Abstract
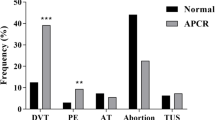
Venous thromboembolism (VTE), including deep venous thrombosis (DVT) and pulmonary embolism (PE), occurs secondary to a number of hereditary and acquired disorders of hemostasis. A recently recognized polymorphism in Factor V (FV) gene H1299R (also named HR2) has been reported to be a possible risk factor for the development of VTE. The aim of this study is to evaluate the role of HR2 polymorphism in VTE in a group of Lebanese patients. Seventy-three VTE patients and 125 healthy subjects were examined for HR2. The average ages for the patients and controls were 45.0 ± 19.1 years and 35.4 ± 18.6 years, respectively. Sixty patients (82.2%) had DVT, eight patients (11%) had PE, and five patients (6.8%) had both. There was significant association between FV Leiden and VTE (p < 0.001). HR2 haplotype had a prevalence of 16.4% in patients. VTE patients with normal FV were 2.7 times more likely to have the HR2 haplotype as compared to controls with normal FV (p = 0.036, 95% CI = 1.04–7.06). We conclude that the FV HR2 haplotype significantly affects the risk of VTE in subjects with normal FV. This finding entails that screening for the HR2 haplotype should be done in VTE patients with normal FV Leiden results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Venous thromboembolism (VTE), including deep venous thrombosis (DVT), more commonly of the lower limbs, and pulmonary embolism (PE), is the formation of an intravascular plug, which partially or completely obstructs blood flow through the affected vessels. VTE is the third most common cardiovascular disease after ischemic heart disease and cerebral stroke [1]. VTE remains a serious disease because it can be fatal. It constitutes a major cause of morbidity and mortality, and it occurs with an incidence of approximately 250,000 cases per year in the United States [2].
VTE occurs secondary to a number of hereditary and acquired disorders of hemostasis including Factor V (FV) Leiden mutation, prothrombin G20210A mutation, protein C deficiency, protein S deficiency, antithrombin deficiency, and the presence of lupus anticoagulant [3]. Other circumstantial conditions can add to the risk of developing VTE, such as pregnancy, use of oral contraceptives, major surgeries, cancer, and long-distance traveling [3, 4]. In fact, many believe that the etiology of VTE is multifactorial. It requires the coexistence of more than one genetic and acquired factor to cause a VTE episode in a patient [5].
Blood coagulation FV is a 330-kDa glycoprotein, activated by thrombin or activated Factor Xa (FXa), which enhances prothrombin activation when complexed with FXa on negatively charged phospholipid surfaces [6]. This leads to the conversion of prothrombin to thrombin. FV is inactivated by protein C (APC), thus regulating the amount of thrombin generated [6]. One of the most common abnormalities is a missense mutation in the FV gene, FV Arg506Gln, known as FV Leiden [7]. This mutation results in the APC resistance phenotype, which is associated with increased risk of VTE [8].
In 1996, a complex haplotype in exon 13 of FV gene (A4070G; His1299Arg) known as R2 was discovered [9]. The R2 polymorphism has been reported to include more than 12 different polymorphisms throughout the gene, which are collectively known as HR2 [10, 11]. Seven of these polymorphisms predict an amino acid change in FV and lead to modifications of the protein. The R2 variation is associated with lowered FV levels and decreased APC ratios. Its association with venous thrombosis has been questioned since some studies reported an increase in thrombotic risk [12], while others observed this association only when co-inherited as a compound heterozygote with the FV Leiden variant [13].
Ethnic variations were highly noted for the HR2 gene polymorphisms. The haplotype is rather frequent, with an allele frequency ranging from 5% to 17% throughout healthy populations from Asia, Australia, Europe, and native African [10, 12, 14–16]. In the Middle East or in the Arab population, studies showed that the prevalence of HR2 haplotype in healthy subjects ranged between 7% and 10.4% [17, 18]. However, the significance of this haplotype has not yet been tested in VTE patients in Lebanon.
