Abstract
The present meta-analysis was undertaken to (1) assess erythroid response rates in myelodysplastic syndromes (MDS) patients treated with epoetin alfa as a monotherapy, (2) gain further insights into predictors of response rates, and (3) compare the erythroid response rates observed with epoetin alfa and darbepoetin alfa. A systematic review of studies from 1990 to 2006 in MDS patients treated with epoetin alfa or darbepoetin alfa was performed and yielded 30 studies evaluating a total of 1,314 patients (epoetin alfa: 22 studies, 925 patients; darbepoetin alfa: eight studies, 389 patients). Pooled estimates of erythroid response rates, stratified by the International Working Group criteria (IWGc) and treatment group, were calculated using random-effects meta-analysis methods. Univariate meta-regression analyses were further conducted to identify study characteristics associated with erythroid response rate. The pooled estimate of erythroid response rate was significantly higher for epoetin alfa IWGc studies (57.6%) as compared to non-IWGc studies (31.6%; p < 0.001). Study factors predictive of higher response rate in the epoetin alfa IWGc studies included higher proportion of patients with RA/RARS (p < 0.001), lower mean baseline serum erythropoietin level (p = 0.007), and fixed dosing regimen (p < 0.001). There was no significant difference in the pooled erythroid response rates between the two agents (epoetin alfa: 57.6% vs. darbepoetin alfa: 59.4%; p = 0.828). The current study reported significantly higher erythroid response rates predominantly in the more recent studies that primarily utilized IWGc to define response. With the use of standardized patient selection and response evaluation methods, epoetin alfa and darbepoetin alfa yielded comparable erythroid response rates in MDS patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Myelodysplastic syndromes (MDS) represent a heterogeneous group of clonal bone marrow stem cell disorders characterized by abnormal proliferation and differentiation of hematopoietic precursors resulting in ineffective hematopoiesis, refractory cytopenias, and a propensity to evolve into acute myeloid leukemia (AML) [1–3].
Patient prognosis and risk of progression to AML can be predicted by the International Prognostic Scoring System (IPSS) for MDS, which is based on the presence or absence of multilineage cytopenias, abnormal marrow cytogenetics, and increased marrow blast counts [4]. The only curative option is allogeneic hematopoietic stem cell transplantation. However, this procedure is limited by donor availability and significant toxicity, especially in the older population, which MDS commonly afflicts. Furthermore, for patients with low or intermediate-1 IPSS scores, several other approaches than hematopoietic transplantation are preferred [5]. Secondly, most patients in the lower risk categories die from causes other than leukemia [6]. In these patients, the course of disease is marked by prolonged survival with chronic cytopenias and infrequent evolution to AML. As such, for a great majority of MDS patients, the goal of disease management is to treat the complications of cytopenia with supportive care for anemia and thrombocytopenia, and antimicrobial therapy for infectious complications. Furthermore, for this largely incurable disease, improving quality of life is an important goal [7].
Anemia, the clinical hallmark of this disease, is present in up to 80–85% of MDS patients at diagnosis, and may also develop during the course of the disease, often necessitating blood transfusions [1]. Unfortunately, repeated transfusions of red blood cells are associated with infectious complications, iron overload, and more importantly, appear to be associated with decreased survival and leukemic evolution in patients with MDS, although that finding might be confounded with worse underlying health status in patients requiring transfusions [6]. Furthermore, transfusion therapy places great strain on the limited donor blood supply, which faces daily challenges of collection, processing, and distribution [8–10].
Recombinant human erythropoietin (epoetin alfa), administered either alone or in combination with granulocyte or granulocyte–macrophage colony-stimulating factors (G-CSF or GM-CSF), has been extensively studied as a means to improve erythropoiesis [11] and reduce red blood cell transfusions in MDS patients with anemia [12–14].
Historically, the use of epoetin alfa in patients with MDS from heterogeneous populations, and more importantly, the absence of standardized response evaluation methods, led to a tremendous variability in reported erythroid response rates to epoetin alfa monotherapy in published literature. In the late 1990s, it was found that patients with low to intermediate-1 (INT-1) disease with low transfusion requirements and lower endogenous serum erythropoietin levels may show the best response to epoetin alfa and thus may be better candidates for erythropoietic therapy [15–17]. Recently, another erythropoiesis-stimulating agent (ESA), darbepoetin alfa, has also been shown to be effective in the treatment of MDS-related anemia [18–20]. In 2000, the International Working Group conducted a review of currently used response definitions and introduced a uniform set of criteria for assessing response in future clinical trials in MDS [7]. These standardized criteria were developed in an effort to improve communication among investigators and to allow comparability among clinical trials. The advent of the International Working Group criteria (IWGc), and revision in 2006, should better enable the comparison of erythroid response rates to erythropoietic therapy [7].
