Abstract
Both-side synchronous involvement has been reported to account for 7–24% of ocular adnexal marginal zone lymphoma (OAML). We conducted a retrospective analysis to identify the clinical features and treatment outcomes of synchronous bilateral OAML (SB-OAML) by treatment modality. We analyzed patients with a histologic diagnosis of SB-OAML, excluding metachronous bilateral involved OAML. We enrolled a total of 95 patients for this analysis, 36 males and 59 females; the median patient age was 42 years (range 16–77 years). Eleven (11.6%) patients had been treated with chemotherapy or chemo-immunotherapy (eight R-CVP, two CVP, and one R-CHOP). The median number of treatments was 6 (range 6–8); there were 9 complete responses (CRs; 81.8%) and 2 partial responses (PRs; 18.2%). Nearly all patients (88.4%) received radiotherapy in both eyes, and the median radiation dose was 27 Gy (range 20–40 Gy) to each eye; 68 CRs (80.9%) and 14 PRs (16.7%) were achieved. Ten-year progression-free survival (PFS) and overall survival (OS) rates were 79.8 and 91.1%, respectively. Radiotherapy continued to be an independent prognostic marker, with the hazard of progression (P = 0.036). Eleven patients (13.1%) had surgery for cataract treatment during follow-up, and patients who received low-dose radiation (< 30.3 Gy) experienced fewer cataract operations. SB-OAML was predominantly observed in young females, and they had good response and prognosis regardless of treatment modalities. Low-dose radiotherapy to both eyes showed a tendency of longer PFS than did chemotherapy and could decrease cataract operations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non-Hodgkin’s lymphomas constitute one half of all orbital malignancies [1, 2]. Five to 15% of all extranodal lymphomas arise in the ocular adnexa: the conjunctiva, the lachrymal gland, the ocular muscles, the orbital fat, the eyelid, and the lachrymal sac [2, 3]. Ocular adnexal marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT) type (OAML) is the most common lymphoma category in these anatomical structures; OAML accounts for more than 90% of ocular lymphomas [4,5,6]. Unlike the datasets from other countries, Korean studies found higher rates of conjunctival involvement [4]. OAMLs present as slowly enlarging lesions and have prolonged survival rates [7,8,9].
OAML is generally responsive to radiation therapy, and therefore, patients with limited-stage disease usually undergo radiation therapy. However, limited-stage OAML has been reported to have a recurrence rate of 25% following radiotherapy [2], and the risk of recurrence is higher when the disease involves both eyes or spreads beyond the conjunctiva [10,11,12,13]. In addition, the target volume of irradiation for conjunctiva-only disease is the whole conjunctiva, and the risk of cataract can be reduced with lens shielding; however, for disease extending beyond the conjunctiva, the whole orbit is generally covered without lens shielding, and thus the risk of cataract can be considerable [12, 14, 15], In addition, the target volume of irradiation for conjunctiva-only disease is the whole conjunctiva and the risk of cataract can be reduced with lens shielding, but for disease extending beyond the conjunctiva, the whole orbit is generally covered without lens shielding so that the risk of cataract can be considerable [16,17,18]. Because of the rarity of the disease and its responsiveness to radiation therapy, only a few trials of systemic chemotherapy or chemo-immunotherapy as a frontline treatment have been conducted in OAML patients. One retrospective study demonstrated the efficacy of combination chemotherapy with cyclophosphamide, vincristine, and prednisolone (CVP) for the frontline treatment of limited-stage OAML [19]. Recently, rituximab has been used to treat OAML, but rituximab monotherapy did not demonstrate adequate efficacy, with frequent early and often distant relapse [20]. These observations suggested the need for a combination of rituximab and conventional cytotoxic chemotherapy to ensure long-term disease control. Prospective trials using rituximab-containing chemo-immunotherapy were conducted for extranodal marginal zone B cell lymphoma, including the MALT-2008-01 and IELSG-19 trials, but these studies enrolled MALT lymphoma patients in various stages and with tumors at various sites [21,22,23].
Researchers observed bilateral involvement in 5–20% of OAML patients in the reported literature [4, 17], but either these authors did not analyze the associations between bilateral involvement and clinical outcomes or their results did not have significant statistical power to show these associations due to the small number of analyzed cases. Only one recently reported large-scale study with long-term follow-up of OAML demonstrated that bilateral involvement was an independent clinical variable associated with inferior outcomes in univariate analysis [8].
