Abstract
CD34 positivity has been considered as an adverse prognostic factor in acute myeloid leukemia (AML). Although nucleophosmin 1-mutated (NPM1m) AML is usually CD34 negative, this marker may be expressed at diagnosis or acquired at relapse in a variable number of cases. Our objective was to ascertain if CD34 expression has any influence on the general outcome of this form of acute leukemia. Analysis of clinical outcome (complete remissions, relapses, disease-free survival, and overall survival) was performed depending on the degree of expression of CD34 determined by flow cytometry, in 67 adult patients with NPM1m AML. CD34 expression did not have any influence on the variables analyzed whatever the percentage of blasts expressing this marker. In contrast to other forms of AML, CD34 expression is not an unfavorable prognostic factor in NPM1m AML, neither at diagnosis nor at relapse.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to the 2008 WHO classification, current characterization of acute myeloid leukemia (AML) relies on cytogenetic/molecular or morphological characteristics of leukemic cells. AML with mutated nucleophosmin 1 (NPM1) is the most frequent subtype of normal karyotype AML listed in the WHO classification yet as a provisional entity [1]. Typically, NPM1-mutated (NPM1m) leukemia exhibits a peculiar cup-like morphology while immunophenotyping discloses a variable degree of myeloid/monocytic differentiation, without expression of CD34 and HLA-DR antigens in the majority of cases. However, NPM1m blasts may express CD34 in a variable proportion, ranging from 0.04 % to more than 20 % of the blastic population [2–4]. Although NPM1m AML is considered to have a relative good prognosis, relapses are also observed. Some additional factors (FLT3-internal tandem duplication (ITD), IDH1/IDH, and DNMT3A mutations) exert an influence on the global outcome [5].
The prognostic value of some immunophenotypic characteristics on the general outcome of AML has been a matter of debate for years [6]. Concerning CD34, the general consensus is that its expression confers a worse prognosis [7–9] although opposite results have also been published [10]. In the case of NPM1m AML, the influence of CD34 has been analyzed by different authors, with inconclusive or contradictory results: in a group of 83 patients studied by the Spanish CETLAM group, CD34 expression was associated with a trend to a worse outcome [2]. In a group of 71 patients studied in China, the expression of CD34 in more than 7 % of blasts was clearly associated with a lower number of complete remissions (CR), shorter disease-free survival (DFS), and worse overall survival (OS) [11]. In a series studied in Toronto, CD34 positivity in more than 20 % of blasts cells had a deleterious influence only on OS [3].
The aim of our study was to analyze the prognostic importance of CD34 expression on blastic cells both at diagnosis and at relapse and the relation of CD34 with the presence/absence of FLT3-ITD, in a group of 67 patients diagnosed with NPM1m AML homogeneously treated in two centers (in the text, center 1 and center 2) of the same institution (Institut Català d’Oncologia) in the metropolitan area of Barcelona (Catalonia, Spain)
Patients and methods
Patients, diagnostic criteria, and treatment
From January 2004 to March 2013, 67 consecutive patients aged between 18 and 70 years old were diagnosed with NPM1m AML at our institution. The diagnosis of AML was made on bone marrow (BM) smears with the exception of “dry tap” samples, in which the diagnosis was made in peripheral blood (PB) or in touch imprints of a BM biopsy. Diagnoses were established according to the 2008 criteria of the WHO classification [1]. Line ascertainment (myeloid/monocytic) was made on the basis of cytology, cytochemistry, and immunophenotyping. Besides NPM1, FLT3 abnormalities were also studied.
Patients were treated with chemotherapy regimens according to the CETLAM 2003 protocol for patients up to 70 years [2], which includes induction therapy with idarubicin (12 mg/m2 on days 1, 3, and 5), cytarabine (500 mg/m2/12 h on days 1, 3, 5, and 7), etoposide (100 mg/m2 on days 1, 2, and 3), and granulocyte colony-stimulating factor (G-CSF) (150 μg/m2 from days 0 to 7). If CR was not attained, a new induction course was repeated with the same drugs and doses. After the achievement of CR, the patients received intensification therapy with cytarabine (500 mg/m2/12 h on days 1–6), mitoxantrone (12 mg/m2 on days 4–6), and G-CSF (150 μg/m2 from days 0 to 6). Patients with favorable genetic characteristics received a second intensification cycle with cytarabine 500 mg/m2/12 h on days 1–6. Patients with intermediate risk (normal karyotype and absence of MLL and FLT3-ITD, which includes the majority of NPM1-AML patients) were allocated to receive autologous hematopoietic stem cell transplantation (HSCT). Patients with poor risk features (unfavorable cytogenetics, MLL rearrangements, FLT3-ITD and monosomal karyotype) were allocated to allogeneic HSCT.
