Abstract
Dramatic progress in the treatment of childhood acute lymphoblastic leukemia (ALL) has been achieved during the last two decades in Western countries, where the 5-year event-free survival (EFS) rate has risen from 30 to 85 %. However, similarly high cure rates have not always been achieved in all centers in developing countries due to limited sources. We evaluated the treatment results of the ALL-Berlin–Frankfurt–Münster (BFM) 95 protocol as used between 1995 and 2009 in the pediatric hematology departments of two university hospitals. A retrospective analysis of 343 children newly diagnosed with ALL (M/F 200/143, median age 6.8 years) was performed. The overall survival (OS) and EFS according to age, initial leukocyte count, immunophenotype, chemotherapy responses (on days 8, 15, and 33), and risk groups were analyzed by Kaplan–Meier survival analysis. Median follow-up time was 6.4 years. Complete remission was achieved in 97 % of children. Five-year EFS and OS were found to be 78.4 and 79.9 %, respectively. Children younger than 6 years old had significantly better EFS and OS (83.7 and 85.2 %) than children aged ≥6 years (71.4 and 72.8 %). Adolescents achieved 63 % EFS and 65 % OS. Patients who had initial leukocyte counts of <20 × 109/L had better EFS and OS (82.2 and 84.6 %) than children with higher initial leukocyte counts (72.6 and 72.6 %). EFS for B-cell precursor and T-cell ALL was 81.5 and 66.7 %, respectively. Children with a good response to prednisolone on day 8 (87 %) achieved significantly better EFS and OS (81.2 and 81.9 % vs. 55.3 and 60.5 %). Children whose bone marrow on day 15 was in complete remission had higher EFS and OS (83.7 and 86.6.1 % vs. 56.4 and 61.5 %). Children in the standard-risk and medium-risk groups obtained statistically significantly higher EFS (95.5 and 82.7 %) and OS (97.7 and 82.3 %) compared to the high-risk group (EFS 56.3 %, OS 63.4 %). The relapse rate was 14.8 %. The median relapse time from diagnosis was 23.2 months. Death occurred in 69 of 343 patients (20.1 %). The major causes of death were infection and relapse. None of the patients died of drug-related toxicity. The ALL-BFM 95 protocol was applied successfully in these two centers. In developing countries in which minimal residual disease cannot be monitored, this protocol can still be used with high survival rates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute lymphoblastic leukemia (ALL) is the most common malignancy among children [1, 2]. Multimodal therapy and enhanced supportive care for ALL have led to significant improvements in survival rates over the last four decades, especially in developed countries. The 5-year overall survival rate in ALL has increased from 30 % in the 1960s to over 85 % in the 2000s [3]. Great success has been achieved in ALL treatment by using well-designed, cooperative, carefully controlled, and innovative clinical protocols. Developments in the understanding of the immunobiology of ALL and better identification of prognostic factors have resulted in better definition of risk groups and the tailoring of therapy [4–6]. Furthermore, the provision of enhanced supportive care with better control of infections, presence of adequate numbers of skilled health care personnel, immediate supply of medications and blood products, and psychosocial support to patients and their families are important contributors to better survival rates [7, 8].
The ALL-Berlin–Frankfurt–Münster (BFM) protocols and their modified versions have been widely used throughout the world [9–14]. The cure rates in BFM protocols in Western countries reach 80–90 %; however, this is not the case in developing countries [7–15]. Modifications have been made to the original ALL-BFM protocols in some centers depending on the availability of resources [11–14]. In Turkey, since January 2000, more than two thirds of pediatric hematology–oncology centers use a modified version of the ALL BFM-95 protocol, called BFM-Turkish (TR) ALL 2000, while a few centers implement the original ALL BFM-95 protocol [11, 16, 17]. Herein, we report the 15-year experiences of two university hospitals in Turkey with the original ALL BFM-95 protocol.
