini E, Petti MC, Moleti ML, Andrizzi C, Pinto RM, Amadori S, Meloni G (1996) Probability of long-term disease-free survival for acute myeloid leukemia patients after first relapse: a single-centre experience. Ann Oncol 7(9):933–938
Thomas X, Fenaux P, Dombret H, Delair S, Dreyfus F, Tilly H, Vekhoff A, Cony-Makhoul P, Leblond V, Troussard X, Cordonnier C, de Revel T, Simon M, Nicolini F, Stoppa AM, Janvier M, Bordessoule D, Rousselot P, Ffrench M, Marie JP, Archimbaud E (1999) Granulocyte-macrophage colony-stimulating factor (GM-CSF) to increase efficacy of intensive sequential chemotherapy with etoposide, mitoxantrone and cytarabine (EMA) in previously treated acute myeloid leukemia: a multicenter randomized placebo-controlled trial (EMA91 Trial). Leukemia 13(8):1214–1220
Revesz D, Chelghoum Y, Le QH, Elhamri M, Michallet M, Thomas X (2003) Salvage by timed sequential chemotherapy in primary resistant acute myeloid leukemia: analysis of prognostic factors. Ann Hematol 82(11):684–690
Lee SS, Lee JH, Lee JH, Kim DY, Kim SH, Lim SN, Lee YS, Seol M, Ryu SG, Kang YA, Jang S, Park CJ, Chi HS, Yun SC, Lee KH (2009) Single-dose mitoxantrone in combination with continuous infusion intermediate-dose cytarabine plus etoposide for treatment of refractory or early relapsed acute myeloid leukemia. Leuk Res 33(4):511–517
Lee JH, Choi SJ, Lee JH, Lee YS, Seol M, Ryu SG, Jang S, Park CJ, Chi HS, Lee JS, Kim WK, Lee KH (2006) Continuous infusion intermediate-dose cytarabine, mitoxantrone, plus etoposide for refractory or early relapsed acute myelogenous leukemia. Leuk Res 30(2):204–210
Price SL, Lancet JE, George TJ, Wetzstein GA, List AF, Ho VQ, Fernandez HF, Pinilla-Ibarz J, Kharfan-Dabaja MA, Komrokji RS (2011) Salvage chemotherapy regimens for acute myeloid leukemia: is one better? Efficacy comparison between CLAG and MEC regimens. Leuk Res 35(3):301–304
Carella AM, Carlier P, Pungolino E, Resegotti L, Liso V, Stasi R, Montillo M, Iacopino P, Mirto S, Pagano L et al (1993) Idarubicin in combination with intermediate-dose cytarabine and VP-16 in the treatment of refractory or rapidly relapsed patients with acute myeloid leukemia. The GIMEMA Cooperative Group. Leukemia 7(2):196–199
Liu Yin JA, Wheatley K, Rees JK, Burnett AK, UK MRC Adult Leukemia Working Party (2001) Comparison of ‘sequential’ versus ‘standard’ chemotherapy as re-induction treatment, with or without cyclosporine, in refractory/relapsed acute myeloid leukaemia (AML): results of the UK Medical Research Council AML-R trial. Br J Haematol 113(3):713–726
Milligan DW, Wheatley K, Littlewood T, Craig JI, Burnett AK, NCRI Haematological Oncology Clinical Studies Group (2006) Fludarabine and cytosine are less effective than standard ADE chemotherapy in high-risk acute myeloid leukemia, and addition of G-CSF and ATRA are not beneficial: results of the MRC AML-HR randomized trial. Blood 107(12):4614–4622
Sung WJ, Kim DH, Sohn SK, Kim JG, Baek JH, Jeon SB, Moon JH, Ahn BM, Lee KB (2005) Phase II trial of amsacrine plus intermediate-dose Ara-C (IDAC) with or without etoposide as salvage therapy for refractory or relapsed acute leukemia. Jpn J Clin Oncol 35(10):612–616
Song LX, Xu L, Li X, Chang CK, Zhang Y, Wu LY, He Q, Zhang QX, Li X (2012) Clinical outcome of treatment with a combined regimen of decitabine and aclacinomycin/cytarabine for patients with refractory acute myeloid leukemia. Ann Hematol 91(12):1879–1886
van Prooijen HC, Dekker AW, Punt K (1984) The use of intermediate dose cytosine arabinoside (ID Ara-C) in the treatment of acute non-lymphocytic leukaemia in relapse. Br J Haematol 57(2):291–299
Franchi A, Papa G, D'Atri S, Piccioni D, Masi M, Bonmassar E (1992) Cytotoxic effects of dacarbazine in patients with acute myelogenous leukemia: a pilot study. Haematologica 77(2):146–150
Chevallier P, Delaunay J, Turlure P, Pigneux A, Hunault M, Garand R, Guillaume T, Avet-Loiseau H, Dmytruk N, Girault S, Milpied N, Ifrah N, Mohty M, Harousseau JL (2008) Long-term disease-free survival after gemtuzumab, intermediate-dose cytarabine, and mitoxantrone in patients with CD33(+) primary resistant or relapsed acute myeloid leukemia. J Clin Oncol 26(32):5192–5197
Chevallier P, Labopin M, Turlure P, Prebet T, Pigneux A, Hunault M, Filanovsky K, Cornillet-Lefebvre P, Luquet I, Lode L, Richebourg S, Blanchet O, Gachard N, Vey N, Ifrah N, Milpied N, Harousseau JL, Bene MC, Mohty M, Delaunay J (2011) A new leukemia prognostic scoring system for refractory/relapsed adult acute myelogeneous leukaemia patients: a GOELAMS study. Leukemia 25(6):939–944
Peterlin P, Guillaume T, Delaunay J, Mohty M, Garnier A, Mahe B, Dubruille V, Blin N, Voldoire M, Touzeau C, Chauvin C, Gastinne T, Béné MC, Le Gouill S, Moreau P, Chevallier P (2016) Similarity of fractionated versus single dose(s) of gemtuzumab ozogamicin as part of the MIDAM salvage regimen in relapsed/refractory acute myeloid leukemia patients. Semin Hematol 53(3):216–217
