Abstract
The incidence of cytomegalovirus (CMV) reactivation/disease after autologous stem cell transplant (ASCT) is much lower than that after allogeneic stem cell transplantation. With the recent use of rituximab during cancer chemotherapy or conditioning regimens prior to transplantation, there has been an increasing concern of opportunistic infections including CMV. In the present study, we reviewed the patients undergoing ASCT from December 2007 to December 2013 to identify those developing CMV reactivation/disease. Out of the 978 patients who underwent ASCT at the Karmanos Cancer Institute, 239 patients were tested for symptomatic CMV reactivation based on clinical suspicion. Of the tested patients, 7/239 (2.9 %) were documented to have CMV reactivation within 90 days of ASCT. The median time to develop CMV viremia was 32 days from transplantation. Of the 239 patients tested, CMV viremia was detected in 3 out of 72 patients who received rituximab as compared to 4 out of 167 patients who did not. Three of these seven viremic patients were treated with anti-viral drugs; viremia resolved in all patients at a median of 24 days. Three patients were found to develop other bacterial and/or fungal infections following CMV viremia. Two of the seven patients died during 1-year follow-up, due to primary disease progression or Candida sepsis. None of the patients developed proven tissue-invasive CMV disease. The study did not evaluate the incidence of asymptomatic CMV infection/reactivation. Despite prior publications based on limited data, rituximab does not appear to contribute to an increased frequency of symptomatic CMV reactivation following ASCT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of cytomegalovirus (CMV) reactivation after autologous stem cell transplantation (ASCT) has been reported (4–9 %) to be much lower than that reported following allogeneic transplantation (21–38 %) [1]. There are reports of CMV infection/disease following ASCT, along with high rates of mortality primarily due to CMV pneumonia [2–6]. However, most of this information is from the era prior to novel chemotherapeutic agents. In recent years, with changing chemotherapeutic regimens, available information is limited on the clinical progression and implications of CMV reactivation after ASCT. One of the recent changes has been the exposure to rituximab during cancer chemotherapy or conditioning regimen.
Rituximab is an anti-CD20 monoclonal antibody that induces complement mediated and antibody dependent cellular toxicity. It has known efficacy in non-Hodgkin’s lymphoma (NHL) [7] and also used as preparative regimen with BEAM (carmustine, etoposide, cytarabine, and melphalan) prior to autologous transplant [8]. There have been reports of increased CMV reactivation attributed to the use of rituximab during the peri-transplantation period [9–11].
The aim of our study is (1) to estimate the burden and determine the characteristics of CMV infection and disease after ASCT in recent years and (2) to assess the effect of exposure to rituximab in the occurrence of CMV infection/disease after ASCT.
Material and methods
Medical records at the Karmanos Cancer Center were searched for occurrence of CMV infection/disease during the 90-day post-transplantation period in patients undergoing ASCT between December 2007 and December 2013. Data of those detected to have CMV viremia by polymerase chain reaction (PCR) within 90 days of ASCT were analyzed. Demographic characteristics, transplant data, and disease outcomes were obtained in all patients.
None of the patients underwent routine surveillance for CMV. Symptoms/signs suggestive of CMV reactivation/infection/disease prompted the clinician to obtain serum CMV PCR test. Most common reasons for serum CMV PCR test included fever not responding to first line antibiotics and persistent respiratory or gastrointestinal symptoms of unclear etiology. None received anti-CMV drugs prior to transplantation.
Standard statistical methods were used to compare variables if needed using SPSS version 21 (IBM, Armonk, NY, USA). Chi square test or Fischer’s exact test were used to compare categorical variables as appropriate.
Definitions
- CMV infection::
-
Isolation of virus or detection of viral proteins or nucleic acid in blood or tissue specimen.
- CMV disease::
-
Histologically proven end-organ disease with CMV infection.
Death was attributed to CMV if there was evidence of autopsy proven organ damage by CMV.