Patients and methods
A retrospective analysis of data of children with B-cell precursor or T-cell ALL, diagnosed and treated between January 1995 and January 2010 according to the original ALL-BFM 95 protocol in the pediatric hematology clinics of the university hospitals of Uludağ University (Bursa) and Dokuz Eylül University (İzmir), was carried out. A total of 343 children, aged between 1 and 18 years old and who completed chemotherapy at least 2 years prior to the analysis, were included in the study. Written informed consent had been obtained for all patients from their legal guardians before initiation of chemotherapy.
The diagnosis was based on morphological evaluation of Wright-stained smears of bone marrow if at least 25 % lymphoblasts were present, the blasts being negative for myeloperoxidase based on cytochemistry. Central nervous system (CNS) involvement was diagnosed if more than 5 cells/μL were present in nontraumatic cerebrospinal fluid at diagnosis and if lymphoblasts were identified unequivocally in cytospin preparations.
Immunophenotyping was carried out from bone marrow. Cell surface antigens were detected by standard indirect immunofluorescence assay with an extensive panel of antibodies. Conventional karyotypic analysis was performed systematically throughout the entire period. Fluorescence in situ hybridization (FISH) and/or reverse transcription polymerase chain (RT-PCR) reaction-based screening for BCR/ABL, MLL/AF4, and TEL/AML was carried out in 261 patients.
Risk group definitions and treatment
Patients were stratified according to the risk criteria set for the ALL-BFM 95 trial [5].
-
High risk (HR): Poor response to prednisone, and/or no complete remission on day 33, and/or positivity for t(9;22) (or BCR/ABL), and/or positivity for t(4;11) (or MLL/AF4) (poor risk genetic features)
-
Medium risk (MR): No HR criteria, initial WBC count of ≥20 × 109/L, and/or age at diagnosis of <1 or ≥6 years, and/or T-cell ALL
-
Standard risk (SR): No HR criteria, initial WBC count of <20 × 109/L, and/or age at diagnosis of between 1 and 6 years
Positivity for t(12;21) was accepted as good risk genetic finding. The details of the ALL-BFM 95 protocol are described elsewhere [5]. All patients were treated according to the original ALL BFM-95 protocol without randomization for the MCA arm in the MR group. The protocol consisted of four phases: induction, consolidation, re-induction, and maintenance therapy. No modifications were made to the original protocol, except for using vincristine instead of vindesine, since vindesine is not available in Turkey. CNS-directed therapy consisted of intrathecal treatment and CNS radiotherapy. The therapeutic irradiation dose for patients with initial involvement of the CNS was 12 Gy for patients aged 1 to 2 years and 18 Gy for patients of more than 2 years of age. Preventive radiotherapy was only indicated for T-cell ALL and the HR group. The duration of treatment was 24 months for all patients in ALL BFM-95. Patients were given prophylactic fluconazole (4–6 mg/kg/day) during the neutropenic period and trimethoprim sulfamethoxazole throughout the whole treatment period. Granulocyte colony-stimulating factor was given after each HR block.
Febrile neutropenia episodes were initially treated empirically with antipseudomonal antibiotics. Empirical antifungal treatment was started in the presence of persistent fever by the fifth day after starting antibiotics.
Response criteria
Standardized response criteria were used to define good prednisone response, complete remission (CR), and relapse. After 7 days of steroid monotherapy, the presence of <1 × 109 /L blasts in the peripheral blood on day 8 was described as a good response to prednisone and ≥1 × 109/L as a poor response to prednisone. CR was defined as <5 % blasts in regenerating bone marrow without evidence of extramedullary residual disease.
Definitions
Patients ≥ 13 years old are defined as adolescents.
Event-free survival (EFS) was defined as the time from diagnosis to the date of the last follow-up in CR or the first event. “Events” were nonresponse to therapy, abandonment of treatment, relapse, or death from any cause. Overall survival (OS) was defined as the time from initiation of treatment to death or date of last follow-up.
Statistical analysis
All statistical analyses were performed using SPSS 15, and P < 0.05 was considered to be statistically significant. Analyses for EFS and OS rates were performed according to the Kaplan–Meier method, and survival curves were compared with the log-rank test.
