Abstract
Ocular adnexal lymphoma (OAL) has been associated with Chlamydophila psittaci infection, for which doxycycline has been suggested as a treatment option. We conducted this study to evaluate the long-term results of first-line doxycycline treatment in patients with OAL. Ninety patients with histologically confirmed OAL with marginal zone B cell lymphoma were enrolled. Each patient received one or two cycles of doxycycline (100 mg bid) for 3 weeks. After a median follow-up period of 40.5 months (8–85), the 5-year progression-free survival (PFS) rate was 60.9 %. All patients were alive at the last follow-up date. Thirty-one patients (34 %) showed local treatment failure without systemic spread. However, PFS rate in these patients was 100 % after salvage chemotherapy and/or radiotherapy. PFS was independently predicted in multivariate analysis by the tumor-node-metastasis (TNM) staging (hazard ratio [HR], 4.35; 95 % confidence interval [CI], 2.03–9.32; P < 0.001) and number of cycles of doxycycline (HR, 0.31; 95 % CI, 0.14–0.69; P = 0.004). No serious adverse event was reported during doxycycline therapy. In conclusion, first-line doxycycline therapy was effective and safe. Patients who failed to respond to doxycycline therapy were successfully salvaged with chemotherapy and/or radiotherapy without compromising long-term outcomes. Patients with T1N0M0 disease could be considered good candidates for first-line doxycycline.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ocular adnexal lymphoma (OAL) occurs in approximately 1–2 % of non-Hodgkin lymphomas (NHL) and 8 % of extranodal lymphomas [1]. The incidence is increasing by approximately 6.3 % annually, according to Surveillance, Epidemiology, and End Results data [2]. In Korea, the frequency of OAL is higher than in Western countries, and younger patients are affected [1, 3, 4]. The major histology is marginal zone B cell lymphoma of the mucosa-associated lymphoid tissue type (MALT), followed by follicular, diffuse large B cell, mantle cell, and small lymphocyticlymphoma in rare cases. Typically, marginal zone B cell lymphoma involving ocular adnexa is a clinically slow growing tumor in the eyelid, orbit, lacrimal gland, or conjunctiva, and the slow growth may contribute to delayed diagnosis.
Chronic antigen stimulation is considered to be a pathogenic mechanism causing malignant transformation of a normal lymphoid cell to MALT lymphoma. Chlamydophila psittaci (Cp) has been suggested as an antigen in OAL [5]. In humans, Cp is an etiological agent of psittacosis, which is caused by exposure to infected animals including birds, domestic mammals, and pets. The risk of OAL is markedly increased by contact with animals, and Cp DNA has been found in 80 % of OAL patients in Italian studies [5, 6]. However, the rate of Cp positivity varies between geographical regions and also between studies from the same country [7, 8]. A report from Korea showed that the Cp DNA detection rate from paraffin-embedded tissues was 79 % in 33 OAL cases, similar to reports from Italy [9, 10].
For patients with localized OAL, radiotherapy confers a high control rate with long-term efficacy. However, radiation to the involved eye can result in complications, including cataract (30–50 %), xerophthalmia (20–40 %), and retinopathy (2 %) [1, 11, 12]. Other options, such as single-agent chemotherapy, immunotherapy with monoclonal anti-CD20 antibody, and antibiotic therapy, have been studied in OAL [1, 13]. Pilot and extended multicenter trials of doxycycline treatment to eradicate Cp have been reported by Ferreri et al. [14, 15]. These authors recently published efficacy and safety data of doxycycline treatment of 47 newly diagnosed OAL patients in an international phase II trial. After a median follow-up of 37 months, the 5-year progression-free survival (PFS) was 55 ± 9 % [16].
We previously reported the efficacy of first-line therapy with doxycycline in 38 patients with newly diagnosed OAL at our institution. After a median follow-up of 26.4 months, doxycycline treatment resulted in a 3-year time-to-treatment failure rate of 84 % [9]. In the current study, we extended the follow-up duration in a larger number of patients who were newly diagnosed with OAL of the MALT type and treated up-front with doxycycline.