Therefore, in this study, we conducted retrospective analyses of synchronous bilateral OAML (SB-OAML) in order to identify its clinical features, prognostic factors, and side effects related to treatment as well as which treatment modality was effective for disease control.
Patients and methods
Patients and data
Eligible patients for this retrospective analysis were initially diagnosed with MZL in accordance with the REAL and WHO classification criteria. Unified case report forms were provided to participating institutions. Because our study was regarding bilaterally involved OAML, all of the patients recruited into this study had to have their diagnoses pathologically confirmed on biopsy. In addition, we excluded patients who had sequentially detected OAML in the contralateral eye after initial treatment for metachronous bilateral involvement. We also excluded patients who had been treated with doxycycline only or had watchful wait status. The collected data included age, gender, performance status, stage according to the Ann Arbor staging system, location of primary involvement, presence of B symptoms, hemoglobin, albumin, initial date of diagnosis, treatment modality utilized, response to treatment, and side effects. For the evaluation of efficacy, baseline at the diagnosis, a contrast-enhanced magnetic resonance imaging (MRI) scan, or computerized tomography (CT) scan and ophthalmic examination were performed. Subsequently, the same imaging study and ophthalmic exam were repeated for response assessment after initial treatment. We also obtained data regarding time to relapse, salvage treatment modality, and response and survival rates of salvage treatment.
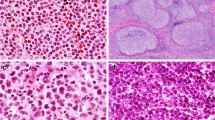
Histology
The diagnosis of MZL was based on the characteristic histologic findings described in the WHO classifications and immunohistochemical staining for CD20 and CD3. In cases in which it was difficult to exclude other low-grade B cell lymphomas, immunohistochemical studies for CD5, CD10, CD23, cyclin D1, BCL6, and Ki-67 were conducted. Because MZL is commonly accompanied by reactive hyperplasia, a PCR-based gene rearrangement study for the IgH gene was conducted when necessary.
Statistical analysis
We compared categorical variables in the two groups via χ2 tests or Fisher’s exact tests, considering P less than 0.05 statistically significant, and all P values corresponded to two-sided significance tests. We estimated overall survival (OS) and progression-free survival (PFS) via the Kaplan-Meier product-limit method. We calculated PFS from the date on which treatment began after relapse to the date on which the disease progression was recognized or the date of death or the date of the final follow-up visit, and we measured OS from the date of relapse to the date of death or the date of the final follow-up visit. We compared survival rates for statistical differences via log-rank analysis and used a Cox regression model for multivariate analysis at P < 0.05 in the univariate (by log-rank test) analysis of OS and PFS. For the numerical variables, we performed receiver operating characteristic (ROC) analysis to estimate the point for optimal sensitivity and specificity toward the progression of MZL or the radiation dosage cutoff point to cataract operation. We conducted all analyses using Statistical Package for the Social Sciences (SPSS) version 20.0 for Windows.
Results
Patients’ characteristics
We enrolled a total of 95 patients in this analysis from 9 institutions in Korea, 36 males and 59 females; the median patient age was 42 years (range 16–77 years). Except for one patient, all patients had 0 or 1 on the ECOG performance status scale. Regional lymph node (LN) enlargement was observed in 13 patients (13.7%), and not all patients presented with B symptoms; one patient had elevated LDH. The low-risk and low- to intermediate-risk rates by IPI were 61.1 and 33.7%, respectively (Table 1).
Treatment modalities and survivals
Eighty-four (88.4%) patients received ocular radiotherapy in both eyes. And among these, five were additionally treated with doxycycline; the median radiation dose was 27 Gy (range 20–40 Gy) to each eye (Table 2). Patients achieved 68 complete responses (CRs; 80.9%) and 14 partial responses (PRs; 16.7%). Eleven (11.6%) patients were treated with chemotherapy or chemo-immunotherapy (8 R-CVP, 2 CVP, and 1 R-CHOP), and two patients who received R-CVP treatment had an additional two cycles of single-maintenance rituximab. The median number of chemotherapy or chemo-immunotherapy treatments was 6 (range 6–8), and there were 9 CRs (81.8%) and 2 PRs (18.2%).