Results
Patients’ characteristics
The median age of the 343 patients was 6.8 years (range 1–17.5 years). Patients’ characteristics are shown in Table 1.
Good response to prednisone was seen in 298 patients (87 %). CR was achieved in 333 of 343 patients (97 %), while 5 patients (1.5 %) had M2/M3 marrow at the end of the induction treatment. Five patients (1.5 %) died during induction treatment due to infection or disease complications.
Survival
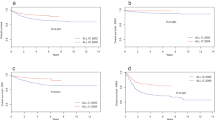
After a median observation period of 6.4 years, the 5-year EFS and OS were 78.4 and 79.9 % for all risk groups, respectively (Fig. 1). The EFS and OS at 5 years for patients <6 years old were 83.7 and 85.2 %, respectively (Fig. 2). Patients between 6 and 18 years old had significantly lower EFS (71.4 %) and OS (72.8 %) rates compared to those <6 years old (P < 0.05 and P < 0.05, respectively). Adolescents achieved 63 % EFS and 65 % OS, lower rates than those seen in younger children (P < 0.05 and P < 0.05). Patients who had initial leukocyte counts of <20 × 109/L had better EFS and OS (82.2 and 84.6 %) than children with higher initial leukocyte counts (72.6 and 72.6 %) (P = 0.038 and P = 0.009, respectively; Fig. 3). The EFS and OS at 5 years for patients with B-cell precursor ALL were 81.5 and 83.4 %, respectively. Patients with T-cell ALL had significantly lower EFS (66.7 %) and OS (66.7 %) compared to those with B-cell precursor ALL (P = 0.021 and P = 0.01, respectively; Fig. 4). Children with good response to prednisolone on day 8 achieved significantly better EFS and OS (81.2 and 81.9 % vs. 55.3 and 60.5 %; P = 0.001 and P = 0.001, respectively; Fig. 5). Children whose bone marrow on day 15 was in complete remission (227 patients, 66.1 %) had higher EFS and OS (83.7 and 86.6.1 % vs. 56.4 and 61.5 %; P = 0.005 and P = 0.001, respectively). Children whose bone marrow on day 33 was in complete remission achieved significantly better EFS and OS (80.5 and 82 %) than children who were not in complete remission (0 %; P = 0.001). The 5-year EFS was 95.5 % in the SR group, 82.7 % in the MR group, and 56.3 % in the HR group. The OS at 5 years in these risk groups was 97.7, 82.3, and 63.4 %, respectively (Fig. 6). Cytogenetic and molecular genetic analysis could be performed in 261 of the patients; 29 children (11 %) had poor and 45 (17.2 %) had good genetic features. The EFS and OS of the patients with good genetic features (94.3 and 97.4 %) were significantly better than in those with poor genetic features (63 and 64 %; P < 0.05 and P < 0.05). There was no significant association between sex and survival rates (P > 0.05).
Fifty-one patients (14.8 %) relapsed within 23.21 ± 13.16 months. The majority of relapses occurred within 2 years of diagnosis. Twenty-one (41 %) of those patients were adolescents. Thirty-eight (74 %) of the relapsed patients had B-cell precursor ALL. Of the 51 relapsed patients, 2 (4 %) were in the SR group, 27 (53 %) were in the MR group, and 22 (43 %) were in the HR group. All relapsed patients were treated with various salvage chemotherapies, and six of them underwent allogeneic transplantation. Fourteen (27.5 %) of the 51 relapsed patients died due to infection or progressive disease.
Death occurred in 69 of 343 patients (20.1 %). Causes of death are shown in Fig. 7. The major causes of death were infection and relapse; no patients died due to drug-related toxicity or bleeding.