Patients and methods
Patients
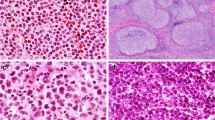
Doxycycline was given as a first-line treatment to 90 patients who had been newly diagnosed with ocular adnexal marginal zone B cell lymphoma at the Seoul National University Hospital between January 2004 and December 2012. Any patient who received combination chemotherapy or radiotherapy in advance was excluded. All study patients were classified according to the American Joint Committee on Cancer (AJCC) tumor, nodes, and metastases (TNM)-based staging system, with the T classification categorized as follows: T1, conjunctival involvement; T2, involvement of the orbit; T3, infiltration of preseptal eyelid tissues; and T4, extension beyond orbit to adjacent structures, such as bone and brain (Fig. 1). This study was approved by the Institutional Review Board at Seoul National University Hospital (H-1403-003-560).
Treatments and response evaluation
Each patient was treated with one or two cycles of doxycycline (100 mg bid) for 3 weeks. Doxycycline outcomes were evaluated in patients who were followed for more than 6 months after completion of therapy. Medical history, ophthalmologic examination with anterior segment photography by experienced ophthalmologists, orbital magnetic resonance imaging (MRI) or computerized tomography (CT) scan of the lesion, physical examinations, complete blood count, and chemical tests including lactate dehydrogenase (LDH) were performed and recorded at baseline. An ophthalmologic examination, complete blood count, chemistry including LDH, and radiologic examination (CT or MRI) were performed every 6 months. Patients who progressed after doxycycline treatment received second-line treatment. Second-line treatment was cyclophosphamide, vincristine, and prednisolone (CVP) combination chemotherapy and/or radiotherapy (30.6 Gy), as decided by the clinician and patient. Thirty-one patients who received second-line therapy assessed response using modified international workshop criteria [17]. Response was defined as follows: complete remission (CR), complete disappearance of all detectable ophthalmic and radiographic evidence of disease and eye-related symptoms if present before therapy; partial remission (PR), 50 % or more decrease in the sum of the product of the greatest diameters; progressive disease (PD), any new lesion or 50 % or more increase from the smallest sum of the product of the greatest diameters; stable disease (SD), an absence of CR, PR, and PD.
Statistical analysis
The primary study end point was PFS, defined as the time elapsed between doxycycline initiation and tumor progression or censoring of patients at the date of last follow-up. All of the study patients were alive at the last follow-up. Survival curves for PFS were determined by the Kaplan-Meier method [18] and compared with results of log-rank tests. Univariate and multivariate analyses of PFS according to clinical factors were performed with a Cox proportional hazards regression model [19]. Absolute lymphocyte and neutrophil counts within 1 week before doxycycline treatment were used to define lymphocytosis and neutrophilia. Lymphocytosis or neutrophilia was defined as an absolute lymphocyte or neutrophil count higher than the respective median value. Two-sided P values <0.05 were considered to indicate statistical significance. All statistical analyses were performed using SPSS statistics software (version 20) (IBM Corp.; Chicago, IL, USA).
Results
Patients
Clinical characteristics of the 90 study patients are listed in Table 1. The median age at diagnosis was 48 years (range, 21–71 years) with a male-to-female ratio of 1:1.6, and all patients had Eastern Cooperative Oncology Group (ECOG) performance status 0–1. The most common site of presentation was conjunctiva (82 %), followed by orbit (13 %), eyelid (3 %), and lacrimal gland (2 %). Serum LDH was elevated in 16 % of patients, and only one patient had B symptoms at diagnosis. Two cycles of doxycycline were administered in 80 % of the patients. Measurable lesions were seen on CT or MRI in 42 % of patients. According to the TNM staging, 62 patients (69 %) were T1N0M0, 22 (24 %) were T2N0-2 M0, 5 (6 %) were T3N0-2 M0, and 1 (1 %) was T4N0M0. Median absolute lymphocyte and neutrophil count was 1.95 × 109/L and 3.01 × 109/L, respectively.