Five-year PFS and OS rates were 91.5 and 100%, and 10-year PFS and OS rates were 79.8 and 91.1%, both respectively (Figs. 1 and 2). In the univariate analysis of potential prognostic markers, older age (≥60) was shown to be a significant predictor of PFS (hazards ratio [HR] 8.414, 95% confidence interval [CI] 2.358–30.028, P = 0.001; Fig. 3). Furthermore, radiotherapy was also a better prognostic factor for PFS than was chemotherapy (HR 0.067, 95% CI 0.009–0.512, P = 0.009; Fig. 4). Other candidate variables such as gender, LN enlargement, serum albumin, hemoglobin, and non-conjunctival lesion were not prognostic in our population (Table 3). In multivariable analysis, radiotherapy continued to be an independent prognostic marker, with the hazard of progression (P = 0.036).
Risk analysis of cataract operation
Among the first-line both-eye radiotherapy patients (n = 84), 11 patients (13.1%) had been operated on for cataract treatment. To identify the optimal prognostic marker according to its sensitivity and specificity toward the risk of cataract operation, we performed ROC curve analysis according to radiation dose. The analysis generated a cutoff radiation dose of 30.3 Gy (sensitivity 90.9%, specificity 66.7%, AUC 0.658, 95% CI 0.505–0.811, P = 0.049).
Discussion
In this analysis, we observed that patients with SB-OAML had good response to treatments and good survival rates. Radiotherapy to both eyes especially showed longer response duration and less relapse risk than chemotherapy.
SB-OAML has been reported to occur in 5–20% of populations in large-scale ocular adnexal lymphoma reports [4, 17]. Like OAML reports, in our study, SB-OAML had been observed younger and female predominant clinical feature [8, 24, 25]. Researchers have suggested a number of theories for the bilateral involvement of OAML, such as common bacterial or chlamydia infection, autoimmunity, Sjögren’s syndrome in same-organ mucosa, and cytogenetic changes [9, 26]. The authors of one study demonstrated that bilateral lesions of adnexal lymphoma shared clonality between lesions [27].
According to recent suggested MALT-International prognostic index(IPI) model [28], components of MALT-IPI were age > 70, LDH > upper normal limit, and stage III/IV. In our study, all patients had limited stage, just 1 elevated LDH, and 5 patients were > 70. Therefore, MALT-IPI could not be applied to our research.
SB-OAML radiotherapy results have not yet been reported. Generally, radiotherapy results in a high rate of local control that ranges from 85 to 100% [9]; in one meta-analysis, the majority of the 503 study patients with stage 1E disease achieved local control. CR rates ranged from 52 to 93%, and the 5-year, systemic-free relapse rates usually exceeded 90%. Overall, systemic relapses occurred in 31 study patients (6.2%), ranging from a low rate of 2.2% (median follow-up of 32 months) to a high rate of 16.8% (median follow-up of 5.9 years). In our study, radiotherapy to both eyes had a 97.6% response rate, 5-year PFS of 86.2%, and OS of 96.3%. Radiotherapy for bilateral OAML results was comparable with those from prior-stage IE OAML radiotherapy.
Radiotoxicity also accompanies good response to radiotherapy; early radiotherapy toxicity is usually manageable and consists of cutaneous or conjunctival reactions, whereas long-term complications, observed in up to 50% of patients, included cataract formation (30–50%) and xerophthalmia (20–40%) [29]. In our observation, incidence of cataract operation was 13% of radiated patients, lower than that in prior reports. Because cataract is a late-toxicity result of radiotherapy, the low cataract incidence in our review might have been caused by our short follow-ups; longer-term follow-ups are needed to obtain more precise incidence of cataract operations. Although radiation doses over 30.6 Gy showed better PFS than did low-dose radiation for PFS in primary OAML in long-term follow-up data [8], lower-dose radiotherapy from 24 to 25 Gy in conventional daily fractions is suggested for reducing radiotoxicity [30,31,32,33]. The dose recommended for MZLs by the National Comprehensive Cancer Network is 24 to 30 Gy, and our data also showed that patients who received less than 30.3 Gy of radiotherapy had fewer cataract operations. Furthermore, ultra-low-dose (two successive fractions of 2 Gy) radiotherapy for definitive management of ocular adnexal B cell lymphoma was reported that associated with high response rates and minimal toxic effects and is much shorter in duration and cost [34, 35].