The purpose of the present meta-analysis was: (1) to assess erythroid response rates in MDS patients treated with epoetin alfa as a monotherapy in studies that did and did not use the IWGc, (2) to gain further insights into predictors of response rates, and (3) to compare the erythroid response rates observed with epoetin alfa and darbepoetin alfa when adjusted for the IWGc.
Materials and methods
Literature search
A systematic search of the medical literature was conducted for studies of epoetin alfa or darbepoetin alfa in patients with MDS for the period 1990 to 2006 using the PubMed database. The search was performed using the following keywords: “epoetin alfa or rHuEPO or darbepoetin alfa or novel erythropoiesis stimulating protein” & “myelodysplastic syndromes”. An additional search for abstracts from the American Society of Clinical Oncology (ASCO) and the American Society of Hematology (ASH) proceedings was also conducted. Results of the search were initially analyzed in title and abstract format. Reference sections from the selected publications were checked for additional articles or abstracts. Items were selected based on an initial search for a full-text analysis to determine the eligibility of the article for our analysis.
Criteria for inclusion of studies for analysis
All studies and abstracts that evaluated the effectiveness of epoetin alfa or darbepoetin alfa as a monotherapy for the treatment of MDS-related anemia were included. The only additional criterion applied was the availability of erythroid response to assess treatment effectiveness in patients naive to erythropoietic treatment. Studies reported in languages other than English were included in this review if the relevant data for the analysis were available from the abstract. Figure 1 summarizes the study disposition.
Data extraction
Two reviewers independently assessed the quality of the data collected using a standardized methodology. Each reviewer evaluated relevant data from the eligible studies and entered the information electronically into a Microsoft Excel data collection form with pre-specified fields. If relevant data were reported only graphically, values were estimated by measuring the charts. Quality control was done by comparing the two independent datasets and any differences were reconciled by a third party, referring to the original sources.
Information regarding the study design and outcomes were collected for each included study. This included the number of patients enrolled, relevant aspects of study design (e.g., definition of erythroid response), baseline characteristics of patients, dosing regimen, and erythroid response rate.
Analytical approach
Studies included in the analysis were stratified by the use or non-use of IWGc erythroid response definition and by treatment group. An attempt was made to recalculate response rates in non-IWGc studies according to the IWGc definition; however, the non-IWGc studies did not provide enough detailed information to reconcile the data. For this reason, in the first objective, epoetin alfa studies using IWGc to define erythroid response were compared to epoetin alfa studies using a different definition of erythroid response (non-IWGc studies). For the second objective, univariate meta-regression analysis was performed using epoetin alfa IWGc studies to identify the potential baseline predictors for response rate. For the third objective, response rates between epoetin alfa and darbepoetin alfa were compared when adjusted for the IWGc. Since all darbepoetin alfa studies included in the analysis used IWGc to define erythroid response, this comparison was based solely on epoetin alfa studies also utilizing IWGc. Since none of the studies used the recent modified IWGc criteria [21], only the original IWGc criteria were used as described below [7].
Erythroid response rate was the outcome measure for these meta-analyses. For IWGc studies, erythroid response was defined as major (i.e., increase of >2 g/dL in Hb level from baseline in patients with a hemoglobin of ≤11g/dL or transfusion independence for transfusion-dependent patients) plus minor (i.e., increase of 1–2 g/dL in Hb level from baseline in patients with a hemoglobin of ≤11 g/dL or 50% reduction in transfusion requirements for transfusion-dependent patients). For the non-IWGc studies, hematologic response rate definitions were variable and included: favorable response, complete response, and partial response (Table 1).
Univariate baseline statistics were generated for epoetin alfa and darbepoetin alfa studies. Frequency counts and percentages were used to summarize categorical variables while means and standard deviations were used for continuous variables. Statistical comparisons between groups were conducted using chi-square tests for categorical variables and two-sided Student’s t tests for continuous variables.