Treatment outcomes
All patients were alive at the time of analysis (May 2013). During the median follow-up period of 40.5 months, median PFS was not reached. The 5-year PFS was 60.9 % by intent-to-treat analysis. Twenty-four patients (27 %) responded to doxycycline and 34 patients achieved stable disease (Table 2). Thirty-one patients (34 %) showed local treatment failure without systemic dissemination. In these patients, median time to treatment failure after doxycycline treatment was 4 months (range, 1–56 months). There was no serious adverse event reported during doxycycline therapy. Thirty-one patients received salvage treatment. Twenty patients who received CVP after doxycycline failure showed complete response in six patients, partial response in 11 patients, and SD in three patients, without any PD. Nine patients who progressed after doxycycline and two patients who had SD with intolerable eye symptoms received radiotherapy. Every patient achieved response, with CR in 9 and PR in 2 patients (Table 3). More patients received CVP chemotherapy in patients with >T1 stage than patients with stage T1. The 5-year PFS in patients treated with salvage radiotherapy and/or CVP was 100 %. Examination of PFS according to TNM staging showed that median PFS in T1N0M0 patients was significantly better than in patients at more advanced T stages (median survival not reached vs. 20 months, log-rank P < 0.0001; see Fig. 2).
Survival analysis and predictive factors
We further analyzed PFS according to clinical variables, such as gender, age, LDH level, laterality, doxycycline cycle, lymphocytosis, neutrophilia, and TNM staging. In univariate analysis, doxycycline cycle and TNM staging were statistically significant (Table 4). There was no significant association between number of cycles and TNM staging (chi-square, P = 0.227). In multivariate analysis, the hazard ratio (HR) of patients with a more advanced stage than T1N0M0 compared to patients with T1N0M0 was 4.35 (95 % confidence interval [CI], 2.03–9.32; P < 0.001), and the HR of two cycles of doxycycline treatment compared to a single cycle was 0.31 (95 % CI, 0.14–0.60; P = 0.004) (Table 4).
Discussion
In this long-term large cohort study, almost two-thirds of patients with OAL remained progression-free 5 years after doxycycline treatment. In addition, none of the patients had disease progression with salvage chemotherapy and/or radiotherapy after doxycycline failure. Our results suggest that patients with low-grade localized OAL can be initially treated with doxycycline without serious complications or compromising the salvage treatment after progression or doxycycline failure. This finding is similar to that of a phase-II trial that reported a 5-year PFS rate of approximately 68 % in 14 patients who achieved Cp eradication after doxycycline treatment of 100 mg twice daily for 3 weeks [16]. The PFS rate in this study is comparable to the results from first-line CVP chemotherapy at our institution [20]. Because our previous data showed that patients who received two cycles of treatment had a higher response rate and rapid response [9], we administered two cycles of doxycycline 100 mg twice daily for 3 weeks as standard in this study. However, patients who complained of eye-related symptoms consistently, or those who showed early disease progression after only one cycle of doxycycline, received salvage therapy in advance.
The geographical difference in Cp infection rate is an important factor for interpretation of discrepancies between results. The reported Cp infection rate is higher in Korea (79 %) and Italy (87 %) than in Austria (54 %) [7]. However, Cp DNA was not detected in OAL specimens in Japanese patients [21, 22]. The lack of benefit of one-cycle doxycycline treatment in a blinded study of 11 Austrian patients may have resulted from the low Cp infection and eradiation rates [23]. Recently, Ferreri et al. showed that Cp eradication was associated with better response rate and 5-year PFS [16].
The Ann Arbor staging system cannot differentiate patients who could benefit more from doxycycline treatment. Therefore, we investigated study patients according to the TNM staging system developed by the American Joint Committee on Cancer [24]. Feasibility of TNM staging was previously studied in 50 Korean patients, and the T1N0M0 group showed a higher 3-year PFS than patients with a more advanced stage [25]. In this study, TNM staging was a significant predictive factor for PFS in univariate and multivariate analysis. This suggests that patients who are staged as T1N0M0 might be good candidates for up-front doxycycline treatment.