Clinical trials of first use of rituximab-containing chemo-immunotherapy have been introduced to avoid radiotoxicity. Recent studies have evaluated combination regimens consisting of rituximab plus cytotoxic chemotherapeutic agents for treating patients with MALT lymphoma in various sites and in stages I–IV and have shown promising results [21,22,23]. A previous phase II study [21], with rituximab plus bendamustine in patients with MALT lymphoma, reported a CR rate of 100% and a 4-year PFS of 91% in non-gastric disease. In another previous phase III study [22], the IELSG-19, rituximab plus chlorambucil for extranodal marginal zone B cell lymphoma showed a CR rate of 78% and 5-year PFS of 71%. R-CVP chemotherapy for advanced stage MZL achieved CR of 60% and PR of 27.5%, and the estimated 3-year PFS and OS rates were 59.5 and 95.0%, respectively [23]. With the first-line R-CVP regimen for OAML, the cumulative complete response achievement was 93.9%. Progression-free survival and overall survival at 4 years were 90.3 and 100%, respectively [36]. In our report, chemotherapy showed poorer PFS than did radiotherapy (P = 0.049). However, because of the small number of chemotherapy-treated patients and the limitations of a retrospective study—the potential bias it might have generated in choosing therapies and influencing outcome and the regimens administered do not really rate among the more effective regimens currently applied especially in view of the population, as most patients were young and fit and would have tolerated therapy such as a rituximab and bendamustine combination. We are not certain about recommending radiotherapy for SB-OAML as a first-choice treatment modality.
Including “watchful wait,” several modalities could be an option for first-line treatment for SB-OAML. Not only chemotherapy or definitive radiotherapy, antibiotics such as doxycycline for the chlamydia infection and radio-immunotherapy are under investigation.
In conclusion, we observed SB-OAML mostly in relatively young and female patients, and nearly all of them responded to radiotherapy or chemo-immunotherapy. Patients with SB-OAML achieved prolonged PFS and OS; for instance, radiotherapy had a better PFS than did chemotherapy. Lower-dose radiotherapy also reduced the incidence of cataract operations.
References
Margo CE, Mulla ZD (1998) Malignant tumors of the orbit. Analysis of the Florida Cancer registry. Ophthalmology 105:185–190
Fung CY, Tarbell NJ, Lucarelli MJ, Goldberg SI, Linggood RM, Harris NL, Ferry JA (2003) Ocular adnexal lymphoma: clinical behavior of distinct World Health Organization classification subtypes. Int J Radiat Oncol Biol Phys 57:1382–1391
Moslehi R, Coles FB, Schymura MJ (2011) Descriptive epidemiology of ophthalmic and ocular adnexal non-Hodgkin’s lymphoma. Expert Rev Ophthalmol 6:175–180
Oh DE, Kim YD (2007) Lymphoproliferative diseases of the ocular adnexa in Korea. Arch Ophthalmol 125:1668–1673
Cho EY, Han JJ, Ree HJ, Ko YH, Kang YK, Ahn HS, Ahn SD, Park CJ, Huh J (2003) Clinicopathologic analysis of ocular adnexal lymphomas: extranodal marginal zone b-cell lymphoma constitutes the vast majority of ocular lymphomas among Koreans and affects younger patients. Am J Hematol 73:87–96
Yoon JS, Ma KT, Kim SJ, Kook K, Lee SY (2007) Prognosis for patients in a Korean population with ocular adnexal lymphoproliferative lesions. Ophthal Plast Reconstr Surg 23:94–99
Oh SY, Ryoo BY, Kim WS, Park YH, Kim K, Kim HJ, Kwon JM, Lee J, Ko YH, Ahn YC, Oh SJ, Lee SI, Kim HJ, Kwon HC, Bang SM, Kim JH, Park J, Lee SS, Kim HY, Park K (2007) Nongastric marginal zone B-cell lymphoma: analysis of 247 cases. Am J Hematol 82:446–452