Hütter-Krönke ML, Benner A, Döhner K, Krauter J, Weber D, Moessner M, Köhne CH, Horst HA, Schmidt-Wolf IG, Rummel M, Götze K, Koller E, Petzer AL, Salwender H, Fiedler W, Kirchen H, Haase D, Kremers S, Theobald M, Matzdorff AC, Ganser A, Döhner H, Schlenk RF (2016) Salvage therapy with high-dose cytarabine and mitoxantrone in combination with all-trans retinoic acid and gemtuzumab ozogamicin in acute myeloid leukemia refractory to first induction therapy. Haematologica 101(7):839–845
Link H, Freund M, Diedrich H, Wilke H, Austein J, Henke M, Wandt H, Fackler-Schwalbe E, Schlimok G, Hoffmann R et al (1990) Mitoxantrone, cytosine arabinoside, and VP-16 in 36 patients with relapsed and refractory acute myeloid leukemia. Haematol Blood Transfus 33:322–325
Amadori S, Arcese W, Isacchi G, Meloni G, Petti MC, Monarca B, Testi AM, Mandelli F (1991) Mitoxantrone, etoposide, and intermediate-dose cytarabine: an effective and tolerable regimen for the treatment of refractory acute myeloid leukemia. J Clin Oncol 9(7):1210–1214
Tribalto M, Cantonetti M, Catalano G, Del Poeta G, Masi M, Pastore S, Pisani F, Stasi R, Papa G (1991) Mitoxantrone in combination with etoposide and cytarabine for treatment of poor prognosis acute non lymphoid leukemia patients. Haematologica 76(5):402–405
Thomas X, Cambier N, Taksin AL, Reman O, Vekhoff A, Pautas C, Leblond V, Soler-Michel P, Ecstein-Fraïssé E, Archimbaud E (2000) Dose-escalation study of single dose mitoxantrone in combination with timed sequential chemotherapy in patients with refractory or relapsing acute myelogenous leukemia. Leuk Res 24(11):957–963
Jackson G, Taylor P, Smith GM, Marcus R, Smith A, Chu P, Littlewood TJ, Duncombe A, Hutchinson M, Mehta AB, Johnson SA, Carey P, MacKie MJ, Ganly PS, Turner GE, Deane M, Schey S, Brookes J, Tollerfield SM, Wilson MP (2001) A multicentre, open, non-comparative phase II study of a combination of fludarabine phosphate, cytarabine and granulocyte colony-stimulating factor in relapsed and refractory acute myeloid leukaemia and de novo refractory anaemia with excess of blasts in transformation. Br J Haematol 112(1):127–137
Lee SR, Yang DH, Ahn JS, Kim YK, Lee JJ, Choi YJ, Shin HJ, Chung JS, Cho YY, Chae YS, Kim JG, Sohn SK, Kim HJ (2009) The clinical outcome of FLAG chemotherapy without idarubicin in patients with relapsed or refractory acute myeloid leukemia. J Korean Med Sci 24(3):498–503
Jabbour E, Garcia-Manero G, Cortes J, Ravandi F, Plunkett W, Gandhi V, Faderl S, O'Brien S, Borthakur G, Kadia T, Burger J, Konopleva M, Brandt M, Huang X, Kantarjian H (2012) Twice-daily fludarabine and cytarabine combination with or without gentuzumab ozogamicin is effective in patients with relapsed/refractory acute myeloid leukemia, high-risk myelodysplastic syndrome, and blast-phase chronic myeloid leukemia. Clin Lymphoma Myeloma Leuk 12(4):244–251
Becker PS, Kantarjian HM, Appelbaum FR, Storer B, Pierce S, Shan J, Faderl S, Estey EH (2013) Retrospective comparison of clofarabine versus fludarabine in combination with high-dose cytarabine with or without granulocyte colony-stimulating factor as salvage therapies for acute myeloid leukemia. Haematologica 98(1):114–118
Becker PS, Kantarjian HM, Appelbaum FR, Petersdorf SH, Storer B, Pierce S, Shan J, Hendrie PC, Pagel JM, Shustov AR, Stirewalt DL, Faderl S, Harrington E, Estey EH (2011) Clofarabine with high dose cytarabine and granulocyte colony-stimulating factor (G-CSF) priming for relapsed and refractory acute myeloid leukaemia. Br J Haematol 155(2):182–189
Kim H, Lee JH, Joo YD, Bae SH, Lee JH, Kim DY, Lee WS, Ryoo HM, Jo JC, Choi Y, Lee KH, CoOperative Study Group A for Hematology (COSAH) (2016) A prospective, multicenter phase II study of continuous infusion of FLAG for patients older than 60 yr with resistant acute myeloid leukemia: a comparison with intensive younger patients' trial. Eur J Haematol 96(2):188–197
Wrzesień-Kuś A, Robak T, Lech-Marańda E, Wierzbowska A, Dmoszyńska A, Kowal M, Hołowiecki J, Kyrcz-Krzemień S, Grosicki S, Maj S, Hellmann A, Skotnicki A, Jedrzejczak W, Kuliczkowski K, Polish Adult Leukemia Group (2003) A multicenter, open, non-comparative, phase II study of the combination of cladribine (2-chlorodeoxyadenosine), cytarabine, and G-CSF as induction therapy in refractory acute myeloid leukemia—a report of the Polish Adult Leukemia Group (PALG). Eur J Haematol 71(3):155–162
