Abstract
The efficacy of danazol was assessed in 50 patients with myelofibrosis and anemia using the recently revised criteria of the International Working Group for Myelofibrosis Research and Treatment. According to them, anemia response (clinical improvement) is defined as transfusion cessation in transfusion-dependent patients or an Hb increase >2 g/dl in patients without transfusion requirements, both maintained for at least 12 weeks. Median follow-up from danazol start was 36 months (interquartile range [IQR] 19.2–58.8). Anemia response was achieved in 15 patients (30 %), including 5 of the 27 with transfusion dependency (18.5 %) and 10 of the 23 without transfusion requirements (43.5 %). Median time to response was 5 months (IQR 4–7) and median duration of the response 14 months (IQR 10–21). Among responder patients, 5 discontinued therapy due to toxicity or personal decision and 1 died from spleen rupture while being in response. A trend for worse response was seen in transfusion-dependent patients (p = 0.055). A platelet increase >50 × 109/l was observed in 3 of 13 thrombocytopenic patients, all of whom had moderate thrombocytopenia. Toxicity was usually moderate, leading to treatment withdrawal in only 4 patients. Danazol is effective in 30 % of patients with anemia-associated myelofibrosis. The responses are less frequent in patients with transfusion dependency.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
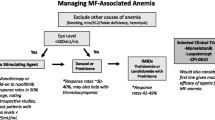
Myelofibrosis (MF), either de novo (primary myelofibrosis or PMF) or evolving from a previously known essential thrombocythemia or polycythemia vera (post-ET or post-PV myelofibrosis), is a BCR/ABL1-negative chronic myeloproliferative neoplasm characterized from the clinical point of view by the progressive development of cytopenias, splenomegaly, and constitutional symptoms [1]. Anemia is the more frequent manifestation of myelofibrosis [2]. Therapeutic options include erythropoiesis-stimulating agents (ESA), androgens, immunomodulating agents, and splenectomy, with responses ranging from 20 to 40 % [2]. However, a substantial proportion of patients does not respond or loses the initial response. Therefore, anemia remains an unmet need in MF, with this being especially so for patients with transfusion dependency. In this sense, attempts to expand its therapeutic options have yielded unsatisfactory results [3]. Recently, the International Working Group for Myelofibrosis Research and Treatment (IWG-MRT) proposed a stringent set of criteria of response for its use in clinical trials [4]. Danazol, a semisynthetic attenuated androgen of widespread use in the anemia of myelofibrosis, might be a good candidate for comparison with newer anemia-treating agents, since it results in an anemia response rate of 37 % [5]. However, the latter figure was based on the use of less strict response criteria, whereas information on the long-term efficacy of the drug is limited.
The primary goal of the present study was to analyze the results of danazol therapy in a large series of MF patients with anemia using the revised criteria of the IWG-MRT. This information could be of interest not only in clinical practice but also in designing clinical trials aimed to assess the efficacy of newer drugs for the anemia of myelofibrosis.
Methods
Patients and diagnostic criteria
Fifty consecutive patients with myelofibrosis received danazol as therapy of anemia between November 1995 and September 2014. Given the type of study, formal consent was not required. The patients’ main characteristics at the time of treatment start are summarized in Table 1. The results in the first 30 patients were reported 10 years ago [5]. The criteria for danazol institution have previously been described [2]. In brief, screening for concurrent causes of anemia (such as iron, folate, or vitamin B12 deficiency, or autoimmune hemolysis when applicable) was carried out and patients treated accordingly in case that one of such causes was detected. If no concurrent cause of anemia was found, patients received danazol as first therapy for the anemia during the first 8 years of the study period. Later on, the initial choice between danazol and ESA was based on the patients’ erythropoietin (Epo) levels: if adequate (>125 mU/ml), patients were started on danazol, whereas if inadequate, an ESA was the first-choice therapy, with the patients being switched to danazol in case of primary or secondary failure.
