Abstract
Computed tomography (CT) as a routine follow-up has been a standard practice for patients with non-Hodgkin lymphoma although it is not recommended in most guidelines. We aimed to describe the value of surveillance CT in detection of disease relapse in patients with diffuse large B-cell lymphoma (DLBCL) and follicular lymphoma grade 3 (FL3) and to evaluate whether relapse detected by different methods influenced outcome. In this retrospective review of consecutive 341 patients with DLBCL or FL3 diagnosed between 2003 and 2009 in complete response (CR) or unconfirmed CR, 113 patients experienced relapses. We found that routine surveillance CT detected asymptomatic relapse in 25 patients (22.1 %; group 1), including 22 of 100 patients with DLBCL and three of 13 with FL3. The first presentation of relapse of the other 88 patients (group 2) included patient-reported symptoms (60.2 %), physical examination (13.3 %), or abnormal laboratory data (4.4 %). For 72 patients received chemotherapy after relapse, the overall survival after relapse was not different between groups 1 and 2 (p = 0.569). The results of our study suggested that routine surveillance CT only has a limited role in the early detection of relapse and the relapse detected by surveillance CT or not has no impact on survival after relapse for patients with DLBCL or FL3.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
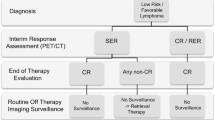
After the introduction of rituximab, a chimeric anti-CD20 monoclonal antibody, the survival of patients with diffuse large B-cell lymphoma (DLBCL) or follicular lymphoma (FL) has been improved [1–3]. However, 25–50 % of patients with DLBCL relapsed from complete response [4, 5]. Salvage treatment with high-dose chemotherapy and autologous stem cell transplantation is potentially curative for relapsed patients with DLBCL [5]. At relapse, there was evidence that the International Prognostic Index (IPI) predicted survival [6–8]. This suggested that early detection of relapse predicted better survival. However, the outcome of asymptomatic relapse detected by routine imaging was not different from that of symptomatic relapse [9, 10].
Previous studies showed that routine surveillance imaging detected only limited cases of relapse and most of the relapses were found by clinical symptoms and signs or laboratory examinations [9–12]. However, routine surveillance imaging is still a standard procedure in the follow-up of post-treatment lymphoma patients. The aims of this retrospective review were to describe the value of surveillance computed tomography (CT) in the detection of disease relapse in DLBCL and FL grade 3 (FL3) patients and to evaluate whether relapse detected by different methods influenced outcome.
Patients and methods
Patients
In order to clarify the value of surveillance CT in detection of disease relapse in aggressive lymphoma patients and to evaluate whether relapse detected by different methods influenced outcome, we retrospectively reviewed patients with DLBCL or FL3 consecutively diagnosed between 2003 and 2009. This review was approved by the Institutional Review Board of Chang Gung Memorial Hospital. Response criteria was according to Cheson et al. [13] Patients with complete response (CR) and unconfirmed CR (CRu) were included. All patients were followed in a 1–3-month interval with a complete physical examination and laboratory evaluations in the first 2 years after completion of treatment. Computed tomography was performed in a 3–6-month interval or when clinically indicated in the first 2 years and in a 12-month interval or clinically indicated thereafter up to 5 years. Other imaging modalities, including gallium scan, magnetic resonance imaging, and positron emission tomography (PET), were not standard methods for evaluation of response and for follow-up. The laboratory evaluation included complete blood count with a differential, serum lactate dehydrogenase, and serum beta 2-microglobulin. The surveillance CT included head, neck, chest, abdomen, and pelvis. Patients with asymptomatic relapse found by surveillance CT scan were assigned as group 1 and patients with first presentation of relapse found by other methods were assigned as group 2. Relapse at more than 5 years after achievement of CR or CRu was not included for analysis.
Statistical analysis
Categorical data was compared by Fisher’s exact or chi-square test. Continuous data was compared by t-test. Overall survival (OS) after relapse was calculated from the date of relapse to the date of death of any cause or the last date of follow-up. Patients were censored at the last follow-up date on which the patients were known to be alive. Survival curves were plotted by Kaplan–Meier method and compared by log-rank test between different groups. All comparisons were considered as significant if the p value was <0.05.
Results
Patient characteristics
Among 341 patients with DLBCL (N = 314) or FL 3 (N = 27) in CR or CRu, 118 patients experienced relapses, including 100 patients of DLBCL and 13 of FL3. The total number of surveillance CT was 1,837 among these 341 patients. The median age at relapse was 68. The characteristics of the relapsed patients are listed in Table 1.