Halpern AB, Othus M, Huebner EM, Buckley SA, Pogosova-Agadjanyan EL, Orlowski KF, Scott BL, Becker PS, Hendrie PC, Chen TL, Percival MM, Estey EH, Stirewalt DL, Walter RB (2017) Mitoxantrone, etoposide and cytarabine following epigenetic priming with decitabine in adults with relapsed/refractory acute myeloid leukemia or other high-grade myeloid neoplasms: a phase 1/2 study. Leukemia 31(12):2560–2567
Pastore D, Specchia G, Carluccio P, Liso A, Mestice A, Rizzi R, Greco G, Buquicchio C, Liso V (2003) FLAG-IDA in the treatment of refractory/relapsed acute myeloid leukemia: single-center experience. Ann Hematol 82(4):231–235
Martin MG, Augustin KM, Uy GL, Welch JS, Hladnik L, Goyal S, Tiwari D, Monahan RS, Reichley RM, Cashen AF, Stockerl-Goldstein K, Westervelt P, Abboud CN, Dipersio JF, Vij R (2009) Salvage therapy for acute myeloid leukemia with fludarabine, cytarabine, and idarubicin with or without gemtuzumab ozogamicin and with concurrent or sequential G-CSF. Am J Hematol 84(11):733–737
Montillo M, Ricci F, Tedeschi A, Cafro AM, Nosari AM, Nichelatti M, Marbello L, Morra E (2009) Twice daily fludarabine/Ara-C associated to idarubicin, G-CSF and ATRA is an effective salvage regimen in non-promyelocytic acute myeloid leukemia. Leuk Res 33(8):1072–1078
Kim H, Lee JH, Joo YD, Bae SH, Lee JH, Kim DY, Lee WS, Ryoo HM, Jo JC, Park JH, Lee KH (2014) Prospective, multicenter, phase II study on reducing the dosage of idarubicin and FLAG for patients younger than 65 years with resistant acute myeloid leukemia: a comparison with a higher dosage trial. Acta Haematol1 32(1):87–96
Bergua JM, Montesinos P, Martinez-Cuadrón D, Fernández-Abellán P, Serrano J, Sayas MJ, Prieto-Fernandez J, García R, García-Huerta AJ, Barrios M, Benavente C, Pérez-Encinas M, Simiele A, Rodríguez-Macias G, Herrera-Puente P, Rodríguez-Veiga R, Martínez-Sánchez MP, Amador-Barciela ML, Riaza-Grau R, Sanz MA, PETHEMA group (2016) A prognostic model for survival after salvage treatment with FLAG-Ida +/− gemtuzumab-ozogamicine in adult patients with refractory/relapsed acute myeloid leukaemia. Br J Haematol 174(5):700–710
Luo S, Cai F, Jiang L, Zhang S, Shen Z, Sun L, Gao S (2013) Clinical study of Mito-FLAG regimen in treatment of relapsed acute myeloid leukemia. Exp Ther Med 5(3):982–986
Thiel A, Schetelig J, Pönisch W, Schäfer-Eckart K, Aulitzky W, Peter N, Schulze A, Maschmeyer G, Neugebauer S, Herbst R, Hänel A, Morgner A, Kroschinsky F, Bornhäuser M, Lange T, Wilhelm M, Niederwieser D, Ehninger G, Fiedler F, Hänel M, East German Study Group Hematology/Oncology (OSHO); Study Alliance Leukemia (SAL) (2015) Mito-FLAG with Ara-C as bolus versus continuous infusion in recurrent or refractory AML—long-term results of a prospective randomized intergroup study of the East German Study Group Hematology/Oncology (OSHO) and the Study Alliance Leukemia (SAL). Ann Oncol 26(7):1434–1440
Camera A, Rinaldi CR, Palmieri S, Cantore N, Mele G, Mettivier V, Miraglia E, Mastrullo L, Grimaldi F, Luciano L, Guerriero A, Rotoli B, Ferrara F (2009) Sequential continuous infusion of fludarabine and cytarabine associated with liposomal daunorubicin (DaunoXome) (FLAD) in primary refractory or relapsed adult acute myeloid leukemia patients. Ann Hematol 88(2):151–158
De Astis E, Clavio M, Raiola AM, Ghiso A, Guolo F, Minetto P, Galaverna F, Miglino M, Di Grazia C, Ballerini F, Marani C, Pastori G, Mitscheunig L, Cruciani F, Lovera D, Varaldo R, Ghiggi C, Lemoli RM, Bacigalupo A, Gobbi M (2014) Liposomal daunorubicin, fludarabine, and cytarabine (FLAD) as bridge therapy to stem cell transplant in relapsed and refractory acute leukemia. Ann Hematol 93(12):2011–2018
Wrzesień-Kuś A, Robak T, Wierzbowska A, Lech-Marańda E, Pluta A, Wawrzyniak E, Krawczyńska A, Kuliczkowski K, Mazur G, Kiebiński M, Dmoszyńska A, Wach M, Hellmann A, Baran W, Hołowiecki J, Kyrcz-Krzemień S, Grosicki S, Polish Adult Leukemia Group (2005) A multicenter, open, noncomparative, phase II study of the combination of cladribine (2-chlorodeoxyadenosine), cytarabine, granulocyte colony-stimulating factor and mitoxantrone as induction therapy in refractory acute myeloid leukemia: a report of the Polish Adult Leukemia Group. Ann Hematol 84(9):557–564
Wierzbowska A, Robak T, Pluta A, Wawrzyniak E, Cebula B, Hołowiecki J, Kyrcz-Krzemień S, Grosicki S, Giebel S, Skotnicki AB, Piatkowska-Jakubas B, Kuliczkowski K, Kiełbiński M, Zawilska K, Kłoczko J, Wrzesień-Kuś A, Polish Adult Leukemia Group (2008) Cladribine combined with high doses of arabinoside cytosine, mitoxantrone, and G-CSF (CLAG-M) is a highly effective salvage regimen in patients with refractory and relapsed acute myeloid leukemia of the poor risk: a final report of the Polish Adult Leukemia Group. Eur J Haematol 80(2):115–126
Scappini B, Gianfaldoni G, Caracciolo F, Mannelli F, Biagiotti C, Romani C, Pogliani EM, Simonetti F, Borin L, Fanci R, Cutini I, Longo G, Susini MC, Angelucci E, Bosi A (2012) Cytarabine and clofarabine after high-dose cytarabine in relapsed or refractory AML patients. Am J Hematol 87(12):1047–1051