Materials and methods
This study was approved by the Scientific Committee for Research Institutional Review Board of the American University of Beirut Medical Center (AUBMC). Seventy-three VTE patients (40 males and 33 females) and 125 healthy subjects (72 males and 53 females) were examined for the HR2 haplotype of FV. The patients were referred between March 2003 and December 2005 to AUBMC, which is a tertiary-care center in Lebanon accommodating patients from the different districts of the country. The control group was randomly selected from donors logged into our HLA registry, and we used their archived DNA material; these represent healthy Lebanese people from different provinces and religious communities of the country. Our control group was previously described in one of our studies [18]. All subjects were of Eastern Mediterranean origin. The average ages for the patients and controls were 45.0 ± 19.1 and 35.4 ± 18.6 years, respectively.
The hospital records for the patients were obtained, and only patients with “definite” VTE events (73 patients) were included in the analysis. The diagnosis of DVT was confirmed by venous Doppler ultrasonography and that of PE by having a positive ventilation–perfusion scan or a positive pulmonary angiogram.
The DNA was originally extracted using the PEL-FREEZ extraction kit (PEL-FREEZ, DYNAL, USA) and stored at −80°C for later use. The CVD StripAssay (ViennaLab, Austria) was used, and its protocol was followed exactly as stated by the manufacturer. This assay screens for several gene mutations, including factor V H1299R (HR2). Briefly, in vitro, the different gene sequences are simultaneously amplified and biotin-labeled in a single amplification reaction (Multiplexing). The thermocycler program consists of an initial step of 94°C for 2 min, followed by 35 cycles of 94°C for 15 s, 58°C for 30 s, 72°C for 30 s, and a final extension step of 72°C for 3 min. The amplification products are selectively hybridized to a test strip, which contains allele-specific (wild type and mutant) oligonucleotide probes immobilized as an array of parallel lines. Bound biotinylated sequences are detected using streptavidin-alkaline phosphatase and color substrates.
Statistical analysis
Chi-square was conducted to compare the genotypes distribution between the patients and controls. When the numbers in one or more of the categories in the contingency table were less than 5, Fisher’s exact test was conducted. p values less than 0.05 were considered to be statistically significant. Odds ratios were calculated when there was significant association between the genotype or allele and the clinical status of the participants.
Results
Sixty patients (82.2%) had DVT, eight patients (11%) had PE, and five patients (6.8%) had both. Ten patients had a history of previous VTE. There was significant association between FV Leiden and VTE (p < 0.001). HR2 haplotype was present in 12 patients (all were heterozygous; allelic frequency of 0.082) and 13 healthy subjects (11 heterozygous and two homozygous; allelic frequency of 0.060), with a prevalence of 16.4% and 10.4%, respectively (p = 0.159).
VTE patients with normal FV were 2.7 times more likely to have the HR2 haplotype as compared to controls with normal FV (p = 0.036, 95% CI = 1.04–7.06). Among the patients who had the HR2 haplotype, three patients had the FV G1691A mutation, one had the prothrombin G20210A mutation, and three were homozygous for the methylenetetrahydrofolate reductase (MTHFR) C677T mutation. Three patients had the HR2 haplotype as the only genetic mutation. The distribution of the inherited thrombophilia among the patients and the controls is shown in Table 1. The distribution of patients and controls with respect to FV and FV HR2 is shown in Table 2. The results of HR2 haplotype and other thrombophilic mutations among VTE patients are shown in Table 3.
Discussion
The pathogenesis of venous thrombosis is multifactorial, involving acquired and genetic factors. In addition to predisposing factors like surgery, pregnancy, and malignancy, genetic predisposition due to molecular abnormalities of components of the coagulation pathway has been found in subjects who had suffered from thromboembolic disease [19]. Although the knowledge of a series of major risk factors for venous thrombosis has been greatly improved, the pathogenesis of many thrombotic events remains unclear, suggesting the possibility of the presence of other yet unknown risk factors [20].