Meta-analysis
Pooled estimates of erythroid response rates and 95% confidence intervals (CI) were calculated and plotted for each group using random-effects meta-analysis methods [22]. Under the random-effects model, it is assumed that in addition to variability within studies, there is also variability among studies. This among-study variability was assessed using the I-squared statistic (i.e., variation attributable to heterogeneity) and tested by the heterogeneity test where a low p value implies that the study results are heterogeneous and a random-effects model, instead of a fixed-effects model is more appropriate. In addition, univariate meta-regression analyses were conducted, with supplemental descriptive statistics, to identify study characteristics that were significant determinants of erythroid response rate using epoetin alfa IWGc studies.
A two-sided alpha error of 0.05 was used to declare statistical significance. All statistical analyses were performed using SAS release 9.1 or newer (SAS Institute, Inc., Cary, NC, USA) or Intercooled Stata 9.0 software.
Results
Selection of studies
The initial search yielded 79 studies from Medline, ASCO/ASH meeting proceedings, or the references sections of identified Medline publications. A total of 30 studies [11, 12, 15, 17–20, 23–44] were included in the current analysis (Fig. 1). Reviews of existing literature, interim or duplicate reports (n = 21), and editorials, letters to the editor, practice guidelines, or case reports (n = 14) were excluded. In addition, studies not using ESA as monotherapy (n = 6), those for which erythroid response rate or standard deviation were not available (n = 5), and studies evaluating erythropoietic agents for an indication other than MDS (n = 3) were also excluded. The remaining study set included 22 unique epoetin alfa studies with non-overlapping patient populations (13 non-IWGc and nine IWGc studies) and eight studies using darbepoetin alfa (all IWGc studies).
Erythroid response to epoetin alfa monotherapy
A total of 925 patients receiving epoetin alfa were evaluable for erythroid response (589 IWGc and 336 non-IWGc). Table 2 describes the baseline characteristics for those patients evaluated for response using non-IWGc vs. IWGc. Of note, the proportion of transfusion-dependent patients at baseline was significantly higher in the non-IWGc group compared to the IWGc group (82% vs. 36%, respectively, p < 0.001).
The pooled erythroid response rate from the meta-analysis based on a random-effects model using all epoetin alfa studies, including both non-IWGc and IWGc studies, was estimated at 43.9% (95% CI: 35.3–52.4%). The high I-squared value indicated the presence of heterogeneity across studies (I-squared: 85.1%) and the chi-square test for heterogeneity was statistically significant (p < 0.001), justifying the choice of the random-effects model. As expected, the estimate of erythroid response rate was significantly higher for the IWGc studies (57.6%, 95% CI: 45.1–70.0%) as compared to the non-IWGc studies (31.6%, 95% CI: 24.9–38.4%; p < 0.001), which demonstrate the importance of adjusting for IWGc in comparing erythroid response rates between epoetin alfa and darbepoetin alfa.
Baseline disease characteristics and treatment regimens predictive of response in MDS
To identify study characteristics predictive of a higher erythroid respond rate in epoetin alfa IWGc studies, the univariate meta-regression analysis was performed. This analysis showed that a higher proportion of patients with refractory anemia or refractory anemia with ringed sideroblasts (RA/RARS; p < 0.001), a lower mean baseline serum erythropoietin level (p = 0.007), and receipt of a fixed dosing regimen compared to a weight-based regimen (p < 0.001) were significant study characteristic predictors of higher response rates. Other factors that did not have a significant impact on erythroid response rate included baseline hemoglobin level (p = 0.375). In studies where data were available, the weighted average time since diagnosis was significantly shorter for the IWGc studies as compared to the non-IWGc studies (Table 3).
Comparison of erythroid response rates between epoetin alfa and darbepoetin alfa
Nine epoetin alfa studies (N = 619 patients; N evaluable = 589) and eight darbepoetin alfa studies (N = 442 patients; N evaluable = 389) using IWGc to define erythroid response were identified for the analysis. Table 4 describes the baseline characteristics of patients treated with epoetin alfa vs. darbepoetin alfa. Baseline characteristics were similar between the two groups with respect to age, gender, proportion of patients with refractory anemia or refractory anemia with ringed sideroblasts, transfusion dependency rates, and mean baseline hemoglobin level. However, the mean baseline serum erythropoietin level was significantly higher in the epoetin alfa group than the darbepoetin alfa group (376 vs. 133 mU/mL, p = 0.003). The average initial weekly dose in the epoetin alfa studies was 47,851 U (range 30,000–80,000 U), while that in the darbepoetin alfa studies was 176 mcg (range 100–315 mcg).