Desai A, Joag MG, Lekakis L, Chapman JR, Vega F, Tibshirani R, Tse D, Markoe A, Lossos IS (2017) Long-term course of patients with primary ocular adnexal MALT lymphoma: a large single-institution cohort study. Blood 129:324–332
Guffey Johnson J, Terpak LA, Margo CE, Setoodeh R (2016) Extranodal marginal zone B-cell lymphoma of the ocular adnexa. Cancer Control 23:140–149
Nam H, Ahn YC, Kim YD, Ko Y, Kim WS (2009) Prognostic significance of anatomic subsites: results of radiation therapy for 66 patients with localized orbital marginal zone B cell lymphoma. Radiother Oncol 90:236–241
Lee SE, Paik JS, Cho WK, Choi BO, Lee SN, Jung SE, Park KS, Kang CS, Kim SH, Yang SW, Cho SG (2011) Feasibility of the TNM-based staging system of ocular adnexal extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma). Am J Hematol 86:262–266
Uno T, Isobe K, Shikama N, Nishikawa A, Oguchi M, Ueno N, Itami J, Ohnishi H, Mikata A, Ito H (2003) Radiotherapy for extranodal, marginal zone, B-cell lymphoma of mucosa-associated lymphoid tissue originating in the ocular adnexa: a multiinstitutional, retrospective review of 50 patients. Cancer 98:865–871
Stefanovic A, Lossos IS (2009) Extranodal marginal zone lymphoma of the ocular adnexa. Blood 114:501–510
Martinet S, Ozsahin M, Belkacemi Y et al (2003) Outcome and prognostic factors in orbital lymphoma: a rare cancer network study on 90 consecutive patients treated with radiotherapy. Int J Radiat Oncol Biol Phys 55:892–898
Raderer M, Streubel B, Woehrer S, Puespoek A, Jaeger U, Formanek M, Chott A (2005) High relapse rate in patients with MALT lymphoma warrants lifelong follow-up. Clin Cancer Res 11:3349–3352
Lee SW, Suh CO, Kim GE, Yang WI, Lee SY, Hahn JS, Park JO (2002) Role of radiotherapy for primary orbital lymphoma. Am J Clin Oncol 25:261–265
Woolf DK, Kuhan H, Shoffren O, Akinnawo EM, Sivagurunathan B, Boyce H, Plowman PN (2015) Outcomes of primary lymphoma of the ocular adnexa (orbital lymphoma) treated with radiotherapy. Clin Oncol 27:153–159
Harada K, Murakami N, Kitaguchi M, Sekii S, Takahashi K, Yoshio K, Inaba K, Morota M, Ito Y, Sumi M, Suzuki S, Tobinai K, Uno T, Itami J (2014) Localized ocular adnexal mucosa-associated lymphoid tissue lymphoma treated with radiation therapy: a long-term outcome in 86 patients with 104 treated eyes. Int J Radiat Oncol Biol Phys 88:650–654
Song EK, Kim SY, Kim TM et al (2008) Efficacy of chemotherapy as a first-line treatment in ocular adnexal extranodal marginal zone B-cell lymphoma. Annals of oncology : official journal of the European society for. Med Oncol 19:242–246
Ferreri AJ, Ponzoni M, Martinelli G, Muti G, Guidoboni M, Dolcetti R, Doglioni C (2005) Rituximab in patients with mucosal-associated lymphoid tissue-type lymphoma of the ocular adnexa. Haematologica 90:1578–1579
Salar A, Domingo-Domenech E, Panizo C, Nicolás C, Bargay J, Muntañola A, Canales M, Bello JL, Sancho JM, Tomás JF, Rodríguez MJ, Peñalver FJ, Grande C, Sánchez-Blanco JJ, Palomera L, Arranz R, Conde E, García M, García JF, Caballero D, Montalbán C, Grupo Español de Linfomas/Trasplante de Médula Ósea (GELTAMO) (2014) First-line response-adapted treatment with the combination of bendamustine and rituximab in patients with mucosa-associated lymphoid tissue lymphoma (MALT2008-01): a multicentre, single-arm, phase 2 trial. Lancet Haematol 1:e104–e111
Zucca E, Conconi A, Martinelli G, Bouabdallah R, Tucci A, Vitolo U, Martelli M, Pettengell R, Salles G, Sebban C, Guillermo AL, Pinotti G, Devizzi L, Morschhauser F, Tilly H, Torri V, Hohaus S, Ferreri AJM, Zachée P, Bosly A, Haioun C, Stelitano C, Bellei M, Ponzoni M, Moreau A, Jack A, Campo E, Mazzucchelli L, Cavalli F, Johnson P, Thieblemont C (2017) Final results of the IELSG-19 randomized trial of mucosa-associated lymphoid tissue lymphoma: improved event-free and progression-free survival with rituximab plus chlorambucil versus either chlorambucil or rituximab monotherapy. J Clin Oncol Off J Am Soc Clin Oncol 35:1905–1912