Exposure to rituximab was considered positive if the drug was used as a part of the primary treatment for malignancy or in the conditioning regimen prior to transplantation.
Neutrophil engraftment was defined as the time to the first of the three consecutive days, in which absolute neutrophil count was ≥0.5 × 109/l.
The study was approved by the Institutional Review Board at Wayne State University and Karmanos Cancer Center, Detroit, MI.
Results
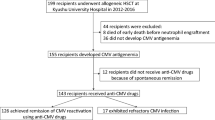
A total of 978 patients underwent ASCT during the study period. Underlying malignancy was multiple myeloma in 601 patients, NHL in 251 patients, Hodgkin’s disease (HD) in 96 patients, and acute myeloid leukemia (AML) in four patients. Other malignancies included breast cancer in 4, testicular cancer in 9, and amyloidosis in 21 patients. Pre-transplant data are summarized in Table 1.
Most patients were undergoing first stem cell transplantation. About one quarter (24 %) of patients were exposed to rituximab. Fifty-seven percent patients were CMV seropositive. With antibiotic-refractory fever, CMV PCR was tested in 239 patients within 90 days of ASCT. CMV reactivation was clinically not suspected in the remaining patients. Hence, they were not tested. CMV PCR was positive in blood in 7 patients (<1 % of total 978, 2.9 % of patients tested for CMV). Of these seven patients, three patients had received rituximab prior to ASCT during induction or preparative regimen. The remaining four did not receive rituximab prior to ASCT.
CMV viremia was detected at a median 32 days from ASCT (range, 18–44 days). Four of the seven CMV PCR positive patients had multiple myeloma, 2 had NHL and 1 had HD. All seven patients who developed CMV viremia were seropositive prior to ASCT; CMV reactivation occurred after neutrophil engraftment in all cases. Details of the CMV reactivation are summarized in Table 2. One of the patients (#6, Table 2) developed fever and shortness of breath; bronchoalveolar lavage was positive on direct immunofluorescence assay for CMV, which was confirmed by culture. Treatment was initiated with intravenous ganciclovir for “CMV pneumonitis.” However, after 14 days, treatment was aborted and alternative diagnosis was sought due to no improvement in symptoms and low clinical suspicion.
Of these seven patients, three developed other bacterial or fungal infections (Table 3) within 60 days of CMV viremia detection. One of the patients (#2) grew Aspergillus niger and methicillin-resistant Staphylococcus aureus (MRSA) in sputum prior to CMV detection in blood. Two patients died within 30 days of detection of CMV viremia; deaths were attributed to primary disease progression and septic shock from candidemia.
Discussion
Nearly one thousand patients undergoing autologous stem cell transplantation were included in the present study; <1 % of the patients were detected to have CMV reactivation. However, not all patients were routinely tested. Of the 239 patients tested for CMV reactivation, 2.9 % developed CMV reactivation.
A total of 72 patients out of 239 received rituximab prior to ASCT. Three of the 72 patients (4.2 %) that received rituximab prior to ASCT and 4 out of 167 patients (2.4 %) never exposed to rituximab prior to ASCT developed CMV viremia after ASCT (Fischer’s exact p value = 0.34). Rituximab does not appear to be a significant risk for symptomatic CMV reactivation. Asymptomatic CMV reactivation however may have occurred; since CMV PCR was not routinely done in the entire population, the current study did not address this issue.
