Abstract
Relapse period is strongly associated with second relapse risk in relapsed acute lymphoblastic leukemia (ALL) in children. In this context, the treatment outcome of very late relapse should be better; however, data regarding very late relapse is limited. We retrospectively analyzed the outcomes of two consecutive Tokyo Children’s Cancer Study Group (TCCSG) ALL trials (1995–2004) with a focus on late relapse, which was divided into two categories: late relapse (6–24 months from the end of therapy, n = 48) and very late relapse (>24 months from the end of therapy, n = 57). Forty-three patients (29 late relapse and 14 very late relapse) received allogeneic hematopoietic stem cell transplantation (HSCT) at second remission. The event-free survival (EFS) probabilities of late relapse and very late relapse were 54.5 ± 7.3 and 64.8 ± 6.8 % at 7 years, respectively (P = 0.36), and were not significantly different. However, the second relapse incidence of late relapse (34.7 ± 7.1 %) was higher than that of very late relapse (15.5 ± 5.1 %, P = 0.03). The second relapse risk was low for very late relapse ALL, which suggests that these patients should be treated without allogeneic HSCT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Current clinical trials have cured more than 80 % of children with acute lymphoblastic leukemia (ALL), and one of the main reasons for this outcome was the adaptation of a risk stratification strategy using biological features and early treatment responses [1–6]. However, relapse remains the most common treatment failure. Salvage therapy for relapsed pediatric ALL typically consists of intensive chemotherapy including allogeneic hematopoietic stem cell transplantation (HSCT) as a consolidation treatment for most relapsed patients, who had a survival probability of 40–60 % after the first relapse [7–9].
Relapse risk-oriented stratification has also contributed to improving the outcome of relapsed childhood ALL [9, 10]. Previous studies demonstrated that the risk of second relapse could be estimated by the relapse period, relapse site, immunophenotype [11–13], and early responses to re-remission induction therapy. Thus, most clinical trial groups for pediatric ALL have adopted a combination of these factors in order to treat relapsed ALL [12, 14, 15].
The relapse period is considered the most important of these risk factors, and the Berlin–Frankfurt–Munster (BFM) group divided the relapse period into three categories: very early (earlier than 18 months from the diagnosis), early (later than 18 months from the diagnosis and earlier than 6 months from the end of the treatment), and late (later than 6 months from the end of the treatment), and showed that late relapse was associated with a good prognosis. The Pediatric Oncology Group also stratified ALL that relapsed within 6 months after the cessation of treatments as being at a higher risk of second relapse [16]. In this context, the second relapse risk of “very late” relapsed ALL should be lower, as suggested by previous studies [17–19]. However, the number of patients analyzed has been limited due to the rarity of very late relapse, and data regarding long-term outcomes is currently insufficient to establish a standard treatment for patients with very late relapse. Thus, we retrospectively analyzed the long-term outcomes of late relapsed ALL patients who were enrolled in two consecutive Tokyo Children’s Cancer Study Group (TCCSG) clinical trials, with a focus on children with very late relapse.
Patients and methods
Patients
In order to identify patients with very late relapse, a total of 1,605 newly diagnosed ALL patients (1–18 years) enrolled in the two consecutive TCCSG trials, L95-14 [20] (between 1995 and 1999, n = 597), L99-15/1502 [21–23] (between 1999 and 2004, n = 754/254) were reviewed as of June 2013. Their front-line treatment schedules and findings have already been reported [20–23], and the duration of chemotherapy was 24 months for all patients except standard risk patients enrolled in L99-15/1502 with 36 months of treatment. The treatment strategy after relapse was decided by each physician.
In the present study, we defined “late relapse” and “very late relapse” as relapse at 6–24 months and later than 24 months after the end of the treatment, respectively (Fig. 1a). Patients who received HSCT at their first remission were excluded.