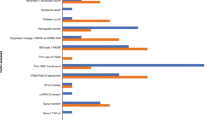
Figure 2a and b show that there was no significant difference in the pooled estimate of the erythroid response rates for either ESA (57.6%, 95% CI: 45.1–70.0% for the epoetin alfa studies vs. 59.4%, 95% CI: 49.0–69.9% for the darbepoetin alfa studies; p = 0.8282). Furthermore, as shown in Fig. 3, when compared to the studies using standard weekly doses of epoetin alfa (30,000–40,000 U; five studies, 393 patients), those studies using higher dosing regimens (60,000–80,000 U; n = 4 studies, 196 patients) showed a significantly higher erythroid response rate (47.8% vs. 63.3%, respectively, p < 0.001). A similar dose relationship was also observed in the darbepoetin alfa group for studies using 100–150 mcg (four studies, 154 patients) vs. studies using 166–300 mcg (four studies, 235 patients; 52.6% vs. 71.1%, respectively, p < 0.001, Fig. 3). No statistically significant difference was noted when erythroid response rates were compared between the two ESAs at corresponding dosing regimens.
a Overall erythroid response rates for epoetin alfa studies using IWGc. Notes: Box symbol denotes point estimate of response rate proportional to the study weight used to pool the results. Line symbol indicates the 95% confidence interval of response rate. b Overall erythroid response rates for darbepoetin alfa studies (all using IWGc). Notes: Box symbol denotes point estimate of response rate proportional to the study weight used to pool the results. Line symbol indicates the 95% confidence interval of response rate
Discussion
The present meta-analysis, using a comprehensive list of epoetin alfa and darbepoetin alfa studies, demonstrated higher erythroid response rates predominantly in the more recent studies that utilized IWGc to define response.
By contrast, the overall low erythroid response rate (31.6%) found in non-IWGc studies is similar to the modest efficacy of epoetin alfa observed in the first meta-analysis by Hellstrom-Lindberg in 1995 [16]. Comparatively little was known about MDS biology at the time of that publication. However, recently, greater refinement occurred in the treatment of these disorders. Noteworthy was the development of standardized response criteria, the IWG criteria, which permitted the comparison of efficacy of different agents in these rather diverse set of disorders. Additionally, the patient selection model proposed by Hellstrom-Lindberg et al. has defined the subset of patients that are most likely to benefit from ESA monotherapy or in combination with G-CSF and would thus be the best candidates for ESA therapy. According to the aforementioned model, endogenous serum erythropoietin levels ≤500 mU/mL and transfusion requirement of <2 packed red blood cell units per month are predictive of improved response to ESA [45]. The present meta-analysis supports these findings as evidenced by the percentage of transfusion-dependent patients being significantly higher in non-IWGc studies where, as mentioned above, response rates were lower as well. Therefore, although higher erythroid response rates in the IWGc group likely reflect inherent differences in the response definitions favoring the IWGc group, the improvement in response is perhaps a compound result of standardized criteria and more refined patient selection (i.e., inclusion of less severely ill patients in studies) over time. Further, the observation of higher response rates in studies incorporating a greater proportion of patients with RA/RARS is consistent with studies that found that epoetin alfa works best in lower risk patients [15, 17, 46]. Furthermore, our results provide further insights into the hypothesis that patients with disease of shorter duration are more likely to respond to epoetin alfa [17]. It is possible, however, that the effect of disease duration in our study might be sustained by other confounding factors, such as the observed proportion of transfusion-dependent patients at baseline. Therefore, the results from our meta-regression analysis should be interpreted cautiously because of lack of individual data.