Roberts DA, Wadleigh M, McDonnell AM, DeAngelo DJ, Stone RM, Steensma DP (2015) Low efficacy and high mortality associated with clofarabine treatment of relapsed/refractory acute myeloid leukemia and myelodysplastic syndromes. Leuk Res 39(2):204–210
Kornblau SM, Gandhi V, Andreeff HM, Beran M, Kantarjian HM, Koller CA, O'Brien S, Plunkett W, Estey E (1996) Clinical and laboratory studies of 2-chlorodeoxyadenosine +/− cytosine arabinoside for relapsed or refractory acute myelogenous leukemia in adults. Leukemia 10(10):1563–1569
Faderl S, Ferrajoli A, Wierda W, Huang X, Verstovsek S, Ravandi F, Estrov Z, Borthakur G, Kwari M, Kantarjian HM (2008) Clofarabine combinations as acute myeloid leukemia salvage therapy. Cancer 113(8):2090–2096
Visani G, Tosi P, Zinzani PL, Manfroi S, Ottaviani E, Testoni N, Clavio M, Cenacchi A, Gamberi B, Carrara P, Gobbi M, Tura S (1994) FLAG (fludarabine + high-dose cytarabine + G-CSF): an effective and tolerable protocol for the treatment of ‘poor risk’ acute myeloid leukemia. Leukemia 8(11):1842–1846
Huhmann IM, Watzke HH, Geissler K, Gisslinger H, Jäger U, Knöbl P, Pabinger I, Korninger L, Mannhalter C, Mitterbauer G, Schwarzinger I, Kalhs P, Haas OA, Lechner K (1996) FLAG (fludarabine, cytosine arabinoside, G-CSF) for refractory and relapsed acute myeloid leukemia. Ann Hematol 73(6):265–271
Nokes TJ, Johnson S, Harvey D, Goldstone AH (1997) FLAG is a useful regimen for poor prognosis adult myeloid leukaemias and myelodysplastic syndromes. Leuk Lymphoma 27(1–2):93–101
Montillo M, Mirto S, Petti MC, Latagliata R, Magrin S, Pinto A, Zagonel V, Mele G, Tedeschi A, Ferrara F (1998) Fludarabine, cytarabine, and G-CSF (FLAG) for the treatment of poor risk acute myeloid leukemia. Am J Hematol 58(2):105–109
Ferrara F, Melillo L, Montillo M, Leoni F, Pinto A, Mele G, Mirto S (1999) Fludarabine, cytarabine, and G-CSF (FLAG) for the treatment of acute myeloid leukemia relapsing after autologous stem cell transplantation. Ann Hematol 78(8):380–384
Robak T, Wrzesień-Kuś A, Lech-Marańda E, Kowal M, Dmoszyńska A (2000) Combination regimen of cladribine (2-chlorodeoxyadenosine), cytarabine and G-CSF (CLAG) as induction therapy for patients with relapsed or refractory acute myeloid leukemia. Leuk Lymphoma 39(1–2):121–129
Hänel M, Friedrichsen K, Hänel A, Herbst R, Morgner A, Neser S, Nicklisch M, Teich M, Ehninger G, Fiedler F (2001) Mito-flag as salvage therapy for relapsed and refractory acute myeloid leukemia. Onkologie 24(4):356–360
Pawson R, Potter MN, Theocharous P, Lawler M, Garg M, Yin JA, Rezvani K, Craddock C, Rassam S, Prentice HG (2001) Treatment of relapse after allogeneic bone marrow transplantation with reduced intensity conditioning (FLAG +/− Ida) and second allogeneic stem cell transplant. Br J Haematol 115(3):622–629
de la Rubia J, Regadera A, Martín G, Cervera J, Sanz G, Martínez J, Jarque I, García I, Andreu R, Moscardó F, Jiménez C, Mollá S, Benlloch L, Sanz M (2002) FLAG-IDA regimen (fludarabine, cytarabine, idarubicin and G-CSF) in the treatment of patients with high-risk myeloid malignancies. Leuk Res 26(8):725–730
Kantarjian H, Gandhi V, Cortes J, Verstovsek S, Du M, Garcia-Manero G, Giles F, Faderl S, O'Brien S, Jeha S, Davis J, Shaked Z, Craig A, Keating M, Plunkett W, Freireich EJ (2003) Phase 2 clinical and pharmacologic study of clofarabine in patients with refractory or relapsed acute leukemia. Blood 102(7):2379–2386
Giles FJ, Cortes JE, Kantarjian HM, O'Brien SM, Estey E, Beran M (2004) A fludarabine, topotecan, and cytarabine regimen is active in patients with refractory acute myelogenous leukemia. Leuk Res 28(4):353–357
Faderl S, Gandhi V, O'Brien S, Bonate P, Cortes J, Estey E, Beran M, Wierda W, Garcia-Manero G, Ferrajoli A, Estrov Z, Giles FJ, Du M, Kwari M, Keating M, Plunkett W, Kantarjian H (2005) Results of a phase 1-2 study of clofarabine in combination with cytarabine (ara-C) in relapsed and refractory acute leukemias. Blood 105(3):940–947
Yavuz S, Paydas S, Disel U, Sahin B (2006) IDA-FLAG regimen for the therapy of primary refractory and relapse acute leukemia: a single-center experience. Am J Ther 13(5):389–393
Hołowiecki J, Grosicki S, Kyrcz-Krzemien S, Skotnicki AB, Piatkowska-Jakubas B, Warzocha K, Seferynska I, Zdziarska B (2008) Daunorubicin, cytarabine and fludarabine (DAF) for remission induction in relapsed or refractory acute myeloid leukemia. Evaluation of safety, tolerance and early outcome—Polish Adult Leukemia Group (PALG) pilot study. Ann Hematol 87(5):361–367