Immunophenotypic analysis
Briefly, 100 μL of BM or PB collected in ethylenediaminetetraacetic (EDTA) acid anticoagulant, previously adjusted to a cellular concentration of 10,000 cells/μL, was incubated in the dark with 5 μL of MoAb for 15 min, in five color combinations. After incubation, red cells were lysed, washed with PBS, centrifuged, decanted, and re-suspended in 500 μL of PBS for analysis. CD34 (clone 581) was supplied by Immunotech (Beckman Coulter, Marseille, France) (center 1) or BD Pharmingen (Becton Dickinson, San Jose, CA, USA) (center 2) and was combined with PE at least in one of the tubes of the diagnostic panel.
Acquisition was performed with a Cytomics FC500 (Beckman Coulter), equipped with CXP software (Beckman Coulter) in center 1 and in a FACSCanto (Becton Dickinson) equipped with FACSDiva software in center 2. A minimum of 20,000 events per tube were acquired whenever possible. Analytical gates were established according to CD45 reactivity and FSS/SSC patterns. CD34 positivity was expressed as the percentage of cells expressing this marker in the blastic region in CD45/side scatter plots. In the majority of cases, these cells coexpressed CD117 with CD13 and/or CD33.
Cytogenetic studies
PB or BM cells were cultured in a RPMI 1640 medium supplemented with fetal calf serum, antibiotic, and glutamine for 24 h. Conventional chromosome G-banding preparations were performed using standard techniques, and karyotypes were described according to the International System for Cytogenetic Nomenclature (ISCN 2013).
Molecular genetic analysis
Diagnostic samples for all patients were analyzed for mutations in the NPM1 and FLT3 genes using standard protocols. DNA was extracted from peripheral blood or bone marrow samples collected in EDTA with the QIAamp DNA Blood Mini Kit (Qiagen, Hilden, Germany) and was diluted with ddH2O. Analysis of FLT3-IT, FLT-D835, and NPM1 exon 12 mutations was performed in genomic DNA by PCR amplification with a 6-FAM labeled primer followed by fragment analysis as previously described with few modifications. Briefly, each PCR reaction was performed in a 50 μL of reaction volume. The master mix contained 0.4 μL Taq at 5 U/μL (Ecogen, Valencia, Spain); 1.25 μL of each primer at 12.5 and 10 μM, respectively; 1 μL of dNTP at 10 mM; and 50 ng DNA template. The mix was subjected to an ABI 9700 thermal cycler (Applied Biosystems, Foster City, CA, USA) for the gene amplification (PCR protocol: initial denaturation of 94 °C for 5 min, followed by 35 or 28 cycles (FLT3-ITD and D835 or NPM1) of 94 °C for 45 s, 56 or 62 °C (FLT3-ITD or NPM1) for 45 s, 72 °C for 45 s, and a final extension step of 72 °C for 7 min). For FLT3-D835 mutations, a final digestion step with EcoRV enzyme at 37 °C was done. All products were then brought into the 3130 Genetic Analyzer (Applied Biosystems, Foster City, CA, USA) and screened for mutations with the GeneMapper software. When possible, the FLT3-ITD ratio was calculated as follows: area behind the mutated allele/area behind the wild-type allele.
Statistical analysis
Baseline demographic and clinical-biological characteristics were presented as median and range for continuous variables and frequency and percentage for categorical variables. Comparisons of these variables between patient groups were performed by chi-square, Fisher’s exact, Student’s t, or Mann-Whitney U test, as appropriate. Complete remission was defined as the achievement of morphological leukemia-free state along with a value for neutrophil count >1000 μL, a platelet count >100.000 μL, and independence from red cell transfusion. Overall survival was defined as the time from diagnosis to time of death from any cause. Disease-free survival was defined as the time from CR achievement to the time of relapse or death from any cause.
The Kaplan-Meier method was used for calculating OS and DFS curves, and log-rank test was used for comparisons between groups. Statistical analyses were carried out using Statistical Package for Social Sciences (SPSS, IBM) package version 15 for Windows.
Results
Patient characteristics
Twenty-nine out of the 67 patients (43 %) were males and 38 were females (57 %). Median age was 53 years (range 18–69). Table 1 summarizes these demographic data along with FLT3 status, number of patients with cytogenetic abnormalities, number of patients with CD34 expression in more than 20 % of blasts, and months of follow-up.