Definition and distribution of late and very late relapse. a Definition of late and very late relapse. Late and very late relapse were defined as 6–24 months and later than 24 months after the end of chemotherapy, respectively. In TCCSG clinical trials, which were included in this analysis, the duration of the chemotherapy regimen was 24 (intermediate and high risk) or 36 (standard risk) months. b Distribution of the late and very late relapse periods
Statistical analysis
Fisher’s exact test was used to compare differences in the distribution of clinical features among each group. The duration of event-free survival (EFS) was defined as the time from relapse to either treatment failure (second relapse, death, or the diagnosis of secondary cancer) or to the final day of observations that confirmed the patient was failure free. Overall survival (OS) was defined as the time from relapse to death from any cause or the time of the last follow-up. The probabilities of EFS and OS were estimated using the Kaplan–Meier analysis, and the significance of differences was evaluated using the log-rank test.
The cumulative incidences of relapse were estimated taking into account the competing events of death without second relapse and development of a secondary malignancy. To determine the cumulative incidence of non-relapse mortality (NRM), relapse and the development of secondary malignancies were considered as competing risk factors. Gray’s test was used to assess the significance of the relapse period on the cumulative incidences. All statistical analyses were performed using the R software 2.13.0 (The R Foundation for Statistical Computing, Vienna, Austria). A 2-sided p value less than 0.05 was considered significant.
Results
Patients
Patient characteristics are summarized in Table 1. A total of 105 patients relapsed 6 months or later after the end of therapy, including 48 who were late relapse patients (6–24 months) and 57 who were very late relapse patients (later than 24 months). The distribution of the relapse period is shown in Fig. 1b. Excluding 2 patients (1 late relapse and 1 very late relapse) due to insufficient follow-up data, the median follow-up period of surviving patients after relapse for the 103 patients was 7.3 years. Although 3 patients (1 patient with late relapse, and 2 patients with very late relapse) died during remission induction chemotherapy, all other patients achieved second remission.
Outcomes after relapse
Second relapse occurred in 24 patients at a median of 556 (range 175–1,379) days after the first relapse, and 16 patients died before the second relapse, including 3 patients who died before they achieved second remission. OS and EFS at 7 years after the first relapse were 67.2 ± 4.9 and 60.2 ± 5.0 %, respectively, and the relapse and non-relapse mortality incidences were 24.4 ± 4.4 and 15.4 ± 3.7 %, respectively.
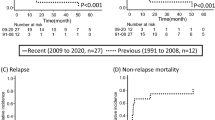
EFS of late relapse patients and very late relapse patients were 54.5 ± 7.3 and 64.8 ± 6.8 % at 7 years, respectively, and this difference was not significant (p = 0.36, Fig. 2a). However, the incidence of relapse was significantly higher in late relapse group (34.7 ± 7.1 %) than in very late relapse group (15.5 ± 5.1 %) (p = 0.031, Fig. 2b), while the non-relapse mortality rates of late relapse patients and very late relapse patients were 10.8 ± 4.6 and 19.8 ± 5.8 %, respectively (p = 0.19, Fig. 2c). Of 4 T-ALL with very late relapse, 2 were alive in CR, 1 died before relapse, and 1 patients suffered relapse.
As with salvage treatment for the first relapse, 29 (60.4 %) of 48 late relapse patients and 14 (24.6 %) of 57 very late relapse patients underwent allogeneic HSCT at the second complete remission (CR2). A median time from the first relapse to HSCT was 201 days for late relapse and 181 days for very late relapse. Second relapse occurred in 9 patients after the HSCT, whereas 8 patients died before second relapse. When the 43 patients who received HSCT in CR2 were censored at the transplantation time in order to focus on the outcomes of patients treated with chemotherapy, EFS of very late relapse patients (73.6 ± 7.0 %) was significantly higher than that late relapse patients (37.4 ± 11.8 %) (p = 0.027, Fig. 3a). The EFS superiority of very late group was reproduced when limited to the patients who were treated with chemotherapy only (p = 0.009, Fig. 3b).