Initial presentation at relapse
Surveillance CT detected relapse in 25 patients (22.1 %; group 1), including 22 of 100 patients (22.0 %) with DLBCL and three of 13 patients (23.1 %) with FL3. On average, 73.5 scans were performed to detect one relapse among the 341 patients. The first presentation of relapse of the other 88 patients (group 2) included patient-reported symptoms (N = 68, 60.2 % of 113 patients), physical examination at follow-up (N = 15, 13.3 %), and abnormal laboratory data (N = 5, 4.4 %). Patient-reported symptoms included enlarged lymph node(s) (N = 26, 38.2 %), gastrointestinal symptoms (N = 12, 17.6 %), neurological deficit (N = 9, 13.2 %), skin/soft tissue tumor (N = 6, 8.8 %), symptoms in nasopharyngeal field (N = 6, 8.8 %), respiratory symptoms (N = 5, 7.4 %), and B symptom(s) (N = 4, 5.9 %).
Interval from latest normal CT to initial presentation of relapse
The mean interval from latest normal CT to initial presentation of relapse was 4.9 months (range, 0.1–32.2 months). The interval was shorter in group 2 as compared to group 1 (mean, 4.5 vs. 6.0 months, p = 0.042). The interval was not different between patients with DLBCL and those with FL3 (mean, 4.5 vs. 4.9 months, p = 0.775).
Number and interval of surveillance CT
The average number of surveillance CT was 5.4 per patient in these 341 patients. Before disease relapse, the average number of CT scan was 3.2 per patient in group 1 and 3.2 in group 2 (p = 0.749), and 3.2 in DLBCL and 3.0 in FL3 (p = 0.993). The mean interval of surveillance CT before relapse was not different between groups 1 and 2 (mean, 4.4 vs. 4.8 months, p = 0.473) and between DLBCL and FL3 (mean, 4.7 vs. 4.5 months, p = 0.423). The mean number of CT per year was not different between groups 1 and 2 (mean, 2.4 vs. 2.3, p = 0.423).
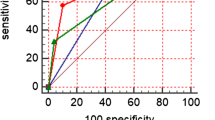
Treatment and overall survival after relapse
After relapse, 23 patients received salvage treatment with cyclophosphamide, etoposide, vincristine, and prednisolone (N = 18) or CHOP-like regimens (N = 5) with or without rituximab; 22 patients received high-dose chemotherapy without autologous stem cell transplantation; 16 patients received high-dose chemotherapy followed by autologous stem cell transplantation; 11 patients received rituximab plus cyclophosphamide, vincristine, and prednisolone; and 41 patients received palliative chemotherapy, local radiotherapy or supportive care. Excluding the 41 patients receiving palliative management, the OS after relapse of the other 72 patients was not different between groups 1 and 2 (both median OS not reached, p = 0.569; Fig. 1).
Discussion
In this retrospective review of 113 relapsed patients with DLBCL or FL3, we found that surveillance CT detected relapse in only 22.1 % of patients and more than 70 CT scans were performed to detect one asymptomatic relapse. Liedkte et al. retrospectively reviewed 108 relapsed aggressive lymphoma patients (75 % of DLBCL) and showed that 22.2 % of relapse was detected by routine surveillance imaging and 77.8 % by reported symptoms/physical findings (72.2 %) or abnormal findings on laboratory examination (5.6 %) [9]. Weeks et al. retrospectively reviewed 36 patients with large cell lymphoma who relapsed from complete response [12]. They found that only two of the 36 relapses were detected before symptoms of relapses. Guppy et al. retrospectively reviewed 117 DLBCL patients who were in complete response and followed with regular surveillance CT [14]. Only 5.7 % of the 35 relapsed patients were detected by surveillance CT. Elis et al. found that routine surveillance CT detected only four relapses of 30 patients with intermediate or aggressive lymphoma [15]. The others were detected by history, physical examination, or laboratory studies. Another large series study of 625 DLBCL patients by Abel et al. showed that 26.0 % of relapse was detected by routine imaging of CT, PET, or PET/CT [11]. PET or PET/CT has been a more sensitive method to detect residual disease than other imaging modalities in lymphoma patients [16–18] but the false-positive rate is higher. The role of PET or PET/CT in follow-up of lymphoma patients should be further evaluated in a larger clinical trial. In the present series, we found that surveillance CT detected less than one quarter of relapsed patients and the most common presentation of relapse was patient-reported symptoms (60.2 %). This suggested that routine surveillance CT only has a limited role in the follow-up of lymphoma patients in CR or CRu.