Studies using darbepoetin alfa reported erythroid response rates similar to those seen with epoetin alfa when the two ESAs were compared on the basis of IWGc. Moreover, both ESAs seem to yield higher but comparable erythroid response rates with the use of higher weekly doses (60,000–80,000 U for epoetin alfa and 166–300 mcg for darbepoetin alfa). When epoetin alfa and darbepoetin alfa studies were compared based on utilization of IWGc, relatively lower endogenous erythropoietin levels (376 vs. 133 mU/mL, p = 0.003) were found on studies involving darbepoetin alfa. Interestingly however, the erythroid response rates were comparable to those in the epoetin alfa studies, supporting the cut-off point of 500 mU/mL of endogenous erythropoietin used by the predictive model described above.
Higher dosing regimens of both epoetin alfa (weekly dose 60–80 K U) and darbepoetin alfa (weekly dose 166–300 mcg) were associated with improved erythroid responses. The optimal dose of either ESA for MDS remains to be determined and perhaps a prospective randomized dose finding study is warranted for both agents.
This study similar to meta-analyses in general has limitations. First, only epoetin alfa studies were considered for the present analysis. Studies using epoetin beta, an ESA not available in the United States, were not included because of the very small number of available reports with this agent. Secondly, studies, although few, were included from peer-reviewed abstracts/posters. A differential distribution of such reports in different study groups may introduce an information bias. In the present analysis, 4/8 darbepoetin alfa studies were in the abstract/poster form as compared to 1/9 IWG epoetin alfa studies. Thirdly, although meta-analysis has the ability to improve the power of small or inconclusive studies, it cannot improve the quality or reporting of the original studies. Fourthly, the lack of primary source data from the original studies is also a further limitation to the analysis, as ecological bias may influence results [47]. In this analysis, the original studies were weighted based on the method of DerSimonian and Laird [22], which tends to favor studies with a larger sample size. However, the quality of the original studies (e.g., randomized vs. observational design) was not considered. Lastly, the total number of epoetin alfa and darbepoetin alfa studies in MDS is relatively small and data regarding reported durations of follow-up are limited, suggesting that these results be considered as hypothesis generating. Further head-to-head randomized trials are necessary to compare the validity of the present results regarding efficacy of epoetin alfa and darbepoetin alfa in MDS.
Safety endpoints were not assessed in this meta-analysis. When ESAs are used according to product labeling in the setting of chemotherapy-induced anemia (target hemoglobin not to exceed 12 g/dL), no effect on survival or other tumor outcomes has been observed [48, 49]. Recent safety signals that have emerged in cancer studies have all been related to investigational uses (treatment beyond correction of anemia, “anemia of cancer”, and potentiation of head and neck cancer radiotherapy). Interestingly, there are recent retrospective reports suggesting that for MDS, the use of ESAs as monotherapy or in combination with G-CSF, is associated with improved survival [50–53]. This is plausible considering the possible impact of transfusion and related iron overload on survival in MDS patients [6, 54, 55]. Furthermore, transfusion-dependent patients are likely to have lower Hb values than non-transfusion-dependent patients, and anemia has been shown to be a significant risk factor for both survival and cardiovascular diseases [4, 56]. It is not unreasonable to speculate that ESAs, by reducing transfusion dependency and correcting anemia, may positively impact survival. However, the counterargument is that transfusion dependence in itself is likely to be an indicator of more severe disease and, as such, it is unlikely that ESAs would reduce the risk of leukemic evolution [54]. On the other hand, it is worthwhile to note that in lower risk MDS, causes of death are not only related to leukemia but also include predominant nonleukemic causes such as cardiac complications (50%), infectious diseases (30%), bleeding (8%), and liver failure (8%) [6]. The causes of death, with the exception of thrombocytopenia-related bleeding, are similar to those found in other disease states such as the thalassemias where chronic transfusion results in iron overload [57, 58]. However, the true risk benefit assessment of ESAs in MDS can only be evaluated in prospective well-designed randomized placebo-controlled studies.
Conclusion
This meta-analysis of patients with MDS treated with epoetin alfa showed significantly higher erythroid response rates over time, particularly in studies utilizing IWGc to define response. The main reason for this finding is improved patient selection and standardized response criteria over time. The current analysis also demonstrated that, in studies using standardized patient selection and response evaluation methods, epoetin alfa and darbepoetin alfa yielded comparable erythroid response rates in anemic MDS patients. Prospective randomized clinical studies are required to evaluate the long-term benefit and safety of ESAs in MDS.