Immunophenotypic analysis
CD34 positivity at diagnosis
The blasts of 8/67 patients (12 %) expressed CD34 in a percentage ≥20 % (median 53 %, range 20–84); on the other hand, a variable degree of CD34 expression but at a percentage <20 % was observed in 32/67 patients (48 %), with a median value of 2.0 % (range 1–15). In 27/67 patients (40 %), CD34 expression was 0 %.
Cytogenetics
Cytogenetic analysis was performed in all but one patient; no growth was obtained in three. Nine patients (13.4 %) presented different and heterogeneous cytogenetic abnormalities, as described in Table 1. The presence of cytogenetic abnormalities was not associated with CD34 expression, albeit with one exception (CD34 13 % in a case with +21). Those cases with CD34 ≥20 % presented no karyotypic abnormalities.
Molecular biology
FLT3 status was studied in all patients. FLT3-ITD was detected in 24/67 patients (36 %) and the FLT3-D835 point mutation in 2/67 patients (3 %) (patients excluded for further analysis). Only four patients with FLT3-ITD were CD34 positive. There was no association between the presence of FLT3-ITD and the percentage of CD34 expression (Table 2). As per the FLT3-ITD ratio, this parameter could be obtained in 13 out of 24 mutated patients. Its median value was 0.72 (range 0.12–2.7) and was higher than 0.5 in 10 cases. Although the number of patients is low, apparently, there was no relationship between the value of the ratio and the percentage of CD34-positive cells.
Clinical correlations of CD34 expression
Complete remission (CR) rate
CR was attained by 54/67 patients (81 %). Neither the frank positivity for CD34 (≥20 %) nor any lower percentage of CD34 expression on blasts at diagnosis influenced the achievement of CR, as can be seen in Table 3.
Thirteen of the patients who achieved CR (24 %) were allocated to receive chemotherapy, 12 (22 %) received autologous HSCT, and 29 (54 %) received allogeneic HSCT.
Disease-free survival (DFS)
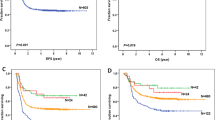
Median DFS (95 % CI) for the 54 patients that attained CR was 32.4 months (0–72.8). DFS was not influenced by CD34 positivity or negativity at diagnosis. In those cases with CD34 expression ≥20 % (n = 6), median DFS (95 % CI) was 17.8 months (0–38.6), while in cases with a lower or nil percentage of CD34 expression (n = 48), median DFS was 32.4 months (0–77.9). The behavior of DFS according to the percentage of CD34 expression is shown in Fig. 1. No statistically significant differences were observed between both groups (p = 0.430).
Relapses
Relapse of AML was observed in 11 out of 54 patients that achieved CR (20 %). The probability of relapse was not related with the expression of CD34 by blastic cells at diagnosis, as summarized in Table 4. Four out of these 11 relapsed patients did not express anymore the mutated form of NPM1 in the relapse episode. These low numbers of patients which maintain mutated NPM1 or that lose these mutation expressed at diagnosis did not allow a reliable statistical analysis exploring the relationship with CD34. Only one of these patients acquired FLT3-ITD at relapse.
Overall survival (OS)
Median OS (95 % CI) of the whole series was 18.9 months (0–53.1). CD34 positivity ≥20 % at diagnosis was not related with OS, its median (95 % CI) being 8.2 months (0–23.7) for the 8 patients with CD34 positivity ≥20 % and 21.7 months (0–61.6) for 59 patients with a lower or nil percentage of CD34 expression in blast cells. These results are represented in Fig. 2, which analyzes OS depending on the percentage of CD34 expression. No statistically significant differences were observed between both groups (p = 0.259).
CD34 acquisition at relapse (11 out of 54 CR patients, 20 %)
Among 11/54 relapsed cases, CD34 positivity ≥20 % of blasts (median 30 %, range 20–80 %) was acquired by seven patients; it is of note that in six of these patients, CD34 was negative or lower that 5 % at first diagnosis. The positivity percentage at diagnosis was already high (CD34 52 %) in the remaining case.