The FV marked by the HR2 haplotype has been shown to contribute by itself to an increased activated protein C (APC) resistance both in normal and thrombophilic patients, independent of the status of FV Leiden carriership [10]. The coinheritance of HR2 and FV Leiden can be associated with severe APC resistance phenotype [21]. Previous studies have shown that the presence of the HR2 haplotype is associated with increased risk of VTE (two- to three-fold) [9, 12, 20–22]. This is in contrast to other studies in which HR2 by itself is not a risk factor for developing VTE [10, 13, 14].
This study investigated VTE risk associated with FV. In our study, the frequency of the FV HR2 haplotype in Lebanese patients with VTE was identical to that found in patients of the same ethnicity in Kuwait [17]. Twelve patients (16.4%) had the HR2 haplotype, all of whom were heterozygous for the mutation. There was significant association between FV Leiden and VTE (p < 0.001). Furthermore, we found coexistence of more than one risk factor in the same patient in 30 (41.1%) of our cases. Such coexistence may add up to the individual risk encountered by each factor alone. In regard to HR2, this haplotype has been found to coexist with other genetic risk factors in six of our cases, half of which were associated with FV Leiden. Other studies have shown such high correlation between HR2 haplotype and FV Leiden mutation [11, 13, 21, 23], with an added risk of three-fold in some studies [11, 13]. Few other studies did not find such association or risk [10, 14]. In our study, no increase in risk of VTE could be demonstrated when the HR2 haplotype was associated with any other inherited thrombophilic defect.
The HR2 haplotype was found to be the only abnormality in three (4.1%) of our patients. It is interesting to report that 11 (15.1%) of 73 cases studied here did not show any genetic mutation. Further investigations are needed to explore other possible unknown defects in these patients. Most important, VTE patients with normal FV were 2.7 times more likely to have the HR2 haplotype as compared to controls with normal FV (p = 0.036, 95% CI = 1.04–7.06).
We conclude that the FV HR2 haplotype significantly affects the risk of VTE in subjects with normal FV. This finding entails that screening for the HR2 haplotype should be considered in VTE patients with normal FV. Moreover, this haplotype may coexist with other thrombophilic mutations. Further larger studies are needed to be conducted in the Lebanese population in order to confirm the importance of screening patients with VTE for the HR2 haplotype.
References
Kniffin WD Jr, Baron JA, Barrett J, Birkmeyer JD, Anderson FA Jr (1994) The epidemiology of diagnosed pulmonary embolism and deep venous thrombosis in the elderly. Arch Intern Med 154:861–866 doi:10.1001/archinte.154.8.861
White RH (2003) The epidemiology of venous thromboembolism. Circulation 107(23):I4–I8 doi:10.1161/01.CIR.0000078468.11849.66
Simioni P, Tormene D, Spiezia L, Tognin G, Rossetto V, Radu C et al (2006) Inherited thrombophilia and venous thromboembolism. Semin Thromb Hemost 32:700–708 doi:10.1055/s-2006-951298
Pymar HC, Creinin MD (2001) The risks of oral contraceptive pills. Semin Reprod Med 19:305–312 doi:10.1055/s-2001-18638
Koeleman BP, Reitsma PH, Bertina RM (1997) Familial thrombophilia: a complex genetic disorder. Semin Hematol 34:256–264
Rosing J, Tans G, Govers-Riemslag JW, Zwaal RF, Hemker HC (1980) The role of phospholipids and factor Va in the prothrombinase complex. J Biol Chem 255:274–283
Bertina RM, Koeleman BP, Koster T, Rosendaal FR, Dirven RJ, de Ronde H et al (1994) Mutation in blood coagulation factor V associated with resistance to activated protein C. Nature 369:64–67 doi:10.1038/369064a0