Among the 57 very late relapse patients, 16 patients relapsed at later than 48 months after the end of the treatment, 14 had bone marrow-related relapse, and 2 had isolated extramedullary relapse. All of these extremely late relapse patients were alive without a second relapse at a median follow-up duration of 4.7 years after the first relapse, although only 1 patient received allogeneic HSCT during CR2.
Although most of the first relapse sites were related to the bone marrow, 10 relapses were isolated to extramedullary regions. All 10 isolated extramedullary relapse patients survived without events, although only 1 patient underwent allogeneic HSCT. The cumulative incidence of second relapse in bone marrow-related relapse was 28.5 ± 5.0 %. When limited to very late relapse patients, the cumulative incidence of relapse in bone marrow-related relapse patients (n = 47) was 19.0 ± 6.2 %. The second relapse site was the bone marrow in 20 patients, isolated extramedullary region in 3 patients (2 bone and 1 mammary gland), and combined in 1 patient (bone marrow and the central nervous system).
Discussion
Advances in treatment strategies have reduced the relapse rate of pediatric ALL to approximately 10 %. The relapse period is a potent risk factor for second relapse, with previous studies reporting that the later relapse occurs, the better the outcome of salvage chemotherapy [11]. Accordingly, very late relapse is considered to be a very good risk factor for relapsed ALL; however, only limited evidence is available because of the small number of patients [17, 18]. In our study, we demonstrated that very late relapse was associated with a lower relapse incidence than that of late relapse.
The relapse site has also been linked to the outcomes of relapsed ALL, and isolated extramedullary relapse is considered to be a good prognostic factor. The BFM group classification for relapsed ALL categorized late and isolated extramedullary relapse as the lowest risk group, and our results confirmed that late and isolated extramedullary relapse could be salvaged without HSCT. Although relapse including bone marrow was considered as a higher risk of relapse, the incidence of bone marrow-related relapse in our cohort was not high when it occurred very late. Extremely late relapse (later than 48 months) in particular had excellent outcomes, and was assumed to be curable without allogeneic HSCT. However, of note, a study reported that relapse period usually depends on the prior treatment, and extremely late relapse might become much fewer by recent intensive chemotherapeutic strategy [24].
The effectiveness of risk-adapted strategies is well recognized not only in de novo ALL, but also relapsed ALL, and excess intensified treatments such as allogeneic HSCT should not be adapted to avoid unnecessary morbidity and non-relapse mortality. In our cohort, of 14 patients with very late relapse and receiving HSCT, 5 patients died before relapse, while only two patients relapsed, which suggested that allogeneic HSCT for very late relapsed ALL may lead to higher non-relapse mortality rates in spite of a lower relapse incidence. Recent studies showed that measuring minimal residual disease (MRD) was useful for stratifying relapsed ALL [9, 10]. Although data regarding MRD was unfortunately not available in our patients, MRD kinetics after salvage treatments may be used to predict a high-risk subgroup in very late relapsed ALL.
Interestingly, some studies suggested that a certain portion of late relapse were not reoccurrence of the first leukemic cells, but independent development from preleukemic clones which had existed at the first onset, especially ALL with ETV6-RUNX1 [25–27], although data regarding this fusion was not available in our cohort. The findings are consistent with our results that very late relapse is associated with lower relapse risk as relapsed ALL, although we unfortunately could not compare molecular profile of leukemic cells at diagnosis and at relapse.
This study had some limitations which may have introduced bias, mainly due to the nature of a retrospective and uncontrolled study. For example, salvage strategies were not uniform, including the indication of allogeneic HSCT. Further prospective studies regarding very late relapse in a larger cohort are required even though it will require a long commitment.
In conclusion, our results demonstrated that the risk of second relapse in very late relapsed ALL was lower than that of late relapsed ALL, and suggested that these patients should be treated without allogeneic HSCT even when first relapse occurs in the bone marrow.
References
Horibe K, Saito AM, Takimoto T, Tsuchida M, Manabe A, Shima M, et al. Incidence and survival rates of hematological malignancies in Japanese children and adolescents (2006–2010): based on registry data from the Japanese Society of Pediatric Hematology. Int J Hematol. 2013;98:74–88.