Discussion
The BFM-based protocols have been widely used for treatment of children with ALL in Turkey, especially since 1995. Most of the centers in Turkey use the Turkish (TR)-ALL BFM 2000, which includes the modification of intravenous high-dose methotrexate at 1 g/m2/36 h instead of 5 g/m2/24 h and related prophylactic 12 Gy of cranial irradiation given in the non-T-cell MR group [11, 18]. The two centers involved in the present study have used the original ALL-BFM 95 protocol since 1995, and to our knowledge, this is the largest cohort with the original ALL-BFM 95 protocol reported from Turkey.
Most of the clinical and biological characteristics of the patients with ALL in this study are similar to those reported from developed countries [9, 10]. The proportion of male patients was 58 % in this study, and a slightly increased male-to-female ratio has also been reported in other studies [10, 11, 15, 17]. The proportion of T-cell ALL in this study was 19 %. Similarly, two other centers using BFM-based protocols in Turkey have also reported the rate of T-cell ALL as 16.2 and 19.6 % [11, 17]. Another recent study from Turkey, including 30 centers using the TR-ALL BFM 2000 protocol, reported that 19.6 % of 1,793 patients had T-cell ALL [18]. The range of T-cell ALL has been reported to be about 17.4 to 26.6 % from the west European countries, USA, Israel, and Egypt [5, 9, 10, 19–21].
Regarding the distribution of risk groups, the majority of the patients in this study were in the MR group, as in other studies [5, 10]. However, a higher proportion of patients were allocated to the HR group (21 %) as compared to other studies reported from Turkey and west European countries (8–12 %) [5, 10]. This may be due to the studied centers in İzmir and Bursa being tertiary referral centers.
Induction failure is a rare event in acute leukemia treatment. The treatment response at the end of induction was 97 % in this study, which is similar to other results reported in the literature [10, 17, 19]. The relapse rate was found to be 14.8 %, which is comparable to the original ALL-BFM 95 trial (16.2 %) [5, 10]. Similarly, the TR-ALL BFM 2000 study reported a relapse rate of 13.5 % [18]. These relapse rates reported from Turkey are lower than the relapse rates of many developing countries, which have rates of up to 30 % [15, 22]. In developing countries, the relapse rates may be higher because of lack of genetic and molecular studies, the giving of lower doses of chemotherapeutic agents, and longer interruption periods. The majority of relapsed patients in this study were from the MR group. The same finding was also reported in the original ALL-BFM 95 trial and other BFM-based studies [10, 11, 17]. These results underline the importance of better delineation of risk groups by minimal residual disease (MRD), which is a more refined way of determining in vivo response at certain time points [23]. Therefore, the ALL-BFM 2000 trial, in addition to the risk criteria defined in ALL-BFM 95, used MRD status as a risk criterion and modified the treatment intensity depending on the MRD status [10, 24]. Recently, there have been attempts in Turkey to detect MRD by flow cytometric analysis, but the logistics and quality control are very complicated. The two centers involved in this study have been sending bone marrow samples at certain time points to Heidelberg, Germany, for detection of MRD by PCR-based analysis for almost 4 years. However, as the price of MRD analysis has not been covered by Turkish social security insurance yet, the analysis cannot be done for all patients.
In the current study, 5-year EFS and OS were 78.4 and 79.9 %, respectively. Our results are similar to the results reported from developed countries and better than the survival rates reported from other developing countries [9–15]. The 5-year EFS and OS rates according to risk groups were almost identical in our study and in the large BFM trial reported from Europe [9, 10]. Accordingly, patients with older age, T-cell leukemia, higher initial leukocyte count, poor response to prednisone, and M3 marrow on days 15 and 33 were found to have lower survival rates, consistent with the risk stratification. It is important to note that our results do not reflect the situation of the whole country. The two well-equipped university hospitals involved in this study are located in two large cities in the west of Turkey, where the socioeconomic level is better compared to other regions of Turkey. A recent study reported from Ankara, the capital of Turkey, also reported higher survival rates [17]. On the other hand, the survival rates of the TR-ALL BFM 2000 study, including a total of 30 centers comprising both university hospitals and less equipped state hospitals across Turkey, are lower compared to our results [18]. The 5-year EFS was 68.4 % in all risk groups and 79.8, 71.8, and 44.4 % in the SR, MR, and HR groups, respectively, in that study. The relatively lower survival rates detected in the TR-ALL BFM 2000 study may be due to the heterogeneity of the study, as it included 30 different centers with different infrastructures. Attempts at standardization of treatment and enhancement of health care facilities and educational programs have already been started for all centers using this protocol in Turkey.