References
Steensma DP, Bennett JM (2006) The myelodysplastic syndromes: diagnosis and treatment. Mayo Clin Proc 81:104–130
Catenacci DV, Schiller GJ (2005) Myelodysplastic syndromes: a comprehensive review. Blood Rev 19:301–319
Hellstrom-Lindberg E (2005) Management of anemia associated with myelodysplastic syndromes. Semin Oncol 42(2 Suppl 1):S10–S13
Greenberg P, Cox C, LeBeau MM et al (1997) International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood 89(6):2079–2088
Cutler CS, Lee SJ, Greenberg P et al (2004) A decision analysis of allogeneic bone marrow transplantation for the myelodysplastic syndromes: delayed transplantation for low-risk myelodysplasia is associated with improved outcome. Blood 104(2):579–585
Malcovati L, Porta MG, Pascutto C et al (2005) Prognostic factors and life expectancy in myelodysplastic syndromes classified according to WHO criteria: a basis for clinical decision making. J Clin Oncol 23:7594–7603
Cheson BD, Bennett JM, Kantarjian H et al (2000) Report of an international working group to standardize response criteria for myelodysplastic syndromes. Blood 96:3671–3674
Goodman C, Chan S, Collins P, Haught R, Chen YJ (2003) Ensuring blood safety and availability in the U.S.: technological advances, costs, and challenges to payment—final report. Transfusion 43:3S–46S
Pitocco C, Sexton TR (2005) Alleviating blood shortages in a resource-constrained environment. Transfusion 45:1118–1126
Blood collection and transfusion in the United States in 1999. Available from URL: http://www.sabm.org/news/detail.php?id=193. Accessed 11 Jul 2007
Italian Cooperative Study Group For rHuEpo in Myelodysplastic Syndromes (1998) A randomized double-blind placebo-controlled study with subcutaneous recombinant human erythropoietin in patients with low-risk myelodysplastic syndromes. Br J Haematol 103:1070–1074
Terpos E, Mougiou A, Kouraklis A et al (2002) Prolonged administration of erythropoietin increases erythroid response rate in myelodysplastic syndromes: a phase II trial in 281 patients. Br J Haemato 118:174–180
Casadevall N, Durieux P, Dubois S et al (2004) Health, economic, and quality-of-life effects of erythropoietin and granulocyte colony-stimulating factor for the treatment of myelodysplastic syndromes: a randomized, controlled trial. Blood 104:321–327
Thompson JA, Gilliland DG, Prchal JT et al (2000) Effect of recombinant human erythropoietin combined with granulocyte/macrophage colony-stimulating factor in the treatment of patients with myelodysplastic syndrome. GM/EPO MDS Study Group. Blood 95:1175–1179
Stenke L, Wallvik J, Celsing F, Hast R (1993) Prediction of response to treatment with human recombinant erythropoietin in myelodysplastic syndromes. Leukemia 7:1324–1327
Hellstrom-Lindberg E (1995) Efficacy of erythropoietin in the myelodysplastic syndromes: a meta-analysis of 205 patients from 17 studies. Br J Haematol 89:67–71
Di Raimondo F, Longo G, Cacciola EJR et al (1996) A good response rate to recombinant erythropoietin alone may be expected in selected myelodysplastic patients. A preliminary clinical study. Eur J Haematol 56:7–11
Musto P, Lanza F, Balleari E et al (2004) Darbepoetin alfa for the treatment of anaemia in low-intermediate risk myelodysplastic syndromes. Br J Haematol 128:204–209
Patton JF, Sullivan T, Mun Y, Reeves T, Rossi G, Wallace JF (2005) A retrospective cohort study to assess the impact of therapeutic substitution of darbepoetin alfa for epoetin alfa in anemic patients with myelodysplastic syndrome. J Support Oncol 3:419–426
Mannone L, Gardin C, Quarre MC et al (2006) High-dose darbepoetin alpha in the treatment of anaemia of lower risk myelodysplastic syndrome results of a phase II study. Br J Haematol 133:513–519
Cheson DB, Greenberg PL, Bennett JM et al (2006) Clinical application and proposal for modification of the International Working Group (IWG) response criteria in myelodysplasia. Blood 108:419–425