Kim H, Park JH, Lee JH, Lee JH, Joo YD, Lee WS, Bae SH, Mo Ryoo H, Lee KH, Cooperative Study Group A for Hematology (2009) Continuous infusion of intermediate-dose cytarabine and fludarabine with idarubicin for patients younger than 60 years with resistant acute myeloid leukemia: a prospective, multicenter phase II study. Am J Hematol 84(3):161–166
Martin MG, Welch JS, Augustin K, Hladnik L, DiPersio JF, Abboud CN (2009) Cladribine in the treatment of acute myeloid leukemia: a single-institution experience. Clin Lymphoma Myeloma 9(4):298–301
Agura E, Cooper B, Holmes H, Vance E, Berryman RB, Maisel C, Li S, Saracino G, Tadic-Ovcina M, Fay J (2011) Report of a phase II study of clofarabine and cytarabine in de novo and relapsed and refractory AML patients and in selected elderly patients at high risk for anthracycline toxicity. Oncologist 16(2):197–206
McLaughlin B, Im A, Raptis A, Agha M, Hou JZ, Redner R, Duggal S, Lin Y, Smith C, Boyiadzis M (2012) Fludarabine and cytarabine in patients with relapsed acute myeloid leukemia refractory to initial salvage therapy. Int J Hematol 96(6):743–747
Bennett JM, Lymann GH, Cassileth PA, Glick JH, Oken MM (1984) A phase II trial of VP 16-213 in adults with refractory acute myeloid leukemia. An Eastern Cooperative Oncology Group study. Am J Clin Oncol 7(5):471–473
Harousseau JL, Hurteloup P, Reiffers J, Rigal-Huguet F, Hayat M, Dufour P, Le Prise PY, Monconduit M, Jaubert J, Carcassonne Y (1987) Idarubicin in the treatment of relapsed or refractory acute myeloid leukemia. Cancer Treat Rep 71(10):991–992
Bezwoda WR, Bernasconi C, Hutchinson RM, Winfield DA, de Bock R, Mandelli F (1990) Mitoxantrone for refractory and relapsed acute leukemia. Cancer 66(3):418–422
Goldberg J, Gryn J, Raza A, Bennett J, Browman G, Bryant J, Grunwald H, Larson R, Vogler R, Preisler H (1993) Mitoxantrone and 5-azacytidine for refractory/relapsed ANLL or CML in blast crisis: a leukemia intergroup study. Am J Hematol 43(4):286–290
Vogler WR, Harrington DP, Winton EF, Lazarus HM, Bennett JM, Cassileth PA, Oken MM (1992) Phase II clinical trial of carboplatin in relapsed and refractory leukemia. Leukemia 6(10):1072–1075
Welborn JL, Kopecky KJ, Meyers FJ, Veith R, Shurafa M, Doroshow JH, Balcerzak SP, Appelbaum FR (1995) Carboplatin infusion in relapsed and refractory acute myeloid leukemia—a Southwest Oncology Group trial. Leukemia 9(7):1126–1129
Gordon MS, Young ML, Tallman MS, Cripe LD, Bennett JM, Paietta E, Longo W, Gerad H, Mazza J, Rowe JM (2000) Phase II trial of 2-chlorodeoxyadenosine in patients with relapsed/refractory acute myeloid leukemia: a study of the Eastern Cooperative Oncology Group (ECOG), E5995. Leuk Res 24(10):871–875
Roboz GJ, Rosenblat T, Arellano M, Gobbi M, Altman JK, Montesinos P, O'Connell C, Solomon SR, Pigneux A, Vey N, Hills R, Jacobsen TF, Gianella-Borradori A, Foss Ø, Vetrhusand S, Giles FJ (2014) International randomized phase III study of elacytarabine versus investigator choice in patients with relapsed/refractory acute myeloid leukemia. J Clin Oncol 32(18):1919–1926
Knapper S, Chevassut T, Duarte R, Bergua JM, Salamero O, Johansen M, Jacobsen TF, Hals PA, Rasch W, Gianella-Borradori A, Smith M (2014) Elacytarabine in relapsed/refractory acute myeloid leukaemia: an evaluation of clinical efficacy, pharmacokinetics, cardiac safety and effects on lipid profile. Leuk Res 38(3):346–351
Bergmann L, Heil G, Kolbe K, Lengfelder E, Puzicha E, Martin H, Lohmeyer J, Mitrou PS, Hoelzer D (1995) Interleukin-2 bolus infusion as late consolidation therapy in 2nd remission of acute myeloblastic leukemia. Leuk Lymphoma 16(3–4):271–279
Ho AD, Lipp T, Ehninger G, Illiger HJ, Meyer P, Freund M, Hunstein W (1988) Combination of mitoxantrone and etoposide in refractory acute myelogenous leukemia—an active and well-tolerated regimen. J Clin Oncol 6(2):213–217
Rowe JM, Mazza JJ, Hines JD, Cassileth PA, Oken MM, Bennett JM, Andersen J (1990) Mitoxantrone and etoposide in patients with relapsed and refractory acute nonlymphocytic leukemia. Haematol Blood Transfus 33:326–329
Hilbe W, Thaler J, Eisterer W, Ludescher C, Niederwieser D (1994) Treatment of relapsed and refractory acute myelogenous leukaemia with aclacinomycin A (ACA) and etoposide (VP-16). Leuk Res 18(9):655–658
Kern W, Braess J, Grote-Metke A, Kuse H, Fuchs R, Hossfeld DK, Reichle A, Wörmann B, Büchner T, Hiddemann W (1998) Combination of aclarubicin and etoposide for the treatment of advanced acute myeloid leukemia: results of a prospective multicenter phase II trial. German AML Cooperative Group. Leukemia 12(10):1522–1526
Boyiadzis M, Redner RL, Raptis A, Hou JZ, Agha M, Foon KA (2011) Gemtuzumab ozogamicin, mitoxantrone, and etoposide in newly diagnosed acute myeloid leukemia patients with persistent leukemia after a course of induction therapy. Ann Hematol 90(6):733–735