New therapeutic interventions are needed for children in the HR ALL group. In our study, children in the SR and MR groups obtained statistically significantly higher EFS compared to the HR group. One of the major findings derived from five consecutive trials (between 1981 and 2000) of the BFM study group for childhood ALL is that intensification of consolidation/re-intensification treatment led to considerable improvement of survival in the HR group [25]. Allogeneic hematopoietic stem cell transplantation in the first complete remission is recommended in very high-risk patients, due to the specific toxicities associated with this procedure [25]. The therapeutic benefit of alternative therapies such as targeted agents, immunotherapy, and/or allogeneic hematopoietic stem cell transplantation in children refractory to conventional treatment has been evaluated by many study groups, and as in Ph + ALL, if agents show truly selective activity and do not impose additional toxicity, it is necessary to administer them in those patient subsets in which current treatment cannot achieve EFS rates comparable to those of the overall ALL group [26].
The death rate was found to be 20.1 % in this study, which was rather high compared to those reported from developed countries [10, 19]. Treatment-related mortality accounts for an increasing percentage of total deaths. When a series of reports that included over 42,000 ALL patients (0–21 years) treated between 1981 and 2007 was reviewed, the rate of death ranged from 0.7 to 4 % during induction and 1.7 to 4.5 % during remission [27]. Our result was comparable to other results reported from Turkey [11, 17, 18]. The most common cause of death in this study and in all other studies reported from Turkey was infection, which still continues to be a major problem in developing countries. Much effort is needed to decrease this high rate of infection in developing countries; in particular, provision of specialized oncology centers with adequate infrastructure including air-cleaning facilities, specialized chemotherapy units, and adequate numbers of trained health care personnel, and the education of parents or patients about personal hygiene, is essential for prevention of infections. It is noteworthy that none of the patients in the present study died due to bleeding or chemotherapy toxicity.
In conclusion, the ALL-BFM 95 protocol was applied successfully in these two centers. In developing countries in which MRD cannot be assessed, this protocol can still be used in selected centers successfully.
References
Centers for Disease Control and Prevention (CDC) (2007) Trends in childhood cancer mortality—United States, 1990–2004. MMWR Morb Mortal Wkly Rep 56(48):1257–1261
Linabery AM, Ross JA (2008) Trends in childhood cancer incidence in the U.S. (1992–2004). Cancer 112(2):416–432
Schrappe M, Nachman J, Hunger S, Schmiegelow K, Conter V, Masera G, Pieters R, Pui CH (2010) Educational symposium on long-term results of large prospective clinical trials for childhood acute lymphoblastic leukemia (1985–2000). Leukemia 24(2):253–254
Silverman LB, Gelber RD, Dalton VK, Asselin BL, Barr RD, Clavell LA, Hurwitz CA, Moghrabi A, Samson Y, Schorin MA, Arkin S, Declerck L, Cohen HJ, Sallan SE (2001) Improved outcome for children with acute lymphoblastic leukemia: results of Dana-Farber Consortium Protocol 91–01. Blood 97(5):1211–1218