The United States Food and Drug Administration first approved rituximab, a monoclonal antibody directed against CD20 antigen on B-lymphocytes, in 1997 for treatment of B-cell NHL. It has since been used as a single agent and in combination for treatment of multiple hematological malignancies and rheumatologic disorders in addition to preparative regimen with BEAM prior to bone marrow transplant. However, there has been an increasing concern of rituximab adversely affecting immunity due to the effect on B cells, among other mechanisms [12]. Among opportunistic pathogens, CMV reactivation has been attributed to rituximab exposure in the post-transplantation period [9–11]. Overall there is limited data on CMV reactivation/disease in the ASCT setting in the era of rituximab. In a small study of 46 ASCT recipients, the risk to develop CMV infection was 18 % in rituximab-exposed patients, compared to 0 in controls (p = 0.04). Risk for CMV disease was 12 % vs. 0, respectively [11]. Similarly, in the study by Al-Rawi et al., at a single center that included 210 patients, CMV reactivation rate after ASCT was 18 % [13]. Routine surveillance of CMV antigen detection in blood was used as the method of detection. The majority of patients received anti-CMV therapy, and none developed symptomatic CMV infection.
Underlying malignancy in patients detected with CMV viremia was multiple myeloma in four out of seven patients in our study. Three of these were treated with bortezomib-based regimens and all four were treated with immunomodulators as a part of the regimen. Recent report from the Rome Transplant Network has indicated a higher risk of CMV reactivation in patients of multiple myeloma treated with bortezomib-based regimens though, as mentioned in the study, this might be the result of increased testing in patients receiving bortezomib [14]. The drug is known to increase susceptibility to viral infections due to decreased number and function of natural killer cells and CD8+/CD4+ T cells. Multiple myeloma patients also have innate immunosuppression as a result of their underlying disease.
Our study included 903 patients undergoing first ASCT and 75 patients undergoing second ASCT for relapsed or progressive underlying malignancy (none of them were planned tandem transplants). Four patients out of these 903 (0.4 %) and three out of the 75 (4 %) developed reactivation of CMV after transplant (Fischer’s exact test p value = 0.01; chi square 0.006). Previously, there have been single center studies in patients undergoing tandem transplants for multiple myeloma. Kim et al. identified CMV reactivation more common in recipients of tandem transplant as compared to single transplants [15]. However, Marchesi et al. did not show increased risk of CMV reactivation with tandem ASCT [16]. More studies are needed to study the effect of second and tandem transplants in the occurrence of CMV reactivation after ASCT. All patients who were detected with CMV viremia were seropositive prior to ASCT (7/553), a known risk factor for CMV infection/disease [3, 4].
Not all patients with viremia were treated with anti-viral agents. The viremia resolved in a median of 24 days (range, 5–95 days) in all seven patients, with or without treatment. No patients had serious clinical sequela from CMV reactivation. Two died within 30 days of detection of CMV viremia, the causes of death were progression of primary disease and septic shock from candida infection. There does not appear to be any benefit of anti-CMV therapy in such ASCT patients, particularly with low-grade CMV viremia. A few patients developed bacterial or fungal infection soon after CMV detection and one patient had Aspergillus and MRSA in respiratory samples. Presence of other infections may simply be a consequence of immune suppression due to CMV reactivation.
Our study reviewed 978 ASCT patients over a period of 6 years. Based on clinical suspicion, 239 (20 % of total) were tested for symptomatic CMV reactivation post-ASCT. The limitation of this retrospective study is that the CMV PCR testing was not routinely performed in all patients. Hence, asymptomatic CMV reactivation may have been missed in this study. It must be pointed out that asymptomatic CMV reactivation in this population may not be of clinical significance.
Conclusion
Symptomatic CMV infection/reactivation remains uncommon in the autologous transplantation setting. Use of rituximab prior to ASCT in induction or conditioning regimens does not increase the risk of symptomatic CMV reactivation/disease. In addition, in individuals with low-grade CMV viremia after auto transplantation, therapy against CMV does not appear to be necessary.