The diagnosis of MF was made according to the criteria in use at the time of first observation, but it was confirmed using the current criteria of the World Health Organization in PMF [6] and the criteria of the International Consensus in post-PV and post-ET myelofibrosis [7]. One of the patients included in the original series was reclassified as having a myelodysplastic syndrome with myelofibrosis according to the current criteria and subsequently excluded from the present analysis. The distribution of the bone marrow histological subtypes was carried out using the European consensus criteria [8].
Treatment schedule, response criteria, and toxicity assessment
Before starting danazol, male patients were asked for prostatic symptoms and serum PSA levels were determined to rule out prostate cancer. All patients were scheduled to receive danazol orally at an initial dose of 600 mg daily, which was maintained for 6 months unless toxicity developed. After this period, responders had a dose reduction to 400 mg daily for an additional 6 months, and then the drug was gradually tapered down to the minimum dose necessary to maintain the response. In patients not showing signs of response at 6 months, therapy was definitively discontinued.
During treatment, standard hematological and biochemical parameters were monitored at every visit and possible adverse effects recorded. In addition, ultrasound imaging was performed annually to exclude the appearance of liver tumors, whereas males were periodically screened for prostate cancer.
The response was assessed using the recently revised criteria of the International Working Group for Myelofibrosis Research and Treatment (IWG-MRT) [4], according to which anemia response (included in the category of “clinical improvement”) is considered in two different situations: (1) transfusion cessation, in transfusion-dependent patients, and (2) an Hb increase >2 g/dl, in patients without transfusion dependency, both lasting for a minimum of 12 weeks. During the initial phase of therapy, patients were monitored on a monthly basis, and thereafter, the timing of monitoring was adjusted based on the response seen in each individual patient. Concerning transfusions, the general policy was to transfuse packed RBCs when the Hb levels dropped below 8 g/dl or the anemia was overtly symptomatic. Thrombocytopenia response was defined as a platelet increase >50 × 109/l in patients with baseline counts <100 × 109/l.
Concomitant therapy
In no patient, danazol was started at the same time as other therapies. However, a previously instituted therapy was maintained in 19 patients, including hydroxyurea (n = 11), low-dose prednisone (n = 5), and anagrelide (n = 3).
Statistical analysis
The primary study outcome was anemia response. In thrombocytopenic patients, platelet response was also analyzed. The following pretreatment variables were evaluated for their potential relationship with anemia response: patient’s age and gender, disease risk score by either the IPSS [9] or the DIPSS [10], depending on whether danazol was instituted at MF diagnosis or later on, constitutional symptoms (weight loss, night sweats, low-grade fever), spleen size, Hb level, reticulocyte counts, transfusion dependency, leukocyte and platelet counts, presence of circulating blast cells, JAK2 mutational status, bone marrow histologic subtypes, and cytogenetics. Quantitative data are expressed as median and interquartile range (IQR) and qualitative data as percentages. Differences in the distribution of categorical and continuous variables were evaluated by the chi-square and the Mann-Whitney U tests. Response duration was defined as the time from the achievement of response to treatment failure, including loss of response, change of therapy, or patient’s death. The probability of survival was analyzed with the Kaplan-Meier method and compared by the log-rank test. In all tests, p values of less than or equal to 0.05 were considered as statistically significant. The statistical analysis was performed using the IBM SPSS 19.0 package (SPSS, Chicago, IL, USA).
Results
After initial screening, no patient potentially eligible for danazol therapy was excluded because of concurrent liver or prostate disease. Table 1 shows the main characteristics of the 50 patients at danazol start. According to the European consensus criteria, 20 patients had MF-1, 17 had MF-2, and 13 had MF-3. Twenty-five percent of the patients had constitutional symptoms and 28 % had >1 % blasts in the peripheral blood. Twenty-seven patients had transfusion dependency at time of danazol initiation. Concerning the prognostic group (IPSS or DIPSS), 27 patients belonged to the intermediate-1 risk category, 15 to the intermediate-2 risk group, and 8 had high-risk myelofibrosis. Metaphases from bone marrow or unstimulated peripheral blood were available in only 19 patients, being normal in 14 of them.