Discussion
As a general rule, the expression of CD34 by blastic cells in AML has been considered by some to be related to outcome [7–9] but the leukemic cells of some forms of AML may not express this marker or express it partially. We have centered our study in acute myeloid leukemia with NPM1 mutation, the most frequent type of cytogenetically normal AML, which exhibits blasts with monocytic features and low or absent expression of CD34, yet a variable number of cases clearly express it [2–4]. Although NPM1m leukemias have a better prognosis than other forms of AML [12], relapses also occur, occasionally with phenotypic changes characterized by the acquisition of CD34. The prognostic value of the expression of CD34 in NPM1m AML has been a matter of debate for years. In 2011, Jiang et al. [13] reported that the bad prognosis conferred by CD34 positivity in AML was counterbalanced by the mutation in NPM1, but they did not analyze separately CD34-positive vs CD34-negative NPM1m cases. In a study of 83 patients of our geographical area (northeast of Spain), Nomdedeu et al. [2] did not observe any correlation between CD34 positivity (≥20 %) and the presence of FLT3-ITD, frequently present in NPM1m AML. CD34 was expressed de novo in four over eight relapsed cases, but no mention was done on the clinical behavior of these cases that acquired CD34 at relapse. A worse prognosis due to the CD34 positivity has also been observed in NPM1m AML patients when blasts also express CD7 [14]. The bad impact on OS conferred by CD34 has also been observed by others [3]. The influence of any degree of expression of CD34 in these types of leukemia has been studied by Zhu et al. [11] that defined a cutoff >7 % of CD34 positivity as predictive of a worse DFS and OS.
As can be seen from the literature, the role of CD34 expression in NPM1m AML is controversial yet a deleterious effect of CD34 positivity in AML as a whole has been widely accepted since the 1990s [7–9, 15, 16]. For this reason, we tried to ascertain if this negative effect is also operative in NPM1m AML both at diagnosis and at relapse and to explore the relationship, if any, between the expression of CD34 and the presence FLT3-ITD.
According to our results, the answer to these questions is negative. Neither the frank positivity of CD34 (expression in ≥20 % of blasts) nor any other lower degree of CD34 expression (from 0 to 15 %) exerted any negative influence on the main clinical variables analyzed, i.e., OS, DFS, and CR. Relapses occurred in 11 out of 57 patients who attained CR, but the degree of CD34 expression at diagnosis did not show any influence of the probability of relapsing. The low numbers of patients that acquire CD34 at relapse do not allow performing a comparison of their clinical behavior with those patients who did not acquire this marker.
FLT3-ITD that frequently accompanies NPM1m AML was also observed in 24 out of our 67 patients (36 %), a higher percentage than that previously reported in our geographical area (22 %) [17], but again, no relationship could be established between the presence of this molecular abnormality and the percentage of expression of CD34 by blasts.
We do not have a clear explanation for the different results observed in our series when compared with some, but not all, of the results reported in the literature, as it also happened with other phenotypic markers that our group has evaluated in terms of their predictive value [18]. It is plausible that besides technical aspects, our current therapeutic protocols and the rather unrestricted practice of stem cell transplantation would overcome the adverse influence of some markers, in this case CD34, by blast cells. According to our findings, the influence of NPM1 mutation on the outcome of this type of AML patients is not modulated by the expression of CD34, as has been claimed for other types of AML.
In all, our study shows that the degree of expression of CD34 by blastic cells does not seem to be related with the outcome of NPM1m AML, thus favoring the idea that the general prognosis of this type of leukemia depends not on phenotypic characteristics but on the molecular lesions, with FLT3-ITD and other molecular abnormalities (DNMT3A, IDH1/2), when present, acting as modulators that do have an impact on the general outcome [19]. In this sense, a multivariate analysis taking age, clinical parameters, cytogenetics and molecular data, flow cytometry findings, and type of treatment into account would be warranted to determine the prognostic impact of CD34 in this form of leukemia.