References
Fassas AB, Bolanos-Meade J, Buddharaju LN et al (2001) Cytomegalovirus infection and non-neutropenic fever after autologous stem cell transplantation: high rates of reactivation in patients with multiple myeloma and lymphoma. Br J Haematol 112:237–241
Boeckh M, Stevens-Ayers T, Bowden RA (1996) Cytomegalovirus pp 65 antigenemia after autologous marrow and peripheral blood stem cell transplantation. J Infect Dis 174:907–912
Konoplev S, Champlin RE, Giralt S et al (2001) Cytomegalovirus pneumonia in adult autologous blood and marrow transplant recipients. Bone Marrow Transplant 27:877–881
Bilgrami S, Aslanzadeh J, Feingold JM et al (1999) Cytomegalovirus viremia, viruria and disease after autologous peripheral blood stem cell transplantation: no need for surveillance. Bone Marrow Transplant 24:69–73
Holmberg LA, Boeckh M, Hooper H et al (1999) Increased incidence of cytomegalovirus disease after autologous CD34-selected peripheral blood stem cell transplantation. Blood 94:4029–4035
Rossini F, Terruzzi E, Cammarota S et al (2005) Cytomegalovirus infection after autologous stem cell transplantation: incidence and outcome in a group of patients undergoing a surveillance program. Transpl Infect Dis Off J Transplant Soc 7:122–125
Coiffier B, Lepage E, Briere J et al (2002) CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large-B-cell lymphoma. N Engl J Med 346:235–242
Fenske TS, Hari PN, Carreras J et al (2009) Impact of pre-transplant rituximab on survival after autologous hematopoietic stem cell transplantation for diffuse large B cell lymphoma. Biol Blood Marrow Transplant J Am Soc Blood Marrow Transplant 15:1455–1464
Goldberg SL, Pecora AL, Alter RS et al (2002) Unusual viral infections (progressive multifocal leukoencephalopathy and cytomegalovirus disease) after high-dose chemotherapy with autologous blood stem cell rescue and peritransplantation rituximab. Blood 99:1486–1488
Suzan F, Ammor M, Ribrag V (2001) Fatal reactivation of cytomegalovirus infection after use of rituximab for a post-transplantation lymphoproliferative disorder. N Engl J Med 345:1000
Lee MY, Chiou TJ, Hsiao LT et al (2008) Rituximab therapy increased post-transplant cytomegalovirus complications in non-Hodgkin’s lymphoma patients receiving autologous hematopoietic stem cell transplantation. Ann Hematol 87:285–289
Kelesidis T, Daikos G, Boumpas D, Tsiodras S (2011) Does rituximab increase the incidence of infectious complications? A narrative review. Int J Infect Dis IJID Off Publ Int Soc Infect Dis 15:e2–e16
Al-Rawi O, Abdel-Rahman F, Al-Najjar R et al (2015) Cytomegalovirus reactivation in adult recipients of autologous stem cell transplantation: a single center experience. Mediterr J Hematol Infect Dis 7:e2015049
Marchesi F, Mengarelli A, Giannotti F et al (2014) High incidence of post-transplant cytomegalovirus reactivations in myeloma patients undergoing autologous stem cell transplantation after treatment with bortezomib-based regimens: a survey from the Rome Transplant Network. Transpl Infect Dis Off J Transplant Soc 16:158–164
Kim JH, Goulston C, Sanders S et al (2012) Cytomegalovirus reactivation following autologous peripheral blood stem cell transplantation for multiple myeloma in the era of novel chemotherapeutics and tandem transplantation. Biol Blood Marrow Transplant J Am Soc Blood Marrow Transplant 18:1753–1758
Marchesi F, Pimpinelli F, Dessanti ML et al (2014) Evaluation of risk of symptomatic cytomegalovirus reactivation in myeloma patients treated with tandem autologous stem cell transplantation and novel agents: a single-institution study. Transpl Infect Dis Off J Transplant Soc 16:1032–1038
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
The study was approved by the Institutional Review Board at Wayne State University and Karmanos Cancer Center, Detroit, MI.
Rights and permissions
About this article
Cite this article
Jain, T., John, J., Kotecha, A. et al. Cytomegalovirus infection in autologous stem cell transplant recipients in the era of rituximab. Ann Hematol 95, 1323–1327 (2016). https://doi.org/10.1007/s00277-016-2700-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-016-2700-4