Danazol was the first treatment in 23 patients; the remainder had previously received other therapies, including hydroxyurea (n = 18), ESA (n = 13), anagrelide (n = 5), prednisone (n = 3), splenectomy (n = 2), and ruxolitinib, interferon, radioactive phosphorus, and cyclosporin A (1 patient each).
Median follow-up from danazol start was 36 months (IQR 19.2–58.8). Anemia response was achieved in 15 of the 50 patients (30 %), including 5 of the 27 with transfusion dependency (18.5 %) and 10 of the 23 without transfusion requirements (43.5 %). Table 2 shows the main characteristics of the responders. Median time to response was 5 months (IQR 4–7), and in only 4 patients, the response was observed within the first 3 months of treatment. Three patients who responded at 6 months showed further improvement of the response between months 7 to 10 of treatment. At univariate analysis, the only pretreatment variable associated with the response (lack of response) was transfusion dependency (p = 0.055). No influence could be demonstrated for other clinico-hematological variables, including spleen size or previous splenectomy. In responder patients, maintenance danazol dose was 200 mg daily. Median duration of anemia response was 14 months (IQR 10–21). At this writing, 2 patients remained on treatment at 10 and 12 months from danazol start, 8 patients lost the response at 3.2–46 months of its achievement, and 5 definitively discontinued treatment while in response due to toxicity or personal decision. Among the latter patients, 4 of them lost the response within 3 months of danazol discontinuation while the remaining 1 maintains the response at 8 months of treatment discontinuation. A platelet increase >50 × 109/l was observed in 3 of the 13 patients with baseline counts <100 × 109/l, for an overall thrombocytopenia response of 23 %; of note, all platelet responders had moderate thrombocytopenia.
Danazol was generally well tolerated. The most frequent toxicity consisted of a moderate increase (grades 1–2 of the WHO scale) in the liver enzymes during the initial months of treatment, which was observed in eight patients and improved in all cases after a dose reduction to 400 mg/day. However, two additional patients had severe cholestatic hepatitis, with bilirubin levels exceeding 20 mg/dl that completely solved at several weeks of danazol discontinuation. Two other patients experienced severe side effects also leading to definitive treatment stop: prostate adenocarcinoma and liver peliosis, respectively. One patient died while in response due to spleen rupture, and other patients decided to stop therapy while being in response. One patient lost the response coincidently with the evolution of myelofibrosis to acute leukemia. One patient had deep vein thrombosis. Headache and mild muscle mass increase were occasionally observed.
During follow-up, evolution to acute leukemia was observed in 8 patients, at a median of 18 months (IQR 13.2–59) from danazol start. At last follow-up, 30 patients had died; median survival from danazol initiation was 3.8 years (95 % CI 2.7–4.9).
Discussion
Anemia is the more frequent manifestation of myelofibrosis. It is mainly due to decreased bone marrow production, ineffective erythropoiesis, hypersplenism, and occasional bleeding [11]. Dilution by the increased plasma volume secondary to splenomegaly can also contribute, as well as iron, vitamin B12, or folate deficiency, or autoimmune hemolysis [11]. The anemia is often accentuated by the cytoreductive agents [12] or the JAK inhibitors [13] given to treat the proliferative manifestations of myelofibrosis. Once the abovementioned causes have been ruled out, therapeutic options include erythropoiesis-stimulating agents (ESA), androgens, immunomodulating drugs, and splenectomy. Anemia response to ESA ranges from 23 to 60 %, depending on the criteria of response used, and it is usually restricted to patients with inadequate Epo levels, being less frequent in patients with large spleens or transfusion dependency [14–17]. With immunomodulating drugs such as thalidomide or lenalidomide, usually given in combination with prednisone, responses are 19 to 35 %, but there is frequent discontinuation due to side effects [18–20]. Anemia response to splenectomy in MF patients is 25 %, with the procedure being associated with substantial risk [21].