Liedkte et al. studied a large series of relapsed aggressive lymphoma patients (N = 108) and showed that the median progression-free survival (PFS) and OS at 5-year were slightly better in the group detected by routine imaging as compared to the group detected by reported symptoms/physical findings or abnormal laboratory findings [9]. However, the statistical differences were not significant (p = 0.12 and 0.13 for PFS and OS, respectively). Goldschmidt et al., using CT, PET, or PET/CT as routine surveillance imaging, also found that the survival was not influenced by the mode of relapse detection in aggressive lymphoma [10]. In the present series, the OS after relapse was not different between relapse detected by surveillance CT and by others in 72 patients receiving aggressive salvage treatment. Because of inadequate data, we were unable to analyze the effect of IPI at relapse on survival.
In the present series, the mean interval from latest normal CT to the presentation of relapse was 4.9 months. If the follow-up interval of routine surveillance CT is scheduled at 6-month, many relapses will not be detected. Abel et al. also observed that the median number of image studies per year was 2.5 in the first 2 years of follow-up [11] and only 26.0 % of relapse was detected through routine imaging in their series. In order to increase the detection rate of relapse by routine imaging, the frequency of routine imaging should be increased, for example, every 3 months. However, without definite evidence of improvement of outcome by early detection of relapse, increased frequency of routine imaging only increases the radiation dose and cost.
Routine imaging is not cost-effective and has long-term risks associated with high radiation exposure. In addition, Thompson et al. reported that surveillance CT was a source of anxiety and fear of recurrence in a cross-sectional observational study of 70 lymphoma patients under long-term follow-up [19]. Based on these retrospective studies, routine surveillance CT does not have benefit to the lymphoma patients in CR or CRu [20].
In conclusion, our results suggested that routine surveillance CT has a limited role in the early detection of relapse and no impact on survival after relapse for patients with DLBCL or FL3 in complete response or unconfirmed complete response. However, a prospective trial is necessary to further confirm the above results.
References
Coiffier B, Lepage E, Briere J, Herbrecht R, Tilly H, Bouabdallah R, Morel P, Van Den Neste E, Salles G, Gaulard P, Reyes F, Lederlin P, Gisselbrecht C (2002) CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large-B-cell lymphoma. N Engl J Med 346:235–242
Pfreundschuh M, Trumper L, Osterborg A, Pettengell R, Trneny M, Imrie K, Ma D, Gill D, Walewski J, Zinzani PL, Stahel R, Kvaloy S, Shpilberg O, Jaeger U, Hansen M, Lehtinen T, Lopez-Guillermo A, Corrado C, Scheliga A, Milpied N, Mendila M, Rashford M, Kuhnt E, Loeffler M (2006) CHOP-like chemotherapy plus rituximab versus CHOP-like chemotherapy alone in young patients with good-prognosis diffuse large-B-cell lymphoma: a randomised controlled trial by the MabThera International Trial (MInT) Group. Lancet Oncol 7:379–391
Hiddemann W, Kneba M, Dreyling M, Schmitz N, Lengfelder E, Schmits R, Reiser M, Metzner B, Harder H, Hegewisch-Becker S, Fischer T, Kropff M, Reis HE, Freund M, Wormann B, Fuchs R, Planker M, Schimke J, Eimermacher H, Trumper L, Aldaoud A, Parwaresch R, Unterhalt M (2005) Frontline therapy with rituximab added to the combination of cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) significantly improves the outcome for patients with advanced-stage follicular lymphoma compared with therapy with CHOP alone: results of a prospective randomized study of the German Low-Grade Lymphoma Study Group. Blood 106:3725–3732
Coiffier B, Thieblemont C, Van Den Neste E, Lepeu G, Plantier I, Castaigne S, Lefort S, Marit G, Macro M, Sebban C, Belhadj K, Bordessoule D, Ferme C, Tilly H (2010) Long-term outcome of patients in the LNH-98.5 trial, the first randomized study comparing rituximab-CHOP to standard CHOP chemotherapy in DLBCL patients: a study by the Groupe d’Etudes des Lymphomes de l’Adulte. Blood 116:2040–2045
Seshadri T, Kuruvilla J, Crump M, Keating A (2008) Salvage therapy for relapsed/refractory diffuse large B cell lymphoma. Biol Blood Marrow Transplant 14:259–267