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7(3):177–188
Stasi R, Brunetti M, Bussa S et al (1997) Response to recombinant human erythropoietin in patients with myelodysplastic syndromes. Clin Cancer Res 3:733–739
Rigolin GM, Porta MD, Bigoni R et al (2002) rHuEpo administration in patients with low-risk myelodysplastic syndromes: evaluation of erythroid precursors response by fluorescence in situ hybridisation on May–Grunwald–Giemsa-stained bone marrow samples. Br J Haematol 119:652–659
Clavio M, Nobili F, Balleari E et al (2004) Quality of life and brain function following high-dose recombinant human erythropoietin in low-risk myelodysplastic syndromes: a preliminary report. Eur J Haemaol 72:113–120
Mele G, Musto C, Vigliotti ML et al (2004) High-dose of epoetin alfa in patients with low-risk myelodysplastic syndromes (MDS): a single institution experience. Blood 140(11) [Abstract]
Aloe Spiriti MA, Latagliata R, Niscola P et al (2005) Impact of a new dosing regimen of epoetin alfa on quality of life and anemia in patients with low-risk myelodysplastic syndrome. Ann Hematol 84:167–176
Stein RS, Abels RI, Krantz SB (1991) Pharmacologic doses of recombinant human erythropoietin in the treatment of myelodysplastic syndromes. Blood 78(7):1658–1663
Adamson JW, Schuster M, Allen S, Haley NR (1992) Effectiveness of recombinant human erythropoietin therapy in myelodysplastic syndromes. Acta Haematol 87(Suppl 1):20–24
Rafanelli R, Grossi A, Longo G, Vannucchi AM, Bacci R, Ferrini PR (1992) Recombinant human erythropoietin for treatment of myelodysplastic syndromes. Leukemia 6(4):323–327
Verhoef GEG, Zachée A, Demuynck H et al (1992) Recombinant human erythropoietin for the treatment of anemia in the myelodysplastic syndromes: a clinical and erythrokinetic assessment. Ann Hematol 64:16–21
Aloe Spiriti MA, Petti MC, Latagliata R et al (1993) Is recombinant human erythropoietin treatment in myelodysplastic syndromes worthwhile? Leuk Lymphoma 9:79–83
Goy A, Belanger C, Casadevall N et al (1993) High doses of intravenous recombinant erythropoietin for the treatment of anaemia in myelodysplastic syndromes. Br J Haematol 84:232–237
Ludwig H, Fritz E, Leitgeb C et al (1993) Erythropoietin treatment for chronic anemia of selected hematological malignancies and solid tumors. Ann Oncol 4:161–167
Zeigler ZR, Jones D, Rosenfeld CS, Shadduck RK (1993) Recombinant human erythropoietin (rHuEPO) for treatment of myelodysplastic syndromes. Stem Cells 11:49–55
Marques da Costa R (1994) Current use of recombinant human erythropoietin (r-huEPO) in the management of symptomatic anaemia in patients with myelodysplastic syndromes (MDS). Sangre 39:105–110
Rose EH, Abels RI, Nelson RA, McCullough DM, Lessin L (1995) The use of r-HuEpo in the treatment of anaemia related to myelodysplasia (MDS). Br J Haematol 89:831–837
Wallvik J, Stenke L, Bernell P, Nordahl G, Hippe E, Hast R (2002) Serum erythropoietin (EPO) levels correlate with survival and independently predict response to EPI treatment in patients with myelodysplastic syndromes. Eur J Haematol 68:180–186
Tsabouri SE, Georgiou I, Katsaraki A, Bourantas KL (2004) Treatment of MDS patients with recombinant human erythropoietin and the role of GSTs. J Exp Clin Cancer Res 23:417–424
Gotlib J, Quesada S, Bhamidipati J et al (2004) Phase II trial of darbepoetin alfa in myelodysplastic syndrome (MDS): preliminary efficacy, safety, and in vitro results. Blood 104(11) [Abstract no. 4737]
Oliva EN, Ronco F, Danova M et al (2004) Darbepoetin efficacy in myelodysplastic syndrome. Blood 104(11) [Abstract no. 4704]
Giraldo P, Nomdedeu B, Loscertales J et al (2005) Darbepoetin alfa for the treatment of anemia in patients with myelodysplastic syndrome. Blood 106(11) [Abstract no. 2542]