Kang HJ, Kim WS, Kim SJ, Lee JJ, Yang DH, Kim JS, Lee SR, Lee GW, Kim HJ, Kim HY, Oh SY, Kim HC, Eom HS, Chung J, Park J, Suh C, Ryoo BY (2012) Phase II trial of rituximab plus CVP combination chemotherapy for advanced stage marginal zone lymphoma as a first-line therapy: consortium for improving survival of lymphoma (CISL) study. Ann Hematol 91:543–551
Nam SW, Woo KI, Kim YD (2018) Characteristics of primary extranodal marginal zone B-cell lymphoma in Korea: conjunctiva versus other ocular adnexa. Br J Ophthalmol 102:502–508
Kiesewetter B, Lukas J, Kuchar A, Mayerhoefer ME, Streubel B, Lagler H, Müllauer L, Wöhrer S, Fischbach J, Raderer M (2014) Clinical features, treatment and outcome of mucosa-associated lymphoid tissue (MALT) lymphoma of the ocular adnexa: single center experience of 60 patients. PLoS One 9:e104004
Ferreri AJ, Dolcetti R, Du MQ et al (2008) Ocular adnexal MALT lymphoma: an intriguing model for antigen-driven lymphomagenesis and microbial-targeted therapy. Ann Oncol 19:835–846
Matsuo T, Ichimura K, Okada H, Shinagawa K, Fukushima K, Okano M, Otsuka M, Yoshino T (2010) Clonal analysis of bilateral, recurrent, or systemically multifocal ocular adnexal lymphoma. J Clin Exp Hematop 50:27–38
Thieblemont C, Cascione L, Conconi A, Kiesewetter B, Raderer M, Gaidano G, Martelli M, Laszlo D, Coiffier B, Lopez Guillermo A, Torri V, Cavalli F, Johnson PW, Zucca E (2017) A MALT lymphoma prognostic index. Blood 130:1409–1417
Sassone M, Ponzoni M, Ferreri AJ (2017) Ocular adnexal marginal zone lymphoma: clinical presentation, pathogenesis, diagnosis, prognosis, and treatment. Best Pract Res Clin Haematol 30:118–130
Yahalom J, Illidge T, Specht L, Hoppe RT, Li YX, Tsang R, Wirth A (2015) Modern radiation therapy for extranodal lymphomas: field and dose guidelines from the international lymphoma radiation oncology group. Int J Radiat Oncol Biol Phys 92:11–31
Kaushik M, Pulido JS, Schild SE, Stafford S (2012) Risk of radiation retinopathy in patients with orbital and ocular lymphoma. Int J Radiat Oncol Biol Phys 84:1145–1150
Tsang RW, Gospodarowicz MK, Pintilie M, Wells W, Hodgson DC, Sun A, Crump M, Patterson BJ (2003) Localized mucosa-associated lymphoid tissue lymphoma treated with radiation therapy has excellent clinical outcome. J Clin Oncol Off J Am Soc Clin Oncol 21:4157–4164
Stafford SL, Kozelsky TF, Garrity JA, Kurtin PJ, Leavitt JA, Martenson JA, Habermann TM (2001) Orbital lymphoma: radiotherapy outcome and complications. Radiother Oncol 59:139–144
Pinnix CC, Dabaja BS, Milgrom SA, Smith GL, Abou Z, Nastoupil L, Romaguera J, Turturro F, Fowler N, Fayad L, Westin J, Neelapu S, Fanale MA, Rodriguez MA, Hagemeister F, Lee HJ, Oki Y, Wang M, Samaniego F, Chi L, Esmaeli B (2017) Ultra-low-dose radiotherapy for definitive management of ocular adnexal B-cell lymphoma. Head Neck 39:1095–1100
Fasola CE, Jones JC, Huang DD, le QT, Hoppe RT, Donaldson SS (2013) Low-dose radiation therapy (2 Gy x 2) in the treatment of orbital lymphoma. Int J Radiat Oncol Biol Phys 86:930–935
Kim SY, Yang SW, Lee WS, Yang JW, Oh SY, Ahn HB, Yang DH, Park SK, Chang JH, Kim HJ, Lee MJ, Cho SG (2017) Frontline treatment with chemoimmunotherapy for limited-stage ocular adnexal MALT lymphoma with adverse factors: a phase II study. Oncotarget 8:68583–68590
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Oh, S.Y., Kim, W.S., Kang, HJ. et al. Treating synchronous bilateral ocular adnexal marginal zone lymphoma: the consortium for improving survival of lymphoma study. Ann Hematol 97, 1851–1857 (2018). https://doi.org/10.1007/s00277-018-3387-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-018-3387-5