Van Den Neste E, Martiat P, Mineur P, Delannoy A, Doyen C, Zenebergh A, Michaux JL, Ferrant A (1998) 2-Chlorodeoxyadenosine with or without daunorubicin in relapsed or refractory acute myeloid leukemia. Ann Hematol 76(1):19–23
Apostolidou E, Estey E, Cortes J, Garcia-Manero G, Faderl S, Thomas D, Tsimberidou A, Kantarjian H, Giles FJ (2003) Mitoxantrone and prolonged infusion gemcitabine as salvage therapy in patients with acute myelogenous leukemia. Leuk Res 27(4):301–304
Willemze R, Suciu S, Archimbaud E, Muus P, Stryckmans P, Louwagie EA, Berneman Z, Tjean M, Wijermans P, Dohner H, Jehn U, Labar B, Jaksic B, Dardenne M, Zittoun R (1997) A randomized phase II study on the effects of 5-Aza-2′-deoxycytidine combined with either amsacrine or idarubicin in patients with relapsed acute leukemia: an EORTC Leukemia Cooperative Group phase II study (06893). Leukemia 11(Suppl 1):S24–S27
Sanz MA, Sanz GF, Martínez JA, Senent L, López F, Palau J, Martín G, Jarque I (1992) Carboplatin alone or in combination in high-risk acute nonlymphoblastic leukemia. Ann Oncol 3(Suppl 3):39–42
Letendre L, Noel P, Tefferi A, Solberg LA Jr, Gastineau DA, Hoagland HC (1995) Continuous infusion etoposide/carboplatin for treatment of refractory acute leukemia. Am J Clin Oncol 18(5):382–384
Amadori S, Picardi A, Fazi P, Testi AM, Petti MC, Montefusco E, Mandelli F (1996) A phase II study of VP-16, intermediate-dose Ara-C and carboplatin (VAC) in advanced acute myelogenous leukemia and blastic chronic myelogenous leukemia. Leukemia 10:766–768
Kornblau SM, Kantarjian H, O'Brien S, Andreeff M, Koller CA, Beran M, Keating M, Estey E (1998) CECA-cyclophosphamide, etoposide, carboplatin and cytosine arabinoside--a new salvage regimen for relapsed or refractory acute myelogenous leukemia. Leuk Lymphoma 28(3–4):371–375
Belhabri A, Thomas X, Troncy J, Assouline D, Michallet M, Wattel E, Tigaud JD, Blanc M, Fière D, Archimbaud E (1999) Continuous-infusion carboplatin in combination with idarubicin or mitoxantrone for high-risk acute myeloid leukemia: a randomised phase II study. Leuk Lymphoma 36(1–2):45–55
Ferrá C, Berlanga JJ, Gallardo D, Ancín I, Marín D, González JR, Peris J, Muñoz J, Sarrá J, Grañena A (2000) Mitoxantrone, etoposide, carboplatinum and ara-C combination therapy (MECA) in refractory and relapsed acute leukemia. Leuk Lymphoma 39(5–6):583–590
Lee EJ, Egorin MJ, Van Echo DA, Cohen AE, Tait N, Schiffer CA (1988) Phase I and pharmacokinetic trial of carboplatin in refractory adult leukemia. J Natl Cancer Inst 80(2):131–135
Meyers FJ, Welborn J, Lewis JP, Flynn N (1989) Infusion carboplatin treatment of relapsed and refractory acute leukemia: evidence of efficacy with minimal extramedullary toxicity at intermediate doses. J Clin Oncol 7(2):173–178
Martínez JA, Martín G, Sanz GF, Sempere A, Jarque I, de la Rubia J, Sanz MA (1991) A phase II clinical trial of carboplatin infusion in high-risk acute nonlymphoblastic leukemia. J Clin Oncol 9(1):39–43
Horikoshi A, Takei K, Hosokawa Y, Sawada S (2008) The value of oral cytarabine ocfosfate and etoposide in the treatment of refractory and elderly AML patients. Int J Hematol 87(2):118–125
Paciucci PA, Davis RB, Holland JF, Martelo O, Schiffer CA (1990) Mitoxantrone and constant infusion etoposide for relapsed and refractory acute myelocytic leukemia. Am J Clin Oncol 13(6):516–519
Daenen S, Löwenberg B, Sonneveld P, van Putten WL, Verhoef G, Verdonck LF, van Veldhoven M, Huijgens PC (1994) Efficacy of etoposide and mitoxantrone in patients with acute myelogenous leukemia refractory to standard induction therapy and intermediate-dose cytarabine with amsidine. Dutch Hematology-Oncology Working Group for Adults (HOVON). Leukemia 8(1):6–10
Jensen MK, Johansen P, Stentoft J, Jensen MK (1994) Salvage therapy with low-dose cytosine arabinoside in refractory or relapsed acute non-lymphocytic leukaemia: a report on 25 patients. Eur J Haematol 52(4):236–239
Venditti A, Stasi R, Del Poeta G, Buccisano F, Aronica G, Bruno A, Pisani F, Caravita T, Masi M, Tribalto M et al (1995) All-trans retinoic acid and low-dose cytosine arabinoside for the treatment of ‘poor prognosis’ acute myeloid leukemia. Leukemia 9(7):1121–1125
Larson RA, Sievers EL, Stadtmauer EA, Löwenberg B, Estey EH, Dombret H, Theobald M, Voliotis D, Bennett JM, Richie M, Leopold LH, Berger MS, Sherman ML, Loken MR, van Dongen JJ, Bernstein ID, Appelbaum FR (2005) Final report of the efficacy and safety of gemtuzumab ozogamicin (Mylotarg) in patients with CD33-positive acute myeloid leukemia in first recurrence. Cancer 104(7):1442–1452
Taksin AL, Legrand O, Raffoux E, de Revel T, Thomas X, Contentin N, Bouabdallah R, Pautas C, Turlure P, Reman O, Gardin C, Varet B, de Botton S, Pousset F, Farhat H, Chevret S, Dombret H, Castaigne S (2007) High efficacy and safety profile of fractionated doses of Mylotarg as induction therapy in patients with relapsed acute myeloblastic leukemia: a prospective study of the alfa group. Leukemia 21(1):66–71