Schrappe M, Valsecchi MG, Bartram CR, Schrauder A, Panzer-Grumayer R, Moricke A, et al. Late MRD response determines relapse risk overall and in subsets of childhood T-cell ALL: results of the AIEOP-BFM-ALL 2000 study. Blood. 2011;118:2077–84.
Conter V, Bartram CR, Valsecchi MG, Schrauder A, Panzer-Grumayer R, Moricke A, et al. Molecular response to treatment redefines all prognostic factors in children and adolescents with B-cell precursor acute lymphoblastic leukemia: results in 3184 patients of the AIEOP-BFM ALL 2000 study. Blood. 2010;115:3206–14.
Vora A, Goulden N, Mitchell C, Hancock J, Hough R, Rowntree C, et al. Augmented post-remission therapy for a minimal residual disease-defined high-risk subgroup of children and young people with clinical standard-risk and intermediate-risk acute lymphoblastic leukaemia (UKALL 2003): a randomised controlled trial. Lancet Oncol. 2014;15:809–18.
Vora A, Goulden N, Wade R, Mitchell C, Hancock J, Hough R, et al. Treatment reduction for children and young adults with low-risk acute lymphoblastic leukaemia defined by minimal residual disease (UKALL 2003): a randomised controlled trial. Lancet Oncol. 2013;14:199–209.
Pui CH, Campana D, Pei D, Bowman WP, Sandlund JT, Kaste SC, et al. Treating childhood acute lymphoblastic leukemia without cranial irradiation. N Engl J Med. 2009;360:2730–41.
Parker C, Waters R, Leighton C, Hancock J, Sutton R, Moorman AV, et al. Effect of mitoxantrone on outcome of children with first relapse of acute lymphoblastic leukaemia (ALL R3): an open-label randomised trial. Lancet. 2010;376:2009–17.
Tallen G, Ratei R, Mann G, Kaspers G, Niggli F, Karachunsky A, et al. Long-term outcome in children with relapsed acute lymphoblastic leukemia after time-point and site-of-relapse stratification and intensified short-course multidrug chemotherapy: results of trial ALL-REZ BFM 90. J Clin Oncol. 2010;28:2339–47.
Eckert C, Henze G, Seeger K, Hagedorn N, Mann G, Panzer-Grumayer R, et al. Use of allogeneic hematopoietic stem-cell transplantation based on minimal residual disease response improves outcomes for children with relapsed acute lymphoblastic leukemia in the intermediate-risk group. J Clin Oncol. 2013;31:2736–42.
Bader P, Kreyenberg H, Henze GH, Eckert C, Reising M, Willasch A, et al. Prognostic value of minimal residual disease quantification before allogeneic stem-cell transplantation in relapsed childhood acute lymphoblastic leukemia: the ALL-REZ BFM Study Group. J Clin Oncol. 2009;27:377–84.
Borgmann A, von Stackelberg A, Hartmann R, Ebell W, Klingebiel T, Peters C, et al. Unrelated donor stem cell transplantation compared with chemotherapy for children with acute lymphoblastic leukemia in a second remission: a matched-pair analysis. Blood. 2003;101:3835–9.
Bailey LC, Lange BJ, Rheingold SR, Bunin NJ. Bone-marrow relapse in paediatric acute lymphoblastic leukaemia. Lancet Oncol. 2008;9:873–83.
van den Berg H, Groot-Kruseman HA, Damen-Korbijn CM, Bont ES, Schouten-van Meeteren AY, Hoogerbrugge PM. Outcome after first relapse in children with acute lymphoblastic leukemia: a report based on the Dutch Childhood Oncology Group (DCOG) relapse all 98 protocol. Pediatr Blood Cancer. 2011;57:210–6.
Bhojwani D, Pui CH. Relapsed childhood acute lymphoblastic leukaemia. Lancet Oncol. 2013;14:e205–17.