References
Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri S, Stein H, et al. (Editors). International Agency for Research on Cancer. World Health Organization classification of tumours of haematopoietic and lymphoid tissues. 4th ed. Lyon: International Agency for Research on Cancer; 2008
Nomdedeu J, Bussaglia E, Villamor N, Martínez C, Esteve J, Tormo M et al (2011) Immunophenotype of acute myeloid leukemia with NPM mutations: prognostic impact of leukemic compartment size. Leuk Res 35:163–168
Dang H, Chen Y, Kamel-Reid S, Brandwein J, Chang H (2013) CD34 expression predicts an adverse outcome in patients with NPM1-positive acute myeloid leukemia. Human Pathology 44:2038–2046
Liu YR, Zhu HH, Ruan GR, Ya ZK, Shi HX, Lay YY et al (2013) NPM1-mutated acute myeloid leukemia of monocytic or myeloid origin exhibit distinct phenotypes. Leuk Res 37:737–741
Krönke J, Bullinger L, Teleanu V, Tschürtz F, Gaidzik VI, Kühn MWM et al (2013) Clonal evolution in relapsed NPM1-mutated acute myeloid leukemia. Blood 122:100–108
Ossenkoppele GJ, van de Loosdrecht AA, Schuurhuis GJ (2011) Review of the relevance of aberrant antigen expression by flow cytometry in myeloid neoplasms. Br J Haematol 153:421–436
Casasnovas RO, Slimane FK, Garand R, Faure GC, Campos L, Deneys V et al (2003) Immunological classification of acute myeloblastic leukemias: relevance to patient outcome. Leukemia 17:515–527
Webber BA, Cushing MM, Li S (2008) Prognostic significance of flow cytometric immunophenotyping in acute myeloid leukemia. Int J Clin Exp Pathol 1:124–133
García-Dabrio C, Hoyos M, Brunet S, Tormo M, Ribera JM, Esteve J et al (2015) Complex measurements may be required to establish the prognostic impact of immunophenotypic markers in AML. Am J Clin Pathol 144:484–92
Iriyama N, Asou N, Miyazaki Y, Tamaguchi S, Sato S, Sakura T et al (2014) Normal karyotype acute myeloid leukemia with the CD7+ CD15+ CD34+ HLA-DR+ immunophenotype is a clinically distinct entity with a favorable outcome. Ann Hematol 93:957–63
Zhu HH, Liu YR, Jiang H, Lu J, Qin YZ, Jiang Q et al (2013) CD34 expression on bone marrow blasts is a novel predictor of poor prognosis independent of FLT3-ITD in acute myeloid leukemia with the NPM1-mutation. Leuk Res 37:624–630
Döhner K, Schlenk RF, Habdank M, Scholl C, Rücker FG, Corbacioglu A et al (2005) Mutant nucleophosmin (NPM1) predicts favorable prognosis in younger adults with acute myeloid leukemia and normal cytogenetics: interaction with other gene mutations. Blood 106:3740–3746
Jiang A, Jiang H, Brandwein J, Kamel-Reid S, Chang H (2011) Prognostic factors in normal karyotype acute myeloid leukemia in the absence of the FLT3-ITD mutation. Leuk Res 35:492–498
Chen CH, Chou WC, Tsay W, Tang JL, Yao M, Huang SY et al (2013) Hierarchical cluster analysis of immunophenotype classify AML patients with NPM1 gene mutation into two groups with distinct prognosis. BMC Cancer 13:107
Thomas X, Archimbaud E, Charrin C, Magaud JP, Fiere D (1995) CD34 expression is associated with major adverse prognostic factors in adult acute lymphoblastic leukemia. Leukemia 9:249–253
Plesa C, Chelghoum Y, Plesa A, Elhamri M, Tigaud I, Michallet M et al (2008) Prognostic value of immunophenotyping in elderly patients with acute myeloid leukemia. Cancer 112:572–580
Pratcorona M, Brunet S, Nomdedéu J, Ribera JM, Tormo M, Duarte R et al (2013) Favorable outcome of patients with acute myeloid leukemia harboring a low-allelic burden FLT3-ITD mutation and concomitant NPM1 mutation: relevance to post-remission therapy. Blood 121:2734–2738
Juncà J, García-Caro M, Granada I, Rodríguez-Hernández I, Torrent A, Morgades M, Ribera JM, Millá F, Feliu E et al (2014) Correlation of CD11b and CD56 expression in adult acute myeloid leukemia with cytogenetic risk groups and prognosis. Ann Hematol 93:1483–1489
Peterlin P, Renneville A, Ben Abdelali R, Nibourel O, Thomas X, Pautas C et al (2015) Impact of additional genetic alterations on the outcome of patients with NPM1-mutated cytogenetically normal acute myeloid leukemia. Haematologica 100:e196–199. doi:10.3324/haematol.2014.115576
Acknowledgments
We would like to acknowledge the Institut Josep Carreras for its contribution in everyday support in the diagnosis and outcome evaluation of our patients.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Juncà, J., Garcia, O., Garcia-Caro, M. et al. CD34 expression and the outcome of nucleophosmin 1-mutated acute myeloid leukemia. Ann Hematol 95, 1949–1954 (2016). https://doi.org/10.1007/s00277-016-2811-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-016-2811-y