Stasi R, Abruzzese E, Lanzetta G, Terzoli E, Amadori S (2005) Darbepoetin alfa for the treatment of anemic patients with low- and intermediate-1-risk myelodysplastic syndromes. Ann Oncol 16:1921–1927
Gabrilove J, Paquette R, Lyons R, et al (2006) Darbepoetin alfa for treating anemia in patients with low-risk myelodysplastic syndromes: Exploratory analysis of baseline predictors of response. J Clin Oncol 24(18S) [Abstract no. 6579 and poster presentation]
Hellstrom-Lindberg E, Gulbradsen N, Lindberg G et al (2003) A validated decision model for treating the anaemia of myelodysplastic syndromes with erythropoietin + granulocyte colony-stimulating factor: significant effects on quality of life. Br J Haematol 120:1037–1046
Jadersten M, Montgomery SM, Dybedal I, Porwit-MacDonald A, Hellstrom-Lindberg E (2005) Long-term outcome of treatment of anemia in MDS with erythropoietin and G-CSF. Blood 106:803–811
Berlin J, Santanna J, Schmid CH, Szczech LA, Feldman H (2002) Individual patient- versus group-level data meta-regressions for the investigation of treatment effect modifiers: ecological bias rears its ugly head. Stat Med 21:171–187
Epoetin alfa (ProcritÒ) product package insert. Available from URL: http://www.orthobiotech.com/common/prescribing_information/PROCRIT/PDF/ProcritBooklet.pdf. Accessed 11 Jul 2007
Darbepoetin Alfa (AranespÒ) product package insert. Available from URL: http://www.aranesp.com/pdf/aranesp_PI.pdf. Accessed 11 Jul 2007
Park S, Kelaidi C, Grabar SO, et al (2006) Prognostic factors and response duration in 419 MDS treated with erythropoietin±GCSF: The GFM experience. Blood 108(11). [Abstract no. 522]
Jadersten M, Malcovati L, Dybedal I, et al (2006) Treatment with erythropoietin and G-CSF improves survival in MDS patients with low transfusion need. Blood 108(11). [Abstract no. 521]
Musto P (2005) Recombinant erythropoietin and survival in myelodysplastic syndromes. Blood 106. [Abstract no. 2539]
Golshayan AR, Jin T, Maciejewski J et al (2007) Efficacy of growth factors compared to other therapies for low-risk myelodysplastic syndromes. Br J Haematol 137:125–132
Malcovati L, Della Porta MG, Cazzola M (2006) Predicting survival and leukemic evolution in patients with myelodysplastic syndrome. Haematologica 91:1588–1590
Armand P, Kim HT, Cutler CS et al (2007) Prognostic impact of elevated pretransplantation serum ferritin in patients undergoing myeloablative stem cell transplantation. Blood 109:4586–4588
Oliva EN, Dimitrov BD, Benedetto F, D, Angelo A, Nobile F (2005) Hemoglobin level threshold for cardiac remodeling and quality of life in myelodysplastic syndrome. Leuk Res 29:1217–1219 Epub 2005 Apr 7
Ladis V, Chouliaras G, Berdousi H, Kanavakis E, Kattamis C (2005) Longitudinal study of survival and causes of death in patients with thalassemia major in Greece. Ann N Y Acad Sci 1054:445–450
Gordeuk VR, McLaren GD, Samowitz W (1994) Etiologies, consequences, and treatment of iron overload. Crit Rev Clin Lab Sci 31:89–133
Acknowledgments
Parts of this work were presented as a poster at the American Society of Clinical Oncology (ASCO) 2006 Annual Meeting and the American Society of Hematology (ASH) 2006 Annual Meeting and Exposition. Financial support for this study was provided by Ortho Biotech Clinical Affairs, LLC. Patrick Lefebvre and Mei Sheng Duh have received research grants from Ortho Biotech Clinical Affairs, LLC. Victor Moyo, Behin Yektashenas, and Suneel Mundle are employees of Ortho Biotech Clinical Affairs, LLC. The authors would like to thank Ahmed Bourezak and Sharon Buteau of Groupe d’analyse, Ltée for their assistance with the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moyo, V., Lefebvre, P., Duh, M.S. et al. Erythropoiesis-stimulating agents in the treatment of anemia in myelodysplastic syndromes: a meta-analysis. Ann Hematol 87, 527–536 (2008). https://doi.org/10.1007/s00277-008-0450-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-008-0450-7