Ivanoff S, Gruson B, Chantepie SP, Lemasle E, Merlusca L, Harrivel V, Charbonnier A, Votte P, Royer B, Marolleau JP (2013) 5-Azacytidine treatment for relapsed or refractory acute myeloid leukemia after intensive chemotherapy. Am J Hematol 88(7):601–605
Itzykson R, Thépot S, Berthon C, Delaunay J, Bouscary D, Cluzeau T, Turlure P, Prébet T, Dartigeas C, Marolleau JP, Recher C, Plantier I, Stamatoullas A, Devidas A, Taksin AL, Guièze R, Caillot D, Vey N, Adès L, Ifrah N, Dombret H, Fenaux P, Gardin C (2015) Azacitidine for the treatment of relapsed and refractory AML in older patients. Leuk Res 39(2):124–130
Stalh M, Podoltsev NA, DeVeaux M, Perreault S, Itzykson R, Ritchie EK, Sekeres MA, Fathi AT, Komrokji RS, Bhatt VR, Al-Kali A, Cluzeau T, Santini V, Brunner A, Roboz GJ, Fenaux P, Litzow M, Vey N, Verma V, Germing U, Montesinos P, Zelterman D, Kim TK, Prebet T, Gore SD, Zeidan AM (2016) The use of hypomethylating agents (HMAs) in patients with relapsed and refractory acute myeloid leukemia (RR-AML): clinical outcomes and their predictors in a large international patient cohort. Blood 128(21):1063
Ritchie EK, Feldman EJ, Christos PJ, Rohan SD, Lagassa CB, Ippoliti C, Scandura JM, Carlson K, Roboz GJ (2013) Decitabine in patients with newly diagnosed and relapsed acute myeloid leukemia. Leuk Lymphoma 54(9):2003–2007
Raffoux E, Cras A, Recher C, Boëlle PY, de Labarthe A, Turlure P, Marolleau JP, Reman O, Gardin C, Victor M, Maury S, Rousselot P, Malfuson JV, Maarek O, Daniel MT, Fenaux P, Degos L, Chomienne C, Chevret S, Dombret H (2010) Phase 2 clinical trial of 5-azacitidine, valproic acid, and all-trans retinoic acid in patients with high-risk acute myeloid leukemia or myelodysplastic syndrome. Oncotarget 1(1):34–42
Daver N, Kantarjian H, Ravandi F, Estey E, Wang X, Garcia-Manero G, Jabbour E, Konopleva M, O'Brien S, Verstovsek S, Kadia T, Dinardo C, Pierce S, Huang X, Pemmaraju N, Diaz-Pines-Mateo M, Cortes J, Borthakur G (2016) A phase II study of decitabine and gemtuzumab ozogamicin in newly diagnosed and relapsed acute myeloid leukemia and high-risk myelodysplastic syndrome. Leukemia 30(2):268–273
Piccaluga PP, Martinelli G, Rondoni M, Malagola M, Gaitani S, Isidori A, Bonini A, Gugliotta L, Luppi M, Morselli M, Sparaventi G, Visani G, Baccarani M (2004) Gemtuzumab ozogamicin for relapsed and refractory acute myeloid leukemia and myeloid sarcomas. Leuk Lymphoma 45(9):1791–1795
Bolaños-Meade J, Smith BD, Gore SD, McDevitt MA, Luznik L, Fuchs EJ, Jones RJ (2011) 5-azacytidine as salvage treatment in relapsed myeloid tumors after allogeneic bone marrow transplantation. Biol Blood Marrow Transplant 17(5):754–758
Al-Ali HK, Jaekel N, Junghanss C, Maschmeyer G, Krahl R, Cross M, Hoppe G, Niederwieser D (2012) Azacitidine in patients with acute myeloid leukemia medically unfit for or resistant to chemotherapy: a multicenter phase I/II study. Leuk Lymphoma 53(1):110–117
Chowdhury S, Seropian S, Marks PW (2009) Decitabine combined with fractionated gemtuzumab ozogamicin therapy in patients with relapsed or refractory acute myeloid leukemia. Am J Hematol 84(9):599–600
Estey E, Thall P, Andreeff M, Beran M, Kantarjian H, O'Brien S, Escudier S, Robertson LE, Koller C, Kornblau S et al (1994) Use of granulocyte colony-stimulating factor before, during, and after fludarabine plus cytarabine induction therapy of newly diagnosed acute myelogenous leukemia or myelodysplastic syndromes: comparison with fludarabine plus cytarabine without granulocyte colony-stimulating factor. J Clin Oncol 12(4):671–678
Tse E, Leung AY, Sim J, Lee HK, Liu HS, Yip SF, Kwong YL (2011) Clofarabine and high-dose cytosine arabinoside in the treatment of refractory or relapsed acute myeloid leukaemia. Ann Hematol 90(11):1277–1281
Yang H, Hoshino K, Sanchez-Gonzalez B, Kantarjian H, Garcia-Manero G (2005) Antileukemia activity of the combination of 5-aza-2′-deoxycytidine with valproic acid. Leuk Res 29(7):739–748
Löwenberg B, van Putten W, Theobald M, Gmür J, Verdonck L, Sonneveld P, Fey M, Schouten H, de Greef G, Ferrant A, Kovacsovics T, Gratwohl A, Daenen S, Huijgens P, Boogaerts M, Dutch-Belgian Hemato-Oncology Cooperative Group; Swiss Group for Clinical Cancer Research (2003) Effect of priming with granulocyte colony-stimulating factor on the outcome of chemotherapy for acute myeloid leukemia. N Engl J Med 349(8):743–752
Leopold LH, Willemze R (2002) The treatment of acute myeloid leukemia in first relapse: a comprehensive review of the literature. Leuk Lymphoma 43(9):1715–1727