All of the patients who failed doxycycline received radiotherapy and/or chemotherapy as salvage treatment. The response rate in these patients was 100 % for radiotherapy and 85 % for CVP. The efficacy of salvage radiotherapy was comparable to that of first-line radiotherapy from previous reports [1], although the response rate of salvage CVP chemotherapy seems to be inferior to that of first-line CVP that we previously reported [20]. There can be a potential bias in efficacy of CVP because the patients who had >T1 disease received more CVP than those who had T1 disease.
It is known that younger patients (mean age 45.9 years) are predominantly affected in Korea [3], and the median age in our study (48 years) was very close to this mean value. Older age has been reported to be a poor prognostic factor for disease-free survival and overall survival in patients with OAL [4, 26, 27]. As younger patients have a better prognosis, a treatment modality that is safe and less complicated, such as doxycycline, could be preferable to radiotherapy or chemotherapy as a first-line therapy. A recent review article has discussed clarithromycin for targeting the Cp infection in patients with OAL; however, the data is limited [28].
Although Cp DNA was not examined in this study, the prevalence of Cp infection has been reported to be approximately 60–80 % in Korean patients with OAL, including results from our institution [9, 10]. For future studies, the feasibility of Cp DNA detection in small biopsy samples should be considered [29].
In conclusion, first-line treatment with doxycycline in patients with localized OAL of MALT is effective without causing serious toxicities. Especially, patients of T1N0M0 stage could be considered good candidates for up-front doxycycline treatment. Patients who failed after doxycycline therapy were successfully salvaged with CVP chemotherapy and/or radiotherapy without compromising the long-term outcomes.
References
Stefanovic A, Lossos IS (2009) Extranodal marginal zone lymphoma of the ocular adnexa. Blood 114(3):501–510. doi:10.1182/blood-2008-12-195453
Moslehi R, Devesa SS, Schairer C, Fraumeni JF Jr (2006) Rapidly increasing incidence of ocular non-Hodgkin lymphoma. J Natl Cancer Inst 98(13):936–939. doi:10.1093/jnci/djj248
Cho EY, Han JJ, Ree HJ, Ko YH, Kang YK, Ahn HS, Ahn SD, Park CJ, Huh J (2003) Clinicopathologic analysis of ocular adnexal lymphomas: extranodal marginal zone b-cell lymphoma constitutes the vast majority of ocular lymphomas among Koreans and affects younger patients. Am J Hematol 73(2):87–96. doi:10.1002/ajh.10332
Meunier J, Lumbroso-Le Rouic L, Vincent-Salomon A, Dendale R, Asselain B, Arnaud P, Fourquet A, Desjardins L, Plancher C, Validire P, Chaoui D, Levy C, Decaudin D (2004) Ophthalmologic and intraocular non-Hodgkin’s lymphoma: a large single centre study of initial characteristics, natural history, and prognostic factors. Hematol Oncol 22(4):143–158. doi:10.1002/hon.741
Ferreri AJ, Guidoboni M, Ponzoni M, De Conciliis C, Dell’Oro S, Fleischhauer K, Caggiari L, Lettini AA, Dal Cin E, Ieri R, Freschi M, Villa E, Boiocchi M, Dolcetti R (2004) Evidence for an association between Chlamydia psittaci and ocular adnexal lymphomas. J Natl Cancer Inst 96(8):586–594
Dolcetti R, Serraino D, Dognini G, Govi S, Crocchiolo R, Ghia P, Pasini E, Ponzoni M, Talamini R, De Paoli P, Doglioni C, Ferreri AJ (2012) Exposure to animals and increased risk of marginal zone B-cell lymphomas of the ocular adnexae. Br J Cancer 106(5):966–969. doi:10.1038/bjc.2012.2