Möricke A, Reiter A, Zimmermann M, Gadner H, Stanulla M, Dördelmann M, Löning L, Beier R, Ludwig WD, Ratei R, Harbott J, Boos J, Mann G, Niggli F, Feldges A, Henze G, Welte K, Beck JD, Klingebiel T, Niemeyer C, Zintl F, Bode U, Urban C, Wehinger H, Niethammer D, Riehm H, Schrappe M, German-Austrian-Swiss ALL-BFM Study Group (2008) Risk-adjusted therapy of acute lymphoblastic leukemia can decrease treatment burden and improve survival: treatment results of 2169 unselected pediatric and adolescent patients enrolled in the trial ALL-BFM95. Blood 1111(9):4477–4489
Pui CH, Mullighan CG, Evans WE, Relling MV (2012) Pediatric acute lymphoblastic leukemia: where are we going and how do we get there? Blood 120:1165–1174
Marwaha RK, Kulkarni RP, Bansal D, Trehan A (2010) Pattern of mortality in childhood acute lymphoblastic leukemia: experience from a single center in northern India. J Pediatr Hematol Oncol 32(5):366–369
Metzger ML, Howard SC, Fu LC, Peña A, Stefan R, Hancock ML, Zhang Z, Pui CH, Wilimas J, Ribeiro RC (2003) Outcome of childhood acute lymphoblastic leukemia in resource-poor countries. Lancet 362(9385):706–708
Schrappe M, Reiter A, Zimmermann M, Harbott J, Ludwig WD, Henze G, Gadner H, Odenwald E, Riehm H (2000) Long-term results of four consecutive trials in childhood ALL performed by the ALL-BFM study group from 1981 to 1995. Berlin-Frankfurt-Munster. Leukemia 14(12):2205–2222
Möricke A, Zimmermann M, Reiter A, Henze G, Schrauder A, Gadner H, Ludwig WD, Ritter J, Harbott J, Mann G, Klingebiel T, Zintl F, Niemeyer C, Kremens B, Niggli F, Niethammer D, Welte K, Stanulla M, Odenwald E, Riehm H, Schrappe M (2010) Long-term results of five consecutive trials in childhood acute lymphoblastic leukemia performed by the ALL-BFM study group from 1981 to 2000. Leukemia 24(2):265–284
Hazar V, Karasu GT, Uygun V, Akcan M, Küpesiz A, Yesilipek A (2010) Childhood acute lymphoblastic leukemia in Turkey: factors influencing treatment and outcome: a single center experience. J Pediatr Hematol Oncol 32(8):e317–e322
Von Stackelberg A, Karatchunsky A, Kudrjashova J, Miakova N, Belikova L, Rumiantzev A, Hartmann R, Henze G (1999) Toxicity supportive care and costs of two chemotherapy protocols for treatment of childhood ALL in Russia: BFM 90m and MB 91. Eur J Cancer 35(9):1349–1355
Campbell M, Salgado C, Quintana J, Becker A, Vargas L, Cabrera ME, Beresi V, Rojas J, Paez E, Tapia S, Zolezzi P, Advis P (1999) Improved outcome for acute lymphoblastic leukemia in children of a developing country: results of the Chilean National Trial PINDA 87. Med Pediatr Oncol 33(2):88–94
Aziz Z, Zahid M, Mahmood R, Maqbool S (1997) Modified BFM protocol for childhood acute lymphoblastic leukemia: a retrospective analysis. Med Pediatr Oncol 28(1):48–53
Bajel A, George B, Mathews V, Viswabandya A, Kavitha ML, Srivastava A, Chandy M (2008) Treatment of children with acute lymphoblastic leukemia in India using a BFM protocol. Pediatr Blood Cancer 51(5):621–625
İrken G, Ören H, Gülen H, Duman M, Uçar C, Atabay B, Yilmaz S, Uysal K, Cevik N (2002) Treatment outcome of adolescents with acute lymphoblastic leukemia. Ann Hematol 81(11):641–645
Kocak U, Gursel T, Kaya Z, Aral YZ, Albayrak M, Keskin EY, Belen B, Isık M, Oner N (2012) ALL-BFM 95 treatment in Turkish children with acute lymphoblastic leukemia—experience of a single center. Pediatr Hematol Oncol 29(2):130–140