Androgens have long been used to treat the anemia of MF [22, 23], with responses ranging from 30 to 60 % of patients. While conventional androgens are associated with important side effects, similar therapeutic results, with less toxicity, have been observed with danazol, a semisynthetic attenuated androgen. Thus, in our original series, anemia response to danazol was 37 % [5]. However, this rate was calculated using criteria of response less strict than those recently proposed by the IWG-MRT [4]. In the present series, including a higher number of patients and with substantially longer follow-up, anemia response was slightly lower (30 %), a fact that should be ascribed to the use of more stringent response criteria. Thus, while in our initial report anemia response was considered for Hb increases >1.5 g/dl lasting for at least 8 weeks, in the present series, the threshold for a favorable response was increased to >2 g/dl and for a minimum duration of 12 weeks, according to the recently revised criteria of the IWG-MRT [4]. In this sense, it must be pointed out that the latter criteria have been proposed for their use in clinical trials in order to demonstrate clear efficacy of new therapies. However, in daily practice, Hb increases between 1.5 and 2 g/dl can be clinically relevant for some patients. For instance, in one of our patients, the Hb value increased from 9.6 to 11.1 g/dl and this was associated with a clear improvement in the symptoms. Therefore, although this response was not considered a therapeutic failure in clinical practice, it did not qualify for clinical improvement by applying the current response criteria.
Median time to response to danazol was 5 months, with only four patients responding within the first 3 months of treatment, a fact stressing the need for allowing a sufficient treatment period before declaring a patient as non-responder. On the other hand, once a response was achieved and progressive dose reduction applied, the minimum necessary dose to maintain the response was 200 mg daily. Of note, a loss of response was seen after a few weeks of the drug discontinuation in four out of the five patients in whom danazol was stopped while in response because of toxicity, a fact that would indicate the need for maintenance therapy.
Concerning the prediction of the response, the only pretreatment variable showing a trend for an association with the response to danazol was transfusion dependency, with only 18.5 % responses observed in this subgroup of patients versus 43.5 % in patients without transfusion requirements. This observation is not exclusive of danazol, as it has also been reported for other anemia-treating drugs such as the ESA [14, 17]. Moreover, with pomalidomide, a newer immunomodulating drug that showed promise in a phase 2 study [24], anemia response rate was 16 % in transfusion-dependent patients, which was not significantly different from the results obtained in the placebo arm that included the administration of low-dose prednisone during the first 3 months [3]. These results would reinforce the notion of transfusion-dependent anemia as the more important unmet clinical need in myelofibrosis. On the other hand, although in our series thrombocytopenia response was observed in almost a quarter of patients with low platelet counts, it must be noted that all responders had moderate thrombocytopenia, while no response was seen in patients with deeper degrees of thrombocytopenia.
Danazol was generally well tolerated. The most frequent toxicity consisted of a moderate increase in the liver enzymes observed during the first months of treatment, which usually improved after reducing the dose to 400 mg daily. However, two patients had severe cholestatic hepatitis leading to definitive danazol discontinuation. An additional patient developed liver peliosis, while prostate cancer was diagnosed in a male patient. These complications, although infrequent, stress the importance of liver monitoring and periodic imaging surveillance during danazol treatment, as well as of systematic screening for prostate cancer in men.
In conclusion, danazol was effective for the anemia in 30 % of MF patients. However, the low response rate observed in patients with transfusion dependency stresses the need for investigating newer agents to treat this important complication of myelofibrosis.