Collina F, De Chiara A, De Renzo A, De Rosa G, Botti G, Franco R (2012) Chlamydia psittaci in ocular adnexa MALT lymphoma: a possible role in lymphomagenesis and a different geographical distribution. Infect Agents Cancer 7:8. doi:10.1186/1750-9378-7-8
Husain A, Roberts D, Pro B, McLaughlin P, Esmaeli B (2007) Meta-analyses of the association between Chlamydia psittaci and ocular adnexal lymphoma and the response of ocular adnexal lymphoma to antibiotics. Cancer 110(4):809–815. doi:10.1002/cncr.22843
Kim TM, Kim KH, Lee MJ, Jeon YK, Lee SH, Kim DW, Kim CW, Kim IH, Khwarg SI, Heo DS (2010) First-line therapy with doxycycline in ocular adnexal mucosa-associated lymphoid tissue lymphoma: a retrospective analysis of clinical predictors. Cancer Sci 101(5):1199–1203. doi:10.1111/j.1349-7006.2010.01502.x
Yoo C, Ryu MH, Huh J, Park JH, Kang HJ, Ahn HS, Lee Y, Kim MJ, Lee H, Kim TW, Chang HM, Lee JL, Kang YK (2007) Chlamydia psittaci infection and clinicopathologic analysis of ocular adnexal lymphomas in Korea. Am J Hematol 82(9):821–823. doi:10.1002/ajh.20962
Cho WK, Lee SE, Paik JS, Cho SG, Yang SW (2013) Risk potentiality of frontline radiotherapy associated cataract in primary ocular adnexal mucosa-associated lymphoid tissue lymphoma. Korean J Ophthalmol 27(4):243–248. doi:10.3341/kjo.2013.27.4.243
De Cicco L, Cella L, Liuzzi R, Solla R, Farella A, Punzo G, Tranfa F, Strianese D, Conson M, Bonavolonta G, Salvatore M, Pacelli R (2009) Radiation therapy in primary orbital lymphoma: a single institution retrospective analysis. Radiat Oncol 4:60. doi:10.1186/1748-717X-4-60
Decaudin D, de Cremoux P, Vincent-Salomon A, Dendale R, Rouic LL (2006) Ocular adnexal lymphoma: a review of clinicopathologic features and treatment options. Blood 108(5):1451–1460. doi:10.1182/blood-2006-02-005017
Ferreri AJ, Ponzoni M, Guidoboni M, De Conciliis C, Resti AG, Mazzi B, Lettini AA, Demeter J, Dell’Oro S, Doglioni C, Villa E, Boiocchi M, Dolcetti R (2005) Regression of ocular adnexal lymphoma after Chlamydia psittaci-eradicating antibiotic therapy. J Clin Oncol 23(22):5067–5073. doi:10.1200/JCO.2005.07.083
Ferreri AJ, Ponzoni M, Guidoboni M, Resti AG, Politi LS, Cortelazzo S, Demeter J, Zallio F, Palmas A, Muti G, Dognini GP, Pasini E, Lettini AA, Sacchetti F, De Conciliis C, Doglioni C, Dolcetti R (2006) Bacteria-eradicating therapy with doxycycline in ocular adnexal MALT lymphoma: a multicenter prospective trial. J Natl Cancer Inst 98(19):1375–1382. doi:10.1093/jnci/djj373
Ferreri AJ, Govi S, Pasini E, Mappa S, Bertoni F, Zaja F, Montalban C, Stelitano C, Cabrera ME, Giordano Resti A, Politi LS, Doglioni C, Cavalli F, Zucca E, Ponzoni M, Dolcetti R (2012) Chlamydophila psittaci eradication with doxycycline as first-line targeted therapy for ocular adnexae lymphoma: final results of an international phase II trial. J Clin Oncol 30(24):2988–2994. doi:10.1200/JCO.2011.41.4466
Cheson BD, Horning SJ, Coiffier B, Shipp MA, Fisher RI, Connors JM, Lister TA, Vose J, Grillo-Lopez A, Hagenbeek A, Cabanillas F, Klippensten D, Hiddemann W, Castellino R, Harris NL, Armitage JO, Carter W, Hoppe R, Canellos GP (1999) Report of an international workshop to standardize response criteria for non-Hodgkin’s lymphomas. NCI Sponsored International Working Group. J Clin Oncol 17(4):1244