Soycan LY, Aydoğan G, Timur Ç, Vergin C, Patıroğlu T, Tanyeli A, Hazar V, Atabay B, Antmen B, Sarper N (2008) Pediatrik ALL tedavisinde ilk çok merkezli tedavi protokolü: BFM-TR ALL 2000. Abstract. 34th National Hematology Conference, Çeşme, İzmir, Turkey (in Turkish)
Pui CH, Pei D, Sandlund JT, Rubnitz JE, Raimondi SC, Onciu M, Campana D, Kun LE, Jeha S, Cheng C, Howard SC, Metzger ML, Bhojwani D, Downing JR, Evans WE, Relling MV (2010) Long-term results of St Jude Total Therapy studies 11, 12, 13A, 13B and 14 for childhood acute lymphoblastic leukemia. Leukemia 24(2):371–382
Stark B, Nirel R, Avrahami G, Abramov A, Attias D, Ballin A, Bielorai B, Burstein Y, Gavriel H, Elhasid R, Kapelushnik J, Sthoeger D, Toren A, Wientraub M, Yaniv I, Izraeli S (2010) Long-term results of the Israeli National Studies in childhood acute lymphoblastic leukemia: INS 84, 89 and 98. Leukemia 24(2):419–424
Hussein H, Sidhom I, Naga SA, Amin M, Ebied E, Khairy A, Kamel A, El-Sharkawy N (2004) Outcome and prognostic factors of acute lymphoblastic leukemia in children at the National Cancer Institute, Egypt. J Pediatr Hematol Oncol 26(8):507–514
Kulkarni KP, Marwaha RK, Trehan A, Bansal D (2009) Survival outcome in childhood ALL: experience from a tertiary care center in North India. Pediatr Blood Cancer 53(2):168–173
Campana D (2012) Minimal residual disease monitoring in childhood acute lymphoblastic leukemia. Curr Opin Hematol 19(4):313–318
Conter V, Venn NC, Tolisano J, Schrauder A, Panzer-Grümayer R, Möricke A, Aricò M, Zimmermann M, Mann G, De Rossi G, Stanulla M, Locatelli F, Basso G, Niggli F, Barisone E, Henze G, Ludwig WD, Haas OA, Cazzaniga G, Koehler R, Silvestri D, Bradtke J, Parasole R, Beier R, van Dongen JJ, Biondi A, Schrappe M (2010) Molecular response to treatment redefines all prognostic factors in children and adolescents with B-cell precursor acute lymphoblastic leukemia: results in 3184 patients of the AIEOP-BFM ALL 2000 study. Blood 115(16):3206–3214
Schrappe M, Möricke A, Reiter A, Henze G, Welte K, Gadner H, Ludwig WD, Ritter J, Harbott J, Mann G, Klingebiel T, Gruhn B, Niemeyer C, Kremens B, Niggli F, Debatin KM, Ratei R, Stanulla M, Beier R, Cario G, Schrauder A, Zimmermann M (2013) Key treatment questions in childhood acute lymphoblastic leukemia: results in 5 consecutive trials performed by the ALL-BFM study group from 1981 to 2000. Klin Padiatr 225(Suppl 1):62S–72S
Schrappe M (2013) Novel treatment approaches for acute lymphoblastic leukemia in childhood and adolescence. Hematol Educ: Educ Program Annu Congr Eur Hematol Assoc 7:16–22
Hunger SP, Baruchel A, Biondi A, Evans WE, Jeha S, Loh M, Moericke A, Pieters R, Relling MV, Schmiegelow K, Schrappe M, Silverman LB, Stanulla M, Valsecchi MG, Vora A, Pui CH (2013) The thirteenth international childhood acute lymphoblastic leukemia workshop report: La Jolla, CA, USA, December 7–9, 2011. Pediatr Blood Cancer 60(2):344–348
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Güneş, A.M., Ören, H., Baytan, B. et al. The long-term results of childhood acute lymphoblastic leukemia at two centers from Turkey: 15 years of experience with the ALL-BFM 95 protocol. Ann Hematol 93, 1677–1684 (2014). https://doi.org/10.1007/s00277-014-2106-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-014-2106-0