References
Tefferi A (2000) Myelofibrosis with myeloid metaplasia. N Engl J Med 342:1255–1265
Cervantes F (2014) How I treat myelofibrosis. Blood 124:2635–2642
Tefferi A, Passamonti F, Barbui T, Barosi G, Begna K, Cazzola M, Cervantes F, Döhner K, Gisslinger H, Gupta V, Li W, Harrison CN, Kiladjian JJ, McMullin MF, Rambaldi A, Schiller GJ, Vannucchi AM, Mesa RA (2013) Phase 3 study of pomalidomide in myeloproliferative neoplasm (MPN)-associated myelofibrosis with RBC-transfusion dependence (abstract). Blood 122:394
Tefferi A, Cervantes F, Mesa R, Passamonti F, Verstovsek S, Vannucchi AM, Gotlib J, Dupriez B, Pardanani A, Harrison C, Hoffman R, Gisslinger H, Kroger N, Thiele J, Barbui T, Barosi G (2013) Revised response criteria for myelofibrosis: International Working Group-Myeloproliferative Neoplasms Research and Treatment (IWG-MRT) and European LeukemiaNet (ELN) consensus report. Blood 122:1395–1398
Cervantes F, Alvarez-Larrán A, Domingo A, Arellano-Rodrigo E, Montserrat E (2005) Efficacy and tolerability of danazol as a treatment for the anaemia of myelofibrosis with myeloid metaplasia: long-term results in 30 patients. Br J Haematol 129:771–775
Tefferi A, Thiele J, Orazi A, Kvasnicka HM, Barbui T, Hanson CA, Barosi G, Verstovsek S, Birgegard G, Mesa R, Reilly JT, Gisslinger H, Vannucchi AM, Cervantes F, Finazzi G, Hoffman R, Gilliland DG, Bloomfield CD, Vardiman JW (2007) Proposals and rationale for revision of the World Health Organization diagnostic criteria for polycythemia vera, essential thrombocythemia, and primary myelofibrosis: recommendations from an ad hoc international expert panel. Blood 110:1092–1097
Barosi G, Mesa RA, Thiele J, Cervantes F, Campbell PJ, Verstovsek S, Dupriez B, Levine RL, Passamonti F, Gotlib J, Reilly JT, Vannucchi AM, Hanson CA, Solberg LA, Orazi A, Tefferi A (2008) Proposed criteria for the diagnosis of post-polycythemia vera and post-essential thrombocythemia myelofibrosis: a consensus statement from the International Working Group for Myelofibrosis Research and Treatment. Leukemia 22:438–439
Thiele J, Kvasnicka HM, Facchetti F, Franco V, van der Walt J, Orazi A (2005) European consensus on grading bone marrow fibrosis and assessment of cellularity. Haematologica 90:1128–1132
Cervantes F, Dupriez B, Pereira A, Passamonti F, Reilly JT, Morra E, Vannucchi AM, Mesa RA, Demory JL, Barosi G, Rumi E, Tefferi A (2009) New prognostic scoring system for primary myelofibrosis based on a study of the International Working Group for Myelofibrosis Research and Treatment. Blood 113:2895–2901
Passamonti F, Cervantes F, Vannucchi AM, Morra E, Rumi E, Pereira A, Guglielmelli P, Pungolino E, Caramella M, Maffioli M, Pascutto C, Lazzarino M, Cazzola M, Tefferi A (2010) A dynamic prognostic model to predict survival in primary myelofibrosis: a study by the IWG-MRT (International Working Group for Myeloproliferative Neoplasms Research and Treatment). Blood 115:1703–1708
Reilly JT (1998) Pathogenesis and management of idiopathic myelofibrosis. Baillière’s Clin Hematol 11:751–767
Martínez-Trillos A, Gaya A, Maffioli M, Arellano-Rodrigo E, Calvo X, Díaz-Beyá M, Cervantes F (2010) Efficacy and tolerability of hydroxyurea in the treatment of the hyperproliferative manifestations of myelofibrosis: results in 40 patients. Ann Hematol 89:1233–1237
Harrison C, Kiladjian JJ, Al-Ali HK, Gisslinger H, Waltzman R, Stalbovskaya V, McQuitty M, Hunter DS, Levy R, Knoops L, Cervantes F, Vannucchi AM, Barbui T, Barosi G (2012) JAK inhibition with ruxolitinib versus best available therapy for myelofibrosis. N Engl J Med 366:787–798