Mangan JK, Luger SM (2011) Salvage therapy for relapsed or refractory acute myeloid leukemia. Ther Adv Hematol 2(2):73–82
Bryan JC, Jabbour EJ (2015) Management of relapsed/refractory acute myeloid leukemia in the elderly: current strategies and developments. Drugs Aging 32(8):623–637
Thol F, Schlenk RF, Heuser M, Ganser A (2015) How I treat refractory and early relapsed acute myeloid leukemia. Blood 126(3):319–327
Kuo YH, Qi J, Cook GJ (2016) Regain control of p53: targeting leukemia stem cells by isoform-specific HDAC inhibition. Exp Hematol 44(5):315–321
Breems DA, Van Putten WL, Huijgens PC, Ossenkoppele GJ, Verhoef GE, Verdonck LF, Vellenga E, De Greef GE, Jacky E, Van der Lelie J, Boogaerts MA, Löwenberg B (2005) Prognostic index for adult patients with acute myeloid leukemia in first relapse. J Clin Oncol 23(9):1969–1978
Hiddemann W, Martin WR, Sauerland CM, Heinecke A, Büchner T (1990) Definition of refractoriness against conventional chemotherapy in acute myeloid leukemia: a proposal based on the results of retreatment by thioguanine, cytosine arabinoside, and daunorubicin (TAD 9) in 150 patients with relapse after standardized first line therapy. Leukemia 4(3):184–188
Giralt S, Estey E, Albitar M, van Besien K, Rondón G, Anderlini P, O'Brien S, Khouri I, Gajewski J, Mehra R, Claxton D, Andersson B, Beran M, Przepiorka D, Koller C, Kornblau S, Kørbling M, Keating M, Kantarjian H, Champlin R (1997) Engraftment of allogeneic hematopoietic progenitor cells with purine analog-containing chemotherapy: harnessing graft-versus-leukemia without myeloablative therapy. Blood 89(12):4531–4536
O'Donnell MR, Tallman MS, Abboud CN, Altman JK, Appelbaum FR, Arber DA, Bhatt V, Bixby D, Blum W, Coutre SE, De Lima M, Fathi AT, Fiorella M, Foran JM, Gore SD, Hall AC, Kropf P, Lancet J, Maness LJ, Marcucci G, Martin MG, Moore JO, Olin R, Peker D, Pollyea DA, Pratz K, Ravandi F, Shami PJ, Stone RM, Strickland SA, Wang ES, Wieduwilt M, Gregory K, Ogba N (2017) Acute myeloid leukemia, version 3.2017, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw 15(7):926–957
Bertoli S, Gadaud N, Tavitian S, Sarry A, Bérard E, Huguet F, Recher C (2016) Is intermediate-dose Cytarabine a good control for patients with relapsed or refractory acute myeloid leukemia? Blood 128:3991
Schlenk RF, Döhner K, Mack S, Stoppel M, Király F, Götze K, Hartmann F, Horst HA, Koller E, Petzer A, Grimminger W, Kobbe G, Glasmacher A, Salwender H, Kirchen H, Haase D, Kremers S, Matzdorff A, Benner A, Döhner H (2010) Prospective evaluation of allogeneic hematopoietic stem-cell transplantation from matched related and matched unrelated donors in younger adults with high-risk acute myeloid leukemia: German-Austrian trial AMLHD98A. J Clin Oncol 28(30):4642–4648
Duval M, Klein JP, He W, Cahn JY, Cairo M, Camitta BM, Kamble R, Copelan E, de Lima M, Gupta V, Keating A, Lazarus HM, Litzow MR, Marks DI, Maziarz RT, Rizzieri DA, Schiller G, Schultz KR, Tallman MS, Weisdorf D (2010) Hematopoietic stem-cell transplantation for acute leukemia in relapse or primary induction failure. J Clin Oncol 28(23):3730–3738
Wattad M, Weber D, Döhner K, Krauter J, Gaidzik VI, Paschka P, Heuser M, Thol F, Kindler T, Lübbert M, Salih HR, Kündgen A, Horst HA, Brossart P, Götze K, Nachbaur D, Köhne CH, Ringhoffer M, Wulf G, Held G, Salwender H, Benner A, Ganser A, Döhner H, Schlenk RF (2017) Impact of salvage regimens on response and overall survival in acute myeloid leukemia with induction failure. Leukemia 31(6):1306–1313
Bennett TA, Montesinos P, Moscardo F, Martinez-Cuadron D, Martinez J, Sierra J, García R, de Oteyza JP, Fernandez P, Serrano J, Fernandez A, Herrera P, Gonzalez A, Bethancourt C, Rodriguez-Macias G, Alonso A, Vera JA, Navas B, Lavilla E, Lopez JA, Jimenez S, Simiele A, Vidriales B, Gonzalez BJ, Burgaleta C, Hernandez Rivas JA, Mascuñano RC, Bautista G, Perez Simon JA, Fuente Ade L, Rayón C, Troconiz IF, Janda A, Bosanquet AG, Hernandez-Campo P, Primo D, Lopez R, Liebana B, Rojas JL, Gorrochategui J, Sanz MA, Ballesteros J (2014) Pharmacological profiles of acute myeloid leukemia treatments in patient samples by automated flow cytometry: a bridge to individualized medicine. Clin Lymphoma Myeloma Leuk 14:305–318
Acknowledgements
We are grateful to Vivia Biotech for an educational grant that supported this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they no competing interests.
Rights and permissions
About this article
Cite this article
Megías-Vericat, J.E., Martínez-Cuadrón, D., Sanz, M.Á. et al. Salvage regimens using conventional chemotherapy agents for relapsed/refractory adult AML patients: a systematic literature review. Ann Hematol 97, 1115–1153 (2018). https://doi.org/10.1007/s00277-018-3304-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-018-3304-y