Kaplan EL, Meier P (1958) Nonparametric-estimation from incomplete observations. J Am Stat Assoc 53(282):457–481. doi:10.2307/2281868
Cox DR (1972) Regression models and life-tables. J R Stat Soc Ser B 34(2):187–220
Song EK, Kim SY, Kim TM, Lee KW, Yun T, Na II, Shin H, Lee SH, Kim DW, Khwarg SI, Heo DS (2008) Efficacy of chemotherapy as a first-line treatment in ocular adnexal extranodal marginal zone B-cell lymphoma. Ann Oncol 2:242–246. doi:10.1093/annonc/mdm457
Daibata M, Nemoto Y, Togitani K, Fukushima A, Ueno H, Ouchi K, Fukushi H, Imai S, Taguchi H (2006) Absence of Chlamydia psittaci in ocular adnexal lymphoma from Japanese patients. Br J Haematol 132(5):651–652. doi:10.1111/j.1365-2141.2005.05943.x
Liu YC, Ohyashiki JH, Ito Y, Iwaya K, Serizawa H, Mukai K, Goto H, Usui M, Ohyashiki K (2006) Chlamydia psittaci in ocular adnexal lymphoma: Japanese experience. Leuk Res 30(12):1587–1589. doi:10.1016/j.leukres.2006.01.015
Grunberger B, Hauff W, Lukas J, Wohrer S, Zielinski CC, Streubel B, Chott A, Raderer M (2006) ‘Blind’ antibiotic treatment targeting Chlamydia is not effective in patients with MALT lymphoma of the ocular adnexa. Ann Oncol 3:484–487. doi:10.1093/annonc/mdj143
Finger PT, th Edition A-UOOTF (2009) The 7th edition AJCC staging system for eye cancer: an international language for ophthalmic oncology. Arch Pathol Lab Med 133(8):1197–1198. doi:10.1043/1543-2165-133.8.1197
Lee SE, Paik JS, Cho WK, Choi BO, Lee SN, Jung SE, Park KS, Kang CS, Kim SH, Yang SW, Cho SG (2011) Feasibility of the TNM-based staging system of ocular adnexal extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma). Am J Hematol 86(3):262–266. doi:10.1002/ajh.21963
Coupland SE, Heimann H, Bechrakis NE (2004) Primary intraocular lymphoma: a review of the clinical, histopathological and molecular biological features. Graefes Arch Clin Exp Ophthalmol Albrecht Graefes Archiv Klin Exp Ophthalmol 242(11):901–913. doi:10.1007/s00417-004-0973-0
Martinet S, Ozsahin M, Belkacemi Y, Landmann C, Poortmans P, Oehlere C, Scandolaro L, Krengli M, Maingon P, Miralbell R, Studer G, Chauvet B, Marnitz S, Zouhair A, Mirimanoff RO (2003) Outcome and prognostic factors in orbital lymphoma: a Rare Cancer Network study on 90 consecutive patients treated with radiotherapy. Int J Radiat Oncol Biol Phys 55(4):892–898
Kiesewetter B, Raderer M (2013) Antibiotic therapy in nongastrointestinal MALT lymphoma: a review of literature. Blood 122(8):1350–1357. doi:10.1182/blood-2013-02-486522
Ponzoni M, Ferreri AJ, Guidoboni M, Lettini AA, Cangi MG, Pasini E, Sacchi L, Pecciarini L, Grassi S, Dal Cin E, Stefano R, Magnino S, Dolcetti R, Doglioni C (2008) Chlamydia infection and lymphomas: association beyond ocular adnexal lymphomas highlighted by multiple detection methods. Clin Cancer Res 14(18):5794–5800. doi:10.1158/1078-0432.CCR-08-0676
Acknowledgments
This study was supported by a grant from the Innovative Research Institute for Cell Therapy, Republic of Korea (A062260).
Conflict of interest
The authors indicated no potential conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Han, J.J., Kim, T.M., Jeon, Y.K. et al. Long-term outcomes of first-line treatment with doxycycline in patients with previously untreated ocular adnexal marginal zone B cell lymphoma. Ann Hematol 94, 575–581 (2015). https://doi.org/10.1007/s00277-014-2240-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-014-2240-8