Moskowitz CH, Nimer SD, Glassman JR, Portlock CS, Yahalom J, Straus DJ, O’Brien JP, Elkin N, Bertino JR, Zelenetz AD (1999) The International Prognostic Index predicts for outcome following autologous stem cell transplantation in patients with relapsed and primary refractory intermediate-grade lymphoma. Bone Marrow Transplant 23:561–567
Blay J, Gomez F, Sebban C, Bachelot T, Biron P, Guglielmi C, Hagenbeek A, Somers R, Chauvin F, Philip T (1998) The International Prognostic Index correlates to survival in patients with aggressive lymphoma in relapse: analysis of the PARMA trial. Parma Group Blood 92:3562–3568
Gisselbrecht C, Glass B, Mounier N, Singh Gill D, Linch DC, Trneny M, Bosly A, Ketterer N, Shpilberg O, Hagberg H, Ma D, Briere J, Moskowitz CH, Schmitz N (2010) Salvage regimens with autologous transplantation for relapsed large B-cell lymphoma in the rituximab era. J Clin Oncol 28:4184–4190
Liedtke M, Hamlin PA, Moskowitz CH, Zelenetz AD (2006) Surveillance imaging during remission identifies a group of patients with more favorable aggressive NHL at time of relapse: a retrospective analysis of a uniformly-treated patient population. Ann Oncol 17:909–913
Goldschmidt N, Or O, Klein M, Savitsky B, Paltiel O (2011) The role of routine imaging procedures in the detection of relapse of patients with Hodgkin lymphoma and aggressive non-Hodgkin lymphoma. Ann Hematol 90:165–171
Abel GA, Vanderplas A, Rodriguez MA, Crosby AL, Czuczman MS, Niland JC, Gordon LI, Millenson M, Zelenetz AD, Friedberg JW, Lacasce AS (2012) High rates of surveillance imaging for treated diffuse large B-cell lymphoma: findings from a large national database. Leuk Lymphoma 53:1113–1116
Weeks JC, Yeap BY, Canellos GP, Shipp MA (1991) Value of follow-up procedures in patients with large-cell lymphoma who achieve a complete remission. J Clin Oncol 9:1196–1203
Cheson BD, Horning SJ, Coiffier B, Shipp MA, Fisher RI, Connors JM, Lister TA, Vose J, Grillo-Lopez A, Hagenbeek A, Cabanillas F, Klippensten D, Hiddemann W, Castellino R, Harris NL, Armitage JO, Carter W, Hoppe R, Canellos GP (1999) Report of an international workshop to standardize response criteria for non-Hodgkin’s lymphomas. NCI Sponsored International Working Group. J Clin Oncol 17:1244–1253
Guppy AE, Tebbutt NC, Norman A, Cunningham D (2003) The role of surveillance CT scans in patients with diffuse large B-cell non-Hodgkin’s lymphoma. Leuk Lymphoma 44:123–125
Elis A, Blickstein D, Klein O, Eliav-Ronen R, Manor Y, Lishner M (2002) Detection of relapse in non-Hodgkin’s lymphoma: role of routine follow-up studies. Am J Hematol 69:41–44
Van Den Bossche B, Lambert B, De Winter F, Kolindou A, Dierckx RA, Noens L, Van De Wiele C (2002) 18FDG PET versus high-dose 67 Ga scintigraphy for restaging and treatment follow-up of lymphoma patients. Nucl Med Commun 23:1079–1083
Kostakoglu L, Leonard JP, Kuji I, Coleman M, Vallabhajosula S, Goldsmith SJ (2002) Comparison of fluorine-18 fluorodeoxyglucose positron emission tomography and Ga-67 scintigraphy in evaluation of lymphoma. Cancer 94:879–888
Juweid ME, Wiseman GA, Vose JM, Ritchie JM, Menda Y, Wooldridge JE, Mottaghy FM, Rohren EM, Blumstein NM, Stolpen A, Link BK, Reske SN, Graham MM, Cheson BD (2005) Response assessment of aggressive non-Hodgkin’s lymphoma by integrated International Workshop Criteria and fluorine-18-fluorodeoxyglucose positron emission tomography. J Clin Oncol 23:4652–4661
Thompson CA, Charlson ME, Schenkein E, Wells MT, Furman RR, Elstrom R, Ruan J, Martin P, Leonard JP (2010) Surveillance CT scans are a source of anxiety and fear of recurrence in long-term lymphoma survivors. Ann Oncol 21:2262–2266
Armitage JO, Loberiza FR (2006) Is there a place for routine imaging for patients in complete remission from aggressive lymphoma? Ann Oncol 17:883–884
Acknowledgments
This work was supported by the Department of Health, Taiwan (grant number: DOH99-TD-C-111-006).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lin, TL., Kuo, MC., Shih, LY. et al. Value of surveillance computed tomography in the follow-up of diffuse large B-cell and follicular lymphomas. Ann Hematol 91, 1741–1745 (2012). https://doi.org/10.1007/s00277-012-1508-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-012-1508-0