Bertina RM, Reitsma PH, Rosendaal FR, Vandenbroucke JP (1995) Resistance to activated protein C and factor V Leiden as risk factors for venous thrombosis. Thromb Haemost 74:449–453
Lunghi B, Iacoviello L, Gemmati D, Dilasio MG, Castoldi E, Pinotti M et al (1996) Detection of new polymorphic markers in the factor V gene: association with factor V levels in plasma. Thromb Haemost 75:45–48 doi:10.1159/000134455
Bernardi F, Faioni EM, Castoldi E, Lunghi B, Castaman G, Sacchi E et al (1997) A factor V genetic component differing from factor V R506Q contributes to the activated protein C resistance phenotype. Blood 90:1552–1557
Castoldi E, Rosing J, Girelli D, Hoekema L, Lunghi B, Mingozzi F et al (2000) Mutations in the R2 FV gene affect the ratio between the two FV isoforms in plasma. Thromb Haemost 83:362–365
Alhenc-Gelas M, Nicaud V, Gandrille S, van Dreden P, Amiral J, Aubry ML et al (1999) The factor V gene A4070G mutation and the risk of venous thrombosis. Thromb Haemost 81:193–197
Faioni EM, Franchi F, Bucciarelli P, Margaglione M, De Stefano V, Castaman G et al (1999) Coinheritance of the HR2 haplotype in the factor V gene confers an increased risk of venous thromboembolism to carriers of factor V R506Q (factor V Leiden). Blood 94:3062–3066
Luddington R, Jackson A, Pannerselvam S, Brown K, Baglin T (2000) The factor V R2 allele: risk of venous thromboembolism, factor V levels and resistance to activated protein C. Thromb Haemost 83:204–208
Benson JM, Ellingsen D, El-Jamil M, Jenkins M, Miller CH, Dilley A et al (2001) Factor V Leiden and factor V R2 allele: high-throughput analysis and association with venous thromboembolism. Thromb Haemost 86:1188–1192
Kostka H, Schwarz T, Schellong S, Mix C, Kuhlisch E, Temelkova-Kurktschiev T et al (2003) Coagulation factor V G allele and HR2 haplotype: factor V activity, activated protein C resistance and risk of venous thrombosis. Blood Coagul Fibrinolysis 14:49–56 doi:10.1097/00001721-200301000-00009
Jadaon MM, Dashti AA (2005) HR2 haplotype in Arab population and patients with venous thrombosis in Kuwait. J Thromb Haemost 3:1467–1471 doi:10.1111/j.1538-7836.2005.01326.x
Zaatari GS, Otrock ZK, Sabbagh AS, Mahfouz RA (2006) Prevalence of factor V R2 (H1299R) polymorphism in the Lebanese population. Pathology 38:442–444 doi:10.1080/00313020600922934
De Stefano V, Finazzi G, Mannucci PM (1996) Inherited thrombophilia: pathogenesis, clinical syndromes, and management. Blood 87:3531–3544
Margaglione M, Bossone A, Coalizzo D, D’Andrea G, Brancaccio V, Ciampa A et al (2002) FV HR2 haplotype as additional inherited risk factor for deep vein thrombosis in individuals with a high-risk profile. Thromb Haemost 87:32–36
Castaman G, Lunghi B, Missiaglia E, Bernardi F, Rodeghiero F (1997) Phenotypic homozygous activated protein C resistance associated with compound heterozygosity for Arg506Gln (factor V Leiden) and His1299Arg substitutions in factor V. Br J Haematol 99:257–261 doi:10.1046/j.1365-2141.1997.3993213.x
Faioni EM, Castaman G, Asti D, Lussana F, Rodeghiero F (2004) Association of factor V deficiency with factor V HR2. Haematologica 89:195–200
Castaman G, Faioni EM, Tosetto A, Bernardi F (2003) The factor V HR2 haplotype and the risk of venous thrombosis: a meta-analysis. Haematologica 88:1182–1189
Author information
Authors and Affiliations
Corresponding author
Additional information
No conflicts of interest. No source of funding.
Rights and permissions
About this article
Cite this article
Otrock, Z.K., Taher, A.T., Shamseddeen, W.A. et al. Factor V HR2 haplotype: a risk factor for venous thromboembolism in individuals with absence of Factor V Leiden. Ann Hematol 87, 1013–1016 (2008). https://doi.org/10.1007/s00277-008-0543-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-008-0543-3