Cervantes F, Alvarez-Larrán A, Hernández-Boluda JC, Sureda A, Torrebadell M, Montserrat E (2004) Erythropoietin treatment of the anaemia of myelofibrosis with myeloid metaplasia: results in 20 patients and review of the literature. Br J Haematol 127:399–403
Cervantes F, Alvarez-Larrán A, Hernández-Boluda JC, Sureda A, Granell M, Vallansot R, Besses C, Montserrat E (2006) Darbepoetin-alpha for the anaemia of myelofibrosis with myeloid metaplasia. Br J Haematol 134:184–186
Tsiara SN, Chaidos A, Bourantas LJ, Kapsali HD, Bourantas KL (2007) Recombinant human erythropoietin for the treatment of anemia in patients with idiopathic myelofibrosis. Acta Haematol 11:156–161
Huang J, Tefferi A (2009) Erythropoiesis stimulating agents have limited therapeutic activity in transfusion-dependent patients with primary myelofibrosis regardless of serum erythropoietin level (letter). Eur J Haematol 83:154–155
Mesa RA, Steensma DP, Pardanani A, Li CY, Elliott M, Kaufmann SH, Wiseman G, Gray LA, Schroeder G, Reeder T, Zeldis JB, Tefferi A (2003) A phase 2 trial of combination low-dose thalidomide and prednisone for the treatment of myelofibrosis with myeloid metaplasia. Blood 101:2534–2541
Mesa RA, Yao X, Li CY, Litzow M, Paietta E, Rowe JM, Tefferi A, Tallman MS (2010) Lenalidomide and prednisone for myelofibrosis: Eastern Cooperative Oncology Group (ECOG) phase 2 trial E4903. Blood 116:4436–4438
Quintás-Cardama A, Kantarjian HM, Manshouri T, Thomas D, Cortes J, Ravandi F, Garcia-Manero G, Ferrajoli A, Bueso-Ramos C, Verstovsek S (2009) Lenalidomide plus prednisone results in durable clinical, histopathologic, and molecular responses in patients with myelofibrosis. J Clin Oncol 27:4760–4766
Tefferi A, Mesa RA, Nagomey DN, Schroeder G, Silverstein MN (2000) Splenectomy in myelofibrosis with myeloid metaplasia: a single-institution experience with 223 patients. Blood 95:2226–2233
Hast R, Engstedt L, Jameson S, Killander A, Lundh B, Reizenstein P, Skarberg KO, Udén AM, Wadman B (1978) Oxymetholone treatment in myelofibrosis. Blut 37:19–26
Brubaker LH, Brière J, Laszlo J, Kraut E, Landaw SA, Peterson P, Goldberg J, Donovan P (1982) Treatment of anemia in myeloproliferative disorders: a randomized study of fluoxymesterone v transfusions only. Arch Intern Med 142:1533–1537
Tefferi A, Verstovsek S, Barosi G, Passamonti F, Roboz GJ, Gisslinger H, Paquette RL, Cervantes F, Rivera CE, Deeg HJ, Thiele J, Kvasnicka HM, Vardiman JW, Zhang Y, Bekele BN, Mesa RA, Gale RP, Kantarjian HM (2009) Pomalidomide is active in the treatment of anemia associated with myelofibrosis. J Clin Oncol 27:4563–4569
Acknowledgments
This work was supported in part by grant RD12/0036/0010 from the Instituto de Salud Carlos III, Spanish Ministry of Health.
Authorship contributions
Francisco Cervantes designed the research, interpreted the results, and wrote the manuscript. Ignacio M. Isola, Juan-Gonzalo Correa, Alberto Alvarez-Larrán, and Juan-Carlos Hernández-Boluda collected the data, revised the manuscript, and approved its final version. Arturo Pereira performed the statistical analysis, interpreted the results, and revised the manuscript.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cervantes, F., Isola, I.M., Alvarez-Larrán, A. et al. Danazol therapy for the anemia of myelofibrosis: assessment of efficacy with current criteria of response and long-term results. Ann Hematol 94, 1791–1796 (2015). https://doi.org/10.1007/s00277-015-2435-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-015-2435-7