Raetz EA, Borowitz MJ, Devidas M, Linda SB, Hunger SP, Winick NJ, et al. Reinduction platform for children with first marrow relapse of acute lymphoblastic Leukemia: A Children’s Oncology Group Study (corrected). J Clin Oncol. 2008;26:3971–8.
Buchanan GR, Rivera GK, Pollock BH, Boyett JM, Chauvenet AR, Wagner H, et al. Alternating drug pairs with or without periodic reinduction in children with acute lymphoblastic leukemia in second bone marrow remission: a Pediatric Oncology Group Study. Cancer. 2000;88:1166–74.
Rizzari C, Valsecchi MG, Arico M, Miniero R, Messina C, De Rossi G, et al. Outcome of very late relapse in children with acute lymphoblastic leukemia. Haematologica. 2004;89:427–34.
Vora A, Frost L, Goodeve A, Wilson G, Ireland RM, Lilleyman J, et al. Late relapsing childhood lymphoblastic leukemia Blood. 1998;92:2334–7.
Chessells JM, Leiper AD, Richards SM. A second course of treatment for childhood acute lymphoblastic leukaemia: long-term follow-up is needed to assess results. Br J Haematol. 1994;86:48–54.
Igarashi S, Manabe A, Ohara A, Kumagai M, Saito T, Okimoto Y, et al. No advantage of dexamethasone over prednisolone for the outcome of standard- and intermediate-risk childhood acute lymphoblastic leukemia in the Tokyo Children’s Cancer Study Group L95-14 protocol. J Clin Oncol. 2005;23:6489–98.
Manabe A, Ohara A, Hasegawa D, Koh K, Saito T, Kiyokawa N, et al. Significance of the complete clearance of peripheral blasts after 7 days of prednisolone treatment in children with acute lymphoblastic leukemia: the Tokyo Children’s Cancer Study Group Study L99-15. Haematologica. 2008;93:1155–60.
Hasegawa D, Manabe A, Ohara A, Kikuchi A, Koh K, Kiyokawa N, et al. The utility of performing the initial lumbar puncture on day 8 in remission induction therapy for childhood acute lymphoblastic leukemia: TCCSG L99-15 study. Pediatr Blood Cancer. 2012;58:23–30.
Kato M, Koh K, Manabe A, Saito T, Hasegawa D, Isoyama K, et al. No impact of enhanced early intensification with intermediate-risk pediatric acute lymphoblastic leukemia: results of randomized trial TCCSG study L99-15. Br J Haematol. 2014;164:376–83.
Pui CH, Pei D, Campana D, Cheng C, Sandlund JT, Bowman WP, et al. A revised definition for cure of childhood acute lymphoblastic leukemia. Leukemia. 2014
Ford AM, Fasching K, Panzer-Grumayer ER, Koenig M, Haas OA. & Greaves MF Origins of “late” relapse in childhood acute lymphoblastic leukemia with TEL-AML1 fusion genes. Blood. 2001;98:558–64.
Konrad M, Metzler M, Panzer S, Ostreicher I, Peham M, Repp R, et al. Late relapses evolve from slow-responding subclones in t(12;21)-positive acute lymphoblastic leukemia: evidence for the persistence of a preleukemic clone. Blood. 2003;101:3635–40.
Inukai T, Yokota S, Okamoto T, Nemoto A, Akahane K, Takahashi K, et al. Clonotypic analysis of acute lymphoblastic leukemia with a double TEL-AML1 fusion at onset and relapse. Leukemia. 2006;20:363–5.
Acknowledgments
We thank Kaori Itagaki for preparing and refining the protocol data for ALL in the TCCSG. We also thank the pediatricians and nurses who participated in the treatment and follow-up of the patients in this study.
Conflict of interest
All authors had no conflict of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Kato, M., Manabe, A., Saito, A.M. et al. Outcome of pediatric acute lymphoblastic leukemia with very late relapse: a retrospective analysis by the Tokyo Children’s Cancer Study Group (TCCSG). Int J Hematol 101, 52–57 (2015). https://doi.org/10.1007/s12185-014-1710-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-014-1710-z